Abstract
Introduction:
Despite international efforts to implement smoking bans, several national legislations still allow smoking and recommend mechanical systems, such as ventilation and air extraction, to eliminate secondhand smoke (SHS) health-related risks. We aimed to quantify the relative contribution of mechanical systems and smoking bans to SHS elimination.
Methods:
A cross-sectional study was conducted in randomly selected establishments from 4 Mexican cities (3 with no ban). SHS exposure was assessed using nicotine passive monitors. Establishment characteristics, presence of mechanical systems, and enforcement of smoking policies were obtained through direct observation and self-report. Multilevel models were used to assess relative contributions to SHS reduction.
Results:
Compared with Mexico City, nicotine concentrations were 3.8 times higher in Colima, 5.4 in Cuernavaca, and 6.4 in Toluca. Mechanical systems were not associated with reduced nicotine concentrations. Concentration differences between cities were largely explained by the presence of smoking bans (69.1% difference reduction) but not by mechanical systems (−5.7% difference reduction).
Conclusions:
Smoking bans represent the only effective approach to reduce SHS. Tobacco control regulations should stop considering mechanical systems as advisable means for SHS reduction and opt for complete smoking bans in public places.
Introduction
Secondhand smoke (SHS) is a well-established health hazard, casually associated with cardiovascular disease and lung cancer (U.S. Department of Health and Human Services, 2006). SHS-related disease and financial burden are fundamental public health concerns reflected in the Framework Convention on Tobacco Control, advocated by 168 countries under the World Health Organization (WHO) sponsorship (WHO, 2003). SHS exposure elimination is considered an attainable primary prevention goal to reduce morbidity and mortality (WHO, 2008).
Efforts to eliminate the health risks associated to SHS can be classified into two categories. First, some countries have allowed mechanical systems, such as area separation, ventilation, and air extraction, in an attempt to reduce SHS exposure while still allowing smoking (WHO, 2009). These types of mechanical systems are advocated by tobacco companies and the hospitality sector as effective means to reduce SHS (Drope, Bialous, & Glantz, 2004). Some experimental research partially supports this claim. For instance, working under ideal circumstances, the most sophisticated smoking rooms, which combine several mechanical systems, are capable of eliminating 90% of SHS (Wagner et al., 2004). The remaining 10%, however, is still transferred to nonsmoking areas. Thus, while mechanical systems may significantly reduce SHS, they can not completely eliminate it.
Second, legislative action against tobacco smoke has increasingly gained public support and has led to substantial changes in policies around the world (WHO, 2008). Currently, 17 countries have followed 100% smoke-free environment policies, advocating complete smoking bans in all public places (WHO, 2009). The WHO position is grounded on evidence showing that no safe levels of exposure to SHS exist (U.S. Department of Health and Human Services, 2006); therefore, all residuals and leakage resulting from the insufficient capability of mechanical systems represent a significant health risk (WHO, 2007). Complete smoking bans have received support from the American Society of Heating, Refrigerating, and Air Conditioning Engineers, who state that no engineering approach is capable of eliminating the health risks associated with SHS once the smoke has been released to the environment (Samet et al., 2005).
While a vast body of literature has been dedicated to discussing mechanical systems versus smoking bans (Akbar-Khanzadeh, 2003; Cenko, Pisaniello, & Esterman, 2004; Dearlove, Bialous, & Glantz, 2002; Drope et al., 2004; Samet et al., 2005; WHO, 2008), no systematic attempt has been conducted to quantify the effectiveness of each approach under nonexperimental conditions. In February 2008, a total smoking ban in all public places, including restaurants and bars, was enforced in Mexico City (Gaceta Oficial del Distrito Federal, 2008). The rest of the country, however, still allowed indoor smoking. This setting provided a unique natural experiment to compare SHS exposure levels between environments enforcing 100% smoke-free policies and environments lacking such policies but where a variety of ventilation/air extraction devices were in use.
Within this context, we compared SHS concentrations in public places between Mexico City and three other Mexican capital cities without a smoking ban, examining the effect of mechanical systems versus smoking bans for SHS exposure control.
Methods
We selected four cities to represent different levels of active smoking as reported by the Global Youth Tobacco Survey, the only available source of State-level prevalence at the time (Reynales-Shigematsu, Rodriguez-Bolanos, Valdés-Salgado, Lazcano-Ponce, & Hernández-Avila, 2009). Mexico City, the country’s capital, represented a high active smoking prevalence (27.8%) city with a smoking ban in place. The other three cities had no smoking ban: Colima represented a low smoking prevalence city (11.5%); Cuernavaca, an intermediate (21.7%); and, Toluca, a high-prevalence city (27.5%).
