Abstract
Objective
Response to treatment in child and adolescent affective disorders is variable, with limited ability of any one treatment to improve outcome across patients. Unfortunately, we know little about the factors that explain this variability in treatment response. Individual differences in the social and affective dynamics of daily life could help to elucidate the characteristics of youth who respond to treatment.
Methods
We used ecological momentary assessment of negative affect, positive affect, and companions in natural settings over 4 days in a sample of young people with depressive and anxiety disorders who participated in an 8-week open trial of cognitive behavioral therapy (CBT), selective serotonin reuptake inhibitors (SSRIs), or a combination of the two. Clinicians rated participants' clinical severity at five time points, and participants reported their symptoms before and after treatment. Latent growth curve models were used to predict rate of change in clinical severity from pretreatment affect in natural settings.
Results
Participants with high positive affect (PA), low negative affect (NA), and a high PA:NA ratio at baseline had lower severity, depressive symptoms, and anxiety symptoms at the end of treatment. Lower posttreatment symptoms were associated with spending more time with fathers and less time with peers before treatment. Although baseline affect was not associated with initial symptom severity, high NA and low PA:NA at baseline were related to slower rate of decline of severity during treatment. When baseline symptoms were included in models, NA and PA:NA predicted rate of decline in severity during treatment, whereas self-reported depressive and anxiety symptoms at baseline did not.
Conclusion
A more typical profile of baseline affective functioning in natural settings—that is, lower NA and higher PA—and time with fathers, could provide a foundation for treatment response in children and adolescents. Affective and social dynamics in natural settings could ultimately help investigate which young people might benefit from current treatments.
Introduction
Response to treatment in child and adolescent depression is variable (e.g., Kennard et al. 2006), and we know little about the factors that explain that variability. Ideally, understanding individual differences that predict treatment response can serve to enhance the application of treatments for depression. A critical first step in investigating treatment response is the examination of candidate individual differences that predict treatment response.
Because depression is considered a disorder of affect regulation (Gross and Muñoz 1995; Forbes and Dahl 2005), variability in affective experience among youth with depression could be a particularly important factor to investigate in association with treatment response. Affective style is conceptualized as a key individual difference contributing to the development and maintenance of depression (Davidson 2000), with characteristics such as the experience of positive affect (PA) and negative affect (NA) and the flexibility of affective response to challenging events proposed as being important to healthy affective functioning. Affective characteristics such as high PA or low NA could have relevance for response to treatment in children and adolescents with depression, because these characteristics could indicate a more adaptive pattern of affective style that could promote improvement (Davidson 2004). For example, research on affective factors in clinical course indicates that experiencing a higher level of PA during a depressive episode appears to protect adolescents from recurrence (Joiner et al. 2002). Given the between-person variability in NA and PA among young people with depression (e.g., Silk et al., 2011), the experience of affect during a depressive episode could provide meaning for the course and treatment of depression.
Affective experience in daily life could be especially reflective of affective style and affective functioning in children and adolescents with depression. It can indicates their typical response to real-world events as they occur, providing an important description of momentary affective processes. To date, studies have traditionally relied on retrospective measures of affect administered in the laboratory. A few recent studies have focused on affective experience in natural settings, for example by using experience sampling techniques, and findings have revealed compelling information about the affective experience of young people with depression. For example, our research on affective experience in natural settings suggests that young people with depression experience higher levels and greater lability of NA (Silk et al. 2011).
Although associated with the experience of depression, high NA and low PA in natural environments may not simply be proxies for depressive symptoms or clinical severity. Rather, these affective characteristics reflect a variety of affective and motivational states. They are likely related to a variety of factors, including stable tendencies such as affective style, acute responses to proximally occurring events, and cognitive factors such as appraisal of events. NA and PA in natural settings can include adaptive responses, whereas depressive symptoms reflect maladaptive responses that interfere with functioning. In addition, depressive symptoms include cognitive and vegetative features in addition to affective features. For example, a longitudinal study of adolescents' NA, PA, and depressive symptoms in natural settings indicated that the three types of affect had distinct patterns of stability and change with development (Weinstein et al. 2007). The dynamics of daily affect such as peak intensity, mean level of NA and PA, and fluctuations in NA and PA can be quite different from the more global mood disturbance of depression. The assessment of depressive symptoms and momentary affect also highlights the distinctions between them: Whereas depression is measured through retrospective report of mood, cognition, and behavior in a clinical setting, measurement of NA and PA in daily life occurs through momentary report in natural contexts.
Social context in natural settings in children and adolescents with depression may have value for predicting treatment response. The development of depression during adolescence is proposed to have a close link to changes in social demands and experiences during this developmental period (Davey et al. 2008). Developmental scientists conceptualize affect as having a social function (Campos et al. 1994), and the affective experiences of children and adolescents with depression may therefore fluctuate especially closely with their social experiences. For example, adolescents with depression report experiencing sensitivity to social rejection and distress in social contexts (Larson et al. 1990). Also, isolation from peer cliques is associated with increasing depressive symptoms during adolescence (Witvliet et al. 2010). Time in social contexts could influence treatment response in young people through processes such as the quality of their relationships or their capacity to engage others for support. In addition, peer and family contexts could have relevance for treatment response, as youth with depression exhibit differences from healthy youth in their social behavior in both family contexts (Sheeber et al. 2009) and peer contexts (Rudolph et al. 1997). Whereas interactions with peers are known to have increasing value during adolescence (Larson and Richards 1991), relationships with parents remain important to adolescents' affective functioning (Morris et al. 2007). Notably, peer social support does not always serve a protective function for depression in young people (Auerbach et al. 2011; Desjardins and Leadbeater 2011), and factors such as co-rumination can link peer social contexts with depressive and anxiety symptoms (Tompkins et al. 2011). Family support is stably related to PA and NA in natural settings across adolescent development (Weinstein et al. 2006), and support from fathers in particular has been observed as buffering the association between social stress and depressive symptoms over time (Desjardins and Leadbeater 2011). Although the literature on peer and family contributions to adolescent depression includes mixed findings on the respective contributions of these two types of companions, spending time with caring family members or peers could serve as a protective factor by supporting healthy affective experience and promoting response to treatment.
In addition, understanding the dynamics of affect and social context in daily life in youth with anxiety is relevant to understanding the treatment of depression in children and adolescents. Broadly, conceptual models have depicted both depression and anxiety as characterized by high levels of NA (Fowles 1988; Clark and Watson 1991), and both types of disorders are considered to involve disruption of affect regulation. Developmentally, it is valuable to consider anxiety and depression together because the two types of affective problems tend to have onset near adolescence and seem to have mutual influence. That is, not only are the two types of disorder frequently comorbid during adolescence (Kessler et al. 2001), but there is a tendency for each to be preceded by the other (Kovacs et al. 1989; Moffitt et al. 2007). Although there have been challenges to the heretofore prevailing view that anxiety disorders tend to precede depressive disorders, longitudinal findings on the two types of symptoms indicate that anxiety symptoms contribute to changes in depressive symptoms even when previous depressive symptoms are taken into account (Keenan et al. 2009). Given these various forms of overlap between depression and anxiety, developmental psychopathologists have argued that depression and generalized-type anxiety can be considered forms of a more general distress disorder (Moffitt et al. 2007).
