Abstract
Asthma remains the most common chronic condition of childhood. Strong evidence has linked exposure to allergens and other triggers commonly found in homes to allergen sensitization and asthma incidence and morbidity. A growing body of evidence has demonstrated that a home visit strategy that includes an environmental component that addresses multiple triggers through multiple interventions is effective. Such home visits reduce exposure to triggers, decrease symptoms and urgent health-care use, and increase quality of life. To make home visits widely available will require health-care payor reimbursement, government and health plan funding, training and certification of home visitors, and active referrals from health-care providers. However, a strategy based solely on education and behavior change is limited, because it cannot adequately reduce exposures due to adverse housing conditions. Therefore, approaches that address substandard housing are needed. These include remediation of existing housing and construction of new asthma-friendly homes. Most studies of remediation have made relatively narrow and focused improvements, such as insulation, heating, or ventilation. Outcomes have been mixed. Studies of new asthma-friendly homes are in their infancy, with promising pilot data. Further investigation is needed to establish the effectiveness of improving housing. A final strategy is improving housing quality through policy change, such as implementation of healthy housing guidelines for new construction, enhancement and increased enforcement of housing codes, and assuring smoke-free multi-unit homes. The combination of home visits, improved housing construction, and policy change has great potential for reducing the global burden of asthma.
Introduction
Asthma remains the most common chronic disease of childhood, affecting 9.1% of all American children. The prevalence and morbidity of asthma among children in the United States have increased dramatically over the past 3 decades. More than 6 million children have current asthma, leading to 205,000 pediatric hospitalizations and 697,000 emergency department visits each year.1 Asthma income and racial disparities continue undiminished.2 Relative to wealthier and white populations, low-income and non-white populations have higher asthma prevalence and experience more serious impacts such as severe attacks leading to emergency department visits and hospitalizations.2–5
Indoor Triggers Play a Major Role in Asthma Incidence and Morbidity
Asthma develops through the interaction of genetic factors with environmental exposures.6 Strong evidence has linked exposure to allergens commonly found in homes, such as those derived from dust mites, cockroaches, rodents, molds, and pet dander, to sensitization and subsequent asthma incidence and morbidity.7–13 Exposure to indoor allergens is widespread, with >92% of homes containing sufficient concentrations of at least 1 allergen in dust to cause symptoms in sensitized individuals and 46% with exposure to 3 or more.14 As much as 40% of the excess asthma risk in non-white children may be attributable to exposure to residential allergens.15 Being poor or a person of color is associated with increased rates of sensitization to several asthma-associated allergens found in homes.16–20
In addition to allergens, other indoor asthma triggers include tobacco smoke,21 nitrogen oxides from combustion devices,22 and irritants from volatile organic compounds and fungi.8
Housing Conditions Generate Exposure to Asthma Triggers
Living in substandard housing often leads to exposure to triggers and higher rates of allergen sensitization.23–26 Features of substandard housing such as excessive moisture and dampness, inadequate or poorly maintained heating and ventilation systems, crowding, pest infestations, deteriorated carpeting, and structural defects are associated with exposure to indoor asthma triggers.27
Interventions to Reduce Exposure to Triggers
Given the important role triggers play in producing asthma exacerbations and inequities, decreasing them has emerged as a major goal of current asthma guidelines.28,29 It is feasible to reduce indoor exposures and doing so improves clinical outcomes. Over the past 2 decades, knowledge of how to reduce exposure to indoor asthma triggers has increased dramatically.7,30–41
Single-trigger interventions generally ineffective
Initial approaches for reducing trigger exposure focused on individual triggers. They generally have had minimal to no success. For example, interventions that target dust mites alone have had limited impact, even those employing multiple modalities.42 Two well-designed, large, randomized studies of bedding encasements did not find improvements in clinical measures.43,44 Acaricides used as a single intervention do not appear to be effective.42 Another example is control of cockroach exposure. While effective strategies to reduce exposure to cockroaches are available (especially integrated pest management), evidence of impact on asthma morbidity is currently lacking.45–47
Single-component interventions also not very effective
Similarly, the evidence for the effectiveness of single interventions on clinical outcomes is weak. While vacuuming and/or steam cleaning may reduce exposure to mites and pet allergens, most studies have not assessed or demonstrated clinical improvements.48,49 High efficiency particulate arrestor (HEPA) air filters may reduce exposure to pet allergens, but clinical impact is uncertain.50–52
Multi-trigger, multi-component approaches more effective
Given the generally unimpressive effects of individual interventions, a new generation of studies has examined the potential benefits of more comprehensive approaches that address multiple triggers and the whole-home environment. Two major strategies for reducing exposures have emerged. The first is home-based education and support. However, a strategy based primarily on education and behavior change is limited in its ability to reduce exposures due to adverse housing conditions. Therefore, a complementary strategy addresses substandard housing conditions related to asthma. In this article, home visits are reviewed first and then improving housing is discussed.
Home visits
A growing body of evidence has demonstrated that a home visit strategy that includes an environmental component focused on multiple triggers through multiple interventions is effective. Such home visits reduce exposure to triggers, decrease symptoms and urgent health-care use, and increase quality of life.7,53–62 Visitors assess home environmental conditions, tailor education on how to eliminate triggers to the client's sensitization status and exposures found in the home, provide trigger reduction resources (eg, vacuums, cleaning supplies, bedding encasements, and referral to smoking cessation), help with cockroach and rodent integrated pest management, make minor repairs, and provide social support. Importantly, visitors build trusting relationships with clients, thus enhancing their effectiveness in motivating behavior changes.
