Abstract
Introduction
SWL and URS are highly effective treatments for urinary lithiasis. While stone size and location are primary determinants of therapy, little is known about other factors associated with treatment. Our objective was to identify patient, provider and practice setting characteristics associated with selection of ureteroscopy or SWL.
Methods
We used the Medicare 5% sample to identify beneficiaries with an incident stone encounter from 1997 –2007. Within this group, we identified beneficiaries undergoing SWL or URS for the management of urinary calculi. Multivariable regression models identified factors associated with use of URS.
Results
The cohort comprised 9358 beneficiaries who underwent an initial procedure. SWL was used in 5208 (56%) beneficiaries, while URS was used in 4150 (44%). Females were less likely than males to undergo URS (OR 0.844, p = 0.006). Providers who more recently completed residency training employed URS more often (p = 0.023). Provider and facility volume were associated with initial procedure selection. The odds of a second procedure following initial SWL were 1.54 times that of URS (p<0.001).
Conclusions
Non-clinical factors are associated with use of URS or SWL for initial stone management, which may reflect provider and/or patient preferences or experience. Further investigation is required to understand the impact of these outcomes on quality and cost of care.
Keywords: ureteroscopy, shock wave lithotripsy, outcomes
Introduction
Urinary lithiasis imposes a significant burden of disease in the United States. The prevalence of stone disease rose from 3.8% in 1976 to 5.2% in 1994.1 More recent analyses suggest that the incidence of stone disease may be rising faster among women than men, although remaining more common in males.2, 3 The healthcare resource burden is significant. In the United States, only urinary tract infection exceeds urinary lithiasis in total urologic treatment expenditures.4 In the Medicare population the annual direct costs of treatment approach $1 billion. In addition to direct costs, patients experience significant morbidity during treatment of a symptomatic stone episode.5
Despite these significant healthcare expenditures and the growing burden of urinary lithiasis in the United States, relatively few studies5, 6 have examined cost drivers of surgical therapy. A model suggests that URS is more cost effective for ureteral calculi than SWL.6 However, practice variation in the surgical management of urinary lithiasis is poorly documented. Therefore, how practice variation may contribute to the cost of disease management is not well understood.
Given this context, we sought to characterize variation in practice for management of urinary calculi with ureteroscopy and SWL. In addition, we sought to document outcomes of therapy in a nationally representative cohort. We hypothesized that patient, provider and care setting characteristics would be associated with treatment selection in this cohort.
Methods
Data Source
We the Medicare 5% sample to identify beneficiaries with an index encounter (not necessarily a surgical procedure) for urinary lithiasis from 1997 – 2007. Race/ethnicity are reported by beneficiaries at the time of enrollment. We used the reported categories of “white” and “black” for this analysis, and included all other categories as “other.”
We obtained research-identifiable files from 1997 – 2007 from CMS. We included beneficiaries aged at least 66 years to provide 365 days of prior coverage to identify comorbid conditions and prior encounters for nephrolithiasis. Claims were restricted to Medicare fee-forservice coverage. The institutional review board of the RAND Corporation and the University of California, Los Angeles determined that the study was exempt from the requirement for review.
Study Population
We used diagnostic codes to identify beneficiaries with an index encounter (not necessarily a surgical procedure) for nephrolithiasis between 1997 and 2007. Beneficiaries with ICD9-CM codes of 592.0, 592.1, and 592.9 were included. In order to minimize recurrent nephrolithiasis, we excluded beneficiaries with any claim for urinary lithiasis in the 365 days prior to the index encounter, as well as beneficiaries with a diagnostic code of 270.0 (disturbance of amino acid transport) or 274.11 (uric acid nephrolithiasis) or 788.0 (flank pain). We used CPT codes to identify the subset of beneficiaries in the cohort who then underwent SWL or ureteroscopic procedures. Patients with initial procedures before January 1, 1998 were excluded in order to have a full year of claims for classification of comorbid conditions. Patients with initial procedures after September 1, 2007 were excluded in order to have at least 120 days of follow-up after the initial procedure.
Outcomes
The primary outcome of the study was the treatment (SWL or URS with or without laser fragmentation) received by the beneficiary. The secondary outcome of the study was performance of a second procedure (SWL or URS) within 120 days of the initial procedure. SWL was identified by CPT code 50590 or IC9-CM procedural code 98.51. URS was defined by CPT codes 52352, 52336, 52351, 52335, 52320, whereas URS with fragmentation (URS+L) was defined by CPT codes 52353, 52337, 52325.
