Abstract
Although stigma is a significant barrier to HIV prevention and treatment globally, the culture-specific psychosocial processes through which HIV-infected Chinese experience stigma have not been described. This study used grounded theory to explore the social and psychological processes of HIV-related stigma experienced by Chinese injection drug users and proposed a culture-specific concept of stigma. The focus group had six participants, and we conducted 16 individual interviews. The core category emerged as “Double struggle: Returning to normalcy.” Key concepts were dual stigma and family support, while keeping secrets and active drug use were factors influencing the struggle to return to normalcy. Family responsibility played an important role in bringing family members together to cope with HIV. Recommendations for Chinese health care providers include leveraging the traditional Chinese concept of family responsibility to establish a family alliance in response to the dual stigma and providing psychological counseling and education in treatment clinics.
Keywords: conceptualization, family responsibility, HIV, injection drug use, stigma
Stigma is a significant barrier to the prevention and treatment of HIV infection. Although attitudes toward persons living with HIV (PLWH) have improved in recent years (Lee, Kochman, & Sikkema, 2002), the insidious effects of stigma are still prevalent in most of the world. HIV-related stigma affects the lives of PLWH by lowering quality of life, limiting access to and use of health services, and reducing adherence to antiretroviral (ARV) treatment (Aranda-Naranjo, 2004; Prachakul, Grant, & Keltner, 2007; Rao, Kekwaletswe, Hosek, Martinez, & Rodriguez, 2007). Partially as a result of stigma, PLWH are depressed and anxious, reporting feelings of grief, guilt, and lack of personal value (Duffy, 2005; Lee et al., 2002).
Information about the psychosocial processes through which PLWH actually experience stigma is limited. Most studies focus on reducing stigmatizing attitudes among the general population. Unfortunately, evidence suggests that reductions in prejudice and discriminatory behavior among HIV-uninfected people do not lead inevitably to improved outcomes for PLWH (Brown, Macintyre, & Trujillo, 2003). Further, the concentration of studies on HIV stigma in developed parts of the world limits generalization of the results to low and moderate resourced countries. A review of HIV stigma scales revealed that 14 scales were developed in the United States, seven in Africa, and only four in Asia, none of which measured stigma from the perspective of PLWH (Earnshaw & Chaudoir, 2009). Finally, studies examining dual stigma, such as stigma attached to HIV-infected injection drug users (IDUs), sex workers (SWs), and men who have sex with men (MSM), are rare. The association of HIV with socially devalued identities is likely a key reason why HIV-related stigma has been so difficult to ameliorate.
Some researchers (Steward et al., 2008) have posited two forms of stigma from the perspective of the infected, namely an interpersonal form and an intrapersonal form. Interpersonal stigma, also known as enacted stigma, refers to external acts of stigma experienced by the stigmatized individual. Intrapersonal stigma comprises both the stigma felt and the stigma internalized by the stigmatized individual. Felt stigma refers to the subjective awareness of stigma, and internalized stigma is the extent to which the stigmatized individual accepts that his or her discredited status is valid. Compared to the interpersonal form of stigma, the intrapersonal form has a stronger influence on the overall well-being of PLWH, especially their psychological health (Steward et al., 2008). However, how dual stigma is internalized by HIV-infected IDUs, SWs, or MSM is unclear.
In China, shame and blame are associated with the way HIV is acquired rather than with the condition of HIV disease itself (Cao, Sullivan, Xu, & Wu, 2006). Chinese health professionals hold more negative attitudes toward PLWH than toward patients with hepatitis (Li et al., 2007). IDUs also experience widespread negative attitudes on the part of the Chinese public. Most Chinese consider drug abuse a bad habit, personality flaw, or moral weakness rather than a medical disorder (Tang & Hao, 2007). In a survey of 446 doctors caring for drug users, almost half thought that punishment should be an important component of drug abuse treatment (Tang, Wiste, Mao, & Hou, 2005).
As a result, HIV-infected IDUs experience stigma associated with both drug use and HIV infection (dual stigma). In our recent study conducted in south central China, HIV-infected IDUs reported higher levels of stigma than those who were infected through sexual activity and exposure to blood (Li, Wang, Williams, & He, 2009). However, the effect of dual stigma is not necessarily additive. In Yunnan Province, with the nation’s highest HIV prevalence and the largest number of PLWH with a history of past or current IDU, the diagnoses of HIV infection and AIDS appear not to exacerbate the stigma already attached to IDUs (Deng, Li, Sringernyuang, & Zhang, 2007). Other studies of medical students in China (Chan, Yang, Zhang, & Reidpath, 2007) and nursing students in Thailand (Chan, Stoove, Sringernyuang, & Reidpath, 2008) revealed that presumed IDUs were less stigmatized after an HIV diagnosis. To date, no studies have examined the psychosocial processes associated with the dual stigma of drug abuse and HIV in China. Better understanding of the dual stigma experienced by HIV-infected IDUs would contribute to the development of strategies to reduce the negative impact of HIV-related stigma among vulnerable groups.