The Seattle-King County Healthy Homes program is an example of a home visit program. Our first Healthy Homes I project delivered home visits to reduce exposure to indoor asthma triggers among children living in ethnically diverse, low-income households.53,63,64 A distinguishing feature of the Healthy Homes I project was its use of community health workers (CHWs). The CHWs shared language, ethnicity, culture, and a personal or family experience with asthma with the participants. The CHW provided a 1-year long, high-intensity intervention. During the first home visit, the CHW conducted a structured home environmental assessment by walking through the home with the caregiver. Following the assessment, the CHW developed an individualized home action plan that described protocol-specified actions to address the triggers and behaviors found by the assessment. Working with families during the following year, the CHW monitored and reinforced behaviors, adjusting plans as needed. Using a randomized controlled trial design, we compared the impact of the high intensity intervention to a low-intensity control group that received only a single visit and bedding covers. The high-intensity intervention yielded significantly greater benefit in caregiver quality-of-life65 [0.58 points, 95% confidence interval (CI) = 0.18, 0.99, P = 0.005] and lower urgent health services utilization (0.97 fewer episodes per year, 95% CI = –1.82, –0.12, P = 0.026). Symptom days decreased more in the high-intensity group, but the difference between groups was not significant (1.24 days per 2 weeks, 95% CI = –2.88, 0.40, P = 0.138).
The Inner City Asthma Study is the largest study to assess home visits.55 This multi-site randomized trial targeted interventions to reduce exposure to asthma triggers to which a child was sensitized. The intervention group had fewer symptoms (0.82 days per 2-week period, P < 0.001) and fewer unscheduled asthma-related visits to the emergency department or clinic (one fewer for every 2.85 children treated, P = 0.04).
Both studies employed CHWs as the home visitors. CHWs bring important strengths to home visit programs, especially when working with low-income, disempowered clients. Because they share community, culture, ethnicity, language, and life experiences with the families, they can bridge the gap between community members and the health system and develop trusting relationships. The CHW tends to function more as a peer and coach than a distant professional. Clients may be more likely to heed their advice and learn new skills as they develop relationships with the CHW. The CHWs model effective trigger control behaviors and tailor their support to a family's needs and priorities by assessing their readiness to take action and by understanding the family's cultural and community context. They help families with concerns extending well beyond asthma, such as housing, domestic violence, and employment to enable the family to focus on asthma.
Providing asthma education in the home, especially when directed toward environmental conditions, offers several advantages over clinic-based approaches. Assessment of the indoor environment is central to identification of exposures, yet it is difficult to do so without directly observing conditions in the home. It is also challenging to teach the exposure reduction skills in the clinic or class room. Home visitors bring education to participants and therefore may increase participation and retention relative to classes.
Protocols and resources to implement home visit programs are widely available.66,67 Implementation of home visit programs is feasible.68,69 Home visit programs are not expensive, with costs per client ranging from $200 to $1500. The range in costs is driven by variation in the type of home visitor and the intensity of the intervention. A recent cost-effectiveness analysis concluded that home visits have a return on investment of 5.3–14.0 and a cost $12–$57 per symptom-free day gained. Note that the annual cost of inhaled fluticasone (220 μg) is ∼$1567.70
Improved housing
Although evidence for the effectiveness of multifaceted, in-home, tailored interventions for asthma is strong, home interventions are limited in their ability to modify the relationship between housing conditions and asthma outcomes. Behavioral interventions alone cannot eliminate substandard housing conditions, such as water intrusion or lack of ventilation systems, which result in exposure to asthma triggers.
Therefore, we and others have begun developing interventions that address substandard housing conditions. Approaches include remediation of existing housing deficiencies to bring homes in line with healthy homes guidelines and construction of new asthma-friendly homes. Several sets of guidelines for such homes are available,71 such as The 7 Principles of a Healthy Home from the National Center for Healthy Housing,72 the U.S. Green Building Council's LEED for Homes,73 the National Association of Home Builders' NAHB Green Home Building Guidelines,74 Enterprise Community Partner's Green Communities Criteria,75 the U.S. Environmental Protection Agency's Energy Star with Indoor Air Package,76 and the American Lung Association's Health House Builder Guidelines.77 The recommendations include designing the foundation and building envelope to prevent water intrusion, incorporating efficient and effective ventilation methods, using hard surface flooring materials, and employing products that minimize emission of volatile organic compounds. The guidelines are heterogeneous and may not offer equivalent health protection.
Remediation of existing housing
Most studies of housing remediation have implemented focused, limited improvements. For example, a large, well-designed, randomized controlled trial of home insulation in New Zealand showed decreased moisture and mold exposure and improved general and respiratory health status.78 Several other studies have focused on remediation of mold-contaminated homes. The largest study (164 homes) was a randomized controlled trial of visible mold eradication (with removal, fungicide application, and ventilation fan installation). It reduced asthma symptoms and medication use, although not peak flow variability.79 A randomized controlled trial in Cleveland remediated mold-contaminated homes, including reduction of water infiltration, removal of water-damaged building materials, and heating/ventilation/air-conditioning alterations. All participants received optimized medical care and asthma education. Children living in the remediated home had significantly reduced symptom days and health-care use.80
Other studies have focused on improving ventilation and decreasing humidity as a means to reduce mite exposure.81–85 Some were able to reduce humidity and mite allergen levels, although with less success in very humid climates.
