Abstract
Background
The importance of gene-gene and gene-environment interactions on asthma is well documented in literature, but a systematic analysis on the interaction between various genetic and environmental factors is still lacking.
Methodology/Principal Findings
We conducted a population-based, case-control study comprised of seventh-grade children from 14 Taiwanese communities. A total of 235 asthmatic cases and 1,310 non-asthmatic controls were selected for DNA collection and genotyping. We examined the gene-gene and gene-environment interactions between 17 single-nucleotide polymorphisms in antioxidative, inflammatory and obesity-related genes, and childhood asthma. Environmental exposures and disease status were obtained from parental questionnaires. The model-free and non-parametrical multifactor dimensionality reduction (MDR) method was used for the analysis. A three-way gene-gene interaction was elucidated between the gene coding glutathione S-transferase P (GSTP1), the gene coding interleukin-4 receptor alpha chain (IL4Ra) and the gene coding insulin induced gene 2 (INSIG2) on the risk of lifetime asthma. The testing-balanced accuracy on asthma was 57.83% with a cross-validation consistency of 10 out of 10. The interaction of preterm birth and indoor dampness had the highest training-balanced accuracy at 59.09%. Indoor dampness also interacted with many genes, including IL13, beta-2 adrenergic receptor (ADRB2), signal transducer and activator of transcription 6 (STAT6). We also used likelihood ratio tests for interaction and chi-square tests to validate our results and all tests showed statistical significance.
Conclusions/Significance
The results of this study suggest that GSTP1, INSIG2 and IL4Ra may influence the lifetime asthma susceptibility through gene-gene interactions in schoolchildren. Home dampness combined with each one of the genes STAT6, IL13 and ADRB2 could raise the asthma risk.
Introduction
Asthma is the most common allergic disease giving rise to the morbidity or school absence in children [1], [2]. The prevalence of childhood asthma is socially burdensome and results in significant medical expenditure around the world [3]. Many gene and environmental factors are associated with this complex disease, but the effect of each of these factors is mild. It was known that common diseases have complex etiologies such as the dependence of genotypic effects on environmental factors (i.e., gene-environment interactions) and genotypes at other loci (i.e., gene-gene interactions). Recently, there has been increased interest in gene-gene and gene-environment interactions, which may affect asthma pathophysiology.
Inflammatory lung diseases such as asthma [4] are associated with reactive oxygen species (ROS). ROS are regulated by some antioxidant genes and transcription factors. The epoxide hydroxylase (EPHX1) and glutathione S-transferase (GST) genetic variants are associated with an increased risk for lifetime asthma [5]. Obesity is an important risk factor in asthma [6], [7], [8]. Genetic variations in the obesity-related genes beta-2 adrenergic receptor (ADRB2), beta-3 adrenergic receptor (ADRB3), insulin induced gene 2 (INSIG2), and peroxisome proliferator-activated receptor gamma (PPARγ) are also included in our study [9]. Mindful of the importance of inflammation in asthma, we further included several inflammatory genes in our analysis. Interleukin (IL)-13, IL-4, interleukin 4 receptor (IL-4Ra), signal transducer and activator of transcription 6 (STAT6) and tumor necrosis factor-alpha (TNFα) genes are key inflammatory genes in the development of allergic diseases such as asthma [10], [11], [12], [13], [14], [15]. Asthma candidate genes are thought to contribute only 40–60% overall risk [16]. Gene-gene and gene-environmental interactions could explain the residual influence for asthma etiology when a single candidate gene is considered. This study is the first to systematically investigate the potential gene-gene and gene-environmental interactions on various physiological pathway genes on asthma.
Indoor exposure to dampness is suspected to be an important environmental factor for the development of asthma and allergic disease in modern societies. The Taiwan Children Health Study (TCHS) is a population-based study from 14 Taiwanese communities representing a wide range of exposures among school-aged children. This study offers an opportunity to investigate the interactive effects of gene-gene and gene-environmental influences on children's health. The multifactor dimensionality reduction (MDR) approach allows high-dimensional interactions of multiple factors to be simultaneously retrieved, and has successfully identified gene-gene interactions in a variety of diseases including breast cancer [17], essential hypertension [18], type II diabetes [19], atrial fibrillation [20], coronary artery calcification [21], and amyloid polyneuropathy [22]. In the present study, gene-gene interactions for childhood asthma were examined based on 17 SNPs in thirteen candidate genes, encompassing three physiological groups. A number of environmental factors thought to affect asthma were considered, and the associations between candidate genes and environmental factors were explored.
Results
Subjects and demographic data
Table 1 shows demographic characteristics and pulmonary function indices for study participants. FEV1, MMEF and FEV1/FVC in asthmatic children are generally lower than non-asthmatic controls. A total of 17 SNPs from thirteen candidate genes were selected for their association with childhood asthma (Table 2). All SNPs were under the Hardy-Weinberg equilibrium (HWE) [23]. Environmental factors including in utero smoking, environmental tobacco smoke (ETS), pets at home, incense burning, carpet use, cockroaches in the home and indoor dampness were used to explore the gene-environment interactions. The genotyping call rate for each SNP was over 98% in our study. Data from 1,310 samples were subjected to further gene-gene and gene-environment interaction analysis.
Table 1. demographic characteristics and pulmonary function indices for study participants.
| Asthmatics | Controls | |
| Characteristic | (N = 235) | (N = 1,075) |
| Gender | ||
| Boy | 128 (54.5) | 522(48.6) |
| Girl | 107 (45.5) | 553(51.4) |
| Age, yr | 12.7±1.0 | 12.8±0.4 |
| BMI | 20.8±4.3 | 20.4±4.1 |
| Pulmonary function indices | ||
| FVC (% predicted) | 99.9±13.3 | 100.1±13.9 |
| FEV1 (% predicted) | 97.6±14.1 | 99.9±21.9 |
| MMEF (% predicted) | 93.7±24.5 | 99.7±22.5 |
| FEV1/FVC (%) | 88.8±6.2 | 90.9±5.4 |
Values were presented by n (%) or mean ± SD.