Earlier work has suggested that HIV-related stigma is a social construct grounded in cultural, social, historical, and situational factors, and the expression of stigma differs in different sociocultural contexts (Parker & Aggleton, 2003) and among different racial groups (Rao, Pryor, Gaddist, & Mayer, 2008). To learn more about the culturally specific experience of stigma associated with the dual conditions of HIV infection and IDU, we conducted a grounded theory study among HIV-infected IDUs in central south China. The study aimed to (a) describe the process of stigma experienced by those who were infected with HIV and also used illegal drugs, (b) explore how the two types of stigma each affected respondents’ lives, and (c) propose a conceptual framework to explain how HIV-related stigma is experienced by IDUs in China.
Methods
A grounded theory design was chosen to explore the stigma experienced by HIV-infected IDUs. Guided by Herbert Blumer’s Symbolic Interactionism, this study sought to understand HIV-infected IDUs’ stigma experience based on meanings derived from social interaction and modified through the respondents’ own interpretations.
Study Location
Hengyang City, an old and important transportation hub in south central Hunan Province, served as the study location. More than 10,000 cases of HIV and AIDS have been diagnosed in Hunan Province, and Hengyang is the most severely affected area of the province (internal information of Hunan Health Department, personal communication, October 20, 2010). Forty percent of PLWH in Hengyang are reported to have been infected through sharing needles. Members of the research team have established a positive relationship with the local AIDS treatment center, have rich experiences working with drug users and PLWH, and are fluent in the local dialects.
Sample
Inclusion criteria were active or former injecting drug use, confirmed positive HIV test results, age greater than 18 years, and ability to communicate in either Mandarin or Hengyang dialect. Potential participants were excluded if they were mentally disabled or too ill to communicate. Purposive sampling was employed to capture a wide range of the stigma experiences and the perceptions of a diversified sample of IDUs. Consistent with ground theory methods, as the study progressed and data were analyzed, additional subjects were recruited to develop emerging categories. One uninfected drug user and one HIV-infected non-drug user were added to the sample for this purpose.
The sample size was determined by information saturation. “Saturation refers to the completeness of all level of codes or the expansion of existing ones. The researcher, by repeatedly checking and asking questions of the data, ultimately achieves a sense of closure” (Hutchinson, 1986, p. 125). After 22 participants were interviewed, no new codes were identified and the study was closed.
Data Collection
Data were collected during one focus group (N = 6) and 16 semi-structured in-depth interviews, which were conducted between April and June 2009. The focus group was conducted before the individual interviews in order to get a wide range of information from participants with diversified backgrounds and communication skills. Individual interviews then expanded and built upon the initial codes identified in the focus group.
Sample characteristics collected included age, race, gender, marital status, educational background, income, employment status, type(s) of drugs used, length of drug use, HIV serostatus, ARV treatment status, and methadone maintenance status. The semi-structured interview schedule comprised a list of open-ended questions based on four broad areas: the effect of drug use on respondents’ lives, the effect of HIV seropositivity on respondents’ lives, respondents’ self-perceptions of the effects of both conditions, and respondents’ interpretations of stigma related to drug abuse and HIV.
The interview questions were revised after the first several interviews as the researchers’ theoretical understanding of the phenomenon grew. Additional questions included “How would you compare AIDS with cancer?”, “How do you think about AIDS and drug abuse?”, and “How do you think the situation would be if you were to become HIV infected?” (for the uninfected drug user). In addition, field notes, made at the time of the interviews, recorded observations of the participants in their treatment or community settings.
We conducted the focus group and interviews in a private room at the Hengyang AIDS clinic, and the participants’ primary health care providers did not take part. The interviewers avoided exhibiting judgmental attitudes regarding participants’ self-reported behaviors, including drug use, sexual behaviors, and medication adherence.
The focus group, with six participants, lasted 50 minutes. The 16 individual interviews ranged from 30 to 80 minutes. All discussions except two individual interviews were tape recorded and transcribed verbatim. Field notes were used to document the two non–tape recorded individual interviews.
The Institutional Review Committee in the School of Nursing, Central South University, approved this study. We provided standard written informed consent. However, one participant preferred to give oral consent. Each participant was assigned a number and referred to by number rather than by name on all data forms and audio-tapes.