Investigators are currently assessing whether a more holistic approach to remediating homes may be more effective than single-focus repairs. The National Center for Healthy Housing has completed an evaluation of the Viking Apartments, a public housing development in Worthington, MN.86 Remediation included installation of a high-efficiency geothermal heating and cooling system, enhanced insulation of the building envelope, improved ventilation, and low-volatile organic compound paints, sealants, and adhesives. We are working with the King County Housing Authority to examine whether weatherizing homes with attention to reducing exposure to asthma triggers might be effective. Weatherization includes cost-effective energy upgrades, related repairs, and health and safety improvements, such as insulation, repairs to heating and ventilation systems, pest-proofing, minor roof and gutter repairs, mold remediation, and carpet removal. Two other similar projects are underway in Mankato, MN, and Washington, DC.87
Creating new asthma-friendly housing
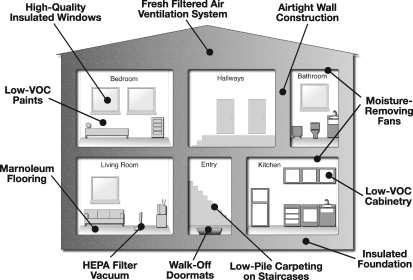
Our Breathe Easy Home pilot project is an example of the new housing construction approach. We assessed whether moving into a new asthma-friendly home provides additional benefits in controlling asthma beyond those offered by CHW home visits.88 The homes include high R-value blown-in insulation in a wall constructed of 2 × 6 advanced framing, exterior envelope made of cement board exterior siding with a modified rain screen and airtight and moisture-tight construction, Energy Star™ compliant argon-filled windows (U < 0.35), insulated foundation, airtight drywall installation, heat-recovery HEPA filtered whole-house ventilation, spot ventilation in all bathrooms and kitchen areas with humidity sensitive controls in bathrooms with showers, hot water heat to avoid dust associated with forced-air systems, hard surface flooring (Marmoleum™) with carpeting only on stairs, low emission finishes, sealed cabinets, and low allergen landscaping (Fig. 1). The additional Breathe Easy Home features added an additional $6000–$7000 in building costs per unit, equal to the cost of 2 pediatric hospitalization ($3343 each).89
FIG. 1.
High-Point Breathe Easy Home.
CHWs helped families learn about their new homes, and gave them home cleaning resources similar to those provided in Healthy Homes I. The lease agreement specifically prohibited smoking or furry pets inside homes.
Children who moved into the Breathe Easy Homes benefited from large increases in symptom-free days (from 8.6 per 2 weeks to 12.4, 95% CI of change = 1.7, 5.9, P = 0.001) and their caretakers showed improvement in asthma-related quality of life (from 5.0 to 5.8 units in the Pediatric Asthma Caregiver Quality of Life scale,65 95% CI of change = 0.3, 1.4, P = 0.002). The proportion with an urgent clinical visit in the prior 3 months decreased from 62% to 21% (95% CI of change = −65.9, − 16.5, P = 0.002). Rescue medication use, activity limitation, and symptom nights in the past 2 weeks all decreased. Lung function measured by FEV1 improved. Exposure to mold, dampness, and rodents after moving into the Breathe Easy Homes decreased dramatically and significantly. Smoking in the home and roaches also showed large and clinically important changes, which did not reach statistical significance. We compared these changes within the Breathe Easy Home group to those observed in an historical comparison group that had received CHW home visits while remaining in old homes. This analysis showed no significant differences in outcomes across the 2 cohorts, although the degree of improvement in the Breathe Easy Home group was greater for all measures except FEV1 and nocturnal asthma symptoms. This study suggests that moving into a healthier home adds benefits beyond those conferred by in-home asthma education alone, but larger and more rigorous studies are needed to confirm these suggestive initial findings.
Where to Go from Here
So where do we stand in regard to implementing effective interventions to reduce exposure to asthma triggers in the home? The evidence for multi-trigger, multi-component home visits is strong, the costs reasonable, and the feasibility of implementation clear. The next task is to overcome barriers to wide-spread dissemination. Health-care payors need to reimburse for home visits, just as they do for asthma medications. Federal, state, and local governments and health plans should fund home visits through public–private partnerships. As the strongest evidence exists for CHW home visit programs, CHW training and certification programs are needed. Implementers of home visit programs should monitor the quality of visits to assure funders of adequate performance. Health-care providers should refer patients with uncontrolled asthma to home visit programs, where available. Overcoming these barriers will not be easy given the orientation of our health system toward high-tech, biomedical, and profit-generating disease control strategies. Home visits cannot be patented and are high-touch. However, health-care reform does include support for CHWs and for health education, making the future a bit brighter.
Important questions regarding home visits remain unanswered regarding the relative merits of different types of home visitors (programs have employed various types of visitors, such as CHWs, sanitarians, nurses, and doctors,57 with current evidence showing no difference in outcomes53,55,58), the most cost-effective intensity and duration of the intervention, the possibility of substituting telephone contact for some of the follow-up visits, the durability of intervention effect, and the role of home visits in higher-income and more privileged populations generally not included in existing studies. Further research to address these issues is warranted.