Table 2. Genotype characteristics of each single nucleotide polymorphism.
| Gene | Chromosome position | Location | Polymorphism | MAF | HWE | P-value* |
| Inflammation SNPs | ||||||
| TNFα, rs1800629 | 6p21.3 | 5′ near gene | A/G | 0.116 | 0.135 | 0.71 |
| IL4, rs2243250 | 5q31.1 | 5′ near gene | C/T | 0.179 | 1.839 | 0.18 |
| IL13, rs20541 | 5q31 | Exon | C/T | 0.313 | 1.759 | 0.18 |
| IL13, rs848 | 5q31 | UTR-3 | G/T | 0.324 | 0.095 | 0.76 |
| IL13, rs1800925 | 5q31 | 5′ promoter region | C/T | 0.142 | 4.571 | 0.03 |
| IL4Ra, rs1805010 | 16p12.1-p11.2 | Missense | G/A | 0.493 | 8.216 | 0.00 |
| STAT6, rs324011 | 12q13 | Intron | C/T | 0.244 | 0.064 | 0.80 |
| Obesity-related SNPs | ||||||
| INSIG2, rs7566605 | 2q14.2 | Intron | C/G | 0.399 | 0.001 | 0.98 |
| PPARγ, rs1801282 | 3p25 | Exon | C/G | 0.045 | 2.391 | 0.12 |
| ADRB2, rs1042713 | 5q31-q32 | Missense | A/G | 0.415 | 2.887 | 0.09 |
| ADRB2, rs1042714 | 5q31-q32 | Missense | C/G | 0.096 | 0.398 | 0.53 |
| ADRB3, rs4994 | 8p12 | Missense | C/T | 0.153 | 0.570 | 0.45 |
| Antioxidative SNPs | ||||||
| EPHX1 exon 4, rs2234922 | 1q42.1 | Exon | A/G | 0.137 | 4.828 | 0.03 |
| EPHX1 exon 3, rs1051740 | 1q42.1 | Exon | C/T | 0.471 | 0.813 | 0.37 |
| GSTP1, rs1695 | 11q13 | Exon | A/G | 0.178 | 0.213 | 0.64 |
| GSTT1 | 22q11.23 | |||||
| GSTM1 | 1p13.3 | |||||
Notes: MAF, minor allele frequency; HWE, Hardy Weinberg Equilibrium.
p-value for Hardy-Weinberg Equilibrium.
Gene-gene interactions in childhood asthma
MDR was used to analyze gene-gene interaction models in childhood asthma. The two- to ten-way gene-gene interaction models are listed in Table 3. The SNP (rs1805010) in the IL4Ra gene had the highest testing-balanced accuracy among the 17 SNPs. A three-way interaction found between GSTP1, IL4Ra and INSIG2 showed the highest testing-balanced accuracy and cross-validation consistency. A two-way interaction model of IL4Ra and INSIG2 also exhibited high testing-balanced accuracy and cross-validation consistency, but the testing-balanced accuracy was lower than the three-way interaction model. In order to elucidate potential two- and three-way gene-gene interactions in childhood asthma, the top ten two-way and three-way interaction models were listed (Table 4, Table 5). The rank was determined by the training-balanced accuracy of MDR. In the two-way gene-gene interaction models (Table 4), interaction between IL4Ra and INSIG2 has the highest training-balanced accuracy at 56.82%. IL4Ra also has a statistically significant interaction with EPHX1 exon4 in childhood asthma. For the three-way interaction models (Table 5), interaction between GSTP1, IL4Ra, and INSIG2 had the highest training-balanced accuracy. The information gain derived by the entropy-based analysis in the MDR software package was all positive in each pair-wise combination of GSTP1, IL4Ra and INSIG2.
Table 3. Summary of MDR gene-gene interaction results.
| Model | Training Bal. Acc. (%) | Testing Bal. Acc. (%) | Cross-validation Consistency |
| IL4Ra | 53.98 | 49.04 | 7/10 |
| IL4Ra, INSIG2 | 56.83 | 55.78 | 9/10 |
| GSTP1, IL4Ra, INSIG2 | 60.93 | 57.83 | 10/10 |
| GSTP1, IL4Ra, INSIG2, IL13 (rs1800925) | 64.99 | 57.75 | 6/10 |
| GSTP1, IL4Ra, INSIG2, ADRB2 (rs1042713), EPHX1 exon 3 | 70.72 | 49.31 | 5/10 |
Table 4. Two-way gene-gene interactions of MDR analysis.
| Rank | Model | Training Bal. Acc. (%) | Testing Bal. Acc. (%) | P-value* | P-value# | |
| 1 | IL4Ra | INSIG2 | 56.82 | 55.78 | 0.011 | 0.007 |
| 2 | IL4Ra | EPHX1 exon 4 | 55.80 | 53.77 | 0.085 | 0.108 |
| 3 | IL4Ra | STAT6 | 55.73 | 53.86 | 0.079 | 0.094 |
| 4 | IL4Ra | GSTT1 | 55.58 | 55.58 | 0.018 | 0.010 |
| 5 | IL4Ra | IL4 | 55.39 | 53.54 | 0.099 | 0.133 |
| 6 | GSTP1 | IL13 (rs1800925) | 55.34 | 54.73 | 0.037 | 0.037 |
| 7 | IL13 (rs848) | ADRB2 (rs1042713) | 55.34 | 53.75 | 0.085 | 0.110 |
| 8 | IL4 | IL13 (rs1800925) | 55.25 | 54.80 | 0.035 | 0.036 |
| 9 | EPHX1 exon 4 | IL13 (rs20541) | 55.17 | 54.80 | 0.035 | 0.036 |
| 10 | IL4Ra | GSTP1 | 55.00 | 53.61 | 0.093 | 0.127 |
Two- or Three-way interactions were validated based on 1000 permutations.
Two- or Three-way interactions were validated based on 1000 explicit tests.
