Introduction
Primary synovial chondromatosis consists of cartilaginous metaplasia of the synovium, which leads to the production of intra-articular and periarticular osteocartilaginous bodies [8, 12, 18, 19]. The nomenclature has evolved with time to include chondromatosis of the joint capsule, diffuse enchondroma of the joint capsule, joint chondroma, synovial osteochondromatosis, and synovial chondromatosis [8, 9, 16, 18, 20]. Primary synovial chondromatosis most commonly occurs in young and middle-aged adults and is rarely found in children (youngest patient reported was 14 years old) [12, 19]. The entity usually involves the synovium of large joints (knee, hip, elbow, and shoulder) [3, 8, 15, 16, 18, 19, 26] but has been reported in the hand [2, 10–12, 20, 26]. To our knowledge, only two cases have been reported in the interphalangeal joint of the thumb [13, 14]. We report on a 13-year-old female with primary synovial chondromatosis of the inter-phalangeal (IP) joint of her thumb.
Case Report
A 13-year-old right-hand dominant female presented with a 3-year history of pain and progressive swelling over the dorsum of her right thumb. She was initially seen by an adult hand surgeon for this mass, and because of her lack of symptoms at that time, she was observed. She gave no history of trauma and no other relevant medical history. On examination, several masses were located both on the dorsal and volar aspects of the thumb IP joint. The masses were focally tender and had a firm and nodular consistency. Range of motion was almost normal at the joint.
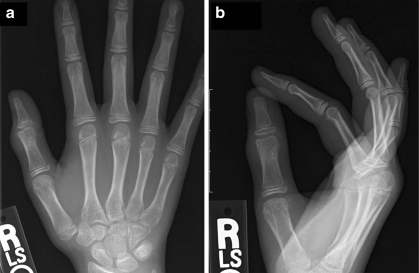
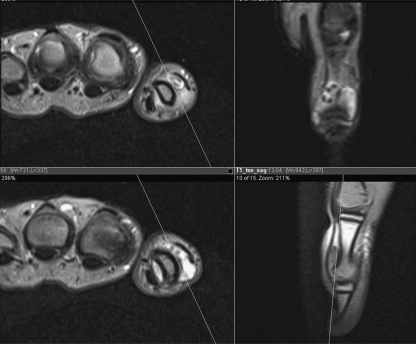
Radiographs of the hand at age 10 years showed mild soft tissue swelling with ossific densities adjacent to the distal aspect of the thumb proximal phalanx but no significant underlying bony erosion (Fig. 1). An MRI was obtained of the right hand which suggested intra-capsular involvement and likely benign entity (Fig. 2). Three years later, the radiographs revealed increased ossification of the densities (Fig. 3).
Fig. 1.
a Anteroposterior (AP) and b lateral radiographs of a 10-year-old female with mild soft tissue swelling and ossific density adjacent to the distal aspect of the thumb proximal phalanx
Fig. 2.
Magnetic resonance imaging of right thumb suggests intra-capsular involvement and loose bodies in the interphalangeal joint
Fig. 3.
AP and lateral radiographs of the same patient at 13 years of age with increased ossification of densities around the thumb proximal phalanx
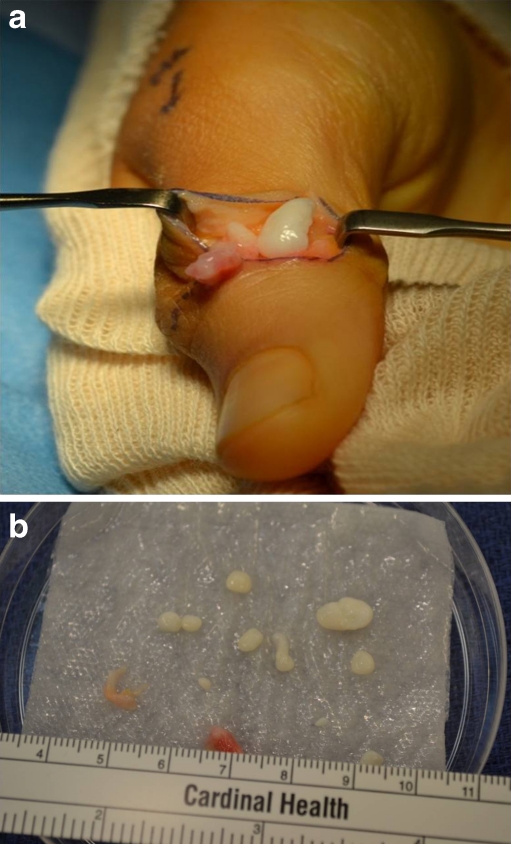
Because the patient had worsening pain and increase in the size of the masses, she underwent joint exploration and synovial biopsy. An “L-type” incision was used on the dorso-radial border of the thumb (Fig. 4). This allowed access to both dorsal and palmar aspects of the IP joint. Multiple firm, smooth, white nodules were found within a fibrous sac arising from the IP joint (Fig. 5). The synovium and loose bodies were excised and sent to pathology.