Restaurant and bar censuses were obtained from municipal authorities. In Mexico City, more than 35,000 establishments were registered, so we restricted the selection process to establishments located in the historic district, a well-defined area with a high density of diverse establishments. In each city, we generated four strata by cross-classifying establishments by establishment type (bars or restaurants) and size (≤100 and >100 m2). In each stratum, we consecutively numbered the establishments and randomly invited 33 to participate, with a recruitment goal of 13 establishments per stratum, for a total of 208. Establishments were invited progressively with replacement as needed upon refusal to participate. All restaurants, bars, and restaurant–bars were included as long as they were established businesses with indoor customer seating areas, willing to participate, and located in a safe city area for the research team. Establishments were excluded if they were a fast-food chain, an unregistered establishment, or if they provided services for less than 8 hr a day.
Of 371 invited establishments, 219 agreed to participate (60%). SHS monitors were lost in 5 establishments, bringing the sample to 214 establishments. Participation rates by city were 44% for Mexico City, 60% for Toluca, 68% for Colima, and 70% for Cuernavaca. Research procedures were conducted with owner or legal representative authorization. Fieldwork was conducted from July to October 2008. All procedures were approved by the Committee for the Protection of Human Subjects of the University of Texas (HSC-SPH-07-0384) and by the Research, Ethical, and Biosecurity Committees of the National Institute of Public Health in Mexico (1456-6307-0).
Nicotine Exposure Measurements
Vapor-phase nicotine was selected to assess SHS exposure, since it is generated exclusively by smoking and inexpensive validated passive monitors were available in the country (Coghlin, Hammond, & Gann, 1989; Jaakkola & Jaakkola, 1997). Nicotine passive monitors, 37-mm clear plastic cassettes containing a sodium bisulfate–coated filter, were built at the National Institute of Public Health in Mexico (Hammond & Leaderer, 1987).
In each city, research teams were trained in the study procedures and testing methods by the principal investigator. Establishments were visited during the work shift with higher customer occupancy as reported by the manager. When available, one smoking and one nonsmoking area were selected for monitoring. Monitors were placed at the center of each designated area away from direct sources of ventilation, at least 50 cm away from any object that could block natural ventilation. Monitors were hung at a standard 2.3 m above the ground to avoid monitor loss or damage. Pilot studies were conducted to assure that monitors placed at 2.3 m reflected concentrations measured at respiratory height (1.6 m). Quality controls consisted of 10% duplicate monitors and 10% blank monitors.
Restaurants and bars have days and hours of no activity, so, to avoid previous dilution effects observed in approaches using weeklong monitoring (Barrientos-Gutierrez, Valdés-Salgado, Reynales-Shigematsu, Navas-Acien, & Lazcano Ponce, 2007), nicotine was monitored for the duration of the work shift with higher customer occupancy (mean monitoring time equals 8.5 hr, SD equals 2.2 hr). Then, all monitors were taken to a laboratory, disassembled, and their filters were placed in individual vials to be refrigerated at 3.3 °C until analyzed. Monitors were analyzed using a nitrogen-selective chromatograph according to standard protocols (Hammond & Leaderer, 1987). Detected nicotine was blank corrected and divided by the total volume of monitored air to obtain micrograms per cubic meter units. The limit of detection (LOD) was 0.03 μg/m3; concentrations under this level were imputed as half of the LOD.
Establishment Characteristics
Managers completed a questionnaire on the physical characteristics of their establishment. Information on type of establishment (bar or restaurant) obtained using the official census was corroborated or corrected using the manager’s report. Maximum occupancy was expressed as the maximum number of customers allowed in the establishment according to the establishment license. A walk-through was conducted to measure the establishment size with a digital laser distance meter and was categorized as ≤100 or >100 m2. The manager questionnaire also asked about customer’s mean age, percent male customers, and neighborhood socioeconomic status (SES) on a scale from 1 (the poorest) to 10 (the richest). We grouped scores 1–4 as low SES, 5–7 as medium SES, and 8–10 as high SES.
Mechanical Systems
All mechanical systems designed to extract, ventilate, or mobilize air, independently of whether they were installed in response to SHS concentrations or because of other reasons, were considered “mechanical systems.” Information on mechanical systems was obtained from the manager’s questionnaire. Presence of an air extraction system installed in the establishment was inquired with the question “In your establishment, is there an air extraction system in the customer area?” (answers “yes” and “no”); if unclear, managers were instructed to consider “extraction system” any mechanism that moved air from inside to outside the venue without recirculation. Information on the main ventilation system available was obtained with the question “In your establishment, what is the main ventilation system available?” (answers “fans,” “air conditioning,” and “natural”). Presence of ventilation and air extraction systems was corroborated by the research team during the walk-through. Given the variety of architectural designs, we also evaluated the number of complete walls in an area to account for natural ventilation. To do so, the percent of closed sides was calculated, dividing the number of complete walls over the total number of walls in the area (a wall was considered complete if no communication with the adjacent area existed after closing doors and windows).
Smoking Bans
Three variables were created to assess specific ways in which smoking bans may affect SHS levels. We assessed smoking policies toward (a) customers and (b) workers from two items of the manager’s questionnaire that asked whether customers or workers were not allowed to smoke in any area, allowed to smoke in designated areas, or allowed to smoke anywhere. To evaluate if these smoking ban policies were effectively implemented, we classified the smoking activity in the establishments during the walk-through and by the management’s report. An establishment was coded as “smoking” if no clear physical separation between areas existed and smoking areas were observed or reported, as “nonsmoking” if smoking was prohibited, and as “mixed” if a clear physical separation between smoking and nonsmoking areas was present.