It is reasonable to offer home visits that address the full spectrum of asthma self-management, going beyond trigger reduction to include proper use of medications, self-monitoring, use of action plans to reverse worsening control, and effective use of the health-care system. Such holistic visits are likely to be more effective than those that focus solely on the home environment and are more acceptable to caregivers who seek a more complete approach to controlling asthma. Our later projects have emphasized an integrated approach to home-based asthma support that includes all these elements.54
The evidence for remediation and construction, while promising, is less substantial. Further investigation is needed to establish the cost-effectiveness of improving housing, at least from the narrow perspective of asthma-related outcomes. However, living in unhealthy housing has many additional risks beyond asthma and living in healthy housing yields benefits beyond decreased asthma morbidity.90–92 Exposure to hazards in homes such as lead, secondhand smoke, asbestos, radon, volatile organic compounds, crowding, tripping hazards, and excess heat and cold is linked to many adverse health outcomes, including lung cancer, injuries, poor mental health, and neurodevelopmental disorders. Therefore, broad strategies to improve housing quality are needed, such as implementation of healthy housing guidelines for new and existing construction, enhancement of housing codes to include elements that promote the health of occupants, increased enforcement of housing codes, policies that assure smoke-free multi-unit homes, and market-based strategies that incentivize construction of healthy housing.
In conclusion, effective control of asthma requires eliminating triggers from the home. We have the knowledge to do so. We now must put this knowledge into practice, and thereby help millions of children with asthma live healthier lives.
Acknowledgments
The author would like to thank David Jacobs and two anonymous reviewers for their comments that resulted in an improved article.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Akinbami LJ. Moorman JE. Garbe PL. Sondik EJ. Status of childhood asthma in the United States, 1980–2007. Pediatrics. 2009;123(Suppl 3):S131–S145. doi: 10.1542/peds.2008-2233C. [DOI] [PubMed] [Google Scholar]
- 2.Gold DR. Wright R. Population disparities in asthma. Annu Rev Public Health. 2005;26:89–113. doi: 10.1146/annurev.publhealth.26.021304.144528. [DOI] [PubMed] [Google Scholar]
- 3.Aligne CA. Auinger P. Byrd RS. Weitzman M. Risk factors for pediatric asthma: Contributions of poverty, race, and urban residence. Am J Respir Crit Care Med. 2000;162:873–877. doi: 10.1164/ajrccm.162.3.9908085. [DOI] [PubMed] [Google Scholar]
- 4.Litonjua AA. Carey VJ. Weiss ST. Gold DR. Race, socioeconomic factors, and area of residence are associated with asthma prevalence. Pediatr Pulmonol. 1999;28:394–401. doi: 10.1002/(sici)1099-0496(199912)28:6<394::aid-ppul2>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 5.Grant EN. Alp H. Weiss KB. The challenge of inner-city asthma. Curr Opin Pulm Med. 1999;5:27–34. doi: 10.1097/00063198-199901000-00005. [DOI] [PubMed] [Google Scholar]
- 6.von Mutius E. Gene-environment interactions in asthma. J Allergy Clin Immunol. 2009;123:3–11. doi: 10.1016/j.jaci.2008.10.046. [DOI] [PubMed] [Google Scholar]
- 7.Institute of Medicine. Clearing the air: Asthma and indoor air exposures. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- 8.Institute of Medicine. Damp indoor spaces and health. Washington, DC: National Academy Press; 2004. [Google Scholar]
- 9.Sporik R. Squillace SP. Ingram JM. Rakes G. Honsinger RW. Platts-Mills TA. Mite, cat, and cockroach exposure, allergen sensitisation, and asthma in children: A case-control study of three schools. Thorax. 1999;54:675–680. doi: 10.1136/thx.54.8.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosenstreich DL. Eggleston P. Kattan M, et al. The role of cockroach allergy and exposure to cockroach allergen in causing morbidity among inner-city children with asthma. N Engl J Med. 1997;336:1356–1363. doi: 10.1056/NEJM199705083361904. [DOI] [PubMed] [Google Scholar]
- 11.Zock JP. Jarvis D. Luczynska C. Sunyer J. Burney P. European Community Respiratory Health Survey. Housing characteristics, reported mold exposure, and asthma in the European Community Respiratory Health Survey. J Allergy Clin Immunol. 2002;110:285–292. doi: 10.1067/mai.2002.126383. [DOI] [PubMed] [Google Scholar]
- 12.Phipatanakul W. Rodent allergens. Curr Allergy Asthma Rep. 2002;2:412–416. doi: 10.1007/s11882-002-0075-1. [DOI] [PubMed] [Google Scholar]
