Abstract
Background
Sleep disturbance is common in carpal tunnel syndrome (CTS), and we hypothesize that it has an important impact on the quality of life of CTS patients. The characteristic of sleep problems associated with CTS has not been evaluated.
Methods
We performed a case–control study to measure the association between a variety of sleep disturbances and CTS. Sixty-two cases with clinically diagnosed CTS and a probable or classic hand diagram were compared to 138 primary care patients without CTS. In addition to demographic features, we collected the nature of sleep disturbance experienced by the patients from a categorical list and the nature, impact, and severity of sleep disturbance using the Insomnia Severity Index.
Results
Patients with CTS complained of significantly more severe problems with sleep than the control population and had multiple sleep complaints compared to the control group. Sixty-three of the 138 control patients indicated that they had one cause of sleeping disturbance with no control patient choosing more than one. In contrast, in CTS patients, 44 of 63 patients indicated they had two or more causes of sleep disturbance. The Insomnia Severity Index was significantly higher in CTS patients and the impact of sleep disturbance on quality of life was higher in the cases.
Conclusion
Sleep disturbance in CTS patients is characterized by a broad array of physical symptoms that have a significant impact on quality of life.
Keywords: Carpal tunnel syndrome, Sleep disturbance, Insomnia, Case–control study
Introduction
Night waking with pain and numbness has long been reported as a common symptom associated with carpal tunnel syndrome [3, 7, 8]. It has been noted that about 80% of carpal tunnel patients have night time waking due to numbness of the hands. Graham et al. have reported that night time numbness is a key characteristic of carpal tunnel syndrome [2] and relief of night time symptoms is one of the sought after outcomes of treatment. We initially became interested in the night time symptoms of carpal tunnel syndrome because we thought they may provide an opportunity to understand and investigate evidence of causation. In the course of our research, we have measured some of the characteristics of the sleep disturbances associated with carpal tunnel syndrome and proposed a theory of causation [4–6]. In spite of the ubiquity of night time symptoms in carpal tunnel syndrome, there has been little elucidation of these characteristics beyond the observation of the frequency of numbness and pain that wake the patient. The purpose of this paper is to report our findings on the characteristics of the sleep disturbances that are associated with carpal tunnel syndrome.
Method
We performed a case–control study with patients from a large urban primary care practice. The study was reviewed and received approval from the university IRB. Our general research strategy was to use a control population, selected from a previous cross-sectional survey, to measure the underlying prevalence of sleeping problems of interest [6]. These primary care patients are from the same study base from which the cases are selected. Details of the case–control method have been reported in detail [4].
Briefly, the cases of CTS were patients referred to an urban hand surgery specialty office with a chief complaint of numbness or tingling of the hands. Cases were identified by their chief complaint and through the history and physical examination performed by the hand surgeon. Controls were chosen from a recent survey population as noted above. Patients from the survey population were included as controls if they had no history of waking at night due to numbness of the hand.
All cases and controls completed a data collection form requesting age, gender, height, weight, and preferred sleep position. Patients indicated if they worked by shift, if they had diabetes, their smoking history, and severity of back or neck pain. Pertinent to this report, we asked patients if they had problems with sleep and the cause of those problems. Patients were asked to indicate from a list one or more problems they experienced with sleeping. The list included “mind is too active”, “need to use bathroom”, “back or neck pain”, “painful joints”, “numbness of hands”, “leg cramps”, and “other”. Patients also completed a short insomnia instrument, the Insomnia Severity Index [1]. All data were collected and entered into Excel and transferred to PASW 18 for analysis.
Results
Cases. Data were collected from 68 consecutive cases of CTS. This included three patients classified by the hand diagram as “unlikely” and two as “possible” who were excluded from the analysis. One patient did not complete the diagram. Twenty-six cases were classified as “probable” and 36 as “classic” by the diagram yielding 62 cases of CTS, 16 men (mean age 51.1, SD 15.6) and 46 women (mean age 54.1, SD 12.0) for the analysis. Controls. One hundred and thirty-eight primary care patients from the survey population, 103 women (mean age 45.1, SD 18.1) and 35 men (mean age 43.7, SD 14.1), were included as the control population.
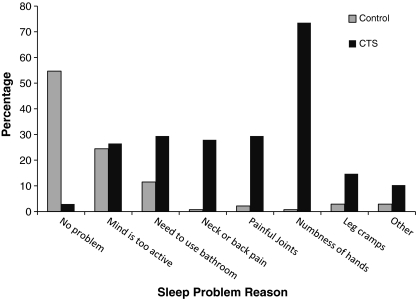
The patients with CTS reported more problems with sleep than the control population. This included not only numbness of the hands but also each of the other specific problems identified (Fig. 1).
Fig. 1.