Methodologically, there are important considerations for measuring affect and social context accurately. To capture affect and behavior, it is critical to assess them in natural settings and as they occur. Retrospective or prospective reporting of internal states, such as affect or physical discomfort, is notoriously flawed (Redelmeier and Kahneman 1996; Levine and Safer 2002; Wirtz et al. 2003). Factors such as peak intensity, expectations, and current state can bias reports of past experiences or predictions of future experiences. In contrast to the challenges of questionnaire methods in laboratory settings, which rely on estimates of past experiences, techniques such as ecological momentary assessment (EMA) have the potential to avoid bias by measuring affective experience and social behavior in real time and in typical settings. When examining affective processes in child and adolescent depression, EMA has the additional advantage of focusing on developmentally relevant contexts, in which naturally occurring events and typical responses can be measured.
The current study examined whether the social and affective dynamics of daily life can explain treatment response in young people with major depressive disorder (MDD) anxiety disorder (ANX), or both types of disorder. Using a structured interview administered by EMA, we measured participant-reported companions and levels of subjective affect across a 4-day period at baseline, before youth began participating in an 8-week open trial of cognitive behavioral therapy (CBT), selective serotonin reuptake inhibitors (SSRIs), or both treatments. Level of affect, variability in affect, and proportion of time with specific companions were examined as predictors of severity and symptoms at the end of treatment. The study was part of a larger research effort to examine neurobehavioral aspects of affect in young people with affective and anxiety disorders. The EMA measures were included in the study to investigate mood and behavior in natural settings, and they allowed us to address the association of baseline affect and social context with treatment response. Based on the literature on affective style and depression, we predicted that high PA, low NA, and high variability in both types of affect would be associated with lower severity and symptoms at the end of treatment. Based on the putative importance of social support for young people with depression, but considering the mixed findings to date on whether and how peers and family contribute to depression, we did not make strong predictions about the association between time with different companions and response to treatment. Our predictions were similar for the depression and anxiety groups.
In addition to investigating the association of affective and social dynamics with treatment outcome, we also examined the predictive utility of NA and PA experienced in natural settings before treatment for the course of treatment response. For this goal, we used latent growth curve models (LGCMs). LGCMs captured individual change over the course of the 8-week treatment period. This allowed us to measure rate of change over the treatment period, not just symptom improvement at the posttreatment assessment point. LGCMs are also able to include cases with incomplete data, allowing us to use all available information rather than losing cases with missing data. Therefore, we were able to examine whether baseline affect provides information regarding which youth will respond more quickly or less quickly over the course of treatment. Using this approach, we regressed the rate of change over the course of treatment on baseline EMA-measured affect and self-reported symptom ratings. We predicted that high PA and low NA at baseline would be associated with a faster rate of clinical improvement. Given that EMA may represent a more “accurate” assessment of affect regulation and functioning than laboratory measures of symptoms, we predicted that EMA-measured affect at baseline would predict treatment response above and beyond self-reported symptoms based on questionnaire data.
Methods
Participants
Participants were 66 children and adolescents aged 8–16 years (mean=12.08, SD=2.78) who had current diagnoses of MDD with comorbid anxiety (n=31), MDD only (n=12), or ANX (n=23). Participants with ANX were recruited for generalized anxiety, social anxiety, or separation anxiety rather than other forms (e.g., obsessive compulsive disorder). The sample was 60% female, and the racial/ethnic composition was 87% Caucasian, 4% African American, 6% Hispanic, and 3% other. In terms of pubertal development, 48.5% of participants were pre/early pubertal based on Tanner staging, 48.5% were mid/late pubertal, and 3% did not complete a physical examination. When analyses were conducted within developmental groups findings were consistent with those reported subsequently. This age range was selected in order to investigate the neurobehavioral features of depressive and anxiety disorders in young people from the period of sensitivity to these disorders that occurs from pre/early puberty through mid-adolescence. A broad age range encompassing the range of pubertal maturation allowed the testing of hypotheses during a period of important social and affective development and early in the course of these disorders. All participants were part of a multidisciplinary study of the neurobehavioral characteristics of early-onset affective disorders. Participants were recruited from the community through radio and newspaper advertisements.
Measures
Diagnosis
Diagnoses were determined through administration of the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Aged Children–Present and Lifetime Version (K-SADS-PL) (Kaufman et al. 1997). Each participant and a parent (or guardian) were interviewed separately by a bachelor's-level research specialist trained according to department-wide reliability standards. Reliability for MDD diagnoses was >90% and was maintained through monthly, department-wide diagnostic reviews. A child psychiatrist provided best-estimate diagnoses. Participants were excluded for use of medication with central nervous system or hypothalamic-pituitary effects within the past 2 weeks or use of fluoxetine within 2 months; significant medical illness; extreme obesity (weight > 150% of ideal body weight); IQ < 70; eating disorder, developmental disorder, schizophrenia, or learning disabilities; and current use of nicotine, illicit drugs, or alcohol. The decision to exclude participants with substance use was guided by the overall goals of the larger study, which focused on the pathophysiology of depression.
Affect and companions
During EMA calls, participants were asked to report, based on their experience at the time the phone rang, what they were doing and who was present (companions did not complete the EMA protocol). They were asked to report their current affective state, using items adapted from the Positive and Negative Affect Scale for Children (PANAS-C; Laurent et al. 1999), a reliable and valid questionnaire about current affect in young people. (We note, however, that psychometric properties have not been investigated for the PANAS as administered in an EMA context, and these might differ from the properties of the paper-and-pencil version.) For each item (e.g., happy), participants rated their affective state on a scale from 1 (very slightly or not at all) to 5 (extremely). The full set of 20 PANAS-C items was asked during the first phone call of each day, and a subset of the same 4 positive and 4 negative items was asked during the remaining calls to reduce time burden on participants. The 8 PANAS-C items included in every call were used to compute mean NA, PA, and PA: NA scores for each call. The mean of these variables for each call was then used to compute the mean for the entire time point (e.g., baseline NA), using the 12 calls for that time point. Baseline lability in PA or NA was computed as the standard deviation in mean PA or NA across the 12 calls for the first weekend. See Table 1 for descriptive statistics for EMA variables.
Table 1.
Descriptive Statistics for Mood and Companion Variables at Baseline
| Mean | SD | |
|---|---|---|
| Affect | ||
| NA | 1.32 | 0.37 |
| PA | 2.86 | 1.05 |
| PA:NA | 2.49 | 1.16 |
| NA lability | 0.24 | 0.22 |
| PA lability | 1.85 | 0.95 |
| Companion | ||
| Sibling | 0.21 | 0.21 |
| Mother | 0.15 | 0.18 |
| Father | 0.08 | 0.11 |
| Peer | 0.37 | 0.20 |
| None | 0.18 | 0.21 |
Note: Values for positive affect (PA) and negative affect (NA) are means of scores derived from relevant items adapted from the PANAS-C (Laurent et al. 1999) across 12 ecological momentary assessment calls. PA:NA is the ratio of mean PA across all calls to mean NA across all calls. Values for lability of PA and NA reflect the standard deviation of mean PA or NA score, respectively, computed for each of the 12 calls. Values for social companions are proportions of calls in which participants reported being in the presence of specific companions. All 12 calls occurred before treatment began.
Severity and symptoms
Clinicians rated severity using the Clinical Global Impressions-Severity (CGI-S) scale (Guy 1976) at baseline and after every 2 weeks of treatment (five time points total). The CGI-S is a single-item seven-point scale, with higher scores reflecting greater severity. It has been used in large and rigorous randomized controlled trials of psychosocial and pharmacologic treatments for adolescent depression (e.g., Keller et al. 2000; March et al. 2004). Psychometrically, the CGI-S provides comparable information to other measures in studies of response to pharmacologic treatments (Leucht and Engel 2006) and is correlated with self-reported and clinician-rated affective symptoms (Zaider et al. 2003). Clinicians administering the CGI-S compared and discussed their ratings during training. The instruments selected for measuring severity and symptoms have been widely used in treatment research on depression and anxiety in youth.