Statistical Analysis
For the descriptive analysis, area nicotine concentrations were averaged by establishment so that each establishment contributed a single measurement. Since nicotine concentrations are known to follow a log-normal distribution in larger samples (Schorp & Leyden, 2002), nicotine concentrations were log transformed. Concentrations were described for the total sample, stratifying by establishment characteristics, mechanical systems, and smoking bans, using interquartile range, maximum and minimum. Descriptive statistics were obtained using Intercooled Stata10 (College Station, TX).
To evaluate which factors were associated with nicotine concentrations, multilevel models were fitted using the log-transformed nicotine concentration for each monitored area (Level 1), nested within establishments (Level 2). Models were built following the general formula:
 |
where ln(nicotine)ij represents nicotine concentrations in area i within establishment j, β0 + ui is the intercept for establishment j, β1–3 are the coefficients for each city as compared with Mexico City, βm are the coefficients for establishment characteristics, βn are the coefficients for the mechanical systems, β0 are the coefficients for the three proposed smoking bans, ϵij is the error at area level (Level 1), and ui is the error at the establishment level (Level 2). Linear regression coefficients were back transformed to estimate exposure ratios.
The relative contribution of mechanical systems and smoking bans to SHS control was quantified assessing the influence of each set of variables over differences in nicotine concentrations between cities. We assumed that these differences were at least partially the result of differences in establishment characteristics, mechanical systems, and smoking bans. Therefore, we started by fitting a model containing only the dummy variables for cities to define a baseline difference. Then, we separately added each group of variables to independently assess their effect over differences between cities. Finally, we fitted a saturated model including all variables and applied a backward selection strategy, keeping variables with p value <.1 and that did not change the coefficients for city variables more than 10%. All regression coefficients were back transformed to represent exposure ratios. Percent change in exposure ratios after each adjustment was computed by (exposure ratioModel a − exposure ratioModel b)/(exposure ratioModel a). All p values were two tailed, and p values <.05 were considered to indicate statistical significance. Multilevel models were computed using MLwiN 2.10 (Bristol, UK, 2009).
Results
Table 1 shows the study sample characteristics. Bars and restaurants were similarly distributed across cities, although Colima had slightly more bars than restaurants. Regarding mechanical systems, Mexico City had the largest proportion of establishments with air extraction systems (57.6%), followed by Toluca. In Colima and Cuernavaca, establishments had fans more frequently than in Mexico City and Toluca, but AC was more frequent in Mexico City (28.8%). As regards to ban mechanism, in Mexico City, 86.5% of establishments were nonsmoking, a very large proportion compared with Toluca (25%), Colima (11.5%), or Cuernavaca (6.1%). Establishments enforced nonsmoking policies more frequently for workers (60%) than for customers (32%).
Table 1.
Sample Description in Four Mexican Cities, Mexico, 2008
| Total (n = 214) | Mexico City (n = 52) | Colima (n = 61) | Cuernavaca (n = 49) | Toluca (n = 52) | |
| Establishment characteristics | |||||
| Type of establishment (n, %) | |||||
| Restaurant | 119 (55.6) | 33 (63.4) | 28 (45.9) | 30 (61.2) | 28 (53.8) |
| Bar | 95 (44.3) | 19 (36.5) | 33 (54.1) | 19 (38.7) | 24 (46.1) |
| Size (n, %) | |||||
| ≤100 m2 | 111 (51.9) | 25 (48.1) | 29 (47.5) | 22 (44.9) | 35 (67.3) |
| >100 m2 | 103 (48.1) | 27 (51.9) | 32 (52.4) | 27 (55.1) | 17 (32.6) |
| Maximum occupancy (, SD) | 108.2 (103.9) | 100.7 (65.1) | 133.5 (130.7) | 121.5 (122.2) | 73 (37.4) |
| Customer age (, SD) | 35.2 (8.1) | 38.4 (7.4) | 34.7 (8.2) | 35.2 (7.9) | 33.9 (8.4) |
| Percent male customers (, SD) | 62.3 (17.2) | 66.3 (14.4) | 62.2 (14.9) | 60.4 (17.4) | 60.8 (19.9) |