Cause of sleep disturbance in cases and controls. Patients with CTS are characterized by a large number of problems that cause waking at night
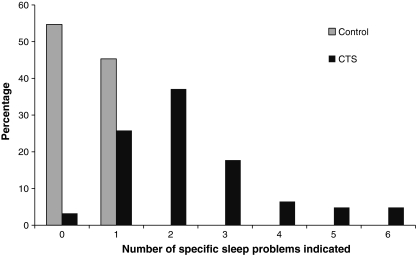
For example, 3 of 138 control patients complained of painful joints causing disturbance with sleep compared to 20 of 62 CTS patients. The CTS patients were also characterized by multiple sleep problems compared to the control group (Fig. 2). Sixty-three of the 138 control patients endorsed one sleeping problem and no control patient endorsed more than one problem. In the CTS patients, all except two patients endorsed at least one problem (“numbness of hands” was one option). Sixteen patients endorsed one option and 44 patients endorsed two or more problems with sleeping.
Fig. 2.
Number of problems indicated by the participants that disrupt sleep in CTS patients and control patients. Patients with CTS indicate more physical complaints listed in Fig. 1 that interfere with sleep than controls
The Insomnia Severity Index is significantly higher in patients with CTS compared to those without. Of the three items characterizing the sleep symptom, “difficulty of staying asleep” was significantly different in the patients with CTS compared to the controls (p < .001). The impact of the sleep disturbance symptoms representing a cause for worry and causing an impairment of quality of life was significantly higher in the CTS patients than in the control group (p < .001). Dissatisfaction with sleep (p < .001) and sleep disturbance that interfered with daily functioning (p = .016) were also significant. There was a significant correlation between all items of the Insomnia Severity Index.
Discussion
We found significant differences in sleep disturbance in the cases and controls. In addition to the expected increase in complaints of numbness at night, the patients with CTS reported greater experience with a wide range of sleep difficulties, and individual patients with CTS were characterized by having multiple sleeping complaints compared to those without CTS. For example, the item “back or neck pain” was endorsed as a cause of sleeping problems by 1 of the 139 (0.7%) patients in the control population and 19 of 62 (30.6%) carpal tunnel patients. In addition, those patients with CTS endorsed more than one sleep problem to a greater extent than non-CTS patients. In our study, these increased night time problems were not associated with age.
The insomnia score for CTS patients was significantly higher than for the control population. When the items were reviewed individually, “difficulty of staying asleep” was significantly higher in patients with CTS. The subscales that score the impact of the symptoms on the patients’ life were all significantly higher in the CTS patients.
In our general evaluation of sleep disturbance and CTS, we found a remarkable similarity in the age and gender distribution of insomnia and the presentation of CTS [5]. We have found that CTS patients have sleep disturbances and insomnia scores greater than those patients without CTS. Since the prevalence of CTS is much less than insomnia, we believe that the etiologic fraction of insomnia attributable to CTS is low. Although night time CTS symptoms might cause insomnia in some patients, insomnia could make people more sensitive to a wide array of night time symptoms, and sleep disturbance may lower the threshold for presentation to the doctor with numbness and tingling that is brought on at night. Insomnia and other sleep disturbances could also influence sleep position, resulting in wrist deviation and causing CTS.
Whether the sleep disturbance is related to the CTS or not, this study shows that patients with CTS have significant problems with a wide variety of sleep disturbances. We are interested if consideration of sleep disturbance in CTS patients is a useful avenue of inquiry and important for patient management or an interesting co-morbidity that has no impact on the care of the nerve compression.
References
- 1.Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/S1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 2.Graham B, Regehr G, Naglie G, Wright JG. Development and validation of diagnostic criteria for carpal tunnel syndrome. J Hand Surg Am. 2006;31(6):919–924. [PubMed] [Google Scholar]
- 3.Katz JN, Larson MG, Sabra A, Krarup C, Stirrat CR, Sethi R, et al. The carpal tunnel syndrome: diagnostic utility of the history and physical examination findings. Ann Intern Med. 1990;112:321–327. doi: 10.7326/0003-4819-112-5-321. [DOI] [PubMed] [Google Scholar]
- 4.McCabe SJ, Gupta A, Tate DE, Myers J. Preferred sleep position on the side is associated with carpal tunnel syndrome. Hand. 2011;6(2):132–7. doi: 10.1007/s11552-010-9308-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McCabe SJ, Uebele AL, Pihur V, Rosales R, Atroshi I. Epidemiologic associations of carpal tunnel syndrome and sleep position: is there a case for causation? Hand. 2007;2:127–134. doi: 10.1007/s11552-007-9035-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McCabe SJ, Xue Y. Evaluation of sleep position as a potential cause of carpal tunnel syndrome: preferred sleep position on the side is associated with age and gender. Hand. 2010;5:361–363. doi: 10.1007/s11552-010-9271-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wainner RS, Fritz JM, Irrgang JJ, Delitto A, Allison S, Boninger ML. Development of a clinical prediction rule for the diagnosis of carpal tunnel syndrome. Arch Phys Med Rehabil. 2005;86:609–618. doi: 10.1016/j.apmr.2004.11.008. [DOI] [PubMed] [Google Scholar]
- 8.Zohn DA, Hughes AC, Haase KH. Carpal tunnel syndrome—a review. Arch Phys Med Rehabil. 1962;43:420–425. [Google Scholar]