At baseline, participants completed the Screen for Childhood Anxiety and Related Disorders (SCARED) (Birmaher et al. 1999) and the Mood and Feelings Questionnaire (MFQ) (Angold et al. 2002) to report symptoms of anxiety and depression, respectively. Both are widely used measures with excellent psychometric properties, and have been used to assess affective symptoms in children and adolescents. The MFQ, for example, has been evaluated carefully for its psychometric features, and it has strong sensitivity and specificity for screening depressive and anxiety disorders (Wood et al. 1995; Katon et al. 2008). The psychometric properties of the SCARED have been examined in two independent samples, with similar findings of strong internal consistency for total score, the variable used in the current study (Birmaher et al. 1999). Clinicians who provided treatment rated depressive symptoms using the Child Depression Rating Scale–Revised (CDRS-R) (Poznanski and Mokros 1996), a 17-item measure based on an interview with the participant and parent.
Procedure
The study protocol was approved by the University of Pittsburgh Institutional Review Board. Participants' parents or guardians were told about the procedures of the study and signed an informed consent form; participants 14–16 years old provided informed consent; and participants <14 years provided oral assent.
EMA
A laboratory staff member visited each participant's home to drop off an answer-only cellular phone and train the participant in its use for EMA. During the home visit, the staff member told the participant when to expect phone calls, what types of experiences would be assessed during the calls, and how to use rating scales for specific queries. Staff members made sure that participants understood the subject matter of the phone calls.
EMA was conducted via cell phone from Friday afternoon to Monday night, with 12 calls per time point and at five time points during the 8-week treatment (see Silk et al., in press, for additional details). EMA was conducted primarily during a weekend so that calls would not interfere with school participation and participants would have more freedom to choose their activities and companions. Based on our experience in previous EMA studies and concerns expressed by parents, weekday calls occurred after school. Calls occurred within the same, prespecified 3-hour time window for all participants, in order to provide consistent assessment points across participants but to reduce predictability of call times within participants. Therefore, the timing of EMA calls was not entirely random but also was not completely predictable. Participants received two calls on Friday (4–7 p.m. and 7–10 p.m.), four each on Saturday and Sunday (11 a.m.–1 p.m., 1–4 p.m., 4–7 p.m., and 7–10 p.m.), and two on Monday (4–7 p.m. and 7–10 p.m.). The Monday calls were included to assess affect and behavior during a weeknight in addition to the weekend. The EMA protocol was conducted at five time points: the weekend before treatment began (i.e., baseline); after weeks 2, 4, and 6 of treatment; and the weekend after treatment ended (i.e., posttreatment). Phone calls were conducted by trained research assistants, using a script developed for the study. Participants responded to EMA phone calls and did not initiate their own assessments (e.g., after the occurrence of a specific event). Average call length was 4.64 minutes. Missing data occurred for 11.5% of the calls. Equipment problems and attrition were both relatively rare (1.7% and 4%, respectively).
To address hypotheses about time with family and peers, participants' open-ended responses to questions about current companions were coded using a system developed for the study. A subset of 100 calls was also double-coded, with reliability coefficients ranging from κ=0.85 to κ=0.98. Coded data were then reduced to the proportion of calls in which participants identified the presence of the following companions: any family member, mother, father, sibling, or peer.
Treatment
Participants and parents chose from three treatment options. Treatment involved an 8-week open protocol, and the options were CBT (n=24); CBT combined with pharmacotherapy using an SSRI (n=21); or SSRI only (n=21). The proportion of participants selecting each treatment option was fairly similar to that of other open trials of treatment for depression with both medication and psychotherapy options (e.g., in the postacute phase of the Treatment Resistant Depression in Adolescents Study, 55% of participants chose to add psychotherapy; Emslie et al. 2010).
CBT was provided at Western Psychiatric Institute and Clinic, and it was tailored to each participant and guided by techniques developed by Brent and colleagues (Brent et al. 1997). CBT was provided by nine trained therapists, who were Ph.D. psychologists, masters-level social workers, or masters-level nurses. Therapists all had training in CBT with children and adolescents and were supervised by a child psychiatrist with expertise in CBT for this population (Dr. Birmaher). Pharmacotherapy was provided by child psychiatrists assisted by psychiatric research nurses.
For pharmacotherapy, participants were scheduled to have face-to-face, weekly meetings with the treating psychiatrist and a psychiatric research nurse for the first month of the study. Medications used in pharmacotherapy were citalopram (10–40 mg) or fluoxetine (5–25 mg). Starting doses were the smallest that were likely to be tolerated by all participants, and would be considered the minimum therapeutic dose. For fluoxetine, 5 mg was selected as the starting dose for participants weighing <30 kg, and 10 mg was selected for participants weighing ≥30 kg. If subjects did not show significant clinical improvement after 2 weeks and were tolerating the age-corresponding dose, the dose was then increased to what would be likely to be therapeutic for the majority of subjects (e.g., for fluoxetine, 10 mg for subjects weighing <30 kg, and 20 mg for participants weighing ≥30 kg). After 4 weeks, if the subject was not responding to this dose, the treating psychiatrist increased the dose as tolerated. In addition, if a subject had an initial brief, but unsustained response to fluoxetine (e.g., was much improved at week 2 but regressed back to baseline on subsequent visits), then the psychiatrist increased the fluoxetine dose as tolerated. The dose of medication could be reduced at any time for side effects at the discretion of the treating psychiatrist.
Symptoms, severity, and improvement were measured at five time points: at baseline; at treatment weeks 2, 4, 6; and after the last treatment session (posttreatment). Because of subjects' declining to complete questionnaires, time constraints, or failure to complete the 8 weeks of treatment, clinician severity ratings were missing for 14 participants at baseline, for 15 at time 2, for 14 at time 3, for 17 at time 4, and for 21 at posttreatment. Analyses included all available data for each time point.
Data analytic strategy
SPSS 17.0 (2006) and Mplus 6.1 (Muthén and Muthén 2010) were used to conduct statistical analyses for the current study. To test whether affect and social context were associated with posttreatment severity and symptoms, EMA data from the first time point (i.e., 12 calls) were collapsed into mean NA, mean PA, mean PA: NA, NA variability, and PA variability, and included in correlations with posttreatment clinician-report and subject-report data.
For LGCM, we included EMA data from the first time point (i.e., 12 calls at baseline), creating a latent variable for each predictor of interest with 12 manifest indicators to account for the repeated measurements. Missing data on dependent variables were handled through the use of the expectation maximization (EM) algorithm. As clinician symptom severity ratings were collected throughout the course of treatment, models accounted for the nesting of multiple assessments within a person. In each model, the EMA affect ratings were used to predict the slope parameter of treatment response. Time was coded so that the intercept reflected the model-implied baseline assessment. Consistent with Mplus convention (Muthén and Muthén 2010), the third time point was allowed to freely estimate. Each latent EMA factor was specified to predict the slope parameter of treatment response. Additionally, to examine the validity of EMA ratings in predicting the symptom severity trajectory over the course of treatment, EMA ratings and subject-report ratings of depression and anxiety were simultaneously entered as predictors of the intercept and slope factors of the clinician-rated symptom severity scores.