- 13.Salo PM. Jaramillo R. Cohn RD. London SJ. Zeldin DC. Exposure to mouse allergen in U.S. homes associated with asthma symptoms. Environ Health Perspect. 2009;117:387–391. doi: 10.1289/ehp.11847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salo PM. Arbes SJ., Jr. Crockett PW. Thorne PS. Cohn RD. Zeldin DC. Exposure to multiple indoor allergens in US homes and its relationship to asthma. J Allergy Clin Immunol. 2008;121:678–684. doi: 10.1016/j.jaci.2007.12.1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lanphear BP. Aligne CA. Auinger P. Weitzman M. Byrd RS. Residential exposures associated with asthma in US children. Pediatrics. 2001;107:505–511. doi: 10.1542/peds.107.3.505. [DOI] [PubMed] [Google Scholar]
- 16.Christiansen SC. Martin SB. Schleicher NC. Koziol JA. Hamilton RG. Zuraw BL. Exposure and sensitization to environmental allergen of predominantly Hispanic children with asthma in San Diego's inner city. J Allergy Clin Immunol. 1996;98:288–294. doi: 10.1016/s0091-6749(96)70152-5. [DOI] [PubMed] [Google Scholar]
- 17.Willies-Jacobo LJ. Denson-Lino JM. Rosas A. O'Connor RD. Wilson NW. Socioeconomic status and allergy in children with asthma. J Allergy Clin Immunol. 1993;92:630–632. [PubMed] [Google Scholar]
- 18.Sarpong SB. Hamilton RG. Eggleston PA. Adkinson NF. Socioeconomic status and race as risk factors for cockroach allergen exposure and sensitization in children with asthma. J Allergy Clin Immunol. 1996;97:1393–1401. doi: 10.1016/s0091-6749(96)70209-9. [DOI] [PubMed] [Google Scholar]
- 19.Lewis SA. Weiss ST. Platts-Mills TAE. Syring M. Gold DR. Association of specific allergen sensitization with socioeconomic factors and allergic disease in a population of Boston women. J Allergy Clin Immunol. 2001;107:615–622. doi: 10.1067/mai.2001.113523. [DOI] [PubMed] [Google Scholar]
- 20.Eggleston PA. Environmental causes of asthma in inner city children. The National Cooperative Inner City Asthma Study. Clin Rev Allergy Immunol. 2000;18:311–324. doi: 10.1385/CRIAI:18:3:311. [DOI] [PubMed] [Google Scholar]
- 21.U.S. Department of Health and Human Services. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2006. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General—Executive Summary. [Google Scholar]
- 22.Hansel NN. Breysse PN. McCormack MC. Matsui EC. Curtin-Brosnan J. Williams DL. Moore JL. Cuhran JL. Diette GB. A longitudinal study of indoor nitrogen dioxide levels and respiratory symptoms in inner-city children with asthma. Environ Health Perspect. 2008;116:1428–1432. doi: 10.1289/ehp.11349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huss K. Rand CS. Butz AM, et al. Home environmental risk factors in urban minority asthmatic children. Ann Allergy. 1994;72:173–177. [PubMed] [Google Scholar]
- 24.Kitch BT. Chew G. Burge HA. Muilenberg ML. Weiss ST. Platts-Mills TA. O'Connor G. Gold DR. Socioeconomic predictors of high allergen levels in homes in the greater Boston area. Environ Health Perspect. 2000;108:301–307. doi: 10.1289/ehp.00108301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dales R. Liu L. Wheeler AJ. Gilbert NL. Quality of indoor residential air and health. Can Med Assoc J. 2008;179:147–152. doi: 10.1503/cmaj.070359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rauh VA. Chew GL. Garfinkel RS. Deteriorated housing contributes to high cockroach allergen levels in inner-city households. Environ Health Perspect. 2002;110:323–327. doi: 10.1289/ehp.02110s2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hyndman S. Hyndman S. Making connections between housing and health. Putting health into place. Syracuse, NY: Syracuse University Press; 1998. pp. 191–207. [Google Scholar]
- 28.National Asthma Education and Prevention Program. Bethesda, MD: National Heart, Lung and Blood Institute; 2007. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. [Google Scholar]
- 29.Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. 2009. www.ginasthma.org/Guidelineitem.asp??l1=2&l2=1&intId=1561. [Jun 6;2010 ]. www.ginasthma.org/Guidelineitem.asp??l1=2&l2=1&intId=1561
- 30.Phipatanakul W. Environmental factors and childhood asthma. Pediatr Ann. 2006;35:646–656. [PubMed] [Google Scholar]
- 31.Eggleston PA. Improving indoor environments: Reducing allergen exposures. J Allergy Clin Immunol. 2005;116:122–126. doi: 10.1016/j.jaci.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 32.Krieger J. Jacobs DE. Ashley PJ. Baeder A. Chew G. Dearborn D. Hynes HP. Miller JD. Morely R. Rabito F. Housing interventions and control of indoor biologic agents: A review of the evidence. J Public Health Manag Pract. 2010 doi: 10.1097/PHH.0b013e3181ddcbd9. (accepted for publication). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Custovic A. Woodcock A. On allergens and asthma (again): Does exposure to allergens in homes exacerbate asthma? Clin Exp Allergy. 2001;31:670–673. doi: 10.1046/j.1365-2222.2001.01092.x. [DOI] [PubMed] [Google Scholar]
- 34.Platts-Mills TAE. Allergen avoidance. J Allergy Clin Immunol. 2004;113:388–391. doi: 10.1016/j.jaci.2003.12.027. [DOI] [PubMed] [Google Scholar]