Table 5. Three-way gene-gene interactions of MDR analysis.
| Rank | Model | Training Bal. Acc. (%) | Testing Bal. Acc. (%) | P-value* | P-value# | ||
| 1 | GSTP1 | IL4Ra | INSIG2 | 60.93 | 57.83 | 0.002 | 0.001 |
| 2 | STAT6 | IL4Ra | INSIG2 | 59.03 | 51.84 | 0.251 | 0.310 |
| 3 | IL13 (rs848) | STAT6 | ADRB2 (rs1042713) | 59.01 | 55.57 | 0.017 | 0.016 |
| 4 | ADRB2 (rs1042714) | IL4Ra | INSIG2 | 58.82 | 55.31 | 0.023 | 0.022 |
| 5 | ADRB3 | IL4Ra | INSIG2 | 58.77 | 56.34 | 0.008 | 0.006 |
| 6 | IL13 (rs1800925) | IL4Ra | INSIG2 | 58.68 | 53.59 | 0.084 | 0.114 |
| 7 | EPHX1 exon 3 | IL4Ra | INSIG2 | 58.62 | 54.23 | 0.057 | 0.073 |
| 8 | EPHX1 exon 3 | IL4Ra | IL4 | 58.47 | 53.08 | 0.122 | 0.161 |
| 9 | ADRB2 (rs1042713) | IL4Ra | INSIG2 | 58.45 | 51.99 | 0.240 | 0.294 |
| 10 | GSTP1 | IL4Ra | STAT6 | 58.38 | 55.12 | 0.028 | 0.026 |
Two- or Three-way interactions were validated based on 1000 permutations.
Two- or Three-way interactions were validated based on 1000 explicit tests.
Moreover, the IL4Ra and INSIG2 gene combination interacted with GSTP1, STAT6, ADRB2, ADRB3, IL13 and EPHX1 exon 3 to reveal a high training-balanced accuracy above 58.38% in childhood asthma.
Gene-environment interactions in childhood asthma
MDR analysis was used to investigate probable gene-environment interactions in childhood asthma, and revealed the interaction between 17 SNPs and 9 environmental factors. Dampness was found to be the most important environmental factor affecting asthma susceptibility (Table 6). Two-way interactions showed higher testing-balanced accuracy and cross-validation consistency, indicating that two-way interaction models were the candidate gene-environment models in our population. The top ten two-way interaction models are shown in Table 7. The interaction of preterm birth and indoor dampness had the highest training-balanced accuracy at 59.09%. IL4Ra-BMI interaction also affected asthma susceptibility with a high training balanced accuracy. In addition, indoor dampness also interacted with many genes including IL13, ADRB2, and STAT6. The lowest training-balanced accuracy was 57.34%, higher than the training-balanced accuracy of 56.98% obtained when home dampness was a single predictor (Table 6). In the two-way interaction listed in Table 7, home dampness seems to be the most important environment factor.
Table 6. Summary of gene-environment interaction results.
| Model | Training Bal. Acc. (%) | Testing Bal. Acc. (%) | Cross-validation Consistency |
| Dampness | 56.98 | 56.98 | 10/10 |
| Preterm birth, Dampness | 59.09 | 55.60 | 8/10 |
| IL4Ra, INSIG2, BMI | 62.00 | 52.17 | 5/10 |
| IL4Ra, INSIG2, IL13 (rs20541) , BMI | 67.88 | 50.60 | 4/10 |
| IL4Ra, INSIG2, EPHX1 exon 3, ADRB2 (rs1042713), BMI | 76.76 | 49.30 | 9/10 |
Table 7. Two-way gene-environment interactions of MDR analysis.
| Rank | Model | Training Bal. Acc. (%) | Testing Bal. Acc. (%) | P-value* | P-value# | |
| 1 | Preterm birth | Dampness | 59.09 | 55.60 | 0.003 | 1.000 |
| 2 | IL4Ra | BMI | 58.42 | 55.26 | 0.008 | 1.000 |
| 3 | Dampness | BMI | 58.27 | 56.88 | 0.002 | 0.934 |
| 4 | Carpet | Dampness | 58.04 | 58.04 | 0.001 | 0.701 |
| 5 | STAT6 | Dampness | 57.85 | 57.22 | 0.001 | 0.914 |
| 6 | IL13 (rs20541) | Dampness | 57.75 | 56.41 | 0.002 | 0.967 |
| 7 | IL13 (rs1800925) | Dampness | 57.54 | 57.54 | 0.001 | 0.883 |
| 8 | Preterm birth | BMI | 57.49 | 56.42 | 0.002 | 0.966 |
| 9 | in utero ETS | Dampness | 57.40 | 56.80 | 0.002 | 0.947 |
| 10 | ADRB2 (rs1042714) | Dampness | 57.34 | 57.03 | 0.001 | 0.914 |
Two-way gene-environment interactions were validated based on 1000 permutations.
Two- or Three-way interactions were validated based on 1000 explicit tests.
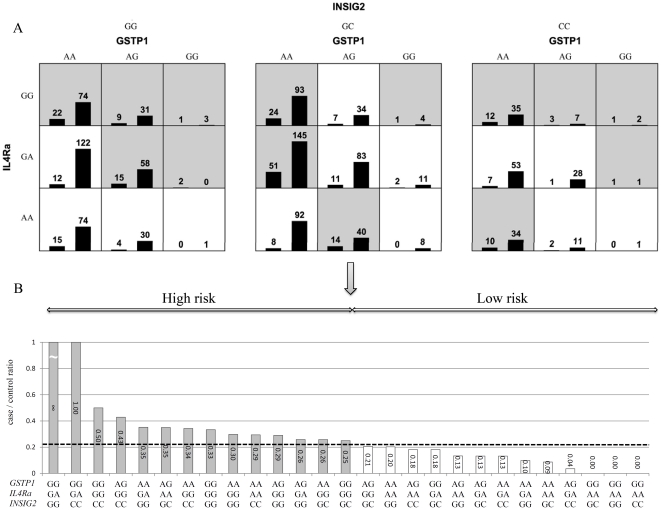
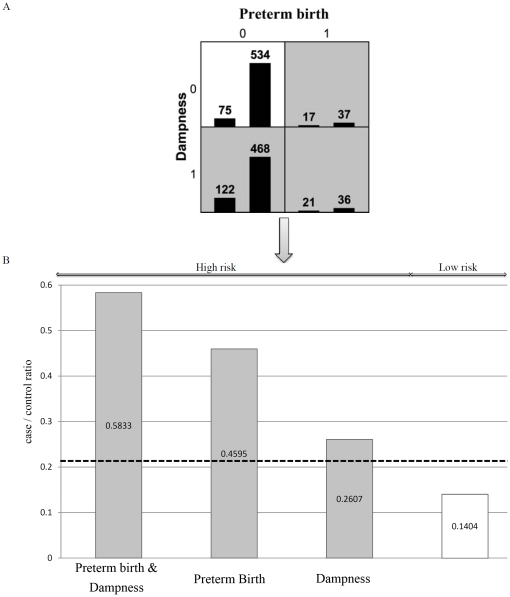
Validation of gene-gene and gene-environment interactions
Two-way and three-way gene-gene and gene-environment interactions were examined using the detailed interaction model of MDR (Fig. 1 and Fig. 2). We used the likelihood ratio tests to validate the gene-gene interactions between IL4Ra and INSIG2 on childhood asthma and the P-value was 0.029. The three-way interaction between GSTP1, IL4Ra, and INSIG2 genes was also significant (P for LRT interaction = 0.003).
