Abstract
Colorectal cancer (CRC) is one of the most common malignant tumours in Poland. Annually approximately 11 000 new cases of CRC are diagnosed, while the number of deaths caused by CRC approaches 8 000. Five-year survival does not exceed 20%. Familial adenomatous polyposis (FAP) is responsible for about 1% of new cases of CRC. The risk of CRC in FAP syndrome is 100%, and the average age of CRC development is 39 years. Early colectomy is the most effective method of CRC prevention. We report an atypical case of CRC in a patient with FAP caused by 2797-2800delAACA mutation of the APC gene.
Keywords: colorectal cancer, APC gene, FAP syndrome, adjuvant chemotherapy, colectomy, follow-up
Introduction
Colorectal cancer is one of the most common malignant tumours. Annually approximately 11 000 new cases of CRC are diagnosed in Poland, while the number of deaths caused by CRC approaches 8 000. Five-year survival does not exceed 20%. The majority of colorectal cancers originate from adenomas. The risk of malignant transformation of a benign lesion is approximately 2% annually. Large polyps, of at least 10 mm diameter, villous polyps and polyps with a high degree of dysplasia are at high risk of malignant transformation [1–4].
Gastrointestinal malignancies have a significant genetic background. Hereditary non-polyposis colorectal cancer (HNPCC) (accounts for approximately 10% of cases of colorectal cancer) and familial adenomatous polyposis syndrome (FAP) (1% of all colorectal cancer cases) are associated with hereditary high penetration mutations in DNA repair and tumour suppressor genes, respectively.
Familial adenomatous polyposis is caused by mutations of the suppressor gene APC (adenomatous polyposis coli – incidence 1/7500 – 1/10 000 in the general population) [5]. Familial adenomatous polyposis predisposes towards multiple polyps in the colon and rectum. The polyps appear starting from the second decade of life and undergo malignant transformation if untreated. The average age of tumour development in a FAP patient is 39 years. The risk of malignancy in FAP is essentially 100%. Total colectomy is the best management that minimizes the risk of colorectal cancer (when the rectum is left intact, there is a risk of rectal cancer) [6–8]. Polyps in the upper gastrointestinal tract are observed in such patients as well as non-gastrointestinal malignancies such as tumours of the thyroid and brain and desmoid tumours.
Hereditary mutations of the APC gene usually result in loss of function of one of the alleles. Small mutations, involving 1 to a few nucleotides, as well as larger mutations, involving respective exons or the whole APC gene, have been observed. The majority of APC gene mutations have been observed in the 5’ part of exon 15 of the APC gene [9, 10]. These mutations are associated with classic FAP form. Mutations of the initial gene sequence to exon 4, exon 9 and the 3’ part of exon 15 are associated with milder disease course referred to as attenuated adenomatous polyposis coli (AAPC) [11].
We present an atypical case of colorectal cancer in the course of FAP associated with “de novo” mutation of the APC gene, review literature related to FAP and provide genetic commentary.
Case report
A 25-year old female patient with cancer of the sigmoid colon was admitted to the Clinic of Oncology, Military Medical Institute in Warsaw, in February 2007, to undergo adjuvant chemotherapy.
On 1 January 2007 the patient was admitted to the Department of General Surgery with symptoms of subileus. Colonoscopy demonstrated a very large number of sitting and pedicular polyps, with diameter of 0.4 cm to 1.2 cm. Gastroscopy was unremarkable. Computed tomography imaging of the abdominal cavity and pelvis demonstrated intestinal obstruction and trace amounts of fluid in the Douglas cavity. She underwent a surgical operation on 13.01.2007 due to intestinal obstruction: her sigmoid colon was resected and permanent colostomy was performed.