Data Analysis
Data analysis was guided by the five steps of grounded theory research described by Stern (1980). Analysis began with data collection. After transcribing the audio interviews, we coded the data immediately. When coding the data, constant comparative analysis was used. Three levels of codings, namely open coding, axial coding, and selective coding, facilitated this process. As concepts emerged, we identified links among the concepts. Codes, categories, and concepts were compared constantly during the analysis process. Two of the authors coded individually, first, and then discussed inconsistent codes. Data management and analysis were assisted by software (NVivo 8.0), which is designed especially for grounded theory analysis.
Results
Description of Study Participants
One focus group with six participants and 16 individual interviews were conducted. The ages of the participants ranged from 30 to 46 years, with a median of 36 years. All participants were Han Chinese. One male participant withdrew during the late stage of the focus group interview due to receiving an emergency cellphone call. All others completed the data collection process without influence from the departure of that participant, which could be confirmed from the field notes recording the atmosphere and smoothness of the interview. However, the dynamics of the group might have been affected to some extent.
The focus group included five men and one woman. Four focus group participants formerly injected drugs and two currently engaged in IDU. Only one member of the focus group had disclosed his HIV status, but the drug using behaviors of five members of the group were well known in their neighborhoods.
Four women and 12 men contributed individual interviews. Among those interviewed, the length of drug use ranged from 5 to 18 years with a median of 9 years, and the median length of time since HIV diagnosis was 3 years (range = 1–7 years). Seven participants were actively using drugs, while five were receiving methadone maintenance therapy. One male participant was not a drug user, and one male drug-using participant was not infected with HIV; both were recruited as a result of theoretical sampling. All participants had disclosed their drug using behaviors, but only nine had disclosed their HIV status to at least three non-family members.
Double Struggle: Returning to Normalcy With HIV and Drug Use
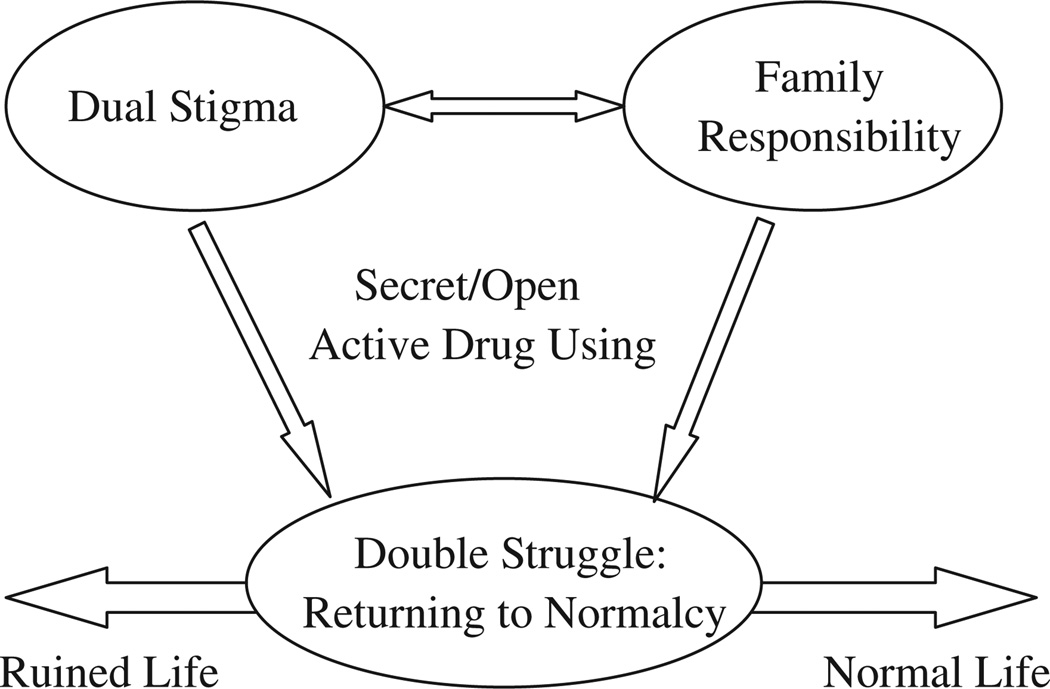
The core category identified in this study was labeled “Double struggle: Returning to normalcy with HIV and drug use.” Dual stigma and family support emerged as key concepts, while keeping secrets and active drug use were factors influencing the struggle to return to normalcy. These relationships are shown in Figure 1 and discussed in later sections.
Figure 1.
The framework of core category, main concepts, and influencing factors.
In the eyes of HIV-infected IDUs, “normal” referred to a condition without drug abuse behavior or HIV infection. When they began using drugs or became HIV infected, our participants immediately internalized the concept that using drugs or contracting HIV infection was abnormal; they began thinking of themselves as abnormal and withdrew from a common social life. A focus group participant said, “Before I took heroin, I had many normal friends [people who don’t use drugs], and we communicated normally, but now… I can’t stay with these normal friends… I can’t marry a normal person….” Another focus group participant added, “I don’t talk to them, because they are normal people… if I were normal, I wouldn’t want to talk with you [refers to himself] either.”