Figure 1. The best three-way gene-gene interaction between IL4Ra, INSIG2, and GSTP1 for childhood asthma.
(A) The 27 genotype combinations displayed by MDR. High-risk genotype combinations are in grey and low-risk genotype combinations in white. The left bar represent the asthma group and the right bar represent the controls. (B) The validation of high and low risk classification by Chi-square test.
Figure 2. The best two-way gene-environment interaction between preterm birth and home dampness for childhood asthma.
(A) The 4 gene-environment combinations displayed by MDR. High-risk genotype combinations are in grey and low-risk genotype combinations in white. The left bar represent the asthma group and the right bar represent the controls. (B) The validation of high and low risk classification by Chi-square test.
Chi-square tests were used to validate the high risk and low risk phenotype classification. The dimensional reduction of the three-way gene-gene interaction between GSTP1, IL4Ra and INSIG2 is shown in Fig. 1A. Of the 27 combinations of three-way gene-gene interaction, GSTP1 GG, IL4Ra GA and INSIG2 GG resulted in the highest risk for childhood asthma. Chi-square tests also showed statistical significance (P<0.001) (Fig. 1B). The detailed model of two-way gene-environment interaction between high risk and low risk groups of childhood asthma is shown in Fig. 2A. In the two-way gene-environment interaction model shown in Fig. 2B, the interaction between preterm birth and indoor dampness revealed the highest risk at 59.09%. The lowest risk combination in preterm birth and dampness was 14.04%. Chi-square tests also showed significant differences between high risk and low risk classification on childhood asthma.
Discussion
To the best of our knowledge, this study is the first to elucidate potential interactions between antioxidative, inflammatory and obesity-related genes on childhood asthma. Using an MDR approach, our study suggests a three-way gene-gene interaction between inflammatory gene IL4Ra, obesity-related gene INSIG2, and antioxidative gene GSTP1. The three-way gene-gene interaction between IL4Ra, INSIG2, and GSTP1 was not only identified in gene-gene analyses but also confirmed in gene-environment analyses in MDR approach. The entropy-based analysis indicated that the interaction between GSTP1, IL4Ra and INSIG2 was synergistic. The results of the gene-environment interaction analyses showed that there was an association between preterm birth and home dampness among schoolchildren. Children carrying asthma candidate genes were more susceptible to adverse effects of home dampness.
The link between asthma and obesity in childhood has been examined in many epidemiological studies [24], [25], [26]. A recent meta-analysis showed that children with high body weight were at increased risk of developing asthma [7]. Patients with allergic asthma showed significant higher BMI and insulin resistance than non-asthmatic controls [27]. Some adipokines secreted by adipose tissue have pro-inflammatory effects and also show the potential to modulate the Th2 immunity [28]. SNP rs7566605 in INSIG2 gene is a common genetic variant associated with obesity [29]. Herbert and colleagues reported the association between SNP (rs7566605) upstream of the INSIG2 with higher BMI [29]. The SNP (rs7566605) genotype CC was significantly associated with obesity. In animal models, the INSIG1 and INSIG2 gene double-knockout mice were found to be more obese than the control mice [30]. We found that the INSIG2 gene played a key role in the three-way gene-gene interaction (Table 3). Our results constitute new evidence that obesity-related genes may show interactive effects with asthma candidate genes, such as antioxidative and Th2 pathway inflammatory genes.
Although the underlying mechanism for the link between asthma and obesity is still not fully understood, some pathophysiological pathways have been suggested , such as altered lung mechanics, enhanced systemic pro-inflammatory state, shared inherited predispositions and dietary intake [31], as well as the increased systemic oxidant stress [8], [32]. In a community-based study, Keaney et al. reported that BMI was strongly associated with the increased systemic oxidative stress, estimated by 8-epi-PGF2α [33]. Correlation between fat accumulation and systemic oxidative stress was also found in animal models. In obese mice, reactive oxygen species (ROS) level was noted to be increased selectively in adipose tissue, accompanied by decreased expression of antioxidative enzymes [34]. ROS is responsible for many chronic lung diseases such as asthma, and is proposed to be the major source of cell and tissue damage [4]. Glutathione-transferases (GSTs) play important roles in airway antioxidant defenses [4], and theGSTP1 gene contributes more than 90% of GST-derived enzyme activity in human lung epithelium [35]. Our findings suggest that the GSTP1 gene may be the most important gene in the antioxidative gene group (Table 3). The three-way gene-gene interaction involves GSTP1 and INSIG2 characterize the obesity affects on antioxidative gene further influence asthma.
Obesity-associated low-grade systemic inflammation has been suggested to be a major factor mediating the asthma susceptibility in many studies [36], [37], [38]. Polymorphisms in the inflammatory gene IL4Ra are associated with numerous atopic diseases such as asthma [39], [40]. In a previous study among German children, the combination of the IL4, IL13, STAT6 and IL4Ra genes was revealed to increase the risk of bronchial asthma up to 16.8 times compared with the effects of individual gene polymorphisms [41]. IL13 and IL4 cytokines produced by Th2 cells and inducing IgE after allergen exposure are noted to share a common receptor IL4Ra [42]. The IL4Ra is a key component in the induction of the Th2 lymphocyte phenotype and its antagonist improved respiratory function and asthma control in human studies [43], [44]. Results from the top ten gene-gene interaction models elucidated the IL4Ra gene as a hub for gene-gene interactions on childhood asthma (Table 5), supporting that the IL4Ra gene may be the key regulatory element of the Th2 immune response. Gene-gene interaction between IL13 and IL4Ra was reported to affect asthma in white Dutch and Chinese populations [45]. Since MDR determines one optimal interaction model that can successfully predict high/low risk asthma phenotype, the combination of IL13 and IL4Ra gene may not be the optimal model in our analysis.