Covariates
Patient age, race (white, black, other) and sex were determined from denominator files. Comorbid conditions were assessed using the Charlson score based on diagnostic codes appearing on encounter claims in the 365 days prior to the index stone encounter. Markers of socioeconomic status were determined at the FIPS county level using data from the ARF. Annual household income was classified as $0 to 35,000, $35,001 to $50,000, and greater than $50,000. Education was measured as the percentage of the population with a college education.
Provider characteristics were identified using the UPIN in the claims files. High volume providers were classified as those in the top quartile for SWL or ureteroscopy. Length of time in practice was determined from the first time the provider appeared in CMS claims data.
Care setting characteristics were identified from claims data and linked data from the AHA. Inpatient and outpatient care settings were determined from claims data. Facility location (urban versus rural), ownership status (not for profit, government owned, for profit) and teaching status (yes or no) were determined from AHA data. Facility volume was determined using claims data; facilities in the top decile for a procedure were classified as high volume.
Local area healthcare resources may also influence treatment selection. For this reason, we used the ARF to identify measures of local healthcare infrastructure. The number of ambulatory surgical centers at the county FIPS level was determined using data from the ARF. Similarly, the number of urologists per capita was determined at the FIPS county level.
Statistical Analysis
We used a logistic regression model to identify patient, provider, care setting and local area characteristics associated with treatment selection (SWL or ureteroscopy). We also used a logistic regression model to compare the likelihood of undergoing a second treatment procedure within 120 days of the initial treatment procedure, controlling for patient, provider, care setting and local area characteristics. Results of our sensitivity analyses, in which we stratified by ICD-9 codes 592.0 and 592.1, did not differ substantially from our primary analysis. Therefore, only the detailed results of our primary analysis are presented herein. Results were considered statistically significant with two-sided α < 0.05. We used SAS version 9.1 (Cary, North Carolina) for all statistical analyses.
Results
The cohort comprised 9358 beneficiaries, among whom 5208 (56%) underwent initial SWL, whereas URS (with or without fragmentation) was initially utilized in 4150(44%). Overall, 59% of beneficiaries were aged between 66 – 74 years. 61% of beneficiaries were male and 92% were white. On univariate analysis (Table 1), there were small differences in characteristics between beneficiaries undergoing SWL versus URS or URS+L. For example, patients with higher Charlson scores were more likely to undergo ureteroscopic intervention (p<0.001). Differences in age, sex, and race were statistically, but not clinically, significant.
Table 1.
Characteristics of study cohort, by initial treatment.
| Characteristic | SWL (n = 5208) |
URS (n = 2645) |
URS+L (n = 1505) |
p value |
|---|---|---|---|---|
| Age | <0.001 | |||
| 66–74 | 3199 (61) | 1481 (56) | 853 (57) | |
| 75–84 | 1752 (34) | 969 (37) | 556 (37) | |
| 85+ | 257 (5) | 195 (7) | 96 (6) | |
| Female | 2000 (38) | 1085 (41) | 525 (35) | <0.001 |
| Race | <0.001 | |||
| White | 4782 (92) | 2459 (93) | 1383 (92) | |
| Black | 236 (5) | 131 (5) | 60 (4) | |
| Other | 190 (4) | 55 (2) | 62 (4) | |
| Charlson Score | <0.001 | |||
| 0 | 4143 (80) | 1928 (73) | 1113 (74) | |
| 1 | 624 (12) | 386 (15) | 212 (14) | |
| ≥2 | 441 (8) | 331 (13) | 180 (12) | |
| Median Household Income | <0.001 | |||
| <$35,000 | 1273 (24) | 668 (25) | 289 (19) | |
| $35,000 – 50,000 | 2890 (56) | 1517 (57) | 867 (58) | |
| >$50,000 | 1034 (20) | 459 (17) | 347 (23) | |
| Education | 0.033 | |||
| <15% | 1360 (26) | 692 (26) | 375 (25) | |
| 15 – 25% | 2074 (40) | 1058 (40) | 554 (37) | |
| >25% | 1765 (34) | 894 (28) | 574 (38) |
On multivariable analysis, few of these differences persisted (Table 2; for analytic purposes, ureteroscopic procedures with or without fragmentation are combined). The odds of female beneficiaries undergoing URS were 0.844 [0.75 – 0.95; p< 0.001] times that of males. Neither age nor race was statistically associated with choice of procedure. Similarly, income, education, and comorbidity were not associated use of URS.
