Abstract
A 48-year-old woman with a history of chronic migraines, initially admitted for inpatient management of intractable migraine headaches, developed new onset abdominal pain, hypotension, and diarrhea on hospital day number ten. In our institution's headache unit, patients are treated by a multidisciplinary approach, including individualized drug therapy based on diagnosis and previous response to therapy. Given the patient's hypotension and clinical appearance, she was transferred to the intensive care unit and treated for septic shock and metabolic acidosis. A bedside colonscopy revealed diffuse ischemic colitis. Final pathology after colon resection showed widespread, transmural necrosis of the colonic wall. We review the pathophysiology of ergotamine use and its potential association with ischemic colitis.
Key Words: Ergotamine, Dihydroergotamine mesylate, Ischemic colitis, Vasospasm
Introduction
The use of ergotamines causing ischemia of peripheral vessels has been reported, particularly in patients with peripheral vascular disease. Ischemic bowel induced by ergotamines is a much rarer event, with few documented cases in the literature. While colitis is always on the differential diagnosis of hospital patients with abdominal pain, the majority of cases are secondary to infectious colitis associated with antibiotic therapy. When suspected, non-occlusive mesenteric ischemia can be treated with anti-coagulation and blood pressure support with intravenous fluids. The predisposition for ischemia in patients with chronic constipation secondary to opioid use is amplified by concomitant use of vasoactive medications to control symptoms of migraine headache. While abdominal CT scanning is frequently used to assess colonic pathology, findings often lag behind those identified at the time of colonoscopy. Patchy areas of ischemia are often managed non-surgically by discontinuing the offending medication. Widespread necrosis, coupled with clinical deterioration, as in this case, mandated immediate surgical intervention to prevent irreversible septic shock.
Case Report
A 48-year-old woman with a long-standing history of intractable migraine headaches was admitted to our institution's specialty headache unit for aggressive management. She had no known history of peripheral vascular or cardiac disease but has been admitted multiple times for treatment of her headaches since her initial diagnosis in 2003. During the course of each of these hospitalizations, she had received one to two courses of dihydroergotamine mesylate (DHE) 45. During this admission she received two courses of DHE 0.5 mg × 1, then 1 mg every 8 h for a total of eight doses, on days 1–3 and the second course of therapy on days 7–9. Several hours after the final dose of her second round she became obtunded, minimally responsive and hypotensive with a blood pressure of 80/45 mm Hg. On physical examination her abdomen was moderately distended with few bowel sounds. Her lactate acid level was 4.5 mmol/l, white blood cell count was 18.0 (with 17% bands), and stool was Clostridium difficile negative.
The patient was transferred to the intensive care unit, given intravenous fluid boluses, started on vasopressors, and given broad spectrum antibiotics. She eventually required intubation. Her chest radiograph was unremarkable, and her abdominal x-rays showed only mild prominence of the colon. Over the next several hours she became progressively acidotic with a worsening bandemia. A bedside colonoscopy showed diffuse ischemic colitis with fecal impaction and no pseudomembranes (fig. 1). The patient was taken to the operating room and underwent a laparotomy. Operative findings showed a peritoneal cavity filled with murky, foul-smelling fluid and gangrene of the descending colon was seen with necrosis in the area immediately distal to the splenic flexure to the sigmoid colon. A large amount of impacted stool was present in the left colon. The vasculature of this area of colon was intact with audible Doppler signals. Upon removal of the gangrenous bowel the patient's condition improved promptly.
Fig. 1.
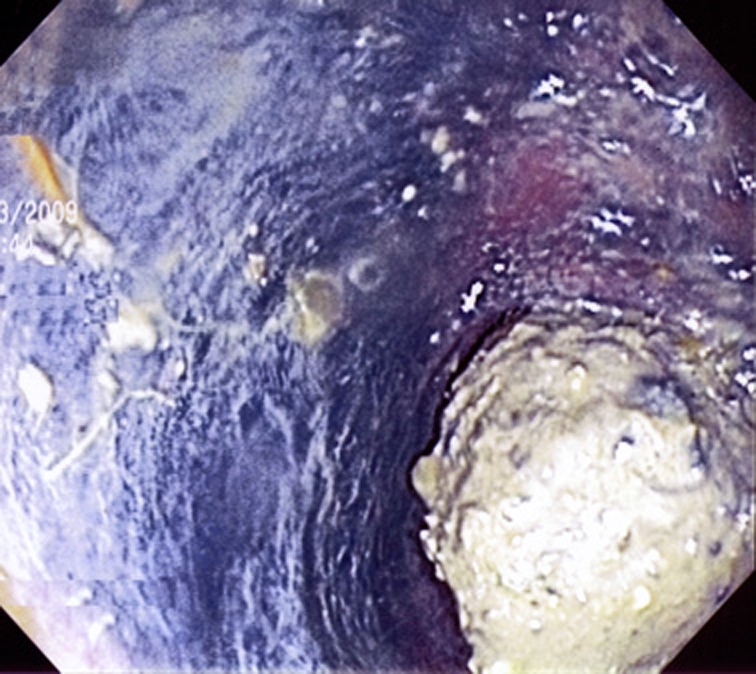
Bedside colonoscopy showing diffuse ischemic colitis with fecal impaction and no pseudomembranes.