Fig. 4.

“L-type” incision on the dorso-radial border of the right thumb
Fig. 5.
a Smooth white nodule within a fibrous sac arising from the thumb interphalangeal joint. b Gross specimens retrieved from joint
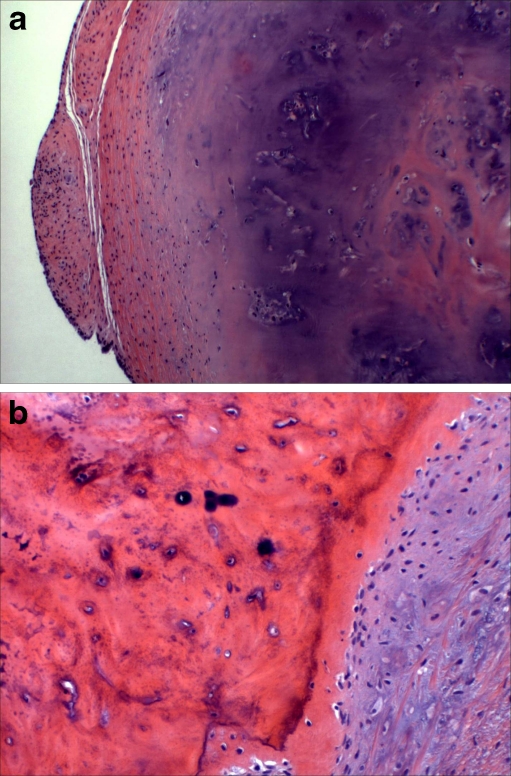
Histologic studies revealed well-circumscribed nodules of cartilage and bone. Several of the fragments were surfaced by a thin layer of synovium. The cartilage was of low-to-moderate cellularity and had unremarkable chondrocytes lying individually within the lacunae, indicative of primary synovial chondromatosis (Fig. 6).
Fig. 6.
a Nodule of cartilage surfaced by a thin layer of synovium (hematoxylin and eosin, original magnification × 100). b Region of ossification within cartilaginous nodule (hematoxylin and eosin, original magnification × 200)
Physical therapy for range of motion was initiated 3 weeks after surgery. Three months after surgery, she had painless range of motion with full extension, but lacking 10° of full flexion. No recurrence was noted at 6 months post surgery.
Discussion
Primary synovial chondromatosis is an uncommon condition characterized by benign metaplasia of synovial tissue into cartilaginous tissue [2, 8, 10, 18, 20]. The exact etiology of synovial chondromatosis remains unclear, but this primary form can originate from synovium or tenosynovium [4, 18, 20]. The tenosynovial form may be caused by trauma, in contrast to “intra-articular” chondromatosis, which has no such association [8, 12, 22].
These two entities are distinct from the more common secondary synovial chondromatosis, which occurs with the implantation of cartilage fragments into the tissue as a result of degenerative disease (osteoarthritis), neuropathic arthropathy, or trauma [1, 20, 26].
Males are affected more than females, commonly ranging in age from the third to fifth decade of life [3, 12, 13, 18]. Typically large joints are involved with the knee being the most common, followed by the hip and elbow [3, 8, 15, 16, 18, 19, 26]. This disease has been documented in the joints of the hand, specifically the metacarpophalangeal joint [2, 7, 11, 20, 22, 23, 26] and interphalangeal joint [6, 10, 12–14, 25]. Only two of these cases involved the thumb interphalangeal joint [13, 14]. When synovial chondromatosis occurs in the smaller joints, it has a predilection towards young women in contrast to that of the larger joints [12, 14].
