Abstract
Objective:
This study evaluated the costs and cost-effectiveness of combining motivational interviewing with feedback to address heavy drinking among university freshmen.
Method:
Microcosting methods were used in a prospective cost and cost-effectiveness study of a randomized trial of assessment only (AO), motivational interviewing (MI), feedback only (FB), and motivational interviewing with feedback (MIFB) at a large public university in the southeastern United States. Students were recruited and screened into the study during freshman classes based on recent heavy drinking. A total of 727 students (60% female) were randomized, and 656 had sufficient data at 3-months’ follow-up to be included in the cost-effectiveness analysis. Effectiveness outcomes were changes in average drinks per drinking occasion and number of heavy drinking occasions.
Results:
Mean intervention costs per student were $16.51 for MI, $17.33 for FB, and $36.03 for MIFB. Cost-effectiveness analysis showed two cost-effective interventions for both outcomes: AO ($0 per student) and MIFB ($36 per student).
Conclusions:
This is the first prospective cost-effectiveness study to our knowledge to examine MI for heavy drinking among students in a university setting. Despite being the most expensive intervention, MIFB was the most effective intervention and may be a cost-effective intervention, depending on a university’s willingness to pay for changes in the considered outcomes.
Alcohol use among college students is a major public health problem and continues to attract the attention of policy makers (National Institute on Alcohol Abuse and Alcoholism [NIAAA], 2007; Wechsler and Nelson, 2008). Excessive drinking among college students is associated with near-term events, including accidents and reduced academic performance, which have negative long-term effects (Perkins, 2002). Students have been shown to experience lasting harm from drinking, even though many who drink in excess eventually mature out of the behavior (Schulenberg et al., 1996; Weingardt et al., 1998).
Among college students, those who have recently transitioned from high school are particularly vulnerable (Bachman et al., 1997). Freshman students often have fewer restrictions on behavior while living on a college campus than while living at home attending high school, in part because of changes to their set of informal social influences (Arnett, 2005). Many colleges have a culture that reinforces heavy drinking (White and Jackson, 2004/2005). Given the challenges to reducing heavy drinking among freshmen in particular, interventions that effectively address behaviors among this group are needed.
Many studies have examined the effectiveness of brief interventions using motivational interviewing (MI) to reduce heavy drinking among college students. MI is a directive, client-centered counseling style for eliciting behavior change by helping clients to explore and resolve ambivalence (Miller and Rollnick, 2002). Most of these studies found reduced drinking among students (Baer et al., 2001; Larimer and Cronce, 2002, 2007; Murphy et al., 2004; Schaus et al., 2009; Tevyaw et al., 2007; Turrisi et al., 2009; Walters et al., 2009; White et al., 2006), and some found reduced drinking among freshmen specifically (e.g., Baer et al., 2001).
Evidence also suggests that motivational interviewing combined with feedback (MIFB) is particularly successful (Clinton-Sherrod et al., 2011; Walters et al., 2009). Feedback involves providing information on personal drinking patterns, comparisons of the student’s drinking patterns with drinking norms, risk factors for heavy drinking, and the harm of heavy drinking. Some studies indicate that feedback alone may reduce problem drinking (Agostinelli et al., 1995; Collins et al., 2002; Larimer and Cronce, 2007; Neighbors et al., 2004; Walters, 2000; Walters et al., 2000, 2007).
Despite increasing attention to student drinking from policy makers and despite the number of studies examining the effectiveness of interventions, little is known about the degree to which interventions for college students—with or without feedback—can be justified fiscally. Several studies reviewing the literature suggest that brief interventions, many of which use MI, can be cost-effective in reducing alcohol use across a number of populations (Broskowski and Smith, 2001; Coffield et al., 2001; Cowell et al., 2010; Latimer et al., 2009; Solberg et al., 2008). To our knowledge, however, there are no published economic evaluations of MI for drinking among college students.