Table 2.
Results of multivariable model identifying characteristics associated with ureteroscopy for initial treatment.
| Characteristic | Odds Ratio | 95% CI | p value | |
|---|---|---|---|---|
| Age | ||||
| 66 – 74 | Reference | -- | -- | |
| 75 – 84 | 0.98 | 0.87 – 1.11 | 0.781 | |
| ≥85 | 1.01 | 0.78 – 1.32 | 0.921 | |
| Year | 1.002 | 0.98 – 1.03 | 0.865 | |
| Race | ||||
| White | Reference | -- | -- | |
| Black | 1.10 | 0.83 – 1.46 | 0.500 | |
| Other | 0.72 | 0.51 – 1.02 | 0.067 | |
| Female | 0.844 | 0.75 – 0.95 | 0.006 | |
| Income | ||||
| <$35,000 | Reference | -- | -- | |
| $35,000 – 50,000 | 1.18 | 1.01 – 1.39 | 0.042 | |
| >$50,000 | 1.06 | 0.83 – 1.35 | 0.661 | |
| College Educated | 1.20 | 0.44 – 3.31 | 0.722 | |
| Charlson | ||||
| 0 | Reference | -- | -- | |
| 1 | 1.07 | 0.90 – 1.27 | 0.468 | |
| ≥2 | 1.07 | 0.88 – 1.32 | 0.495 | |
| High SWL volume (MD) | 0.18 | 0.16 – 0.21 | <0.001 | |
| High URS volume (MD) | 4.71 | 4.14 – 5.36 | <0.001 | |
| Practice Start Year | 1.05 | 1.01 – 1.09 | 0.023 | |
| Outpatient Setting | 0.09 | 0.07 – 0.10 | <0.001 | |
| Urban Location | 0.95 | 0.81 – 1.12 | 0.560 | |
| Ownership | ||||
| Not for profit | Reference | -- | -- | |
| Government | 0.92 | 0.77 – 1.10 | 0.343 | |
| For Profit | 0.90 | 0.75 – 1.08 | 0.244 | |
| Teaching Hospital | 0.90 | 0.75 – 1.08 | 0.260 | |
| No. ASC in FIPS | ||||
| 0 | Reference | -- | -- | |
| 1–3 | 1.13 | 0.93 – 1.36 | 0.217 | |
| 4–8 | 1.15 | 0.91 – 1.47 | 0.239 | |
| ≥9 | 1.04 | 0.79 – 1.36 | 0.794 | |
| No. Urologists in FIPS | ||||
| 0 | Reference | -- | -- | |
| 1–6 | 1.01 | 0.83 – 1.23 | 0.901 | |
| 7–25 | 1.15 | 0.91 – 1.47 | 0.688 | |
| ≥26 | 1.04 | 0.79 – 1.36 | 0.826 | |
| High Volume URS facility | 1.44 | 1.17 – 1.76 | <0.001 | |
| High Volume SWL facility | 0.32 | 0.25 – 0.41 | <0.001 |
In contrast to patient-related factors, a number of provider characteristics were associated with initial procedure. Providers who more recently started practice were more likely to use URS (OR 1.05 per year, 95% CI 1.01 – 1.09; p = 0.023). Provider volume was strongly associated with the initial procedure selection: beneficiaries treated by providers in the highest volume quartile were overwhelmingly likely to undergo the high volume procedure. For example, the odds of a beneficiary undergoing URS when the provider performed high volume URS were 4.71 times that of undergoing SWL (95% CI 4.14 – 5.36; p<0.001).
Few care setting characteristics were associated with use of URS or SWL. Facility ownership, urban location, and teaching status were not associated with the initial procedure. The number of ambulatory surgical centers and the number of urologists in the local area were also not associated with SWL or URS. The odds of a beneficiary undergoing URS were 44% higher when treated at a high volume URS facility; in contrast, the odds of undergoing ureteroscopy were 68% lower when a beneficiary was treated at a high volume SWL facility.