- 35.Burr ML. Matthews IP. Arthur RA, et al. Effects on patients with asthma of eradicating visible indoor mould: A randomised controlled trial. Thorax. 2007;62:766–771. doi: 10.1136/thx.2006.070847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arlian L. Neal J. Morgan M, et al. Reducing relative humidity is a practical way to control dust mites and their allergens in homes in temperate climates. J Allergy Clin Immunol. 2001;107:99–104. doi: 10.1067/mai.2001.112119. [DOI] [PubMed] [Google Scholar]
- 37.Storey E. Dangman KH. Schenck P. Yang C, et al. Farmington, CT: University of Connecticut Health Center, Center for Environments and Health; 2004. Guidance for clinicians on the recognition and management of health effects related to mold exposure and moisture indoors. [Google Scholar]
- 38.Howden-Chapman P. Pierse N. Nicholls S, et al. Effects of improved home heating on asthma in community dwelling children: Randomised controlled trial. BMJ. 2008;337:a1411. doi: 10.1136/bmj.a1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wright GR. Howieson S. McSharry C, et al. Effect of improved home ventilation on asthma control and house dust mite allergen levels. Allergy. 2009;64:1671–1680. doi: 10.1111/j.1398-9995.2009.02098.x. [DOI] [PubMed] [Google Scholar]
- 40.Simpson A. Custovic A. Prevention of allergic sensitization by environmental control. Curr Allergy Asthma Rep. 2009;9:363–369. doi: 10.1007/s11882-009-0053-y. [DOI] [PubMed] [Google Scholar]
- 41.WHO expert meeting on policy recommendations on damp and mould interventions, Bonn, Germany. Copenhagen, WHO Regional Office for Europe. Feb 9–10, 2009. 2009. www.euro.who.int/Housing/support/20090107_1. [Jun 6;2010 ]. www.euro.who.int/Housing/support/20090107_1
- 42.Gøtzsche PC. Johansen HK. House dust mite control measures for asthma: Systematic review. Allergy. 2008;63:646–659. doi: 10.1111/j.1398-9995.2008.01690.x. [DOI] [PubMed] [Google Scholar]
- 43.Woodcock A. Forster L. Matthews E. Martin J. Letley L. Vickers M. Britton J. Strachan D. Howarth P. Altmann D. Frost C. Custovic A. Control of exposure to mite allergen and allergen-impermeable bed covers for adults with asthma. N Engl J Med. 2003;349:225–236. doi: 10.1056/NEJMoa023175. [DOI] [PubMed] [Google Scholar]
- 44.Terreehorst I. Hak E. Oosting AJ, et al. Evaluation of impermeable covers for bedding in patients with allergic rhinitis. N Engl J Med. 2003;349:237–246. doi: 10.1056/NEJMoa023171. [DOI] [PubMed] [Google Scholar]
- 45.Williams MK. Barr DB. Camann DE, et al. An intervention to reduce residential insecticide exposure during pregnancy among an inner-city cohort. Environ Health Perspect. 2006;114:1684–1689. doi: 10.1289/ehp.9168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang CL. Bennett GW. Comparative study of integrated pest management and baiting for German cockroach management in public housing. J Econ Entomol. 2006;99:879–885. doi: 10.1603/0022-0493-99.3.879. [DOI] [PubMed] [Google Scholar]
- 47.Arbes SJ. Sever M. Archer J, et al. Abatement of cockroach allergen (Bla g 1) in low-income, urban housing: A randomized controlled trial. J Allergy Clin Immunol. 2003;112:339–345. doi: 10.1067/mai.2003.1597. [DOI] [PubMed] [Google Scholar]
- 48.Vojta PJ. Randels SP. Stout J, et al. Effects of physical interventions on house dust mite allergen levels in carpet, bed, and upholstery dust in low-income, urban homes. Environ Health Perspect. 2001;109:815–819. doi: 10.1289/ehp.01109815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Popplewell EJ. Innes VA. Lloyd-Hughes S, et al. The effect of high-efficiency and standard vacuum-cleaners on mite, cat and dog allergen levels and clinical progress. Pediatr Allergy Immunol. 2000;11:142–148. doi: 10.1034/j.1399-3038.2000.00058.x. [DOI] [PubMed] [Google Scholar]
- 50.Wood RA. Air filtration devices in the control of indoor allergens. Curr Allergy Asthma Rep. 2002;2:397–400. doi: 10.1007/s11882-002-0073-3. [DOI] [PubMed] [Google Scholar]
- 51.Kilburn S. Lasserson TJ. McKean M. Pet allergen control measures for allergic asthma in children and adults. Cochrane Database Syst Rev. 2003;(1):CD002989. doi: 10.1002/14651858.CD002989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sublett JL. Seltzer J. Burkhead R. Williams PB. Wedner HJ. Phipatanakul W. American Academy of Allergy, Asthma & Immunology Indoor Allergen Committee. Air filters and air cleaners: Rostrum by the American Academy of Allergy, Asthma & Immunology Indoor Allergen Committee. J Allergy Clin Immunol. 2010;125:32–38. doi: 10.1016/j.jaci.2009.08.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Krieger JW. Takaro TK. Song L. Weaver M. The Seattle-King County Healthy Homes project: A randomized, controlled trial of a community health worker intervention to decrease exposure to indoor asthma triggers. Am J Public Health Apr. 2005;95:652–659. doi: 10.2105/AJPH.2004.042994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Krieger J. Takaro TK. Song L, et al. The Seattle-King County Healthy Homes II Project: A randomized controlled trial of asthma self-management support comparing clinic-based nurses and in-home community health workers. Arch Pediatr Adolesc Med. 2009;163:141–149. doi: 10.1001/archpediatrics.2008.532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Morgan WJ. Crain EF. Gruchalla RS, et al. Inner-City Asthma Study Group: Results of a home-based environmental intervention among urban children with asthma. N Engl J Med. 2004;351:1068–1080. doi: 10.1056/NEJMoa032097. [DOI] [PubMed] [Google Scholar]