| Socioeconomic status neighborhood (n, %) | |||||
| Low | 77 (35.9) | 27 (51.9) | 20 (32.8) | 18 (36.7) | 12 (23) |
| Medium | 117 (54.7) | 24 (46.1) | 30 (49.1) | 28 (57.1) | 35 (67.3) |
| High | 20 (9.4) | 1 (1.9) | 11 (18) | 3 (6.1) | 5 (9.6) |
| Mechanical systems | |||||
| Air extraction system (n, %) | |||||
| No | 161 (72.2) | 30 (57.6) | 53 (86.8) | 41 (83.6) | 37 (71.1) |
| Yes | 53 (24.7) | 22 (42.3) | 8 (13.1) | 8 (16.3) | 15 (28.9) |
| Ventilation system (n, %) | |||||
| Natural | 79 (36.9) | 23 (44.2) | 11 (18) | 13 (26.5) | 32 (61.5) |
| Fan | 95 (44.3) | 14 (26.9) | 38 (80.3) | 26 (53.0) | 17 (32.6) |
| AC | 40 (18.6) | 15 (28.8) | 12 (19.6) | 10 (20.4) | 3 (5.8) |
| Percent closed sides (n, %) | |||||
| <100% | 84 (39.3) | 33 (64.5) | 18 (29.5) | 27 (55.1) | 6 (11.6) |
| 100% | 130 (60.7) | 19 (36.5) | 43 (70.5) | 22 (44.9) | 46 (88.4) |
| Smoking bans | |||||
| Smoking policy for customers (n, %) | |||||
| No smoking | 68 (31.7) | 45 (86.5) | 7 (11.5) | 3 (6.1) | 13 (25) |
| Smoking in specific areas | 51 (23.8) | 6 (11.5) | 17 (27.8) | 6 (12.2) | 22 (42.3) |
| Smoking anywhere | 95 (44.3) | 1 (1.9) | 37 (60.6) | 40 (81.6) | 17 (32.6) |
| Smoking policy for workers (n, %) | |||||
| No smoking | 127 (59.3) | 43 (82.6) | 26 (42.6) | 27 (55.1) | 31 (59.6) |
| Smoking in specific areas | 68 (31.7) | 9 (17.3) | 28 (45.9) | 14 (28.5) | 17 (32.6) |
| Smoking anywhere | 19 (8.9) | 0 (0) | 7 (11.5) | 8 (16.3) | 4 (7.7) |
| Effectively implemented smoking ban policies (n, %) | |||||
| All nonsmoking | 81 (37.9) | 49 (94.2) | 12 (19.6) | 4 (8.2) | 16 (30.7) |
| All smoking | 111 (51.2) | 1 (1.9) | 42 (68.8) | 40 (81.6) | 28 (53.8) |
| Mixed | 22 (10.3) | 2 (3.8) | 7 (11.5) | 5 (10.2) | 8 (15.4) |
Median nicotine concentrations by sample characteristics are presented in Table 2. Mexico City (1 μg/m3) had the lowest concentrations observed, followed by Colima (2.6 μg/m3), Cuernavaca (3.1 μg/m3), and Toluca (3.7 μg/m3). As for mechanical systems, places with air extraction systems had higher concentrations (3.8 μg/m3) than those without them (1.9 μg/m3). Establishments with fans (2.9 μg/m3) or air conditioning systems (2.5 μg/m3) had higher nicotine concentrations than places with natural ventilation (1.6 μg/m3). Places with less than 100% of closed sides had lower concentrations (1.5 μg/m3) than those completely enclosed (2.7 μg/m3). Regarding smoking bans, places completely banning smoking showed lower concentrations than those with unrestricted smoking (1.0 vs. 5.2 μg/m3 for customer and 1.5 vs. 6.2 μg/m3 for worker’s ban). In a similar manner, places having only nonsmoking areas were less polluted (1.0 μg/m3) than those with smoking or mixed areas (5.1 and 2.5 μg/m3 respectively).
Table 2.
Averaged Establishment Nicotine Exposure (in micrograms per cubic meter), Mexico, 2008
| Nicotine centile distribution |
|||||
| Min | 25 | Median | 75 | Max | |
| City | |||||
| Mexico City | <LD | 0.6 | 1.0 | 2.5 | 9.1 |
| Colima | 0.5 | 1.0 | 2.6 | 5.7 | 42.2 |
| Cuernavaca | 0.6 | 0.9 | 3.1 | 12.8 | 75.6 |
| Toluca | 0.6 | 1.5 | 3.7 | 14.6 | 118.3 |
| Mechanical systems | |||||
| Air extraction system | |||||
| No | <LD | 0.9 | 1.9 | 5.7 | 118.3 |
| Yes | <LD | 1.1 | 3.8 | 14.0 | 96.8 |
| Ventilation system | |||||
| Natural | <LD | 0.8 | 1.6 | 5.7 | 83.6 |
| Fan | 0.5 | 1.1 | 2.9 | 10.2 | 118.3 |
| AC | <LD | 0.7 | 2.5 | 9.4 | 96.8 |
| Percent closed sides | |||||
| <100% | <LD | 0.8 | 1.5 | 6.2 | 118.3 |
| 100% | <LD | 1.0 | 2.7 | 7.9 | 96.8 |
| Smoking bans | |||||
| Smoking policy for customers | |||||
| No smoking | <LD | 0.6 | 1.0 | 2.4 | 9.1 |
| Smoking in specific areas | 0.5 | 0.9 | 1.9 | 6.3 | 74.1 |
| Smoking anywhere | 0.5 | 1.7 | 5.2 | 15.0 | 118.3 |
| Smoking policy for workers | |||||
| No smoking | <LD | 0.8 | 1.5 | 3.8 | 74.1 |
| Smoking in specific areas | 0.5 | 1.2 | 5.2 | 14.6 | 118.3 |
| Smoking anywhere | 0.6 | 2.3 | 6.2 | 21.0 | 83.6 |
| Effectively implemented smoking ban policies | |||||
| All nonsmoking | <LD | 0.6 | 1.0 | 2.0 | 73.2 |
| All smoking | 0.5 | 7 | 5.1 | 14.7 | 118.3 |
| Mixed | 0.5 | 0.9 | 2.5 | 8.2 | 54.7 |
Note. <LOD = under limit of detection (0.03 μg/m3).