The articular form of primary synovial chondromatosis can slowly progress, and patients will have symptoms present for months to years [8, 12]. Common presenting complaints include pain, swelling, and restriction of motion. Milgram described three separate phases: (1) active intrasynovial disease with no free loose bodies; (2) transitional lesions with osteochondral nodules in the synovial membrane and osteochondral bodies lying free within the joint cavity; and (3) multiple free osteochondral bodies, with now quiescent intrasynovial disease [16]. This patient likely had an initial presentation in the early phase (soft tissue swelling but no pain), and her symptoms worsened as she progressed to the transitional phase. The natural history of this condition is not well known. Milgram has described cases where some of the nodules have been resorbed spontaneously and not extruded into the joint [16]. However, if extra-capsular chondromatous lesions are present, then the lesions seem to behave more like a neoplasm versus a reactive process and surgical intervention is recommended.
Malignant transformation of this disease into synovial chondrosarcoma is exceedingly rare [8, 12, 15, 18], but Davis et al. have reported a risk of malignant change of 5% (3 of 53 patients) [3]. As with other case reports on malignant transformation, all of these cases were in large joints [3, 5, 17, 21, 24]. To our knowledge, no cases of malignant transformation have been seen in the finger joints.
Controversy remains regarding the extent of surgical treatment for primary synovial chondromatosis. The debate centers on preventing recurrence of the disease. Murphy et al. advocated removal of loose bodies with synovectomy. They stated that the synovium “nourishes” the loose bodies which can remain viable and increase in size [18]. In contrast, Jeffreys recommended removal of loose bodies alone, with no recurrences reported [8]. The recurrence rate has been reported as high as 15%; however, most of these cases involved large joints [3, 15]
Three cases of recurrence have been reported in the hand (two interphalangeal joints and one metacarpophalangeal joint) [6, 11, 12]. Other authors recommend that synovectomy should be done only if pain and swelling are the main symptoms. If mechanical symptoms predominate, then removal of loose bodies alone may be sufficient [12, 15]. Since recurrence has been noted even after synovectomy (4 years later) [6, 12], we recommend that patients be counseled in this regard and offered periodic follow-ups to detect for recurrence.
Acknowledgments
Conflicts of Interest No pharmaceutical, industry, or outside support was used for this study. The authors report no conflicts of interest. No funding was received for this work from any of the following organizations: NIH, Wellcome Trust, Howard Hughes Medical Institute, and others.
References
- 1.Bui-Mansfield LT, Rohini D, Bagg M. Tenosynovial chondromatosis of the ring finger. Am J Roentgenol. 2005;184:1223–4. doi: 10.2214/ajr.184.4.01841223. [DOI] [PubMed] [Google Scholar]
- 2.Cremone JC, Wolff TW, Wolfort FG. Synovial chondromatosis of the hand. Plast Reconstr Surg. 1982;69:871–874. doi: 10.1097/00006534-198205000-00030. [DOI] [PubMed] [Google Scholar]
- 3.Davis RI, Hamilton A, Biggart JD. Primary synovial chondromatosis. A clinico-pathologic review and assessment of malignant potential. Human Pathol. 1998;29:683–688. doi: 10.1016/S0046-8177(98)90276-3. [DOI] [PubMed] [Google Scholar]
- 4.Debenedetti MJ, Schwinn CP. Tenosynovial chondromatosis in the hand. J Bone Joint Surg. 1979;61A:898–903. [PubMed] [Google Scholar]
- 5.Hamilton A, Davis RI, Nixon JR. Synovial chondrosarcoma complicating synovial chondromatosis. Report of a case and review of the literature. J Bone Joint Surg. 1987;69A:1084–1088. [PubMed] [Google Scholar]