Pathological evaluation:
macroscopic: a fragment of the large intestine 10 cm in length; a tumour completely obstructing the intestinal lumen is located 1 cm and 4 cm from the margins of surgical section;
microscopic: moderately differentiated adenocarcinoma (mucosal adenocarcinoma G2), infiltrating the full thickness of the intestinal wall and peri-intestinal fat tissue (T3) and metastases in the lymph nodes (2/9 lymph nodes with metastases – N1). The final diagnosis: pT3N1Mx – Aster – Coller C2 (TNM classification stage IIIB) [12, 13].
After the result was obtained, the patient was referred to the Clinic of Oncology of the Medical Military Institute in Warsaw to undergo further therapy. Due to associated adverse prognostic factors in the postoperative pathological examination (infiltration of the full thickness of the intestinal wall with infiltration of the peri-intestinal fat tissue, metastases in the lymph nodes) and intraoperative detection of a small amount of fluid in the peritoneal cavity (the fluid was not taken for cytological examination during the operation), the patient was qualified for adjuvant chemotherapy according to the regimen: oxaliplatin, 5-fluorouracil, leucovorin (FOLFOX) at doses: 85 mg/m2 day 1, 400 mg/m2 “bolus” day 1 and 2, and 600 mg/m2 day 1 and 2, 200 mg/m2 “bolus” day 1 and 2, respectively.
The patient received a total of 12 cycles of FOLFOX chemotherapy until August 2007. The maximal toxicity observed during chemotherapy was: grade 1 leucopenia, grade 1 neutropenia, grade 1 anaemia and grade 2 thrombocytopenia according to common toxicity criteria (CTC) that required 20% dose reduction (thrombocytopenia required delays of subsequent chemotherapy courses and thus after the 9th course the decision was taken to reduce doses of chemotherapy).
Due to the genetic aetiology of FAP, the patient was qualified for molecular testing of the APC gene to possibly detect an APC gene mutation and subject other members of her family to molecular testing.
Molecular analysis
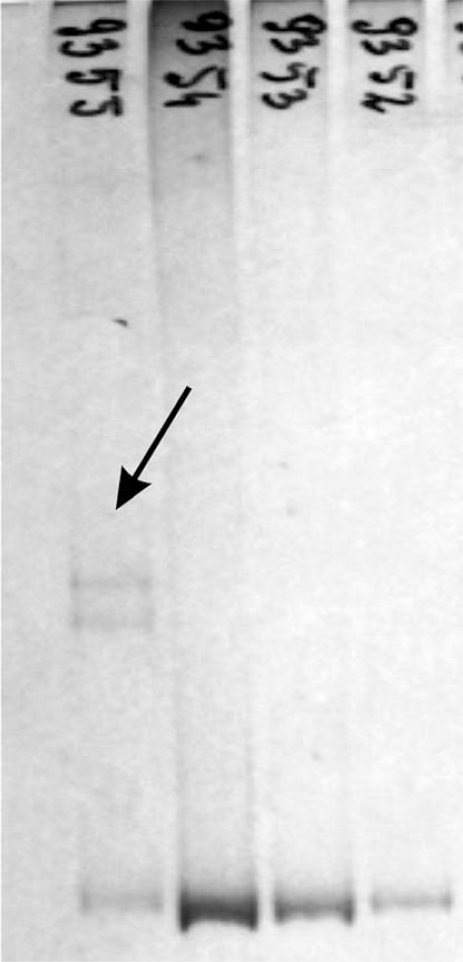
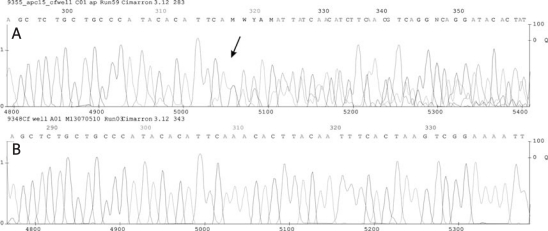
DNA was extracted from the peripheral blood cells using a phenol extraction method. The encoding sequence of the APC gene was analysed using the screening methods PCR-HD and PCR-SSCP [14]. Additional conformers were observed in the PCR-HD analysis of fragment C in exon 15 (Figure 1). This fragment was sequenced. Direct PCR sequencing was performed using DYEnamic ET-Terminator (Amersham-Bioscience). The reaction was performed according to the manufacturer's instructions. The product of the sequencing was separated on an automatic Megabace 500 sequencing system. The results were analysed using sequence analysis software (Amersham-Bioscience). A mutation, 2797-2800delAACA, was identified that shifted the reading frame and formation of the STOP signal in codon 953 (Figure 2). The detected mutation is a de novo mutation that has not yet been reported in other populations. Siblings of the proband did not have this mutation.