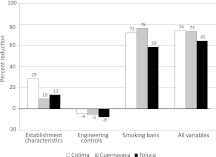
Table 3 shows the exposure ratios estimated from the regression models, and Figure 1 shows the percent change in the exposure ratios after each adjustment. In the unadjusted models, exposure ratios were significantly higher in Colima (3.8 times higher), Cuernavaca (5.4 times), and Toluca (6.4 times) when compared with Mexico City. After adjusting for establishment characteristics, the exposure ratios were slightly reduced (17.3%, average change). Establishment type and customer’s age were the only two establishment characteristics associated with nicotine concentrations. Adjusting in turn for mechanical system variables, nicotine concentration differences between Mexico City and all other cities increased (−5.7% average change). Establishments with air extraction systems had 1.88 times higher concentrations than their counterparts. Adjusting in turn for smoking bans, differences between cities became nonstatistically significant (69.1% average change) except for Toluca. All three ban variables were associated with nicotine concentration levels. The final model included type of establishment, customer age, smoking policy toward customers, and effectively implemented smoking ban policies in the areas. In the final model, differences between cities were nonstatistically significant (70.7% average change) except for Toluca.
Table 3.
Environmental Nicotine ER in Restaurants and Bars, Mexico, 2008
| Adjusted for |
||||||||||
| Unadjusted |
Establishment characteristics |
Mechanical systems |
Smoking bans |
All |
||||||
| ER (95% CI) | p Value | ER (95% CI) | p Value | ER (95% CI) | p Value | ER (95% CI) | p Value | ER (95% CI) | p Value | |
| State (Mexico City, ref) | ||||||||||
| Colima | 3.82 (2.20, 6.64) | <.001 | 2.72 (1.67, 4.45) | <.001 | 3.99 (2.20, 7.23) | <.001 | 1.07 (0.55, 2.08) | <.001 | 0.99 (0.54, 1.81) | .002 |
| Cuernavaca | 5.43 (3.03, 9.72) | 4.90 (2.97, 8.08) | 5.71 (3.17, 10.28) | 1.28 (0.61, 2.69) | 1.44 (0.74, 2.80) | |||||
| Toluca | 6.40 (3.61, 11.35) | 5.54 (3.32, 9.26) | 6.89 (3.7, 12.82) | 2.64 (1.40, 5.00) | 2.27 (1.27, 4.05) | |||||
| Establishment characteristics | ||||||||||
| Type of establishment (Restaurant, ref) | ||||||||||
| Bar | 4.94 (3.35, 7.28) | <.001 | 4.21 (2.80, 6.31) | <.001 | 3.77 (2.67, 5.31) | <.001 | ||||
| Size (≤100 m2, ref) | ||||||||||
| >100 m2 | 0.84 (0.54, 1.31) | .440 | 1.17 (0.76, 1.79) | .471 | ||||||
| Maximum occupancy | 1.00 (1.00, 1.00) | .077 | 1.00 (1.00, 1.00) | .317 | ||||||
| Customer’s age | 0.95 (0.93, 0.98) | <.001 | 0.98 (0.96, 1.00) | .067 | 0.98 (0.96, 1.00) | .046 | ||||
| Percent male customers | 1.01 (1.00, 1.02) | .143 | 1.00 (0.99, 1.02) | .505 | ||||||
| Socioeconomic status neighborhood (Low, ref) | ||||||||||
| Medium | 1.01 (0.63, 1.62) | .913 | 0.89 (0.61, 1.29) | .819 | ||||||
| High | 1.18 (0.53, 2.65) | 0.87 (0.45, 1.68) | ||||||||
| Mechanical systems | ||||||||||
| Air extraction system (No, ref) | ||||||||||
| Yes | 1.23 (0.74, 2.05) | .424 | 1.87 (1.09, 3.22) | .023 | ||||||
| Ventilation system (Natural, ref) | ||||||||||
| Fan | 1.77 (1.09, 2.88) | .041 | 1.55 (0.97, 2.46) | .099 | ||||||
| AC | 1.04 (0.56, 1.92) | 0.96 (0.49, 1.87) | ||||||||
| Percent closed sides (<100%, ref) | ||||||||||
| 100% | 1.53 (0.98, 2.39) | .061 | 0.95 (0.61, 1.48) | .821 | ||||||
| Smoking bans | ||||||||||
| Smoking policy for customers (No smoking, ref) | ||||||||||
| Smoking in specific areas | 2.77 (1.64, 4.68) | <.001 | 1.12 (0.59, 2.14) | .044 | 1.38 (0.79, 2.42) | .037 | ||||
| Smoking anywhere | 6.28 (3.99, 9.88) | 2.17 (1.03, 4.56) | 2.23 (1.18, 4.21) | |||||||
| Smoking policy for workers (No smoking, ref) | ||||||||||
| Smoking in specific areas | 3.04 (1.93, 4.79) | <.001 | 1.76 (1.14, 2.73) | .039 | ||||||
| Smoking anywhere | 4.04 (1.91, 8.54) | 1.58 (0.78, 3.22) | ||||||||
| Effectively implemented smoking ban policies (All nonsmoking, ref) | ||||||||||
| All smoking | 5.59 (3.69, 8.48) | <.001 | 2.28 (1.21, 4.29) | .041 | 1.92 (1.09, 3.37) | .020 | ||||
| Mixed | 2.87 (1.50, 5.50) | 1.80 (0.88, 3.70) | 2.38 (1.26, 4.50) | |||||||
| Variance components (SE) | ||||||||||
| Workplace-level variance Ujk | 2.191 (0.299) | <.001 | 1.082 (0.207) | .001 | 1.609 (0.245) | <.001 | 1.368 (0.227) | <.001 | 0.906 (0.197) | <.001 |