Results
Choice of treatment
Choice of treatment was not related to age, gender, race, socioeconomic status, or symptom level (F=0.34–1.41, χ2=1.08–2.81, p>0.20). There was a statistical trend for choice of treatment to differ by diagnostic group [χ 2(4)=8.79, p=0.07] and with baseline clinician-rated severity [F(2,49)=2.30, p=0.11]. MDD/ANX participants were more likely than MDD participants to choose treatment with CBT over SSRIs [for MDD/ANX group, 39% chose CBT and 18% chose SSRIs; for MDD only, 17% chose CBT and 50% chose SSRIs; χ2(1)=4.30, p<0.05]. Participants who received either SSRIs or CBT + SSRIs tended to have higher severity than those who received CBT alone [F(1,33)=3.80, p=0.06 and F(1,35)=3.91, p=0.06, respectively].
Association of clinical severity with demographic and affective variables
Pre- and posttreatment severity were unrelated to treatment type, age, and gender (F=0.02–3.04, r=0.04-.19, p=0.09–0.90). In addition, to confirm that baseline EMA-measured affect did not simply represent clinical severity, we tested correlations between baseline affect variables and baseline severity. Correlations were modest and nonsignificant (e.g., r=0.13, p=0.36 for NA).
Baseline affect and posttreatment severity
As indicated in Table 2, higher PA, lower NA, and a higher PA:NA ratio predicted lower posttreatment severity, depressive symptoms, and anxiety symptoms (see Table 2). Lability in PA or NA was unrelated to posttreatment severity and symptoms.
Table 2.
Association of Pretreatment Affect and Social Context with Posttreatment Severity
| Severity | Depressive symptoms (CDRS-R) | Depressive symptoms (MFQ) | Anxiety symptoms | |
|---|---|---|---|---|
| Affect | ||||
| NA | 0.31* | 0.38* | 0.49** | 0.51** |
| PA | −0.32* | −0.33* | −0.35* | −0.44** |
| PA:NA | −0.38** | −0.43** | −0.51** | −0.57** |
| NA Lability | 0.08 | 0.19 | 0.02 | −0.09 |
| PA Lability | −0.05 | −0.18 | 0.04 | −0.06 |
| Companion | ||||
| Sibling | −0.33** | −0.35* | −0.04 | 0.04 |
| Mother | 0.12 | 0.05 | −0.02 | 0.08 |
| Father | −0.28 | −0.43** | −0.42** | −0.48** |
| Peer | 0.19 | 0.34* | 0.33* | 0.44** |
| None | 0.04 | 0.11 | −0.12 | −0.31 |
Note: All values are Pearson r statistics. Clinicians rated severity using the Clinical Global Impressions-Severity Scale (Guy 1976) and depressive symptoms using the Child Depression Rating Scale-Revised (CDRS-R; Poznanski and Mokros 1996). Participants self-reported depressive symptoms using the Mood and Feelings Questionnaire (MFQ; Angold et al. 2002) and anxiety symptoms using the Screen for Child Anxiety Related Emotional Disorders (Birmaher et al. 1999). Affect values are means of affective items over 12 time points, and companion values reflect proportion of time points at which participant reported reported the presence of the companion. NA=negative affect; PA=positive affect; PA:NA ratio of positive affect to negative affect.
p<0.05; **p<0.01.
Baseline social context and posttreatment severity
Clinician-rated severity and depressive symptoms at the end of treatment were lower in participants who spent a higher proportion of time with a sibling before treatment. Clinician-rated depressive symptoms and subject-reported depressive and anxiety symptom levels were lower posttreatment in participants who spent a higher proportion of time with fathers before treatment. In contrast to findings for proportion of time with fathers, clinician-rated depressive symptoms and subject-reported depression and anxiety symptoms at the end of treatment were higher in participants who spent a greater proportion of time with peers. Proportion of time with mothers was unrelated to severity and symptoms at the end of treatment.
LGCMs for changes in severity
Growth model of symptom severity over the course of treatment
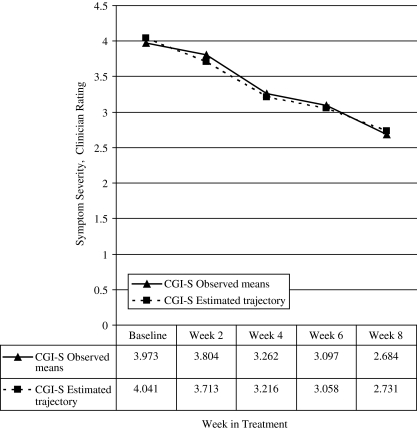
The unconditional LGCM for clinician-rated measure of symptom severity (CGI-S) fit the data well: χ2 (8, N=68)=9. 44; p=0.31 comparative fit index (CFI)=0.98; Tuker–Lewis index (TLI)=0.98; and root mean square error of approximation (RMSEA)=0.04. Time points were fixed incrementally to reflect the assessment schedule (e.g., baseline fixed at 0, time 2 at 1); however, a time score was estimated for time 3 clinician reports [b=2.519, p<0.001, 95% CI (2.08, 2.96)] to improve model fit. The LGCM had a significant mean intercept [Mi=4.04, p<0.001, 95% CI (3.89, 4.19)]; and slope [Ms=−0.33, p=0.018, 95% CI (−0.38, −0.28)]. The variance for the intercept was significant, [di=0.32, p=0.03, 95% CI (0.08, 0.57)], but the variance for the slope was non-significant, (ds=0.01, p=0.33, 95% CI [−.09, .03]), indicating substantial variation across subjects in initial symptom severity but not symptom trajectory. Even without significant growth in the unconditional model, including predictors can influence the slope so that it may vary as a function of these additional variables (Fisher and Kim 2007). Specifically, we were able to demonstrate the significant predictive effects of the EMA affect scores on the trajectory of symptom severity over time. These seemingly contradictory results may be the result of increased power to detect slope variability when covariates and outcomes are included in the model. The intercept and slope were not significantly correlated. Mean levels of clinician-rated symptom severity scores across the course of treatment are presented in Figure 1.
FIG. 1.
Observed means and estimated trajectories for clinician-reported symptom severity over 8 weeks of treatment with cognitive behavioral therapy (CBT), selective serotonin reuptake inhibitors (SSRIs), or both, collapsed across treatments. CGI-S, Clinical Global Impressions-Severity.
Symptom severity model conditioned on race, age, gender, and diagnosis
We examined the unique effects of race (0=African-American, 2=Hispanic, 3=Caucasian), gender (1=female, 2=male), age, and diagnosis (0=ANX, 1=MDD with or without an anxiety diagnosis) on our LGCM of clinician-rated symptom severity. All covariates were simultaneously entered into the baseline model, allowing for us to examine the effects of each covariate while controlling for all other covariates. The conditioned model fit the data well: χ2 (20, N=71)=19.97, p=0.86; CFI=1.00; TLI=1.00; and RMSEA <0.001. None of the covariates was significantly associated with the intercept or slope factors, indicating that the initial level and change in symptom severity scores did not differ by race, age, gender, or diagnosis.