Figure 1.
PCR HD analysis of fragment C of exon 15 of the APC gene
Arrow indicates additional conformers in patient no. 9355 occurring in association with 2797-2800delAACA
Figure 2.
Sequencing of fragment G of exon 15 of the APC gene
A – patient 9355. B – control. Arrow indicates the site of 2797-2800delAACA
After completion of chemotherapy in September 2007, before a decision was made on further treatment, follow-up imaging examinations were performed: computed tomography imaging of the abdomen and pelvis (which did not demonstrate any lesions suspected of recurrence or dissemination of the disease) and colonoscopy that confirmed presence of multiple polyps in the large intestine; the two most suspicious polyps were removed.
Pathomorphological report:
microscopic: polyp from the transverse colon – tubular adenoma, resected completely; polyp from the sigmoid colon – highly differentiated adenocarcinoma, the cancer focus is on the top of the adenoma, the section line is in the unchanged mucosa.
Due to high risk of relapse of adenocarcinoma in the remaining polyps of the large intestine and in view of no recurrence or dissemination of the disease in the imaging studies, a decision was taken to proceed to surgical treatment after completion of the adjunctive therapy. On 24.10.2007 the patient underwent colectomy (the rectum was left intact since no polyps were visualized in the rectum) in the Clinic of Oncological Surgery and continuity of the gastrointestinal tract was restored.
Pathomorphological report:
macroscopic: large intestine with multiple polyps;
microscopic: numerous polyps with evidence of high degree dysplasia and two foci (in the transverse colon and sigmoid colon) of highly differentiated adenocarcinoma; no lymph node involvement was found (0/10 lymph nodes).
According to the characteristics of FAP syndrome, the follow-up assessments included: upper gastrointestinal endoscopy every 24 months, rectoscopy every 6-12 months and imaging studies every 12 months until 5 years after completion of the treatment (the last CT of the abdominal cavity and pelvis was performed in March 2008; no significant abnormalities were detected).
Discussion
Familial adenomatous polyposis (FAP) syndrome is an autosomal dominant disorder. It is responsible for 1% of cases of colorectal cancer. Its genetic background substantiates the use of molecular diagnosis, so that mutation carriers can be detected long before they develop clinical symptoms that make clinical diagnosis possible. The risk of developing FAP in an APC gene mutation carrier is essentially 100%. A screening programme should be developed for such persons to detect the polyps and then monitor them, to avoid cancer development. Another advantage of such programmes is that they alleviate constant stress in individuals who are not mutation carriers, in whom the cancer risk is as low as in the general population. Radical surgical operation is largely crippling but cannot be avoided. It is quite difficult to determine when it should be performed. It is a seriously crippling procedure should it not be performed too early, because polyps in intestinal polyposis take longer to develop cancer than with HNPCC; however, too long delay may lead to cancer. FAP is characterized by high variability. This phenomenon is typical not only for carriers of the same mutation but also for members of a single family who also carry the same mutation [4]. Studies correlating genotype and phenotype have been carried out for years and a pattern can be observed. However, deviations that have been observed from this pattern lead to the situation that identification of a certain mutation and its correlation with a specific disease course cannot be the sole reason for therapeutic consequences. The management and dates of possible procedures must be determined on the basis of examinations concerning a particular patient and they cannot be used in other carriers of the same mutation due to the variable course of the disease [12]. Some authors suggest that phenotype inter-patient variability with respect to various APC gene mutations can be explained by the proposed “just right” signalling model related to abnormal regulation of β-catenin levels. Proper accumulation of β-catenin in the cell nucleus leads to activation of transcription factor and promotes tumour growth [15, 16]. According to some authors, colorectal bleeding and frequent diarrhoea are the most common specific (“intestinal”) symptoms related to the large intestine polyps in this syndrome, while “non-specific intestinal” symptoms include abdominal pain and weight loss and weakening [6, 11].