| Individual-level variance eijk | 0.524 (0.158) | 0.512 (0.152) | 0.502 (0.150) | 0.506 (0.151) | 0.522 (0.155) | |||||
Note. ER = exposure ratios.
Figure 1.
Percent change in exposure ratios between each city and Mexico City after adjusting for establishment characteristics, engineering controls, smoking bans, and for all variables at the same time (compared with unadjusted exposure ratios). For instance, after adjusting for establishment characteristics, the difference in nicotine concentrations between Colima and Mexico City decreased by 29%.
Discussion
Taking advantage of a natural experiment occurring in Mexico, we found that median nicotine concentrations in three selected cities with no smoking ban were 3.8–6.4 times higher than in Mexico City where a smoking ban had been implemented. Whereas after adjusting for potential smoking bans, the nicotine concentration differences between cities were mostly flattened, except for Toluca, adjusting for mechanical systems did not reduce, and even slightly increased, the differences in nicotine concentrations. Our findings provide the first real-life quantification of the relative contributions to SHS reduction of mechanical systems and smoking ban policies, representing the first large-scale measurement of their effectiveness. We found that the only approach to satisfactorily control SHS exposure is an effective application of smoking ban policies. Neither wall design, ventilation type, or air extraction had a major impact in reducing nicotine concentrations. Furthermore, establishments with some mechanical systems, such as fans or air extraction systems, showed higher concentrations than those without them.
Tobacco companies have frequently proposed air extraction and ventilation systems as adequate approaches to reduce or control SHS (Drope et al., 2004), despite repeated warnings by WHO regarding the ineffectiveness of such devices to eliminate SHS-associated health risks (WHO, 2007). We found the relative contribution of ventilation and air extraction systems to SHS reduction to be negligible compared with reductions attained from smoking bans. Furthermore, ventilation and air extraction systems could be getting installed more frequently in highly polluted establishments, or could help to create a false sense of security leading to increased consumption, explaining the higher concentrations observed in places with these mechanical devices. This finding is of interest since ventilation, air extraction, and area separation are still portrayed as adequate measures to eliminate or control SHS exposure, echoing in recently approved legislative efforts to eliminate SHS (Cámara de Senadores de los Estados Unidos Mexicanos, 2008).
Our findings suggest that in restaurants and bars, smoking ban policies are an effective tool to reduce SHS. WHO considers smoking bans to be the only effective way of reducing SHS exposure (WHO, 2007). Around the world, reductions in SHS concentrations have been observed after implementation of smoking ban policies. For instance, an 83% reduction in nicotine levels was reported in Ireland after the enactment of the smoke-free law (Mulcahy, Evans, Hammond, Repace, & Byrne, 2005), a 94% reduction in urinary cotinine was observed among non-casino hospitality workers in New York following the ban (Abrams et al., 2006), and a 98% reduction in environmental nicotine was observed in Norway after the ban (Ellingsen et al., 2006). In our study, Mexico City had the highest prevalence of nonsmoking establishments (94.2%) and the highest prevalence of nonsmoking policies toward customers (86.5%) and workers (82.6%). Thus, it is reasonable to assume that lower concentrations found in Mexico City are a direct consequence of the smoking ban, particularly considering that Mexico City has the highest active smoking prevalence in Mexico. The reduction of differences between Mexico City and all other cities, observed after adjusting for the smoking bans, suggests that those differences were the result of the ban and not the effect of differences in establishment characteristics between cities or the effect of mechanical devices to control SHS.