They described struggling to escape from the attributes of drug abuse and HIV infection. During the interviews, participants tended to misuse personal pronouns with the effect of distancing themselves from drug abuse or HIV infection. Examples include participants who, referring to themselves, said: “When you came, they run away,” “They ignored you,” and “I am the only boy of their family.” All the second and third personal pronouns referred to the patients themselves.
HIV-infected IDUs live lives of extreme contradictions that lead to constant struggle. One contradiction was represented by the strong desire to stop using heroin in the face of continuing use. Almost every participant wished to stop using drugs; however, few were prepared to experience the physical and psychological symptoms of abstinence:
Who doesn’t want to stop using drugs? Most of them went to voluntary or compulsory abstinence center for many times, the results are the same [go back to drug again]… I was the most successful one for not using drugs for 8 years….
Some participants offered explanations for returning to drug use, such as “Since there is no more hope after getting HIV infected, there is no need to stop drug using,” or “Eight out of 10 people in the [abstinence] center said that heroin are better than ARV medications.”
Other contradictions were related to struggling to live with HIV, such as not wanting people to know their HIV status but being unable to obtain financial and emotional support without revealing their infection. They didn’t know whether to live with HIV or commit suicide. One person believed she might commit suicide if her situation deteriorated, while another continued to live only for her daughter’s sake. Most participants were taking ARV medications, but they still were not hopeful. They considered that life was just counting days.
Family Responsibility: A Sudden Pain Would Be Better
Family responsibility was a key concept that comprised two dimensions. One was the family members’ responsibilities to take care of the participant, and the other was the perceived responsibility of the participant to take good care of the whole family. Families of all of the participants initially tried many methods to help participants stop illicit drug use, but frequent relapses were discouraging. Most participants found that their families were more accepting of the HIV diagnosis than of drug use behavior. “When it is the time [to have a meal or take ARV medication], they will call me to remind me…. They care for me much more recently compared to when I was using drugs.”
On the other hand, the participants’ perceptions of their responsibilities to their families encouraged them to live a life that appeared normal. They felt a need to save money or to earn money for children and other family members:
All worries were about my daughter. What would she do if both of us [participant and her husband] died? She always encouraged me and asked me to take medication… If I can persist with treatment until she graduates and finds a job, there is nothing I will regret even if I died….
Participants who reported ongoing family support and a sense of need to do something for the family were able to return to normal daily lives. For others, negative coping styles emerged, such as binge use of heroin, drug dealing, or contemplation of suicide.
She [my mother] never came to the hospital to see me. She thought she would lose face if she came. She was ashamed of her daughter… [There was] no one I could depend on, so I decided to sell heroin….
Another participant’s CD4+ T cell counts were lower than 250 cells/mm3, but she refused to take ARV, saying “[I] owe them [family members] too much… I don’t want them to be sorry for me, to have tears for me. A sudden pain might be better [for them] than long-term pain…. ” She considered suicide as a “sudden pain” that would spare her family the long term pain of her illness.
Dual Stigma
Dual stigma, the second key concept in the model, refers to the concomitant experience of drug-related stigma and HIV-related stigma. Almost all the IDUs reported experiencing both social stigma and family stigma as a result of drug use and HIV infection. Social stigma was reflected in perceptions of negative treatment by non-family members. The negative treatment reported included avoidance, disdain, denial of recognition by acquaintances, and job loss. Participants speculated that there were two reasons for these behaviors. One was that people feared the IDUs would attempt to borrow money from them; the other was fear that the IDU would threaten them in some way or commit an actual crime. One participant said:
I signed a contract for a job on July 1st, but after I came back from the Reeducation Through Labor Center (RTLC) because of an occasional use of heroin, they fired me. And then, I looked for other jobs, but they didn’t employ me, just because I was there [RTLC] for two times… My neighbors seem good to me, because they know I never borrow or steal money from them, but they fear of infection of this disease, so they kept certain distance with me at first….
Another participant stated:
My family moved to Beijing now, and they even don’t leave a telephone number to me, they lost hope on me, because my relapse, plus I got this disease… I once handed a candy to a child. His grandma immediately refused, and said, “You will not eat things from this aunt, because she doesn’t have good teeth.”
Family stigma was reflected in families who did not provide money or care to the IDUs. Participants suggested this dereliction of the widely held Chinese duty to care for family members was because drug using behavior was hard to conceal, and when it was disclosed, the whole family was discriminated against. Family members of drug users would lose face in the neighborhood and work place. In addition, few families could afford the financial expenses associated with heroin use.