The patient had no prior complaints that could suggest multiple polyps that usually accompany FAP syndrome. This could have been related to the polyp size (the largest one measured 1.2 cm). Subileus was its first symptom but was related to the tumour obstructing the intestinal lumen rather than the polyps themselves.
The presence of unfavourable prognostic factors in the postoperative histopathological testing was the reason for adjuvant chemotherapy given after the first surgical procedure for intestinal obstruction. These factors were associated with high probability of disseminated disease. And so the surgical procedure (prophylactic colectomy) was delayed until the chemotherapy had been completed and disease relapse and dissemination had been ruled out.
The prognosis in early FAP is favourable. The patients can live for many years after a prophylactic surgical procedure. Unfortunately, with time some patients develop malignancies in other locations: in the stomach, duodenum, small intestine, or mesentery (desmoid tumours).
Oncological follow-up and endoscopic follow-up of the upper gastrointestinal tract and rectoscopic follow-up are very important in these patients. One must not forget to perform genetic testing of close family members (siblings, children, parents).
The longest follow-up reported in the available literature is 18 years (on average 14 years). Eight patients died out of the group of 110 patients (62 males and 48 females): 2 due to colorectal cancer that developed prior to proctocolectomy, 2 due to complications related to desmoid tumours, 2 due to primary adenocarcinoma of the lung, 1 due to complications during the first day after the operation and 1 for reasons unrelated to APC or its treatment. Fourteen patients were lost to follow-up. APC mutation was detected in 50 families [17].
Our patient was diagnosed with colorectal familial adenomatous polyposis and a pathogenic APC gene mutation was identified in her. This mutation is a novel mutation that has not been previously reported in any population. Lack of previous reports for this mutation and its de novo occurrence in the family make it impossible to compare the disease course. However, mutations in this region of the APC gene usually cause the classic form of colorectal polyposis. The reported case is not different from this form of the disease. Polyps could have appeared in the second decade of the patient's life or at its end. Their small size did not cause mechanical intestinal dysfunction, observed with larger polyps. What should be noted is that the tumour developed out of only one of multiple polyps, reaching a very large size. It is difficult to speculate whether the tumour developed from a polyp, or it was a sporadic tumour at a young age. However, the latter are very rare. The reported case may indicate that a variable rate of tumour development occurs not only between different patients, but also between different tumours in the same patient [18]. Thus we can conclude that prophylactic colectomy should be considered in hereditary predisposition to malignancies despite small polyps, due to the risk that one of the polyps may undergo a rapid malignant transformation.