Evidence on alcohol use in other settings and evidence on behaviors other than drinking suggest that MI may be cost-effective. A recent study focusing on youth in a hospital emergency department setting found that, compared with usual care, MI is cost-effective in reducing alcohol consumption (Neighbors et al., 2010). MI has also been shown to be cost-effective in reducing consumption of other substances, such as tobacco (Ruger et al., 2008). However, these studies were not in college settings, and therefore no direct evidence exists on the costs or effectiveness of such interventions in a college setting. The evidence to date thus provides insufficient guidance on how much decision makers should be willing to invest to reduce harm from drinking among students.
The current study addresses this important gap in the literature. It presents the results of a cost-effectiveness analysis (CEA) using combinations of MI and feedback to reduce heavy drinking in a college setting: assessment only (AO), MI, feedback only (FB), and MIFB. CEA compares the intervention arms within a study to describe the additional cost required to achieve a given gain in the outcome compared with the next best alternative intervention, where the outcome is expressed in some form of natural unit (e.g., average number of drinks per drinking day). An alternative approach, cost-benefit analysis, measures outcomes in dollar terms. However, because health outcomes are particularly difficult to monetize (Drummond et al., 2005), CEA is preferred and used in the current study.
The current study has two important features. First, it focuses on immediate drinking outcomes. It is first necessary to establish an impact of such interventions on drinking before the impact on consequent outcomes—such as accidents, academic performance, and employment—can be assessed. Second, study participants are freshman students, who are particularly vulnerable to negative consequences of heavy drinking.
Method
Overview
The perspective of the analysis determines the costs and outcomes used in the CEA, and answers the question, whose costs are compared with whose effectiveness? This study takes the perspective of the intervention provider, the university. The university covers the immediate costs of intervention services and has primary stake in reducing problem drinking among students. Costs that are realized in the longer term were considered secondary and excluded, including employment after college, general health care costs associated with drinking and its consequences, criminal justice costs of behavior related to drinking, and any labor market impact of school performance. Effectiveness was assessed using measures of drinking in the short term, 3 months after baseline. All cost estimates are presented in 2009 U.S. dollars (2009 was the last year of the study). The study was conducted under Department of Health and Human Services regulations for the protection of human subjects. The research plan, operational protocols, instrumentation, and consent forms were reviewed and approved by internal institutional review boards at the authors’ institution and the university from which participants were recruited.
Sample and procedures
The sample and study procedure and design are detailed elsewhere (Clinton-Sherrod et al., 2011). Here we summarize the key features.
Participants were recruited from a large public university in the southeastern United States between October 2005 and April 2009. Students were recruited by graduate assistants (GAs) during freshman classes. Informed consent was given at recruitment during class. Students were screened into the study if they had at least one heavy drinking episode (five or more drinks on an occasion for men and four or more drinks on an occasion for women) during the past 2 weeks. Excluded were part-time students, nonfreshmen, students who had received treatment or counseling for drug or alcohol use, those with a history of head injury, and those with a current diagnosis of a mental health disorder. Within 1 month of recruitment, participants completed a computer-administered baseline assessment and were randomized to one of four intervention conditions. The baseline assessment contained an extensive array of measures of demographics, school performance, alcohol use, peak estimated blood alcohol concentration (eBAC), and other related factors. Participants also were invited to complete briefer assessments of drinking and other behaviors by Internet survey 3, 6, and 12 months after baseline. Because evidence suggests that the strongest effect for a brief intervention is at 3 months, with steady decline over time in group differences and in maintaining lower drinking levels (Carey et al., 2009; Cunningham et al., 2010; Schaus et al., 2009), the current study used the effectiveness measures at the 3-month follow-up. Incentives to participate were $10 for the initial baseline assessment and $20 for the 3-month follow-up assessment.
The four intervention conditions used an assessment with combinations of MI and feedback. In the AO condition, participants completed the baseline assessment only and received no intervention or feedback. Participants randomized to the AO condition received feedback at the end of the study (i.e., after the 12-month follow-up). In the MI condition, participants received a single, brief (30- to 45-minute) counseling session (as described in Miller and Rollnick, 1991, 2002). MI was delivered by trained GAs in a student counseling center office soon after assessment. For the FB condition, the feedback report was automatically generated using baseline assessment data, formatted by the GA, and then e-mailed to the participant 1 week after the baseline assessment. The MIFB condition consisted of the counseling delivered in the MI condition and a review of the report used in the FB condition.