Final pathology on the surgical specimen showed 86 cm of patchy, dark green/black large bowel, consistent with ischemic necrosis. The bowel wall was intact throughout. The final diagnosis was gangrenous large bowel, ischemic colitis with thrombi or emboli noted. A hypercoaguable panel was performed following the operation and the patient was negative for clotting disorders.
Discussion
The differential diagnosis of ischemic colitis includes arterial occlusion, caused by emboli or thrombus, venous thrombosis, and non-occlusive ischemia caused by systemic hypotension or, as is strongly suspected in this case, ergotamine-induced vasospasm. A diagnosis of ergotamine-induced vasospasm is a diagnosis of exclusion, made when all other etiologies of ischemia have been ruled out. In this case, an arterial occlusion is unlikely, because there was no palpable thrombus and there was no clear ischemic demarcation to suggest a major vessel distribution. The patient had no history of cardiac arrhythmias, such as atrial fibrillation, to predispose her to emboli. Furthermore she was a non-smoker and had no other cardiac risk factors such as atherosclerosis or hyperlipidemia. She reported no history of post-prandial pain or food fear. Emboli to inferior mesenteric artery (IMA) are exceedingly rare, and there are no reported cases of spontaneous emboli or thrombosis to IMA. All reported cases of IMA thrombosis are subsequent to trauma [1, 2].
Venous thrombosis as a cause of ischemia in this patient is equally unlikely as there were no signs of venous congestion or stasis at the time of surgery. The patient had no hypercoagulable disorder and on examination the colon was not edematous and no clot was identified in the vasculature. Ischemia secondary to systemic hypotension alone would have resulted in a watershed-type distribution of gangrene. In this case the watershed areas were preserved and the segment between the watershed areas was necrotic. The most probable cause of this event was non-occlusive mesenteric ischemia in the IMA distribution and more specifically the left colic artery due to intense vasoconstriction induced by high-dose ergotamine use. Underlying bowel wall distention from the impacted stool in combination with vasoconstriction from ergotamine is the most likely etiology for this patient's bowel ischemia.
DHE is indicated for the acute treatment of migraine headaches with or without aura and the acute treatment of cluster headache episodes [3]. Its therapeutic activity in the treatment of migraine headaches is generally attributed to the agonist effect at 5-HT1D receptors. According to the neurovascular theory of migraine, it is hypothesized that activation of 5-HT1D receptors on intracranial blood vessels leads to vasoconstriction. The 5-HT1D receptors on sensory nerve endings of the trigeminal are also activated, causing inhibition of pro-inflammatory neuropeptide release. The combination of these two effects leads to relief of migraine headache. Ergotamine and DHE cause vasoconstriction of both arteries and veins due to alpha-adrenergic agonistic action, and they may also have possible interaction with prostaglandins, calcium and serotonin. DHE was developed in 1943 for migraine prophylaxis and shown in four studies in 1987 and five studies in 2001 to have less effect on peripheral arteries than ergotamine. As indicated in this case, however, DHE still carries some risk. A European consensus report in 2000 concluded that ergotamine is not a drug of first choice in the triptan era, but may be useful in longstanding migraine attacks with multiple recurrences [4].
Ergotamine is known to cause peripheral ischemia, as has been reported in several case studies, most commonly in the lower limbs [5, 6, 7, 8, 9]. Incidents of myocardial infarction [10] and stroke [11] have also been reported. A causal relationship has not however been clearly established and is still the subject of some debate [12]. Other reports of ergotamine causing ischemic bowel appear in the literature [13, 14, 15]. In previous reported cases of colitis, expectant management with bowel rest was successful. This is the first reported cases of ischemia progressing to gangrene such that colon resection was required. It should be noted in this case that the patient's dose of DHE was greater than the recommended amount. The recommended dosing of DHE 45 is 1 mg IV/IM/SC, repeated once every 24 h for a total dose not to exceed 6 mg in 7 days. In this case, the patient received 17 mg of DHE over the course of 9 days. Although ischemic colitis is considered a rare side effect of high-dose ergotamine use, it is a very real risk of which clinicians need to remain aware.