References
- 1.Sciallero S, Bonelli L, Aste H, et al. Do patients with rectosigmoid adenomas 5 mm or less in diameter need total colonoscopy? Gastrointest Endosc. 1999;50:314–21. doi: 10.1053/ge.1999.v50.97110. [DOI] [PubMed] [Google Scholar]
- 2.Patel K, Hoffman NE. The anatomical distribution of colorectal polyps at colonoscopy. J Clin Gastroenterol. 2001;33:222–5. doi: 10.1097/00004836-200109000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Velayos Jimenez B, Duran Rigueira M, Arevalo Serna JA, et al. Distribution of polyps in the inside region of Vizcaya (Spain): implications for diagnostic tests and colorectal cancer screening. Gastroenterol Hepatol. 2003;26:401–6. doi: 10.1016/s0210-5705(03)70380-x. [DOI] [PubMed] [Google Scholar]
- 4.Lewis JD, Ng K, Hung KE, et al. Detection of proximal adenomatous polyps with screening sigmoidoscopy: a systematic review and meta-analysis of screening colonoscopy. Arch Intern Med. 2003;163:413–20. doi: 10.1001/archinte.163.4.413. [DOI] [PubMed] [Google Scholar]
- 5.Groden J, Thliveris A, Samowitz W, et al. Identification and characterization of the familial adenomatous polyposis coli gene. Cell. 1991;66:589–600. doi: 10.1016/0092-8674(81)90021-0. [DOI] [PubMed] [Google Scholar]
- 6.Croner SR, Brueckl MW, Reingruber B, Hohenberger W, Guenther K. Age and manifestations related symptoms in familial adenomatous polyposis. BMC Cancer. 2005;5:1–7. doi: 10.1186/1471-2407-5-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nowacki MP. Rak jelita grubego. In: Krakowski M, editor. Zalecenia postępowania diagnostyczno-terapeutycznego w nowotworach zlosliwych [Polish] Gdansk: Wydawnictwo Via Medica; 2007. pp. 153–7. [Google Scholar]
- 8.Boardman LA, Schmidt S, Lindor NM, et al. A search for germline APC mutations in early onset colorectal cancer or familial colorectal cancer with normal DNA mismatch repair. Genes Chromosomes Cancer. 2001;30:181–6. [PubMed] [Google Scholar]
- 9.Plawski A, Lubinski J, Banasiewicz T, et al. Novel germline mutations in the adenomatous polyposis coli gene in Polish families with familial adenomatous polyposis. J Med Genet. 2004;41:e11. doi: 10.1136/jmg.2003.010215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Plawski A, Podralska M, Slomski R. Recurrent APC gene mutations in Polish FAP families. Heredit Cancer Clin Pract. 2007;5:195–8. doi: 10.1186/1897-4287-5-4-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nandakumar G, Morgan JA, Silverberg D, Steinhagen M. Familial polyposis Coli: clinical manifestations, evaluation, management and treatment. Mt Sinai J Med. 2004;71:384–91. [PubMed] [Google Scholar]
- 12.Astler VB, Coller FA. The prognostic significance of direct extension of carcinoma of the colon and rectum. Ann Surg. 1954;139:846–52. doi: 10.1097/00000658-195406000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nowacki MP. Rak jelita grubego. In: Krzakowski M, editor. Onkologia kliniczna [Polish] Warszawa: Wydawnictwo Medyczne Borgis; 2006. p. 894. [Google Scholar]
- 14.Plawski A, Jura J, Slomski R. Wykrywanie mutacji punktowych w genie supresorowym APC człowieka metodŐ heterodupleksów [Polish] Przykłady analiz DNA. 2001:80–9. [Google Scholar]
- 15.Albuquerque C, Breukel C, Van der Luijt R, et al. The “just-Right” signaling model: APC somatic mutations are selected based on a specific level of activation of the beta-catenine signaling cascade. Hum Mol Genet. 2002;11:1549–60. doi: 10.1093/hmg/11.13.1549. [DOI] [PubMed] [Google Scholar]
- 16.Scott RJ. Familial adenomatous polyposis (FAP) and other polyposis syndromes. Heredit Cancer Clin Pract. 2003;1:19–30. [Google Scholar]
- 17.Parc Y, Piquard A, Dozis RR, Parc R, Tiret E. Long-term outcome of familial adenomatous polyposis patients after restorative coloproctectomy. Ann Surg. 2004;239:378–82. doi: 10.1097/01.sla.0000114216.90947.f6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Plawski A, Nowakowska D, Podralska M, et al. The AAPC case, with an early onset of colorectal cancer. Int J Colorectal Dis. 2007;22:449–51. doi: 10.1007/s00384-006-0146-1. [DOI] [PubMed] [Google Scholar]