Of those beneficiaries undergoing an initial SWL, 38% underwent an additional procedure within 120 days. When the initial procedure was ureteroscopic, fewer second procedures were performed: 9% for URS, 18% for URS+L. A multivariable model was used to quantify the odds of undergoing a second procedure within 120 days of the initial procedure, controlling for patient, provider and care setting characteristics. The odds of a second procedure following an initial URS were 0.63 times those of a second procedure following an initial SWL. Beneficiaries undergoing treatment by high volume SWL providers were at increased likelihood of a second procedure (OR 1.19, 95% CI 1.04 – 1.35; p = 0.012), as were those undergoing treatment at a teaching facility (OR 1.22; 95% CI 1.01 – 1.45; p= 0.035).
Discussion
In a cohort of Medicare beneficiaries, we found significant variation in the use of competing technologies for management of urinary lithiasis. Males were more likely to undergo ureteroscopy, and URS was more commonly utilized by recently trained providers. Provider and facility volume were also associated with selection of initial treatment.
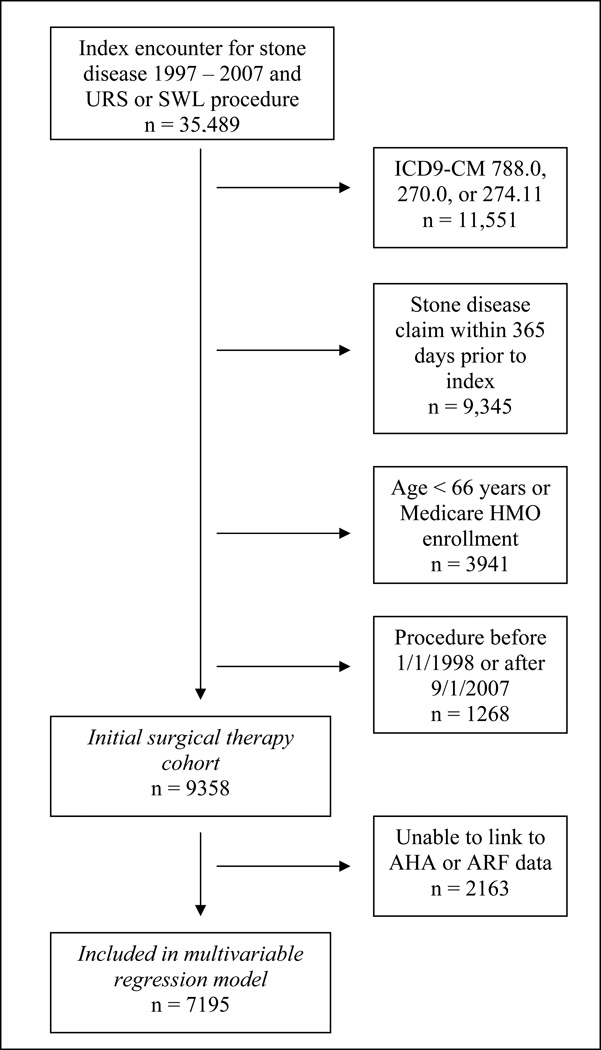
While stone size and location are undoubtedly the most important clinical factors associated with treatment selection, our results suggest that a number of non-clinical factors may play a role in the surgical management of urinary lithiasis. (Figure 1) Males appear more likely to undergo ureteroscopy than females in this cohort, although the reason for differential treatment selection is unclear.
Figure.
Flow chart of patients in cohort.
Provider characteristics were also associated with treatment selection. Provider volume was strongly associated with procedure selection: patients treated by high volume ureteroscopists tended to undergo ureteroscopy; similar findings were observed for SWL. Interestingly, providers who more recently started practice were more likely to use ureteroscopy than SWL. A recent analysis of board certification logs by Matlaga et al also suggests that more recently trained urologists are more likely to use ureteroscopy than SWL.9 These findings suggest that lack of familiarity or training with ureteroscopic technology may be a barrier to its uptake. Whether practice patterns will change over time as recently trained urologists continue to enter the workforce remains to be seen.
Facility ownership was not associated with selection of the initial treatment procedure. Other investigators have demonstrated an association between individual physician ownership of ambulatory surgical centers and surgical volume.10, 11 Differences between our results and those of other investigators are likely due to the manner in which ownership (e.g. facility for profit status vs. individual physician level) is defined; the extent to which ownership incentives may influence provider behavior in our sample remains uncertain.