Asthma is a complex disease affected by many genetic factors, which in turn may be influenced by environmental exposures. Taiwan is located in a subtropical climate zone, with high temperatures and humidity (monthly mean 68–80%). Home dampness is a common problem and an important environmental factor for asthma [46], [47], [48], [49]. However, few studies are concerned with the genetic modification effects of home dampness on childhood asthma [50]. In our data, the gene-environmental MDR analyses showed that home dampness is the most important environmental factor on childhood asthma (Table 7). Using home dampness as a predictor, the testing accuracy on asthma is 56.98% (Table 6). Home dampness combined with each one of the genes STAT6, IL13 and ADRB2 raised the testing accuracy on asthma higher than 57.34% (Table 7). Our findings from interaction models with significant permutated p-values but non-significant explicit p-values might be due to the strong marginal effects from environment variables.
The six-way interaction model also showed 10/10 cross-validation consistency and high training-balanced accuracy (tables 3), but this result was not followed-up due to low testing-balanced accuracy. Low testing-balanced accuracy may be caused by the model over-fitting problem, in which the generated model fits the training data too well, increasing the high generalization error [51]. The presence of noise or paucity of representative samples in the training dataset is possible causes of model over-fitting. A model that is too complex may fit the noise, leading to lower testing-balanced efficiency. In our analysis, we used a 10-fold cross-validation approach to avoid the model over-fitting problem.
Our study has some limitations. Asthma assessment was based on parental questionnaire reports. Although misclassification of asthma status may have arisen, questionnaires are widely used to define respiratory outcomes in epidemiologic studies among children [52], [53]. Another possible limitation is the retrospective recall of environmental exposures by questionnaire, which is likely to have resulted in some misclassification. However, the reliability and validity of questionnaire on measuring dampness exposure has been verified by a strong association between inspectors and self-reported dampness [51], [52]. Due to limitations of the MDR model approach, any participants with missing data were eliminated in our study, which made selection bias possible. However, in our analysis it was found that participants without missing data did not differ greatly from all eligible participants on most of the demographic factors (data not shown).
In conclusion, our study suggests that gene-gene interactions may occur between different pathophysiological pathways and a significant three-way gene-gene interaction between GSTP1, INSIG2 and IL4Ra on childhood asthma. Home dampness combined with each one of the genes STAT6, IL13 and ADRB2 could also raise the asthma risk. Further classifying asthma into different phenotypes and whole genome association genotyping will improve the understanding of gene-gene interactions. The MDR interaction model may work as a phenotype predictor based on the genetic information to improve the clinical diagnosis.
Materials and Methods
Ethics Statement
The study protocol was approved by the institutional review board of National Taiwan University Hospital and complied with the principles outlined in the Helsinki Declaration. All participants gave written informed consent.
Study population
The study protocol was approved by the institutional review board of National Taiwan University Hospital and complied with the principles outlined in the Helsinki Declaration. TCHS recruited 4,134 seventh-grade children from 14 diverse communities in Taiwan. The design and study protocol for the TCHS has been published previously [50], [54]. Information on childhood exposure to indoor dampness and health status were collected with a questionnaire, which was completed by the child's parents or guardians. In this study, a total of 3,810 children who provided their oral mucosa were subjected for genotyping. All participating children were arranged to measure height/weight and complete pulmonary function tests with functional vital capacity (FVC), forced expiratory volume in 1 second (FEV1) and maximal mid-expiratory flow (MMEF) recorded. The sex-specific percentage predicted pulmonary function indices were estimated by using linear regression models [55], [56].
Definition of asthma
Children were considered to have asthma if there was an affirmative answer to the question “Has a doctor ever diagnosed this child as having asthma?” There were 235 asthmatic children in our cohort. Family history of asthma or atopic diseases, and a personal history of wheeze or bronchitis may affect asthma susceptibility. With a proper consideration for non-asthmatic selection, the control group in present study comprised of 1,075 children without wheeze, bronchitis, or family history of either asthma or atopic disease.
Environmental exposure assessment
Environmental factors comprised in utero exposure to maternal smoking (in utero ETS), preterm birth, pet ownership, cockroaches in the home, household carpet use and environmental tobacco smoke (ETS) at home. Body mass index (BMI) was calculated as weight/(height)2[kg/m2] and we categorized the study participants into quartiles. The baseline questionnaire collected information on several dampness indices at home. Home dampness was established by an affirmative answer to one of following questions: “Have you had visible mould in the walls or bathroom in your house in the past 12 months?”; “Have you perceived mould odor in the house during the past 12 months?” and “Have you perceived wet stamps due to moisture in the ceilings, floors or walls of your house during the past 12 months?”.
DNA collection and genotyping
Genomic DNA was isolated from cotton swabs containing oral mucosa using the phenol/chloroform extraction method [50], [54]. All oral mucosa samples were stored at −80°C. The 17 single nucleotide polymorphisms (SNPs) were assessed by real-time polymerase chain reaction (PCR) using the TaqMan Allelic Discrimination (AD) assay on an ABI PRISMTM 7900 Sequence Detector (Applied Biosystems, Foster City, CA).
Multifactor dimensionality reduction (MDR) analysis
The selected candidate genes were classified into three categories: inflammatory genes, obesity-related genes, and antioxidative genes. Gene-gene and gene-environment interactions were detected by an open-source MDR software package [57], [58]. MDR is a model-free and non-parametrical approach method that can identify high dimensional gene-gene or gene-environment interactions in a small population [57]. The combinations of factors which provide the most information in high risk and low risk group classification are suggested to be the most significant gene-gene or gene-environment interactions. There are no underlying assumptions about the independence or biological relevance of SNPs or any other factor. Previous studies have shown MDR to be a useful method for identifying gene-gene interactions in high dimensional data [58].