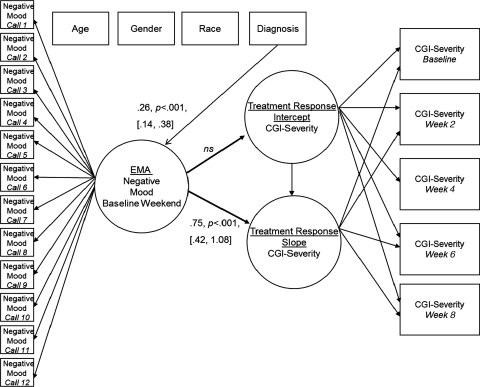
Baseline EMA-measured affect and symptom severity over the course of treatment
Each latent EMA mood factor (e.g., a latent variable for NA using affect data from all 12 baseline calls) was specified to predict the conditioned intercept and slope parameters of symptom severity. Age, gender, and race were also covariates on the latent EMA mood factors. Age was associated with PA [β=−0.54, p<0.001, 95% CI (−0.69, −0.40)], and PA:NA ratio [β=−0.43, p<0.001, 95% CI (−0.62, −0.27)], such that younger children experienced more PA. Diagnosis was associated with NA [β=0.26, p<0.001, 95% CI (0.14, 0.38)], indicating that subjects with an MDD diagnosis experienced higher NA than did subjects who had only ANX. Gender and race were not associated with any of the mood factors.
None of the affect variables predicted the intercept factor of symptom severity, indicating, as mentioned previously, that EMA-measured affect was not associated with initial symptom severity. NA [β=0.75, p<0 .001, 95% CI (0.42, 1.08)] predicted the slope factor, such that subjects with higher NA experienced slower decreases in severity across the course of treatment (see Figure 2). Additionally, PA:NA ratio predicted the slope factor of symptom severity [β=−0.64, p=0.047, 95% CI (−1.18, −0.11)], indicating that subjects with higher PA:NA experienced faster decreases in symptom severity over the course of treatment. However, neither PA nor PA variability predicted the slope factor of symptom severity, suggesting that EMA-measured PA and variability in PA at baseline were not associated with changes in symptom severity over the course of treatment. This pattern of findings also suggests that the PA:NA ratio might reflect findings for NA.
FIG. 2.
Results of the latent growth curve model with pretreatment (i.e., baseline) negative affect in natural settings, as measured by ecological momentary assessment (EMA), predicting clinician-rated severity over the course of treatment. For ease of presentation, factor loadings, error terms, and nonsignificant covariate regression paths are not depicted. Time points were fixed incrementally to reflect the assessment schedule. However, a time score was allowed to freely estimate for time 3 clinician reports. This resulted in the baseline time point fixed at 0, week 2 fixed at 1, week 4 fixed at 2.5, week 6 fixed at 3, and week 8 fixed at 4. CGI, Clinical Global Impressions scale (Guy 1976).
We then examined the predictive validity of EMA-measured affect over and above baseline self-report ratings of depressive (MFQ) and anxiety (SCARED) symptoms when predicting the symptom severity trajectory over the course of treatment. EMA-measured affect variables and self-reported symptoms were entered simultaneously in models predicting the conditioned trajectory of symptom severity. Self-reported symptoms did not predict the intercept or slope of symptom severity over the course of treatment. However, NA [β=0.76, p=0.001, 95% CI (0.50, 1.23)] significantly predicted the slope factor of symptom severity. These findings indicate the utility of EMA-measured affect over that of subject self-report to predict treatment responses. Specifically, NA and PA:NA were predictive of rate of change in symptoms over the course of treatment, whereas and self-reported symptoms were not.
Discussion
The current study is the first to examine real-life affect and social context as predictors of treatment response in young people with depression. Using EMA, an innovative method for treatment outcome research, we found that both affect and companions before treatment predicted psychopathology posttreatment, and that pretreatment affect predicted the rate of response during treatment. Specifically, PA, NA, and the ratio of PA to NA predicted clinician-rated severity, self-reported severity, and self-reported symptom levels at the end of treatment. Regarding companions, spending more time with fathers and less time with peers before treatment predicted lower levels of symptoms posttreatment. High NA at baseline predicted slower decrease in clinician-rated severity across treatment, and higher PA:NA at baseline predicted more rapid decrease in severity. These findings as a whole suggest that the assessment of mood and behavior in natural settings can provide important information about both the outcome of treatment and the course of treatment. Furthermore, of significance to clinical practice, EMA-measured affect provided additional information above and beyond traditional self-report assessment methods in the prediction of which subjects would respond more quickly to treatment.
Participants who had an EMA-measured affective profile postulated to be associated with healthy affective functioning—that is, low NA, high PA, and high PA:NA—had better response after treatment and responded more rapidly during treatment. Notably, NA, PA, and PA:NA were unrelated to severity at baseline, indicating that they did not simply represent level of illness. Therefore, our focus was somewhat different from studies examining whether baseline severity or clinical course influences treatment response and posttreatment severity (e.g., Curry et al. 2006). By focusing on affective characteristics rather than on severity as a predictor, we were able to examine an additional aspect of affective function in relation to treatment. Perhaps the experience of manageable levels of NA plus adequate levels of PA, despite the presence of affective disorder, provides a foundation for responding to treatment. One possibility for the mechanisms of this foundation is strengths in affect regulation, which might serve to buffer young people from the effects of depression and provide advantages in making use of treatment. Treatment might therefore build upon affect regulation foundations to promote reduction in severity and improvement in functioning. This pattern of EMA-measured affect could reflect functioning in neural circuits of affect, such as lower reactivity in threat circuits or higher reactivity in reward circuits, which, as we have found, can predict treatment response in depressed adolescents (Forbes et al. 2010). Individual differences in EMA-measured affect in young people with affective disorders therefore could have meaning for improvement with psychosocial or pharmacologic treatment. Young people with more aberrant patterns of affect might be more difficult to treat or might benefit from a different treatment strategy than those with a more typical pattern of subjective affect. Ultimately, because we did not measure affect regulation directly, it will be important to conduct more research in order to address the association between affect regulation and treatment response, as well as the role of subtleties of affect in daily life as a mechanisms of treatment response.
Consistent with models proposing that the PA:NA ratio is important for affective and cognitive functioning (Fredrickson and Losada 2005), the balance of PA and NA was associated with treatment response. However, it is important to note that even though the PA:NA ratio could have unique meaning for affective functioning and treatment response, a statistical possibility is that our findings for the PA:NA ratio were driven by the findings for NA. If meaningful, findings with PA:NA suggest that a variety of affective processes, as well as their interaction, could contribute to treatment response and that successful treatment might enhance synergy between PA and NA systems.
Our social context findings point out the value of time with fathers and siblings for treatment response in young people. Despite the developmental task of individuating from parents and increasingly focusing efforts on peer status, peer affiliation, and romantic relationships during late childhood and adolescence (Steinberg and Silk 2002), adolescents continue to rely on parents for promoting healthy affective functioning (Collins et al. 2000). Just as young people with depression are more likely to have family interactions characterized by parental reinforcement of adolescent dysphoric affect (Sheeber et al. 1998) and punitive responses to positive affect (Whittle et al. 2009), the current findings suggest that family relationships can play a role in supporting improvement with treatment. Although we did not measure the quality of participants' relationships with their family members, spending more time with a father, for example, could indicate that the father–child relationship is close or positive. A close father–child relationship could provide a unique kind of support for improvement and response to treatment in young people. In fact, research on family interactions indicates that support and conflict in father–child relationships—more so than in mother–child relationships—is associated with adolescents' depressive symptoms (Sheeber et al. 2007). The mechanisms for the association between supportive father–child relationships and treatment response could include fathers' encouragement of engagement in treatment or of strong therapeutic alliance, factors that may be especially important for psychosocial treatments such as CBT (Keijsers et al. 2000). That time with fathers—not mothers—was particularly predictive suggests in addition that fathers' engagement with their children could be especially valuable.