- 56.Eggleston PA. Butz A. Rand C, et al. Home environmental intervention in inner-city asthma: A randomized controlled clinical trial. Ann Allergy Asthma Immunol. 2005;95:518–524. doi: 10.1016/S1081-1206(10)61012-5. [DOI] [PubMed] [Google Scholar]
- 57.Carter MC. Perzanowski MS. Raymond A, et al. Home intervention in the treatment of asthma among inner-city children. J Allergy Clin Immunol. 2001;108:732–737. doi: 10.1067/mai.2001.119155. [DOI] [PubMed] [Google Scholar]
- 58.Parker EA. Israel BA. Robins TG, et al. Evaluation of community action against asthma: A community health worker intervention to improve children's asthma-related health by reducing household environmental triggers for asthma. Health Educ Behav. 2008;35:376–395. doi: 10.1177/1090198106290622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fisher E. Strunk RC. Highstein GR. Kelley-Sykes R. Tarr KL. Asthma coaches: A randomized controlled evaluation of the 2 impact of community health workers on hospitalization for asthma. Arch Pediatr Adolesc Med. 2009;163:225–232. doi: 10.1001/archpediatrics.2008.577. [DOI] [PubMed] [Google Scholar]
- 60.Crocker DD. Hopkins D. Kinyota S, et al. A systematic review of home-based multi-trigger multi-component environmental interventions to reduce asthma morbidity. J Allergy Clin Immunol. 2009;123:S20. [Google Scholar]
- 61.Postma J. Karr C. Kieckhefer G. Community health workers and environmental interventions for children with asthma: A systematic review. J Asthma. 2009;46:564–576. doi: 10.1080/02770900902912638. [DOI] [PubMed] [Google Scholar]
- 62.Bryant-Stephens T. Kurian C. Guo R. Zhao H. Impact of a household environmental intervention delivered by lay health workers on asthma symptom control in urban, disadvantaged children with asthma. Am J Public Health. 2009;99:S657–S665. doi: 10.2105/AJPH.2009.165423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Takaro TK. Krieger JW. Song L. Effect of environmental interventions to reduce exposure to asthma triggers in homes of low-income children in Seattle. J Expo Anal Environ Epidemiol. 2004;14:S133–S143. doi: 10.1038/sj.jea.7500367. [DOI] [PubMed] [Google Scholar]
- 64.Krieger JK. Takaro TK. Allen C. Song L. Weaver M. Chai S. Dickey P. The Seattle-King County healthy homes project: Implementation of a comprehensive approach to improving indoor environmental quality for low-income children with asthma. Environ Health Perspect. 2002;110(Suppl 2):311–322. doi: 10.1289/ehp.02110s2311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Juniper EF. Guyatt GH. Feeny DH. Ferrie PJ. Griffith LE. Townsend M. Measuring quality of life in the parents of children with asthma. Qual Life Res. 1996;5:27–34. doi: 10.1007/BF00435966. [DOI] [PubMed] [Google Scholar]
- 66.Seattle-King County Healthy Homes. www.kingcounty.gov/healthservices/health/chronic/asthma.aspx. [Jun 6;2010 ]. www.kingcounty.gov/healthservices/health/chronic/asthma.aspx
- 67.US Environmental Protection Agency. Implementing An Asthma Home Visit Program: 10 Steps To Help Health Plans Get Started. Aug, 2005. www.epa.gov/asthma/pdfs/implementing_an_asthma_home_visit_program.pdf. [Jun 6;2010 ]. www.epa.gov/asthma/pdfs/implementing_an_asthma_home_visit_program.pdf
- 68.Hoppin P. Jacobs M. Ribble M. Dorchester, MA: Asthma Regional Council of New England; Sep, 2006. [Jun 6;2010 ]. Enhancing asthma management using in-home environmental interventions: A review of public health department programs. [Google Scholar]
- 69.Friedman AR. Butterfoss FD. Krieger JW. Peterson JW. Dwyer M. Wicklund K. Rosenthal MP. Smith L. Allies community health workers: Bridging the gap. Health Promot Pract. 2006;7(2 Suppl):96S–107S. doi: 10.1177/1524839906287065. [DOI] [PubMed] [Google Scholar]
- 70.Drugstore.Com. www.drugstore.com/pharmacy/prices/drugprice.asp?ndc=00173071920&trx=1Z5006. [Jun 5;2010 ]. Drugstore.Comwww.drugstore.com/pharmacy/prices/drugprice.asp?ndc=00173071920&trx=1Z5006
- 71.National Center for Healthy Housing. Comparing Green Building Guidelines and Healthy Homes Principles: A Preliminary Investigation. Apr, 2006. www.centerforhealthyhousing.org/Green_Analysis.pdf. [May 30;2010 ]. www.centerforhealthyhousing.org/Green_Analysis.pdf