The MDR algorithm determines one optimal model that can successfully predict a high risk and low risk phenotype in a study population. Subjects with missing values in any of the factors should be deleted prior to data import. Firstly, the sample dataset is divided into training and an independent testing sub dataset for cross-validation. Cross-validation aims to avoid the model over fitting problem. Secondly, an exhaustive search of a listed of n genetic and environmental factors is performed. For example, for two loci with three genotypes each, there are nine possible combinations. Then, the case/control ratio for each combination is counted. Finally, each combination is assigned as high risk or low risk based on the comparison to the sample population case/control ratio. If the case/control ratio of a multifactor combination is higher than the original population, then this combination is labeled as a high risk group and vice versa. Multidimensional data are reduced to one dimension with two classes via this rocess.
An MDR model with the best testing-balanced accuracy and cross-validation consistency is selected. For example, in a 10-fold cross-validation, the original dataset is divided into 10 subsets. The maximum value of cross-validation consistency is 10 if the same combination of factors is identified across all 10 subsets, and the minimum value is 1. When the number of cases and controls are not equal, balanced-accuracy weighs the classification accuracy of the two classes equally, which is more powerful than using accuracy alone. Testing balanced-accuracy is obtained from the sum of true positive plus true negative divided by the total number of samples in the testing dataset.
For those interaction models that showed higher testing-balanced accuracy, we further used permutation tests, explicit tests [59], and the likelihood ratio test (LRT) comparing a full model that included an interaction term with a reduce model to validate the MDR interaction results on childhood asthma. The significant difference between high and low risk group on childhood asthma was also validated by chi-square tests. Furthermore, we used the entropy-based analysis included in the MDR software package to determine whether the interactions are synergistic or non-synergistic [60].
Acknowledgments
The authors thank all the field workers who supported the data collection, the school administrators and teachers, and especially the parents and children who participated in this study.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This study was supported by grants #98-2314-B-002-138-MY3, #96-2314-B-006-053 and #95-2314-B-006-103 from Taiwan National Science Council. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Spee-van der Wekke J, Meulmeester JF, Radder JJ, Verloove-Vanhorick SP. School absence and treatment in school children with respiratory symptoms in The Netherlands: data from the Child Health Monitoring System. J Epidemiol Community Health. 1998;52:359–363. doi: 10.1136/jech.52.6.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Silverstein MD, Mair JE, Katusic SK, Wollan PC, O'Connell EJ, et al. School attendance and school performance: a population-based study of children with asthma. J Pediatr. 2001;139:278–283. doi: 10.1067/mpd.2001.115573. [DOI] [PubMed] [Google Scholar]
- 3.Weiss KB, Sullivan SD. Socio-economic burden of asthma, allergy, and other atopic illnesses. Pediatr Allergy Immunol. 1994;5:7–12. doi: 10.1111/j.1399-3038.1994.tb00341.x. [DOI] [PubMed] [Google Scholar]
- 4.Rahman I, MacNee W. Oxidative stress and regulation of glutathione in lung inflammation. Eur Respir J. 2000;16:534–554. doi: 10.1034/j.1399-3003.2000.016003534.x. [DOI] [PubMed] [Google Scholar]
- 5.Salam MT, Lin PC, Avol EL, Gauderman WJ, Gilliland FD. Microsomal epoxide hydrolase, glutathione S-transferase P1, traffic and childhood asthma. Thorax. 2007;62:1050–1057. doi: 10.1136/thx.2007.080127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beuther DA, Sutherland ER. Overweight, obesity, and incident asthma: a meta-analysis of prospective epidemiologic studies. Am J Respir Crit Care Med. 2007;175:661–666. doi: 10.1164/rccm.200611-1717OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Flaherman V, Rutherford GW. A meta-analysis of the effect of high weight on asthma. Arch Dis Child. 2006;91:334–339. doi: 10.1136/adc.2005.080390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shore SA. Obesity and asthma: possible mechanisms. J Allergy Clin Immunol. 2008;121:1087–1093; quiz 1094–1085. doi: 10.1016/j.jaci.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 9.Rooyen JM, Pretorius PJ, Britz M, Huisman HW, Schutte AE, et al. Genetic polymorphisms of beta2- and beta3-adrenergic receptor genes associated with characteristics of the metabolic syndrome in black South African women. Exp Clin Endocrinol Diabetes. 2008;116:236–240. doi: 10.1055/s-2007-992785. [DOI] [PubMed] [Google Scholar]
- 10.Busse WW, Lemanske RF., Jr Asthma. N Engl J Med. 2001;344:350–362. doi: 10.1056/NEJM200102013440507. [DOI] [PubMed] [Google Scholar]
- 11.Wills-Karp M, Chiaramonte M. Interleukin-13 in asthma. Curr Opin Pulm Med. 2003;9:21–27. doi: 10.1097/00063198-200301000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Wenzel S, Wilbraham D, Fuller R, Getz EB, Longphre M. Effect of an interleukin-4 variant on late phase asthmatic response to allergen challenge in asthmatic patients: results of two phase 2a studies. Lancet. 2007;370:1422–1431. doi: 10.1016/S0140-6736(07)61600-6. [DOI] [PubMed] [Google Scholar]
- 13.Schedel M, Carr D, Klopp N, Woitsch B, Illig T, et al. A signal transducer and activator of transcription 6 haplotype influences the regulation of serum IgE levels. J Allergy Clin Immunol. 2004;114:1100–1105. doi: 10.1016/j.jaci.2004.07.048. [DOI] [PubMed] [Google Scholar]