Some methodological issues need to be taken into account when interpreting our findings. Although we did not have preban exposure data to examine changes in nicotine concentrations in Mexico City, the setting of this natural experiment provided a useful venue for comparisons. Considering geographic, demographic, and smoking characteristics, it would have been reasonable to expect Mexico City concentrations to be at least as high as Toluca if the ban had not been enacted. Nicotine was measured directly as opposed to self-reported work exposure, providing a standardized objective measurement of exposure. Measurements were obtained during the highest occupancy shift, representing a worst-case exposure scenario. We chose this monitoring approach rather than week monitoring to avoid the dilution effect previously observed in studies using weeklong SHS exposure (Barrientos-Gutierrez et al., 2007; Navas-Acien et al., 2004). Highest occupancy shift measures provide a good estimation of what restaurant and bar workers experience 2–3 days out of their workweek, representing a fairly frequent degree of exposure. Data on ventilation and air extraction were limited to presence/absence of the equipment and therefore does not reflect actual use. A more refined measure should be used in future studies, evaluating time of activity of the equipment. Few SHS exposure evaluation studies have been conducted in random samples of establishments, relying more often on small convenience samples. Random samples obtained from governmental registries should provide a more representative study population.
Our findings suggest that the implementation of smoking bans has the potential to significantly reduce SHS concentrations in restaurants and bars, even in a highly complex and populated city such as Mexico City. In contrast, mechanical systems did not reduce SHS concentrations. This evidence is critical to advancing legislative actions in countries where indoor smoking is still allowed in the presence of mechanical systems. Tobacco control regulations should stop considering mechanical systems as advisable means for SHS reduction and opt for complete smoking bans in public places.
Funding
Study funded by the National Council for Science and Technology in Mexico (Grant 69760-S0008-2007-1), the National Institute for Occupational and Environmental Health Centers for Disease Control and Prevention to the Southwest Center for Occupational and Environmental Health at the University of Texas School of Public Health (Grant T42 OH008421), and the National Institute of Environmental Health Sciences to the Center for Research in Environmental Diseases at the University of Texas MD Anderson Cancer Center (Grant ES007784).
Declaration of Interests
None declared.
Acknowledgments
We are thankful for the logistic support provided by the Federal Health Secretary and the Health Secretaries from the State of Colima, State of Morelos, State of Mexico, and Mexico City. Critical local support was provided by the State Councils against Addictions from Colima and Morelos, and the Mexiquense Institute against Addictions. We remain grateful for the work and commitment of our field coordinators (Esteban Cortes, Benjamin Morales, Alberto Terrón, and Carmen Valladolid) and laboratory personnel (Abigail Flores, Leopoldo Parada, Lisset Orgaz). *Ronald “Ron” Baxter Harrist deceased on June 19, 2010.
References
- Abrams SM, Mahoney MC, Hyland A, Cummings KM, Davis W, Song L. Early evidence on the effectiveness of clean indoor air legislation in New York State. American Journal of Public Health. 2006;96:296–298. doi: 10.2105/AJPH.2004.055012. doi:AJPH.2004.055012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akbar-Khanzadeh F. Exposure to environmental tobacco smoke in restaurants without separate ventilation systems for smoking and nonsmoking dining areas. Archives of Environmental Health. 2003;58:97–103. doi: 10.3200/AEOH.58.2.97-103. doi:10.3200/AEOH.58.2.97-103. [DOI] [PubMed] [Google Scholar]
- Barrientos-Gutierrez T, Valdés-Salgado R, Reynales-Shigematsu LM, Navas-Acien A, Lazcano Ponce EC. Involuntary exposure to tobacco smoke in public places in Mexico. Salud Pública De México. 2007;43(Suppl. 2):S205–S212. doi: 10.1590/s0036-36342007000800010. doi:10.1590/S0036-36342007000800010. [DOI] [PubMed] [Google Scholar]
- Cámara de Senadores de los Estados Unidos Mexicanos. Ley General Para El Control Del Tabaco. Vol. 115. Gaceta Oficial del Senado de la República; 2008. Retrieved from http://www.senado.gob.mx/gace.php?sesion=2008/02/26/1. [Google Scholar]
- Cenko C, Pisaniello D, Esterman A. A study of environmental tobacco smoke in south Australian pubs, clubs and cafes. International Journal of Environmental Health Research. 2004;14:3–11. doi: 10.1080/09603120310001633903. doi:10.1080/09603120310001633903. [DOI] [PubMed] [Google Scholar]