My mom is a strong-minded woman, she became a widow when she was 36 years old, but she bought two apartments for me and my brother… I used all of her money, stole valuable things from my home. Once I threatened her with a knife to demand money… I was a jerk then… My mom lost face in the neighborhood.
Secrecy Vs. Disclosure: A Shadow in My Heart
The process of “struggling” led to two different outcomes: some participants pretended to live a “normal” life, while others withdrew from “normal” social interactions. Secrecy was one of the factors that influenced this process. Active drug using behaviors are harder to conceal than HIV infection. Participants who kept their HIV infection secret and also stopped using drugs reported that they could live a normal life physically and socially, although not psychologically. For example, one participant who had been drug-free for years moved from his village to the city after his HIV diagnosis. He found a job in the city, where no one knew his secret. He reported that he basically lived a “normal” life now:
I found a job in the city and earn 1,000 Yuan [$154 U.S.] per month. It is not much, but enough for basic life. No one knows my drug-using history and my AIDS. It is OK… But there is a shadow in my heart. After all I used drugs before and now have this disease…. When my new colleagues chat about AIDS, I feel very uncomfortable…. It seems I have disguised my facts….
Among our 22 participants, most had not experienced HIV-related discrimination from the public because they kept the diagnosis a secret. On one hand, this self-protective behavior helped them live a so-called normal life; but on the other hand, it deprived them of many health care privileges: “According to the Four Free and One Care policy, we can apply for subsidies [from local government], but we don’t dare [to apply, in case the HIV status is disclosed].”
One participant came to the AIDS clinic for intravenous infusion every day. When asked why he did not choose to be hospitalized so that his health insurance would cover some of the expense, he responded, “If I live in the hospital, my colleagues must come to see me; they are gonna to know….” One female participant also expressed her concern: “I couldn’t reveal which hospital I was in when my best friends called….”
Keeping the HIV diagnosis secret in order to live a normal life was intended to protect not only the participant but also his or her entire extended family. Keeping this secret illustrated the participants’ commitment to “family responsibility”:
Who wants to be seen on TV [when talking about a TV program focusing on HIV stigma]? I bet no one. You might [be willing to] go on, but you have family, have relatives and friends. You can’t ruin their lives; you can’t be so selfish.
The long-term effect of HIV disclosure was not as bad as participants imagined. Most participants who disclosed their sero-status reported experiencing discrimination at first, followed by acceptance by their neighbors. As they established contacts with others in their communities, they eventually struggled back to normal life, not only physically and socially, but also psychologically: “Sometimes I help them [her neighbors] carry stuff, and they appreciate me very much…. They don’t fear me. They know this disease. They watch television and they know the transmission routes….” And:
After my story was reported by the TV show, “Qun Qing Ji” [looking for love], there were changes. They don’t fear the disease as before. Some already knew and understood [this disease]. They dare to buy my fish again, and we communicate much better than before.
Active Drug Use Vs. Stopping Drug Use
Ongoing drug use significantly influenced the participants’ struggles back to normalcy. After receiving an HIV diagnosis, those who continued using drugs and committing crimes found that family members gave up on providing support. Examples included leaving the participant to live in a lonely room or house and no longer providing them with food or money. In contrast, although HIV-infected participants who had stopped using drugs did report continuing social stigma from both their drug use history and their HIV diagnosis, the family stigma they reported was related only to HIV.
Most participants who had stopped drug use reported receiving even more care and emotional support from their families after they were diagnosed with HIV because the participants and family had been educated about transmission routes and treatment information at their local AIDS clinics. “No matter what kind of disease you have, your family will accept you always,” and “Parents never dislike and avoid their children,” were typical expressions. Four participants were rejected by their families, but all believed that the key reason for their exclusion was actively using or selling drugs:
My elder sister didn’t call when I was using heroin. After I got married and stopped using drugs, she changed her attitude and began to give me much economic support, great support…. When she got to know my disease, she seemed to be in a bad mood but was better than when I was using drugs….”
Other participants said:
They [siblings] give me money because they know I am not using heroin anymore; otherwise, they won’t give me money…. [Her family member said] this disease is not horrible, we still accept you and can take care of you, but if you insist on hanging out with that guy [an HIV-infected IDU who was seriously ill], you should never come back….
And:
My sisters and brothers all know [about the HIV diagnosis]…. We live together, eat at the same table, and don’t use serving chopsticks. They got this kind of knowledge after I was diagnosed. Now my family members don’t reject me.
Serving chopsticks, also translated as public chopsticks, are used in restaurants to move food from the serving dishes to diners’ plates. They are not commonly used in the home or among friends.