- 14.Trabetti E, Patuzzo C, Malerba G, Galavotti R, Martinati LC, et al. Association of a lymphotoxin alpha gene polymorphism and atopy in Italian families. J Med Genet. 1999;36:323–325. [PMC free article] [PubMed] [Google Scholar]
- 15.Shin HD, Park BL, Kim LH, Jung JH, Wang HJ, et al. Association of tumor necrosis factor polymorphisms with asthma and serum total IgE. Hum Mol Genet. 2004;13:397–403. doi: 10.1093/hmg/ddh036. [DOI] [PubMed] [Google Scholar]
- 16.McLeish S, Turner SW. Gene-environment interactions in asthma. Arch Dis Child. 2007;92:1032–1035. doi: 10.1136/adc.2006.112185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ritchie MD, Hahn LW, Roodi N, Bailey LR, Dupont WD, et al. Multifactor-dimensionality reduction reveals high-order interactions among estrogen-metabolism genes in sporadic breast cancer. Am J Hum Genet. 2001;69:138–147. doi: 10.1086/321276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moore JH, Williams SM. New strategies for identifying gene-gene interactions in hypertension. Ann Med. 2002;34:88–95. doi: 10.1080/07853890252953473. [DOI] [PubMed] [Google Scholar]
- 19.Cho YM, Ritchie MD, Moore JH, Park JY, Lee KU, et al. Multifactor-dimensionality reduction shows a two-locus interaction associated with Type 2 diabetes mellitus. Diabetologia. 2004;47:549–554. doi: 10.1007/s00125-003-1321-3. [DOI] [PubMed] [Google Scholar]
- 20.Tsai CT, Lai LP, Lin JL, Chiang FT, Hwang JJ, et al. Renin-angiotensin system gene polymorphisms and atrial fibrillation. Circulation. 2004;109:1640–1646. doi: 10.1161/01.CIR.0000124487.36586.26. [DOI] [PubMed] [Google Scholar]
- 21.Bastone L, Reilly M, Rader DJ, Foulkes AS. MDR and PRP: a comparison of methods for high-order genotype-phenotype associations. Hum Hered. 2004;58:82–92. doi: 10.1159/000083029. [DOI] [PubMed] [Google Scholar]
- 22.Soares ML, Coelho T, Sousa A, Batalov S, Conceicao I, et al. Susceptibility and modifier genes in Portuguese transthyretin V30M amyloid polyneuropathy: complexity in a single-gene disease. Hum Mol Genet. 2005;14:543–553. doi: 10.1093/hmg/ddi051. [DOI] [PubMed] [Google Scholar]
- 23.Balding DJ. A tutorial on statistical methods for population association studies. Nat Rev Genet. 2006;7:781–791. doi: 10.1038/nrg1916. [DOI] [PubMed] [Google Scholar]
- 24.Shaheen SO, Sterne JA, Montgomery SM, Azima H. Birth weight, body mass index and asthma in young adults. Thorax. 1999;54:396–402. doi: 10.1136/thx.54.5.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hancox RJ, Milne BJ, Poulton R, Taylor DR, Greene JM, et al. Sex differences in the relation between body mass index and asthma and atopy in a birth cohort. Am J Respir Crit Care Med. 2005;171:440–445. doi: 10.1164/rccm.200405-623OC. [DOI] [PubMed] [Google Scholar]
- 26.von Mutius E, Schwartz J, Neas LM, Dockery D, Weiss ST. Relation of body mass index to asthma and atopy in children: the National Health and Nutrition Examination Study III. Thorax. 2001;56:835–838. doi: 10.1136/thorax.56.11.835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Husemoen LL, Glumer C, Lau C, Pisinger C, Morch LS, et al. Association of obesity and insulin resistance with asthma and aeroallergen sensitization. Allergy. 2008;63:575–582. doi: 10.1111/j.1398-9995.2007.01613.x. [DOI] [PubMed] [Google Scholar]
- 28.Heijink IH, Vellenga E, Borger P, Postma DS, de Monchy JG, et al. Interleukin-6 promotes the production of interleukin-4 and interleukin-5 by interleukin-2-dependent and -independent mechanisms in freshly isolated human T cells. Immunology. 2002;107:316–324. doi: 10.1046/j.1365-2567.2002.01501.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Herbert A, Gerry NP, McQueen MB, Heid IM, Pfeufer A, et al. A common genetic variant is associated with adult and childhood obesity. Science. 2006;312:279–283. doi: 10.1126/science.1124779. [DOI] [PubMed] [Google Scholar]
- 30.Engelking LJ, Liang G, Hammer RE, Takaishi K, Kuriyama H, et al. Schoenheimer effect explained–feedback regulation of cholesterol synthesis in mice mediated by Insig proteins. J Clin Invest. 2005;115:2489–2498. doi: 10.1172/JCI25614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weiss ST. Obesity: insight into the origins of asthma. Nat Immunol. 2005;6:537–539. doi: 10.1038/ni0605-537. [DOI] [PubMed] [Google Scholar]
- 32.Komakula S, Khatri S, Mermis J, Savill S, Haque S, et al. Body mass index is associated with reduced exhaled nitric oxide and higher exhaled 8-isoprostanes in asthmatics. Respir Res. 2007;8:32. doi: 10.1186/1465-9921-8-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Keaney JF, Larson MG, Vasan RS, Wilson PW, Lipinska I, et al. Obesity and systemic oxidative stress: clinical correlates of oxidative stress in the Framingham Study. Arterioscler Thromb Vasc Biol. 2003;23:434–439. doi: 10.1161/01.ATV.0000058402.34138.11. [DOI] [PubMed] [Google Scholar]
- 34.Furukawa S, Fujita T, Shimabukuro M, Iwaki M, Yamada Y, et al. Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Invest. 2004;114:1752–1761. doi: 10.1172/JCI21625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fryer AA, Hume R, Strange RC. The development of glutathione S-transferase and glutathione peroxidase activities in human lung. Biochim Biophys Acta. 1986;883:448–453. doi: 10.1016/0304-4165(86)90283-7. [DOI] [PubMed] [Google Scholar]
- 36.Sutherland TJ, Cowan JO, Young S, Goulding A, Grant AM, et al. The association between obesity and asthma: interactions between systemic and airway inflammation. Am J Respir Crit Care Med. 2008;178:469–475. doi: 10.1164/rccm.200802-301OC. [DOI] [PubMed] [Google Scholar]