- 72.National Center for Healthy Housing. Seven Principles of a Healthy Home. National Center for Healthy Housing. www.nchh.org/What-We-Do/Healthy-Homes-Principles.aspx. [May 29;2010 ]. www.nchh.org/What-We-Do/Healthy-Homes-Principles.aspx
- 73.U.S. Green Building Council's LEED for Homes. Apr, 2009. www.usgbc.org/DisplayPage.aspx?CMSPageID=147&. [May 30;2010 ]. www.usgbc.org/DisplayPage.aspx?CMSPageID=147&
- 74.National Association of Home Builders' NAHB Green Home Building Guidelines. 2007. www.nahb.org/generic.aspx?sectionID=222&genericContentID=56077. [May 30;2010 ]. www.nahb.org/generic.aspx?sectionID=222&genericContentID=56077
- 75.Enterprise Community Partner's Green Communities Criteria. 2008. www.greencommunitiesonline.org/tools/criteria. [May 30;2010 ]. www.greencommunitiesonline.org/tools/criteria
- 76.U.S. Environmental Protection Agency's (EPA) Energy Star with Indoor Air Package. Feb, 2008. www.energystar.gov/ia/partners/bldrs_lenders_raters/downloads/IAPBuild508.pdf. [May 30;2010 ]. www.energystar.gov/ia/partners/bldrs_lenders_raters/downloads/IAPBuild508.pdf
- 77.American Lung Association's Health House Builder Guidelines. www.alaw.org/air_quality/healthy_house_programs. [May 30;2010 ]. www.alaw.org/air_quality/healthy_house_programs
- 78.Howden-Chapman P. Matheson A. Crane J, et al. Effect of insulating existing houses on health inequality: Cluster randomised study in the community. BMJ. 2007;334:460–464. doi: 10.1136/bmj.39070.573032.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Burr ML. Matthews IP. Arthur RA, et al. Effects on patients with asthma of eradicating visible indoor mould: A randomised controlled trial. Thorax. 2007;62:766–771. doi: 10.1136/thx.2006.070847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kercsmar CM. Dearborn DG. Schluchter M, et al. Reduction in asthma morbidity in children as a result of home remediation aimed at moisture sources. Environ Health Perspect. 2006;114:1574–1580. doi: 10.1289/ehp.8742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Arlian L. Neal J. Morgan M, et al. Reducing relative humidity is a practical way to control dust mites and their allergens in homes in temperate climates. J Allergy Clin Immunol. 2001;107:99–104. doi: 10.1067/mai.2001.112119. [DOI] [PubMed] [Google Scholar]
- 82.Niven R. Fletcher AM. Pickering AC, et al. Attempting to control mite allergens with mechanical ventilation and dehumidification in British houses. J Allergy Clin Immunol. 1999;103(5 Pt 1):756–762. doi: 10.1016/s0091-6749(99)70416-1. [DOI] [PubMed] [Google Scholar]
- 83.Fletcher AM. Pickering CA. Custovic A, et al. Reduction in humidity as a method of controlling mites and mite allergens: The use of mechanical ventilation in British domestic dwellings. Clin Exp Allergy. 1996;26:1051–1056. doi: 10.1111/j.1365-2222.1996.tb00643.x. [DOI] [PubMed] [Google Scholar]
- 84.Harving H. Korsgaard J. Dahl R. Clinical efficacy of reduction in house-dust mite exposure in specially designed, mechanically ventilated “healthy” homes. Allergy. 1994;49:866–870. doi: 10.1111/j.1398-9995.1994.tb00789.x. [DOI] [PubMed] [Google Scholar]
- 85.Warner JA. Frederick JM. Bryant TN, et al. Mechanical ventilation and high-efficiency vacuum cleaning: A combined strategy of mite and mite allergen reduction in the control of mite-sensitive asthma. J Allergy Clin Immunol. 2000;105:75–82. doi: 10.1016/s0091-6749(00)90181-7. [DOI] [PubMed] [Google Scholar]
- 86.Jacobs DE, et al. An Evaluation of the Health Outcomes of Green and Healthy Housing Rehabilitation. Proceedings of the Healthy Buildings 2009 Conference, International Society of Indoor Air Quality; Sep 15;2009 . [Google Scholar]
- 87.National Center for Healthy Housing. Research. www.nchh.org/Home.aspx. [Jun 27;2010 ]. www.nchh.org/Home.aspx
- 88.Takaro TT. Krieger J. Song L. Sharify D. Beaudet N. The breathe easy home: impact of asthma-friendly home design and construction on asthma clinical outcomes and trigger exposure. American J Public Health. doi: 10.2105/AJPH.2010.300008. (accepted for publication). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project (HCUP) http://hcupnet.ahrq.gov/HCUPnet.jsp. [Jun 27;2010 ]. http://hcupnet.ahrq.gov/HCUPnet.jsp [PubMed]
- 90.Krieger J. Higgins DL. Housing and health: Time again for public health action. Am J Public Health. 2002;92:758–768. doi: 10.2105/ajph.92.5.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Thomson H. Thomas S. Sellstrom E. Petticrew M. The health impacts of housing improvement: A systematic review of intervention studies from 1887 to 2007. Am J Public Health. 2009;99(Suppl 3):S681–S692. doi: 10.2105/AJPH.2008.143909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.WHO. Large analysis and review of European housing and health status (LARES) 2007. www.euro.who.int/__data/assets/pdf_file/0007/107476/lares_result.pdf. [Jun 6;2010 ]. www.euro.who.int/__data/assets/pdf_file/0007/107476/lares_result.pdf