A Deserved Punishment: Internalizing Stigma
IDUs adopted the common view that drug-abusing behaviors were discreditable and they devalued themselves, which was reflected in expressions of internalized stigma. Participants described their personalities after they began using heroin as “selfish,” “withdrawn,” “irritable,” an “incomplete personality,” and “dared to do anything [i.e., commit crimes].” They said they despised themselves and described themselves as abnormal persons.
Learning that they were HIV infected was a heavy psychological blow, which greatly increased the participants’ internalized stigma. HIV-infected IDUs internalized the common view that HIV was a horrible and contagious condition. They became hypersensitive to people’s words and behaviors, and expected people to be afraid of them and to discriminate against them. As a result, our participants initially avoided others. When eating with others, they insisted on using serving chopsticks to prevent infecting others:
My new colleagues sometimes chat about AIDS. Their words may mean nothing, but I feel uncomfortable when I hear things, such as that Hengyang is the most severely HIV-impacted area, and I am just from Hengyang…. They don’t know the transmission routes and consider it is easy to get infected if contacting with AIDS patients…. I just leave as soon as possible.
One participant said, “If I found out that someone had this disease, I would say the same words: Don’t play with him, or don’t touch him.” And another said, “Their reactions [discriminatory behaviors] are understandable. If it were me, I would do the same.”
Second, they blamed themselves greatly for becoming HIV infected. Most believed that they deserved to get such an incurable disease. They experienced substantial psychological pressure for bringing shame and burden to themselves and their whole families. Some of the participants gave in to despair and developed negative coping strategies: “People wish we would die earlier. Yes, we are a burden on society, useless. To die earlier may be better for society, family, and also a way out for us. Life is meaningless.” Another said, “I am getting worse and worse. The better my parents treat me, the more pressure I feel…. They help me wash face and feet, give me money…. I just don’t want to be their burden anymore.” One said:
I planned to give up drugs before, in order to live a normal life as others. But after the diagnosis of AIDS, I thought it was meaningless even if I stopped using drugs. I am not using now, but I am not sure how long I can continue. Once I had the determination to stop [heroin], but now I don’t have such a mind set.
And another added, “My mind went blank when I got my diagnosis. I expected to die soon, so I began to use heroin heavier than before, 1 gram per time.”
Third, the participants considered HIV much more horrible than drug abuse or cancer. They believed that HIV was incurable and contagious, and that once infected, death would come soon. In contrast, they thought that it was possible to abstain from drugs and that after stopping drug use people could return to a normal life. Death from cancer was considered normal; while death from HIV was viewed as a deserved punishment.
They think getting this disease must be related to prostitution or using drugs. This disease was called “flirt disease.” People who got it deserved to die…. As for cancer, it was believed to be the result of using pesticides. Cancer patients received pity from people, so they prefer to die of cancer compared to AIDS…. They seem proud to die of cancer [because they can honestly tell the reason of death].
Thus, although former IDUs might receive more family support and experience less stigma after they get infected with HIV, they described much more internalized stigma.
Discussion
The notion of normal described by these HIV-infected IDUs illustrated Goffman’s theory that:
… the stigmatized individual tends to hold the same beliefs about identity that we do. The standards the individual has incorporated from the wider society equip him to be intimately alive to what others see as his failing, inevitably causing him, if only for moments, to agree that he does indeed fall short of what he really ought to be. (Goffman, 1963, p. 7)
The Chinese HIV-infected IDUs in our study believed that IDUs and HIV-infected patients were members of a category of abnormal individuals. Their belief was consistent with that of society. They internalized this cognition and initially isolated themselves, even if they did not actually experience stigma. Once they succeeded in making a secret of their disease and received support from family members, they could return to a symbolic restoration of normal life.
HIV-infected IDUs reported much more stress from their HIV diagnosis than from their drug dependence. Most held misbeliefs about HIV and ARV treatment. They doubted that ARV treatment would be effective and believed that one day they would die in pain. Some believed that heroin was better than ARV medications and named individuals they knew who used heroin rather than ARV medication and who appeared to be healthy. This torturous thinking provided a rationale for using drugs.
In contrast, family members rejected HIV-infected IDU members mainly because of active drug abusing behaviors, which was morally and economically unacceptable to families. When the drug use stopped, most families were willing to accept the responsibilities associated with caring for someone living with HIV infection.
In the traditional Chinese value system of “Xiao-Ti,” children, especially sons, are expected to take good care of their parents, and to live long enough to bury the parents after their death (Zuo, 2008). HIV-infected IDUs consider themselves unable to fulfill their responsibilities because of poor health status and active drug-abusing behaviors. The high value placed on family responsibility creates guilt for HIV-infected drug users, with contradictory consequences. On the one hand, guilt can be a motivation for taking ARVs and living without drugs in order to try to meet their obligations. But on the other hand, for those who are unable to abstain from drug use, the pressure can be intolerable. Some individuals respond negatively to the public and mental stress, with profound depression and even suicide attempts.