In contrast, time with peers had a negative influence on outcome, with a greater proportion of time spent with peers predicting higher depressive and anxiety symptoms at the end of treatment. Co-rumination between depressed adolescents and their peers has been proposed as a mechanism for social influence on affective state (Hankin et al. 2010), and this could have been part of the content of time our participants spent with their peers. We did not measure co-rumination in this study, although we are currently investigating the use of co-rumination about problems or symptoms as an affect regulation strategy in young people with affective disorders. Peer characteristics are likely to have an important contribution to treatment response in youth, with the potential for negative influence by peers who also have high levels of affective symptoms or difficulties with affect regulation.
By including both youth with anxiety disorders and youth with depressive disorders, we were able to investigate the similarities and differences between the two types of disorders, for predictors of treatment response. Anxiety and depression were distinguished by affect in natural settings before treatment, but they did not differ in the value of baseline affect for predicting treatment response. Whereas youth with depression had higher and more variable NA before treatment than did youth with anxiety, our growth curve models indicated that the diagnostic groups did not differ in the predictors of treatment response. That is, both youth with depression and youth with anxiety had lower severity after treatment and faster decrease in severity during treatment if they had low NA and high PA:NA before treatment.
Notably, EMA predicted treatment response above and beyond the contributions of initial symptom severity. Although both EMA and symptom ratings involved self-report by youth and could be expected to capture overlapping constructs, the two types of self-report did not have similar predictive value for treatment response. That is, when both types of self-report data were included in growth curve models, only EMA-measured affect in natural settings contributed to the decrease in severity during treatment. This pattern of findings indicates that the experience of affect in natural settings, rather than the recall of recent emotional experiences in a laboratory setting, could be more meaningfully and importantly related to improvement with treatment. Although symptom severity and EMA-measured affect have conceptual commonalities—such as the experience of high NA and low PA mood states in depression—the two types of self-report have important differences. In particular, there is evidence that retrospective and laboratory reports contain reporting biases (Levine and Safer 2002). One explanation for our findings is that baseline affect predicts treatment response because EMA captures “true” mood more effectively than do self-report questionnaires. Perhaps EMA-measured affect reflects a different aspect of affective functioning in the daily lives of children and adolescents than do those aspects described by self-reported symptoms or clinical severity. Although self-report of symptoms necessarily plays an important role in the diagnosis and treatment of depression and anxiety in young people, it may be that EMA-measured affect and companions can make a unique contribution to understanding the ability to make use of treatment. This finding has implications for the measurement of affective characteristics in treatment research, indicating that self-reported symptoms on standard questionnaires might have limited prognostic utility. In addition, the constructs of NA and clinical severity have conceptual similarities but are not identical, with NA including current, short-term experience of several aspects of affect and severity including the experience of problematic, longer-term affect.
Conclusion
Our conclusions are limited by the design of our study, which did not allow rigorous comparisons among treatment types. The study was not explicitly designed to compare psychotherapy with pharmacotherapy, and we note that we did not randomly assign participants to treatment type. Therefore, our results cannot inform decisions about which young people might be assigned to which type of treatment. Instead, our results speak to the baseline affective and social dynamics that are related to improvement more generally, as it occurs in the context of the current, standard set of treatments used with young people. We acknowledge that our results cannot guide treatment decisions; however, they represent a valuable first step toward understanding treatment response. Future research using randomized controlled trials (RCTs) can provide meaningful tests of hypotheses about the distinctions among treatment types in predicting response. By using both EMA and a design that allows comparison among treatments, future studies can contribute to the long-term goal of identifying which participants benefit from particular treatments.
Other methodological limitations include the relatively broad age range of the sample, the use of the same form of CBT for depression and anxiety groups, and the implications for generalizability of excluding participants with substance use. Our sample was small and limits the strength of any conclusions that can be made from our findings. Therefore, we recommend that future research attempt to replicate these findings. Also, our decision not to conduct EMA during the day on weekdays reduced similarity between weekend and weekday sampling. Future studies could include calls at lunchtime or immediately after school to increase sampling on weekdays. EMA included assessment of companions but did not assess the quality or intensity of the interactions with those companions, which limits our ability to make conclusions about the meaning of our findings about social context. In future studies, longitudinal measurement of symptoms, severity, and functioning after the conclusion of treatment and in larger samples will allow the investigation of the long-term value of EMA predictors of treatment response, as well as of the modeling of real-world mood as a predictor of different trajectories of response maintenance or recurrence.
Important future directions include investigating the mechanisms of treatment response by examining real-world affective and social experience, affect regulation, and brain function both before and during treatment. Indeed, we have begun to link EMA-measured affective experience to the neural mechanisms of affect (Forbes et al. 2009), and we plan to examine more nuanced associations between brain function and subjective experience. An important set of questions to be answered next concerns how affect and social context in young people with affective disorders change as a function of treatment.
Overall, this study provides a critical first step in understanding how real-world experience of NA and PA and time spent in social contexts can characterize response to treatment in children and adolescents with affective disorders. Our findings indicate that relationships with fathers and peers could provide a foundation for treatment outcome, albeit in opposite ways, suggesting that relationships could play a role in treatment response. Findings also indicate that EMA-measured affect has assessment utility, insofar as it captures an aspect of affective functioning that is somewhat distinct from affective symptoms or clinical severity. In addition, although more research is needed before recommending clinical applications of this work, our findings suggest that EMA-measured affect could have future clinical utility. With greater sophistication in addressing this topic, it may be possible to use affective and social functioning sampled in natural environments to make treatment decisions based on patterns of experience and behavior. Eventually, by strengthening our understanding of the characteristics of young people who respond to treatments, research using EMA in the context of RCTs could contribute to assigning young people to treatments, and possibly even refining existing treatments for subgroups of those with affective disorders. Ultimately, we can hope to improve the rate of treatment response in young people with depression and anxiety.
Clinical significance
The sampling of affect and social companions in natural settings using EMA could provide important information about both the outcome of treatment and the course of treatment for young people with depression and anxiety. In particular, lower levels of negative affect and more time spent with fathers predicted treatment response. In addition, we found that EMA-measured affect provided additional information above and beyond traditional self-report assessment methods (i.e., symptoms and severity) in the prediction of which subjects responded more quickly to treatment. Although more research is needed to determine how EMA-measured affect and companions can contribute to treatment decisions, these findings have potential future clinical utility.
Disclosures
Dr. Birmaher is a consultant for Schering Plough and has participated in forums sponsored by Dey Pharma, L.P. Drs. Forbes, Stepp, Dahl, Ryan, Axelson, and Silk, and Ms. Whalen have no financial relationships with any pharmaceutical company.
Acknowledgments
We thank the research assistants and clinicians who contributed to the study and the families who participated.