- 6.Harvey FJ, Negrine J. Synovial chondromatosis in the distal interphalangeal joint. J Hand Surgery. 1990;15A:102–105. doi: 10.1016/S0363-5023(09)91115-7. [DOI] [PubMed] [Google Scholar]
- 7.Hettiaratchy SP, Nanchahal J. Synovial chondromatosis of the metacarpophalangeal joint. J Hand Surgery. 2002;27B(1):104–106. doi: 10.1054/jhsb.2001.0677. [DOI] [PubMed] [Google Scholar]
- 8.Jeffreys TE. Synovial chondromatosis. J Bone Joint Surg Br. 1967;49B:530–534. [PubMed] [Google Scholar]
- 9.Jones HT. Loose body formation in synovial osteochondromatosis with special reference to the etiology and pathology. J Bone Joint Surg. 1924;6A:407–458. [Google Scholar]
- 10.Kettelkamp DB, Dolan J. Synovial chondromatosis of an interphalangeal joint of a finger. Report of a case. J Bone Joint Surg. 1966;48A:329–332. [PubMed] [Google Scholar]
- 11.Kriegs-Au G, Muller D. Recurrent chondromatosis of the metacarpophalangeal joint of the thumb—differential diagnosis and therapy [German] Handchir Mikrochir Plast Chir. 2004;36:323–327. doi: 10.1055/s-2004-821283. [DOI] [PubMed] [Google Scholar]
- 12.Kumar A, Thomas AP. Recurrent synovial chondromatosis of the index finger—case report and literature review. Hand Surgery. 2000;5:181–183. doi: 10.1142/S0218810400000259. [DOI] [PubMed] [Google Scholar]
- 13.Lewis MM, Marshall JL, Mirra JM. Synovial chondromatosis of the thumb. A case report and review of the literature. J Bone Joint Surg. 1974;56A:180–183. [PubMed] [Google Scholar]
- 14.Malhotra R, Gaur S, Dave PK, et al. Synovial chondromatosis of the interphalangeal joint of the thumb: a case report. J Hand Surg. 1994;19A:460–461. doi: 10.1016/0363-5023(94)90063-9. [DOI] [PubMed] [Google Scholar]
- 15.Maurice H, Crone M, Watt I. Synovial chondromatosis. J Bone Joint Surg. 1988;70B:807–811. doi: 10.1302/0301-620X.70B5.3192585. [DOI] [PubMed] [Google Scholar]
- 16.Milgram JW. Synovial osteochondromatosis a histopathological study of thirty cases. J Bone Joint Surg Am. 1977;59A:792–801. [PubMed] [Google Scholar]
- 17.Mullins F, Berard CW, Eisenberg SH. Chondrosarcoma following synovial chondromatosis. A case study. Cancer. 1965;18:1180–1188. doi: 10.1002/1097-0142(196509)18:9<1180::aid-cncr2820180918>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 18.Murphy FP, Dahlin DC, Sullivan CR. Articular synovial chondromatosis. J Bone Joint Surg Am. 1962;44A:77–86. [Google Scholar]
- 19.Nashi M, Manjunath B, Banerjee B, et al. Synovial chondromatosis in a child: an unusual cause of shoulder pain case report. J Shoulder Elbow Surg. 1998;7:642–643. doi: 10.1016/S1058-2746(98)90015-5. [DOI] [PubMed] [Google Scholar]
- 20.Ozcelik IB, Kuvat SV, Mersa B, et al. Synovial chondromatosis of the metacarpophalangeal joint of the ring finger. Acta Orthop Traumatol Turc. 2010;44(4):337–339. doi: 10.3944/AOTT.2010.2324. [DOI] [PubMed] [Google Scholar]
- 21.Perry BE, McQueen DA, Lin JJ. Synovial chondromatosis with malignant degeneration to chondrosarcoma. J Bone Joint Surg Am. 1988;70A:1259–1261. [PubMed] [Google Scholar]
- 22.Reed SC, Wright CS. Synovial chondromatosis of the metacarpophalangeal joint. Case report and review of the literature. Canadian J Surg. 1996;39:407–409. [PMC free article] [PubMed] [Google Scholar]
- 23.Szepesi J. Synovial chondromatosis of the metacarpophalangeal joint. Acta Orthop Scand. 1975;46:926–930. doi: 10.3109/17453677508989280. [DOI] [PubMed] [Google Scholar]
- 24.Taconis WK, Heul RO, Taminiau AMM. Synovial chondrosarcoma. Report of a case and review of the literature. Skeletal Radiol. 1997;26:682–685. doi: 10.1007/s002560050312. [DOI] [PubMed] [Google Scholar]
- 25.Takami H, Takahashi S, Ando M. Synovial chondromatosis of the proximal interphalangeal joint of a finger. J hand Surg. 1994;19A:794–796. doi: 10.1016/0363-5023(94)90185-6. [DOI] [PubMed] [Google Scholar]
- 26.Warme BA, Tigrani DY, Ward CM. Metacarpophalangeal joint synovial osteochondromatosis: a case report. The Iowa Orthopaedic Journal. 2000;28:91–93. [PMC free article] [PubMed] [Google Scholar]