Our analysis also examined factors associated with use of a second treatment procedure (URS or SWL) within 120 days of an initial procedure. In our cohort, almost 2 in 5 beneficiaries undergoing SWL underwent a second procedure, as compared with an average of only 1 in 8 after ureteroscopic intervention. It is well established that SWL may require more procedures than URS to completely treat a stone.12 However, the “right” rate of additional treatment following an initial SWL is unclear. The smaller focal zones of new lithotripter models may decrease the efficiency of stone fragmentation.13 Lower shock wave frequencies increase the efficacy of fragmentation, at the cost of a longer treatment.14 SWL is very successful at treating stones less than 10mm in size, but stone free rates are markedly lower as size increases.15, 16 Although it is unclear to what extent misaligned financial incentives influence practice, SWL has one of the highest reimbursements per unit time of any urologic procedure,6, 17 and a significant proportion of urologists report ownership interests in lithotripters.18, 19 From a societal perspective, the ideal procedure mix would balance overall costs, access, benefits, and potential harms of treatment in accord with best evidence.
Our analysis has several limitations. In addition to the characteristics we evaluated, patient preferences and values likely play an important role in treatment selection. Unfortunately, the role of patient preferences cannot be assessed in this claims-based analysis. High volume providers or facilities may have unique characteristics that we are unable to capture in this analysis, and we did not account for possible clustering of outcomes by facility or provider. We could not differentiate mobile and fixed lithotripter facilities. Treatment selection may be influenced by patient preference for a non-invasive procedure.21 However, medical decision-making and patient preferences for ureteroscopy or SWL have not been systematically evaluated to date. The dynamics of shared decision-making between patient and provider require further investigation.
The claims-based nature of our analysis precludes use of important clinical factors (i.e. stone size or location). Billing codes do not reliably distinguish between renal and ureteral calculi;22 sensitivity analysis stratifying by diagnostic codes of 592.0 and 592.1 yielded broadly similar results. Thus, our findings should be interpreted cautiously, especially when assessing whether a particular technology is applied appropriately. Use of Medicare claims data may limit generalizability. Medicare data was selected because certain provider and care setting characteristics would have been otherwise unavailable. Observed patterns of care may not apply to younger patients, although patterns of care are frequently similar between private- and government-payer beneficiaries.
Despite these limitations, our findings retain significant validity. We examined variation in practice patterns and outcomes in a large, community-based cohort, and used multivariable models to identify associations between treatment selection and patient, provider and care setting characteristics. While more granular clinical data is required to understand these practice patterns, we believe the results provide a valid description of surgical management among Medicare beneficiaries.
CONCLUSION
In this longitudinal analysis of Medicare beneficiaries, we found significant variation in treatment selection and outcomes for surgical management of urinary lithiasis. The extent to which these practice patterns contribute to the high cost of stone disease management remains unclear. These findings highlight the need for improved understanding of practice patterns and patient preferences in the surgical management of stone disease in order to optimize quality of care for urinary lithiasis in the United States.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Stamatelou KK, Francis ME, Jones CA, et al. Time trends in reported prevalence of kidney stones in the United States: 1976–1994. Kidney Int. 2003;63:1817. doi: 10.1046/j.1523-1755.2003.00917.x. [DOI] [PubMed] [Google Scholar]
- 2.Pearle MS, Calhoun EA, Curhan GC. Urologic diseases in America project: urolithiasis. J Urol. 2005;173:848. doi: 10.1097/01.ju.0000152082.14384.d7. [DOI] [PubMed] [Google Scholar]