- Coghlin J, Hammond SK, Gann PH. Development of epidemiologic tools for measuring environmental tobacco smoke exposure. American Journal of Epidemiology. 1989;130:696–704. doi: 10.1093/oxfordjournals.aje.a115391. [DOI] [PubMed] [Google Scholar]
- Dearlove JV, Bialous SA, Glantz SA. Tobacco industry manipulation of the hospitality industry to maintain smoking in public places. Tobacco Control. 2002;11:94–104. doi: 10.1136/tc.11.2.94. doi:10.1136/tc.11.2.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drope J, Bialous SA, Glantz SA. Tobacco industry efforts to present ventilation as an alternative to smoke-free environments in North America. Tobacco Control. 2004;13(Suppl. 1):i41–i47. doi: 10.1136/tc.2003.004101. doi:10.1136/tc.2003.004101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellingsen DG, Fladseth G, Daae HL, Gjølstad M, Kjærheim K, Skogstad M, et al. Airborne exposure and biological monitoring of bar and restaurant workers before and after the introduction of a smoking ban. Journal of Environmental Monitoring. 2006;8:362–368. doi: 10.1039/b600050a. doi:10.1039/B600050A. [DOI] [PubMed] [Google Scholar]
- Gaceta Oficial del Distrito Federal. Decreto Por El Que Se Reforman, Adicionan y Derogan La Ley De Proteccion a La Salud De Los no Fumadores Del Distrito Federal y La Ley Para El Funcionmiento De Establecimientos Mercantiles Del Distrito Federal. 2008. Retrieved from http://www.asambleadf.gob.mx/al/pdf/010803000036.pdf. [Google Scholar]
- Hammond SK, Leaderer BP. A diffusion monitor to measure exposure to passive smoking. Environmental Science & Technology. 1987;21:494–497. doi: 10.1021/es00159a012. doi: 10.1021/es00159a012. [DOI] [PubMed] [Google Scholar]
- Jaakkola MS, Jaakkola JJ. Assessment of exposure to environmental tobacco smoke. European Respiratory Journal: Official Journal of the European Society for Clinical Respiratory Physiology. 1997;10:2384–2397. doi: 10.1183/09031936.97.10102384. doi:10.1183/09031936.97.10102384. [DOI] [PubMed] [Google Scholar]
- Mulcahy M, Evans DS, Hammond SK, Repace JL, Byrne M. Secondhand smoke exposure and risk following the Irish smoking ban: An assessment of salivary cotinine concentrations in hotel workers and air nicotine levels in bars. Tobacco Control. 2005;14:384–388. doi: 10.1136/tc.2005.011635. doi:10.1136/tc.2005.011635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navas-Acien A, Peruga A, Breysse P, Zavaleta A, Blanco-Marquizo A, Pitarque R, et al. Secondhand tobacco smoke in public places in Latin America, 2002–2003. Journal of the American Medical Association. 2004;291:2741–2745. doi: 10.1001/jama.291.22.2741. doi:10.1001/jama.291.22.2741. [DOI] [PubMed] [Google Scholar]
- Reynales-Shigematsu LM, Rodriguez-Bolanos R, Valdés-Salgado R, Lazcano-Ponce EC, Hernández-Avila M. Encuesta de tabaquismo en jovenes: Analisis descriptivo 2003, 2005, 2006, 2008. Primera edicion. ed. Cuernavaca, Mexico: Instituto Nacional de Salud Publica de Mexico; 2009. Retrieved from http://www.insp.mx/produccion-editorial/654-encuesta-de-tabaquismo-en-jovenes-en-mexico.html. [Google Scholar]
- Samet J, Bohanon H, Jr., Coultas D, Houston T, Persily A, Schoen L, et al. ASHRAE position document on environmental tobacco smoke. American Society of Heating, Refrigerating and Air-Conditioning Engineers. 2005 Retrieved from http://www.ashrae.org/content/ASHRAE/ASHRAE/ArticleAltFormat/20058211239_347.pdf. [Google Scholar]
- Schorp MK, Leyden DE. Distribution analysis of airborne nicotine concentrations in hospitality facilities. Environment International. 2002;27:567–578. doi: 10.1016/s0160-4120(01)00110-6. doi:10.1016/S0160-4120(01)00110-6. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. The health consequences of involuntary exposure to tobacco smoke: A report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services; 2006. Retrieved from http://www.surgeongeneral.gov/library/secondhandsmoke/ [Google Scholar]
- Wagner J, Sullivan D, Faulkner D, Fisk W, Alevantis L, Dod R, et al. Environmental tobacco smoke leakage from smoking rooms. Journal of Occupational and Environmental Hygiene. 2004;1:110–118. doi: 10.1080/15459620490275902. doi:10.1080/15459620490275902. [DOI] [PubMed] [Google Scholar]
- World Health Organization. WHO framework convention on tobacco control (WHO FCTC) Geneva, Switzerland: 2003. Retrieved from http://www.who.int/fctc/en/ [Google Scholar]
- World Health Organization. Policy recommendations on protection from exposure to second-hand tobacco smoke. Geneva, Switzerland: 2007. Retrieved from http://www.who.int/tobacco/resources/publications/wntd/2007/pol_recommendations/en/index.html. [Google Scholar]
- World Health Organization. WHO report on the global tobacco epidemic, 2008: The MPOWER package. Geneva, Switzerland: 2008. Retrieved from http://www.who.int/tobacco/mpower/mpower_report_full_2008.pdf. [Google Scholar]
- World Health Organization. WHO report on the global tobacco epidemic, 2009: Implementing smoke-free environments. Geneva, Switzerland: 2009. Retrieved from http://www.who.int/tobacco/mpower/en/ [Google Scholar]