References
- Angold A. Erkanli A. Silberg J. Eaves L. Costello EJ. Depression scale scores in 8-17-year-olds: Effects of age and gender. J Child Psychol Psychiatry. 2002;43:1052–1063. doi: 10.1111/1469-7610.00232. [DOI] [PubMed] [Google Scholar]
- Auerbach RP. Bigda–Peyton JS. Eberhart NK. Webb CA. Ho MH. Conceptualizing the prospective relationship between social support, stress, and depressive symptoms among adolescents. J Abnorm Child Psychol. 2011;39:475–487. doi: 10.1007/s10802-010-9479-x. [DOI] [PubMed] [Google Scholar]
- Birmaher B. Brent DA. Chiappetta L. Bridge J. Monga S. Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): A replication study. J Am Acad Child Adolesc Psychiatry. 1999;38:1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- Brent DA. Holder D. Kolko D. Birmaher B. Baugher M. Roth C. Iyengar S. Johnson BA. A clinical psychotherapy trial for adolescent depression comparing cognitive, family, and supportive therapy. Arch Gen Psychiatry. 1997;54:877–885. doi: 10.1001/archpsyc.1997.01830210125017. [DOI] [PubMed] [Google Scholar]
- Campos JJ. Mumme DL. Kermoian R. Campos R. A functionalist perspective on the nature of emotion. In: Fox NA, editor. 2-3. Vol. 59. The development of emotion regulation: Biological and behavioral considerations; 1994. pp. 284–303. Serial No. 240. [PubMed] [Google Scholar]
- Clark LA. Watson D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. J Abnorm Psychol. 1991;100:316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- Collins WA. Maccoby EE. Steinberg L. Hetherington EM. Bornstein MH. Contemporary research on parenting. The case for nature and nurture. Am Psychol. 2000;55:218–232. [PubMed] [Google Scholar]
- Curry J. Rohde P. Simons A. Silva S. Vitiello B. Kratochvil C. Reinecke M. Feeny N. Wells K. Pathak S. Weller E. Rosenberg D. Kennard B. Robins M. Ginsburg G. March J. Predictors and moderators of acute outcome in the Treatment for Adolescents with Depression Study (TADS) J Am Acad Child Adolesc Psychiatry. 2006;45:1427–1439. doi: 10.1097/01.chi.0000240838.78984.e2. [DOI] [PubMed] [Google Scholar]
- Davey CG. Yucel M. Allen NB. The emergence of depression in adolescence: Development of the prefrontal cortex and the representation of reward. Neurosci Biobehav Rev. 2008;32:1–19. doi: 10.1016/j.neubiorev.2007.04.016. [DOI] [PubMed] [Google Scholar]
- Davidson RJ. Affective style, psychopathology, and resilience: Brain mechanisms and plasticity. Am Psychol. 2000;55:1196–1214. doi: 10.1037//0003-066x.55.11.1196. [DOI] [PubMed] [Google Scholar]
- Davidson RJ. Well-being and affective style: Neural substrates and biobehavioural correlates. Philos Trans R Soc Lond B Biol Sci. 2004;359:1395–1411. doi: 10.1098/rstb.2004.1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desjardins TL. Leadbeater BJ. Relational victimization and depressive symptoms in adolescence: Moderating effects of mother, father, and peer emotional support. J Youth Adolesc. 2011;40:531–544. doi: 10.1007/s10964-010-9562-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emslie GJ. Mayes T. Porta G. Vitiello B. Clarke G. Wagner KD. Asarnow JR. Spirito A. Birmaher B. Ryan N. Kennard B. DeBar L. McCracken J. Strober M. Onorato M. Zelazny J. Keller M. Iyengar S. Brent D. Treatment of Resistant Depression in Adolescents (TORDIA): Week 24 outcomes. Am J Psychiatry. 2010;167:782–791. doi: 10.1176/appi.ajp.2010.09040552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher PA. Kim HK. Intervention effects on foster preschoolers' attachment-related behaviors from a randomized trial. Prev Sci. 2007;8:161–170. doi: 10.1007/s11121-007-0066-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes EE. Dahl RE. Neural systems of positive affect: Relevance to understanding child and adolescent depression? Dev Psychopathol. 2005;17:827–850. doi: 10.1017/S095457940505039X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes EE. Hariri AR. Martin SL. Silk JS. Moyles DL. Fisher PM. Brown SM. Ryan ND. Birmaher B. Axelson DA. Dahl RE. Altered striatal activation predicting real-world positive affect in adolescent major depressive disorder. Am J Psychiatry. 2009;166:64–73. doi: 10.1176/appi.ajp.2008.07081336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes EE. Olino TM. Ryan ND. Birmaher B. Axelson D. Moyles DL. Dahl RE. Reward-related brain function as a predictor of treatment response in adolescents with major depressive disorder. Cogn Affect Behav Neurosci. 2010;10:107–118. doi: 10.3758/CABN.10.1.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowles DC. Psychophysiology and psychopathology: A motivational approach. Psychophysiology. 1988;25:373–391. doi: 10.1111/j.1469-8986.1988.tb01873.x. [DOI] [PubMed] [Google Scholar]
- Fredrickson BL. Losada MF. Positive affect and the complex dynamics of human flourishing. Am Psychol. 2005;60:687–686. doi: 10.1037/0003-066X.60.7.678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ. Muñoz R. Emotion regulation and mental health. Clin Psychol. 1995;2:151–164. [Google Scholar]
- Guy W. Clinical Global Impressions. In: Guy W., editor. ECDEU Assessment Manual for Psychopharmacology, revised. Rockville, MD.: National Institute of Mental Health; 1976. [Google Scholar]
- Hankin BL. Stone L. Wright PA. Corumination, interpersonal stress generation, and internalizing symptoms: accumulating effects and transactional influences in a multiwave study of adolescents. Dev Psychopathol. 2010;22:217–35. doi: 10.1017/S0954579409990368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joiner TE., Jr. Lewinsohn PM. Seeley JR. The core of loneliness: Lack of pleasurable engagement––more so than painful disconnection––predicts social impairment, depression onset, and recovery from depressive disorders among adolescents. J Pers Assess. 2002;79:472–491. doi: 10.1207/S15327752JPA7903_05. [DOI] [PubMed] [Google Scholar]
- Katon W. Russo J. Richardson L. McCauley E. Lozano P. Anxiety and depression screening for youth in a primary care population. Ambul Pediatr. 2008;8:182–188. doi: 10.1016/j.ambp.2008.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman J. Birmaher B. Brent D. Rao U. Flynn C. Moreci P. Williamson DE. Ryan N. Schedule for affective disorders and schizophrenia for school-age children–present and lifetime version (K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Keenan K. Feng X. Hipwell A. Klostermann S. Depression begets depression: Comparing the predictive utility of depression and anxiety symptoms to later depression. J Child Psychol Psychiatry. 2009;50:1167–1175. doi: 10.1111/j.1469-7610.2009.02080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keijsers GP. Schaap CP. Hoogduin CA. The impact of interpersonal patient and therapist behavior on outcome in cognitive-behavior therapy. A review of empirical studies. Behav Modif. 2000;24:264–297. doi: 10.1177/0145445500242006. [DOI] [PubMed] [Google Scholar]
- Keller MB. McCullough JP. Klein DN. Arnow BA. Dunner DL. Gelenberg AJ. Markowitz JC. Nemeroff CB. Russell JM. Thase ME. Trivedi MH. Zajecka J. A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy, and their combination for the treatment of chronic depression. N Engl J Med. 2000;342:1462–1470. doi: 10.1056/NEJM200005183422001. [DOI] [PubMed] [Google Scholar]