- 3.Scales CD, Jr, Curtis LH, Norris RD, et al. Changing Gender Prevalence of Stone Disease. J Urol. 2007;177:979. doi: 10.1016/j.juro.2006.10.069. [DOI] [PubMed] [Google Scholar]
- 4.Litwin MS, Saigal CS. Introduction. Washington, DC: US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2007. [Google Scholar]
- 5.Saigal CS, Joyce G, Timilsina AR. Direct and indirect costs of nephrolithiasis in an employed population: opportunity for disease management? Kidney Int. 2005;68:1808. doi: 10.1111/j.1523-1755.2005.00599.x. [DOI] [PubMed] [Google Scholar]
- 6.Lotan Y, Gettman MT, Roehrborn CG, et al. Management of ureteral calculi: a cost comparison and decision making analysis. J Urol. 2002;167:1621. [PubMed] [Google Scholar]
- 7.Flegal KM, Carroll MD, Ogden CL, et al. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 303:235. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 8.Pareek G, Hedican SP, Lee FT, Jr, et al. Shock wave lithotripsy success determined by skin-to-stone distance on computed tomography. Urology. 2005;66:941. doi: 10.1016/j.urology.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 9.Matlaga BR. Contemporary surgical management of upper urinary tract calculi. J Urol. 2009;181:2152. doi: 10.1016/j.juro.2009.01.023. [DOI] [PubMed] [Google Scholar]
- 10.Hollingsworth JM, Ye Z, Strope SA, et al. Physician-ownership of ambulatory surgery centers linked to higher volume of surgeries. Health Aff (Millwood) 2010;29:683. doi: 10.1377/hlthaff.2008.0567. [DOI] [PubMed] [Google Scholar]
- 11.Strope SA, Daignault S, Hollingsworth JM, et al. Physician ownership of ambulatory surgery centers and practice patterns for urological surgery: evidence from the state of Florida. Med Care. 2009;47:403. doi: 10.1097/mlr.0b013e31818af92e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Preminger GM, Tiselius HG, Assimos DG, et al. 2007 guideline for the management of ureteral calculi. J Urol. 2007;178:2418. doi: 10.1016/j.juro.2007.09.107. [DOI] [PubMed] [Google Scholar]
- 13.Lingeman JE. Extracorporeal shock wave lithotripsy--what happened? J Urol. 2003;169:63. doi: 10.1016/S0022-5347(05)64035-9. [DOI] [PubMed] [Google Scholar]
- 14.Pace KT, Ghiculete D, Harju M, et al. Shock wave lithotripsy at 60 or 120 shocks per minute: a randomized, double-blind trial. J Urol. 2005;174:595. doi: 10.1097/01.ju.0000165156.90011.95. [DOI] [PubMed] [Google Scholar]
- 15.Albala DM, Assimos DG, Clayman RV, et al. Lower pole I: a prospective randomized trial of extracorporeal shock wave lithotripsy and percutaneous nephrostolithotomy for lower pole nephrolithiasis-initial results. J Urol. 2001;166:2072. doi: 10.1016/s0022-5347(05)65508-5. [DOI] [PubMed] [Google Scholar]
- 16.Preminger GM, Assimos DG, Lingeman JE, et al. Chapter 1: AUA guideline on management of staghorn calculi: diagnosis and treatment recommendations. J Urol. 2005;173:1991. doi: 10.1097/01.ju.0000161171.67806.2a. [DOI] [PubMed] [Google Scholar]
- 17.Lotan Y, Cadeddu JA, Roehrborn CG, et al. The value of your time: evaluation of effects of changes in medicare reimbursement rates on the practice of urology. J Urol. 2004;172:1958. doi: 10.1097/01.ju.0000142016.51680.fa. [DOI] [PubMed] [Google Scholar]
- 18.Gee WF, Holtgrewe HL, Blute ML, et al. 1997 American Urological Association Gallup survey: Changes in diagnosis and management of prostate cancer and benign prostatic hyperplasia, and other practice trends from 1994 to 1997. J Urol. 1998;160:1804. doi: 10.1016/s0022-5347(01)62418-2. [DOI] [PubMed] [Google Scholar]
- 19.O'Leary MP, Baum NH, Blizzard R, et al. 2001 American Urological Association Gallup Survey: changes in physician practice patterns, satisfaction with urology, and treatment of prostate cancer and erectile dysfunction. J Urol. 2002;168:649. doi: 10.1016/s0022-5347(05)64706-4. [DOI] [PubMed] [Google Scholar]
- 20.Scales CD, Jr, Voils CI, Fesperman SF, et al. Barriers to the practice of evidence-based urology. J Urol. 2008;179:2345. doi: 10.1016/j.juro.2008.01.109. [DOI] [PubMed] [Google Scholar]
- 21.Pearle MS, Nadler R, Bercowsky E, et al. Prospective randomized trial comparing shock wave lithotripsy and ureteroscopy for management of distal ureteral calculi. J Urol. 2001;166:1255. [PubMed] [Google Scholar]
- 22.Semins MJ, Trock BJ, Matlaga BR. Validity of administrative coding in identifying patients with upper urinary tract calculi. J Urol. 2010;184:190. doi: 10.1016/j.juro.2010.03.011. [DOI] [PubMed] [Google Scholar]