Conclusion
This is the fourth reported case of ischemic colitis secondary to high-dose ergotamine use reported in the literature and the first to require colon resection. While DHE can be useful in patients with refractory migraines, patients should be informed of the risks of both peripheral and visceral ischemia before deciding on this treatment. Finally, ischemic colitis should be considered in the differential diagnosis of all patients taking ergotamines who present with abdominal pain.
Footnotes
The authors have no conflicts of interest to disclose.
This is an Open Access article licensed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs 3.0 License (www.karger.com/OA-license), applicable to the online version of the article only. Distribution for non-commercial purposes only.
References
- 1.Huggard T, Herstein A. Thrombosis of the inferior mesenteric artery. Can Med Assoc J. 1950;62:502–503. [PMC free article] [PubMed] [Google Scholar]
- 2.Koh KS, Danzinger RG. Massive intestinal infarction in young women: complication of use of oral contraceptives? Can Med Assoc J. 1977;116:513–515. [PMC free article] [PubMed] [Google Scholar]
- 3.Tfelt-Hansen PC, Koehler PJ. History of the use of ergotamine and dihydroergotamine in migraine 1906 and onward. Cephalalgia. 2008;28:877–886. doi: 10.1111/j.1468-2982.2008.01578.x. [DOI] [PubMed] [Google Scholar]
- 4.Tfelt-Hansen P, Saxena PR, Dahlof C, Pascual J, Lainez M, Henry P, Diener H, Schoenen J, Ferrari MD. Ergotamine in the acute treatment of migraine: a review and European consensus. Brain. 2000;123(part 1):9–18. doi: 10.1093/brain/123.1.9. [DOI] [PubMed] [Google Scholar]
- 5.Fischbach R, Gross-Fengels W, Schmidt R. Ergotism: an occasional unrecognized cause of acute ischemia of the extremities (in German) Rontgenblatter. 1990;43:213–219. [PubMed] [Google Scholar]
- 6.McKiernan TL, Bock K, Leya F, Grassman E, Lewis B, Johnson SA, Scanlon PJ. Ergot induced peripheral vascular insufficiency, non-interventional treatment. Cathet Cardiovasc Diagn. 1994;31:211–214. doi: 10.1002/ccd.1810310310. [DOI] [PubMed] [Google Scholar]
- 7.Zavaleta EG, Fernandez BB, Grove MK, Kaye MD. St Anthony's fire (ergotamine induced leg ischemia) – a case report and review of the literature. Angiology. 2001;52:349–356. doi: 10.1177/000331970105200509. [DOI] [PubMed] [Google Scholar]
- 8.Halloul Z, Meyer F, Lippert H, Buerger T. Ergotamine-induced acute vascular insufficiency of the lower limb – a case report. Angiology. 2001;52:217–221. doi: 10.1177/000331970105200310. [DOI] [PubMed] [Google Scholar]
- 9.Demir S, Akin S, Tercan F, Aribogan A, Oguzkurt L. Ergotamine-induced lower extremity arterial vasospasm presenting as acute limb ischemia. Diagn Interv Radiol. 2010;16:165–167. doi: 10.4261/1305-3825.DIR.1931-08.2. [DOI] [PubMed] [Google Scholar]
- 10.de Labriolle A, Genee O, Heggs LM, Fauchier L. Acute myocardial infarction following oral methyl-ergotamine intake. Cardiovasc Toxicol. 2009;9:46–48. doi: 10.1007/s12012-009-9031-9. [DOI] [PubMed] [Google Scholar]
- 11.Pezzini A, Del Zotto E, Giossi A, Volonghi I, Grassi M, Padovani A. The migraine-ischemia stroke connection: potential pathogenic mechanisms. Curr Mol Med. 2009;9:215–226. doi: 10.2174/156652409787581583. [DOI] [PubMed] [Google Scholar]
- 12.Velentgas P, Cole JA, Mo J, Sikes CR, Walker AM. Severe vascular events in migraine patients. Headache. 2004;44:642–651. doi: 10.1111/j.1526-4610.2004.04122.x. [DOI] [PubMed] [Google Scholar]
- 13.Rogers DA, Mansberger JA. Gastrointestinal vascular ischemia caused by ergotamine. South Med J. 1989;82:1058–1059. doi: 10.1097/00007611-198908000-00034. [DOI] [PubMed] [Google Scholar]
- 14.Rutgeerts L, Ghillebert G, Drognee W, Tanghe W, Vuylsteke P, Decoster M. Ischemic colitis in a patient with Crohn's disease taking an oral contraceptive and an ergotamine alkaloid. Acta Clin Belg. 1993;48:48–51. doi: 10.1080/17843286.1993.11718284. [DOI] [PubMed] [Google Scholar]
- 15.Stillman AE, Weinberg M, Mast WC, Palpant S. Ischemic bowel disease attributable to ergot. Gastroenterology. 1977;72:1336–1337. [PubMed] [Google Scholar]