- Kennard B. Silva S. Vitiello B. Curry J. Kratochvil C. Simons A. Hughes J. Feeny N. Weller E. Sweeney M. Reinecke M. Pathak S. Ginsburg G. Emslie G. March J. Remission and residual symptoms after short-term treatment in the Treatment of Adolescents with Depression Study (TADS) J Am Acad Child Adolesc Psychiatry. 2006;45:1404–1411. doi: 10.1097/01.chi.0000242228.75516.21. [DOI] [PubMed] [Google Scholar]
- Kessler RC. Avenevoli S. Merikangas K. Mood disorders in children and adolescents: An epidemiologic perspective. Biol Psychiatry. 2001;49:1002–1014. doi: 10.1016/s0006-3223(01)01129-5. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Gatsonis C. Paulauskas SL. Richards C. Depressive disorders in childhood. IV. A longitudinal study of comorbidity with and risk for anxiety disorders. Arch Gen Psychiatry. 1989;46:776–782. doi: 10.1001/archpsyc.1989.01810090018003. [DOI] [PubMed] [Google Scholar]
- Larson R. Richards MH. Daily companionship in late childhood, early adolescence: Changing developmental contexts. Child Dev. 1991;62:284–300. doi: 10.1111/j.1467-8624.1991.tb01531.x. [DOI] [PubMed] [Google Scholar]
- Larson RW. Raffaelli M. Richards MH. Ham M. Jewell L. Ecology of depression in late childhood and early adolescence: A profile of daily states and activities. J Abnorm Psychol. 1990;99:92–102. doi: 10.1037//0021-843x.99.1.92. [DOI] [PubMed] [Google Scholar]
- Laurent J. Catanzaro SJ. Joiner TE., Jr. Rudolph KD. Potter KI. Lambert S. Osborne L. Gathright T. A measure of positive and negative affect for children: Scale development and preliminary validation. Psychol Assess. 1999;11:326–338. [Google Scholar]
- Leucht S. Engel RR. The relative sensitivity of the Clinical Global Impressions Scale and Brief Psychotic Rating Scale in Antipsychotic Drug Trials. Neuropsychopharmacology. 2006;31:406–412. doi: 10.1038/sj.npp.1300873. [DOI] [PubMed] [Google Scholar]
- Levine LJ. Safer MA. Sources of bias in memory for emotions. Curr Dir Psychol Sci. 2002;11:169–173. [Google Scholar]
- March J. Silva S. Petrycki S. Curry J. Wells K. Fairbank J. Burns B. Domino M. McNulty S. Vitiello B. Severe J. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. JAMA. 2004;292:807–820. doi: 10.1001/jama.292.7.807. [DOI] [PubMed] [Google Scholar]
- Moffitt TE. Harrington H. Caspi A. Kim–Cohen J. Goldberg D. Gregory AM. Poulton R. Depression and generalized anxiety disorder: Cumulative and sequential comorbidity in a birth cohort followed prospectively to age 32 years. Arch Gen Psychiatry. 2007;64:651–660. doi: 10.1001/archpsyc.64.6.651. [DOI] [PubMed] [Google Scholar]
- Morris AS. Silk JS. Steinberg L. Myers SS. Robinson LR. The role of the family context in the development of emotion regulation. Soc Dev. 2007;16:361–388. doi: 10.1111/j.1467-9507.2007.00389.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L. Muthén B. Los Angeles, CA: Muthén & Muthén; 2010. MPlus user's guide: Version 6.1. [Google Scholar]
- Poznanski E. Mokros H. Los Angeles, CA: WPS; 1996. Children's Depression Rating Scale-Revised (CDRS-R) [Google Scholar]
- Redelmeier DA. Kahneman D. Patients' painful memories of painful medical treatments: Real-time and retrospective evaluations of two minimally invasive procedures. Pain. 1996;66:3–8. doi: 10.1016/0304-3959(96)02994-6. [DOI] [PubMed] [Google Scholar]
- Rudolph KD. Hammen C. Burge D. A cognitive-interpersonal approach to depressive symptoms in preadolescent children. J Abnorm Child Psychol. 1997;25:33–45. doi: 10.1023/a:1025755307508. [DOI] [PubMed] [Google Scholar]
- Sheeber Allen NB. Leve C. Davis B. Shortt JW. Katz LF. Dynamics of affective experience and behavior in depressed adolescents. J Child Psychol Psychiatry. 2009;50:1419–1427. doi: 10.1111/j.1469-7610.2009.02148.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheeber L. Hops H. Andrews J. Alpert T. Davis B. Interactional processes in families with depressed and non-depressed adolescents: Reinforcement of depressive behavior. Behav Res Ther. 1998;36:417–427. doi: 10.1016/s0005-7967(97)10030-4. [DOI] [PubMed] [Google Scholar]
- Sheeber LB. Davis B. Leve C. Hops H. Tildesley E. Adolescents' relationships with their mothers and fathers: Associations with depressive disorder and subdiagnostic symptomatology. J Abnorm Psychol. 2007;116:144–154. doi: 10.1037/0021-843X.116.1.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silk JS. Forbes EE. Whalen DJ. Jakuback JL. Thompson WK. Ryan ND. Axelson DA. Birmaher B. Dahl RE. Daily emotional dynamics in depressed youth: A cell-phone ecological momentary assessment study. J Exp Child Psychol. 2011;110:241–257. doi: 10.1016/j.jecp.2010.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L. Silk JS. Parenting adolescents. In: Bornstein M.H., editor. Handbook of Parenting. Mahwah, NJ: Lawrence Erlbaum; 2002. pp. 103–133. [Google Scholar]
- Tompkins TL. Hockett AR. Abraibesh N. Witt JL. A closer look at co-rumination: Gender, coping, peer functioning and internalizing/externalizing problems. J Adolesc. 2011;34:801–811. doi: 10.1016/j.adolescence.2011.02.005. [DOI] [PubMed] [Google Scholar]
- Weinstein SM. Mermelstein RJ. Hankin BL. Hedeker D. Flay BR. Longitudinal patterns of daily affect and global mood during adolescence. J Res Adolesc. 2007;17:587–600. doi: 10.1111/j.1532-7795.2007.00536.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein SM. Mermelstein RJ. Hedeker D. Hankin BL. Flay BR. The time-varying influences of peer and family support on adolescent daily positive and negative affect. J Clin Child Adolesc Psychol. 2006;35:420–430. doi: 10.1207/s15374424jccp3503_7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittle S. Yap MB. Yucel M. Sheeber L. Simmons JG. Pantelis C. Allen NB. Maternal responses to adolescent positive affect are associated with adolescents' reward neuroanatomy. Soc Cogn Affect Neurosci. 2009;4:247–56. doi: 10.1093/scan/nsp012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wirtz D. Kruger J. Napa Scollon C. Diener E. What to do on spring break? The role of predicted, on-line, and remembered experience in future choice. Psychol Sci. 2003;14:520–524. doi: 10.1111/1467-9280.03455. [DOI] [PubMed] [Google Scholar]
- Witvliet M. Brendgen M. van Lier PA. Koot HM. Vitaro F. Early adolescent depressive symptoms: Prediction from clique isolation, loneliness, and perceived social acceptance. J Abnorm Child Psychol. 2010;38:1045–1056. doi: 10.1007/s10802-010-9426-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood A. Kroll L. Moore A. Harrington R. Properties of the mood and feelings questionnaire in adolescent psychiatric outpatients: A research note. J Child Psychol Psychiatry. 1995;36:327–34. doi: 10.1111/j.1469-7610.1995.tb01828.x. [DOI] [PubMed] [Google Scholar]
- Zaider TI. Heimberg RG. Fresco DM. Schneier FR. Liebowitz MR. Evaluation of the Clinical Global Impression Scale among individuals with social anxiety disorder. Psychol Med. 2003;33:611–622. doi: 10.1017/s0033291703007414. [DOI] [PubMed] [Google Scholar]