The Chinese concept of family is grounded in Confucianism, wherein the value of the family is much greater than that of the individual (Ge, 2009). With this cultural background, family members strive to hold the whole family together through difficult times. The situation is similar to that in Africa where the family plays a very important role in supporting and caring for PLWH as a way of reducing the burden of stigma and promoting health outcomes (Iwelunmor, Airhihenbuwa, Okoror, Brown, & Belue, 2006–2007). However, some families isolate or blame PLWH for the heavy burden they bring to their families (Maman et al., 2009), which was also confirmed by our study results. The reason may be that participants who continued to actively use drugs often did not maintain good relationships with their family members.
Recommendations
Psychological consultation and education are needed to correct HIV-infected IDUs’ misbeliefs and to support their efforts to abstain from drugs, to enhance ARV treatment maintenance and adherence, and to improve their physical and mental quality of life. It is also necessary to increase family support for HIV-infected drug users in the Chinese cultural context. One strategy could be to take advantage of the traditional concepts of Chinese family responsibilities by including family members in HIV and drug abuse treatment plans, with the goal of establishing a family alliance in response to the dual diagnoses of HIV and drug use. Working with family members to provide support for abstaining from drugs may in some instances be an effective way to restore family function. Additional research to explore family-based interventions to improve treatment outcomes is urgently needed.
Limitations
Participants were recruited from one HIV treatment site and referred by physicians and patients; thus, they were not from a random sample of HIV-infected IDUs in Hengyang. Hengyang is an inner city in south central China and Han is the predominant nationality, so caution should be used when considering applying this conceptual framework to other parts of China or to communities outside of China.
Clinical Considerations.
Discussing illegal drug use with the whole family rather than the patient alone and emphasizing the patient’s obligation to the family could be an effective strategy for stigma-reduction in Chinese HIV treatment settings.
Psychological counseling is urgently needed in clinics to alleviate the internalized stigma experienced by HIV-infected IDUs.
HIV-related education is needed to correct HIV-infected IDUs’ misbeliefs and to support them in their efforts to abstain from drugs, to enhance ARV treatment maintenance and adherence, and to improve their physical and mental quality of life.
Footnotes
Disclosures
The authors report no real or perceived vested interests that relate to this article (including relationships with pharmaceutical companies, biomedical device manufacturers, grantors, or other entities whose products or services are related to topics covered in this manuscript) that could be construed as a conflict of interest.
Contributor Information
Xianhong Li, School of Nursing of Central South University, Hunan, China.
Honghong Wang, School of Nursing of Central South University, Hunan, China.
Guoping He, School of Nursing of Central South University, Hunan, China.
Kristopher Fennie, Yale School of Nursing, New Haven, CT, USA.
Ann Bartley Williams, UCLA School of Nursing, Los Angeles, CA, USA.
References
- Aranda-Naranjo B. Quality of life in the HIV-positive patient: Implications and consequences. Journal of the Assocication of Nurses in AIDS Care. 2004;15 Suppl. 5:S20–S27. doi: 10.1177/1055329004269183. [DOI] [PubMed] [Google Scholar]
- Brown L, Macintyre K, Trujillo L. Interventions to reduce HIV/AIDS stigma: What have we learned? AIDS Education and Prevention. 2003;15(1):49–69. doi: 10.1521/aeap.15.1.49.23844. [DOI] [PubMed] [Google Scholar]
- Cao X, Sullivan SG, Xu J, Wu Z. Understanding HIV-related stigma and discrimination in a"blameless" population. AIDS Education and Prevention. 2006;18(6):518–528. doi: 10.1521/aeap.2006.18.6.518. [DOI] [PubMed] [Google Scholar]
- Chan KY, Stoove MA, Sringernyuang L, Reidpath DD. Stigmatization of AIDS patients: Disentangling Thai nursing students’ attitudes towards HIV/AIDS, drug use, commercial sex. AIDS and Behavior. 2008;12(1):146–157. doi: 10.1007/s10461-007-9222-y. [DOI] [PubMed] [Google Scholar]