- 37.Sutherland ER. Obesity and asthma. Immunol Allergy Clin North Am. 2008;28:589–602, ix. doi: 10.1016/j.iac.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sin DD, Sutherland ER. Obesity and the lung: 4. Obesity and asthma. Thorax. 2008;63:1018–1023. doi: 10.1136/thx.2007.086819. [DOI] [PubMed] [Google Scholar]
- 39.Mitsuyasu H, Izuhara K, Mao XQ, Gao PS, Arinobu Y, et al. Ile50Val variant of IL4R alpha upregulates IgE synthesis and associates with atopic asthma. Nat Genet. 1998;19:119–120. doi: 10.1038/472. [DOI] [PubMed] [Google Scholar]
- 40.Hershey GK, Friedrich MF, Esswein LA, Thomas ML, Chatila TA. The association of atopy with a gain-of-function mutation in the alpha subunit of the interleukin-4 receptor. N Engl J Med. 1997;337:1720–1725. doi: 10.1056/NEJM199712113372403. [DOI] [PubMed] [Google Scholar]
- 41.Kabesch M, Schedel M, Carr D, Woitsch B, Fritzsch C, et al. IL-4/IL-13 pathway genetics strongly influence serum IgE levels and childhood asthma. J Allergy Clin Immunol. 2006;117:269–274. doi: 10.1016/j.jaci.2005.10.024. [DOI] [PubMed] [Google Scholar]
- 42.White SR, Martin LD, Stern R, Laxman B, Marroquin BA. Expression of IL-4/IL-13 receptors in differentiating human airway epithelial cells. Am J Physiol Lung Cell Mol Physiol. 2010;299:L681–693. doi: 10.1152/ajplung.00422.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Borish LC, Nelson HS, Lanz MJ, Claussen L, Whitmore JB, et al. Interleukin-4 receptor in moderate atopic asthma. A phase I/II randomized, placebo-controlled trial. Am J Respir Crit Care Med. 1999;160:1816–1823. doi: 10.1164/ajrccm.160.6.9808146. [DOI] [PubMed] [Google Scholar]
- 44.Sandford AJ, Chagani T, Zhu S, Weir TD, Bai TR, et al. Polymorphisms in the IL4, IL4RA, and FCERIB genes and asthma severity. J Allergy Clin Immunol. 2000;106:135–140. doi: 10.1067/mai.2000.107926. [DOI] [PubMed] [Google Scholar]
- 45.Chan IH, Leung TF, Tang NL, Li CY, Sung YM, et al. Gene-gene interactions for asthma and plasma total IgE concentration in Chinese children. J Allergy Clin Immunol. 2006;117:127–133. doi: 10.1016/j.jaci.2005.09.031. [DOI] [PubMed] [Google Scholar]
- 46.Simoni M, Lombardi E, Berti G, Rusconi F, La Grutta S, et al. Mould/dampness exposure at home is associated with respiratory disorders in Italian children and adolescents: the SIDRIA-2 Study. Occup Environ Med. 2005;62:616–622. doi: 10.1136/oem.2004.018291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jaakkola JJ, Hwang BF, Jaakkola N. Home dampness and molds, parental atopy, and asthma in childhood: a six-year population-based cohort study. Environ Health Perspect. 2005;113:357–361. doi: 10.1289/ehp.7242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hagmolen of Ten Have W, van den Berg NJ, van der Palen J, van Aalderen WM, Bindels PJ. Residential exposure to mould and dampness is associated with adverse respiratory health. Clin Exp Allergy. 2007;37:1827–1832. doi: 10.1111/j.1365-2222.2007.02841.x. [DOI] [PubMed] [Google Scholar]
- 49.Lawson JA, Rennie DC, Senthilselvan A, Cockcroft DW, McDuffie HH. Regional variations in risk factors for asthma in school children. Can Respir J. 2005;12:321–326. doi: 10.1155/2005/942637. [DOI] [PubMed] [Google Scholar]
- 50.Tsai CH, Tung KY, Chen CH, Lee YL. Tumour necrosis factor G-308A polymorphism modifies the effect of home dampness on childhood asthma. Occup Environ Med. 2011 doi: 10.1136/oem.2010.060970. [DOI] [PubMed] [Google Scholar]
- 51.Motsinger AA, Ritchie MD. The effect of reduction in cross-validation intervals on the performance of multifactor dimensionality reduction. Genet Epidemiol. 2006;30:546–555. doi: 10.1002/gepi.20166. [DOI] [PubMed] [Google Scholar]
- 52.Tsai CH, Huang JH, Hwang BF, Lee YL. Household environmental tobacco smoke and risks of asthma, wheeze and bronchitic symptoms among children in Taiwan. Respir Res. 2010;11:11. doi: 10.1186/1465-9921-11-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hwang BF, Lee YL. Air pollution and prevalence of bronchitic symptoms among children in Taiwan. Chest. 2010;138:956–964. doi: 10.1378/chest.09-2600. [DOI] [PubMed] [Google Scholar]
- 54.Tung KY, Tsai CH, Lee YL. Microsomal Epoxide Hydroxylase Genotypes/Diplotypes, Traffic Air Pollution and Childhood Asthma. Chest. 2010 doi: 10.1378/chest.10-2479. [DOI] [PubMed] [Google Scholar]
- 55.Islam T, Gauderman WJ, Berhane K, McConnell R, Avol E, et al. Relationship between air pollution, lung function and asthma in adolescents. Thorax. 2007;62:957–963. doi: 10.1136/thx.2007.078964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wang WH, Hwang BF, Chen JM, Wu YF, Lee YL. Pulmonary Function, Traffic-related Air Pollution and Incident Bronchitis among Children. in Press. (Submitted)
- 57.Hahn LW, Ritchie MD, Moore JH. Multifactor dimensionality reduction software for detecting gene-gene and gene-environment interactions. Bioinformatics. 2003;19:376–382. doi: 10.1093/bioinformatics/btf869. [DOI] [PubMed] [Google Scholar]
- 58.Ritchie MD, Hahn LW, Moore JH. Power of multifactor dimensionality reduction for detecting gene-gene interactions in the presence of genotyping error, missing data, phenocopy, and genetic heterogeneity. Genet Epidemiol. 2003;24:150–157. doi: 10.1002/gepi.10218. [DOI] [PubMed] [Google Scholar]
- 59.Greene CS, Himmelstein DS, Nelson HH, Kelsey KT, Williams SM, et al. Enabling personal genomics with an explicit test of epistasis. Pac Symp Biocomput. 2010:327–336. doi: 10.1142/9789814295291_0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Moore JH. Detecting, characterizing, and interpreting nonlinear gene-gene interactions using multifactor dimensionality reduction. Adv Genet. 2010;72:101–116. doi: 10.1016/B978-0-12-380862-2.00005-9. [DOI] [PubMed] [Google Scholar]