- Chan KY, Yang Y, Zhang KL, Reidpath DD. Disentangling the stigma of HIV/AIDS from the stigmas of drugs use, commercial sex and commercial blood donation—a factorial survey of medical students in China. BMC Public Health. 2007;7(280):1–12. doi: 10.1186/1471-2458-7-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng R, Li J, Sringernyuang L, Zhang K. Drug abuse, HIV/AIDS and stigmatisation in a Dai community in Yunnan, China. Social Science & Medicine. 2007;64(8):1560–1571. doi: 10.1016/j.socscimed.2006.12.011. [DOI] [PubMed] [Google Scholar]
- Duffy L. Suffering, shame, and silence: The stigma of HIV/AIDS. Journal of the Association of Nurses in AIDS Care. 2005;16(1):13–20. doi: 10.1016/j.jana.2004.11.002. [DOI] [PubMed] [Google Scholar]
- Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: A review of HIV stigma mechanism measures. AIDS and Behavior. 2009;13(6):1160–1177. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ge Z. The traditional Chinese family oriented culture and its modern values. Zheng Gong Yan Jiu Dong Tai. 2009;2–3:9–10. [Google Scholar]
- Goffman E. Stigma: Notes on the management of spoiled identity. Englewood Cliffs, NJ: Prentice-Hall, Inc; 1963. [Google Scholar]
- Hutchinson S. Grounded theory: The method. In: Munhall PL, Boyd CO, editors. Nursing research: A qualitative perspective. Norwalk, CT: Appleton-Century-Crofts; 1986. pp. 111–130. [Google Scholar]
- Iwelunmor J, Airhihenbuwa C, Okoror T, Brown D, Belue R. Family systems and HIV/AIDS in South Africa. International Quarterly of Community Health Education. 2006–2007;27(4):321–335. doi: 10.2190/IQ.27.4.d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee RS, Kochman A, Sikkema KJ. Internalized stigma among people living with HIV-AIDS. AIDS and Behavior. 2002;6(4):309–319. [Google Scholar]
- Li L, Wu Z, Zhao Y, Lin C, Detels R, Wu S. Using case vignettes to measure HIV-related stigma among health professionals in China. International Journal of Epidemiology. 2007;36(1):178–184. doi: 10.1093/ije/dyl256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Wang H, Williams AB, He G. Stigma reported by people living with HIV in south central China. Journal of the Association of Nurses in AIDS Care. 2009;20(1):22–30. doi: 10.1016/j.jana.2008.09.007. [DOI] [PubMed] [Google Scholar]
- Maman S, Abler L, Parker L, Lane T, Chirowodza A, Ntogwisangu J, Fritz K. A comparison of HIV stigma and discrimination in five international stites: The influence of care and treatment resources in high prevalence settings. Social Science & Medicine. 2009;68(12):2271–2278. doi: 10.1016/j.socscimed.2009.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: A conceptual framework and implications for action. Social Science & Medicine. 2003;57(1):13–24. doi: 10.1016/s0277-9536(02)00304-0. [DOI] [PubMed] [Google Scholar]
- Prachakul W, Grant JS, Keltner NL. Relationships among functional social support, HIV-related stigma, social problem solving, and depressive symptoms in people living with HIV: A pilot study. Journal of the Association of Nurses in AIDS Care. 2007;18(6):67–76. doi: 10.1016/j.jana.2007.08.002. [DOI] [PubMed] [Google Scholar]
- Rao D, Kekwaletswe TC, Hosek S, Martinez J, Rodriguez F. Stigma and social barriers to medication adherence with urban youth living with HIV. AIDS Care. 2007;19(1):28–33. doi: 10.1080/09540120600652303. [DOI] [PubMed] [Google Scholar]
- Rao D, Pryor JB, Gaddist BW, Mayer R. Stigma, secrecy, and discrimination: Ethnic/racial differences in the concerns of people living with HIV/AIDS. AIDS and Behavior. 2008;12(2):265–271. doi: 10.1007/s10461-007-9268-x. [DOI] [PubMed] [Google Scholar]
- Stern PN. Grounded theory methodology: Its uses and processes. Image. 1980;12(7):20–23. doi: 10.1111/j.1547-5069.1980.tb01455.x. [DOI] [PubMed] [Google Scholar]
- Steward WT, Herek GM, Ramakrishna J, Bharat S, Chandy S, Wrubel J, Ekstrand ML. HIV-related stigma: Adapting a theoretical framework for use in India. Social Science & Medicine. 2008;67(8):1225–1235. doi: 10.1016/j.socscimed.2008.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang YL, Hao W. Improving drug addiction treatment in China. Addiction. 2007;102(7):1057–1063. doi: 10.1111/j.1360-0443.2007.01849.x. [DOI] [PubMed] [Google Scholar]
- Tang YL, Wiste A, Mao PX, Hou YZ. Attitudes, knowledge, and perceptions of Chinese doctors toward drug abuse. Journal of Substance Abuse Treatment. 2005;29(3):215–220. doi: 10.1016/j.jsat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Zuo Y. Chinese concept of ancestor and its modern explanation. Tribune of Study. 2008;24(9):57–60. [Google Scholar]