A total of 727 students provided baseline data and were randomized into an intervention condition. Of these, 657 participants provided data at the 3-month followup; 1 participant was dropped because data on a baseline covariate were missing. Thus, the analysis sample was 656. At baseline, nearly 60% of participants were women, almost all (99%) were younger than age 20, and most were White (87%) and living in a residence hall (91%). Drinking was heavy among the sample. The eBAC peak value of participants from a 30-day timeline feedback was 223 mg/dl, with 90% of participants exceeding the limit for being prosecuted for driving while intoxicated on at least 1 day (McMillen et al., 2009).
In the main study, five outcomes were examined, each with reference to the past 30 days: average number of drinks per drinking episode, number of heavy episodic drinking days, number of days with any drinking, maximum drinks in a drinking episode, and peak eBAC. For each outcome and study group, drinking was lower at follow-up than at baseline. Comparing study arms, the reduction in drinking was typically greater for MIFB and lower for AO. Compared with AO, MIFB had statistically significantly lower average drinks per drinking episode and fewer heavy episodic drinking days. No differences were significant for the other three outcomes (Brown et al., 2011, unpublished data).
Cost data
Costs were placed into two exclusive categories: variable and fixed. Both types of costs are the product of quantity (number of hours or number of units) and price (per hour or per unit). Variable costs are proportional to the number of participants and are incurred in delivering the intervention to each participant (e.g., the cost of delivering MI). Importantly, these variable costs were compared with effectiveness and entered directly into the CEA. Fixed costs comprise computer equipment and staff training costs and do not vary proportionally with the number of participants. These fixed costs did not enter directly into the CEA for three reasons. First, the fixed costs do not vary across the active interventions (MI, FB, and MIFB). Second, the current study examined immediate, short-term outcomes. By definition, fixed costs cannot be affected in a short period and are thus omitted from this analysis. Third, the number of participants over which fixed costs would be spread would be somewhat arbitrary and not necessarily equal to the number of study observations.
The estimates exclude costs incurred only in conducting the research and not in supporting the delivery of interventions. For example, project administration costs (e.g., processing and mailing incentives or scheduling) are not included in this study. Also, scales of stages of readiness to change behavior were used in analyses, but the scales were not intended to be directly used in supporting MI or FB, and they would not be used if there were no research study; the cost of collecting data using these scales was thus omitted from the study.
Fixed costs.
Although fixed costs are not directly compared with effectiveness in the analyses, they are reported separately so that the resources needed to set up and deliver the interventions are documented. The quantity and price of the computers used by participants to complete assessments were directly available in study records. The cost of training GAs in MI included both formal and informal on-the-job training and the cost of the GAs’ and trainer’s time. All staff received formal training. By using graduate students as staff, the multiyear study experienced regular staff turnover as students graduated, and existing GAs provided on-the-job training to incoming GAs. Training time was collected using logs tracking the number of hours spent in formal and informal training. The trainees’ (GAs’) and the trainer’s pay for training time was available in study records. The pay was loaded with administrative overhead of the host institution, which covered the use of the host building, nonstudy equipment, library, and costs of general operations, maintenance, and administration.
Variable costs.
The amount of time spent on the different intervention activities was collected prospectively using logs that recorded the start and end times for each participant by intervention condition. The loaded hourly pay of each GA conducting the intervention was obtained as described for fixed costs.
Effectiveness data
The two effectiveness measures used in the current study were those for which the interventions were found to have significant impact in previous analyses (presented in Brown et al., 2011, unpublished data): average drinks per drinking occasion and heavy episodic drinking. Average drinks per drinking occasion is the mean number of drinks a participant consumed per drinking occasion during the past month. Participants could report more than one drinking occasion on a drinking day. Heavy episodic drinking is the number of days during the past month on which men reported drinking five or more drinks on an occasion and women reported drinking four or more drinks on an occasion. These and other outcome measures were collected using a method similar to the Timeline Followback and the Form 90 manual (Miller and Tonigan, 1996; Sobell et al., 1988).
Other measures collected at baseline and follow-up were not included in this analysis because there were no differences between AO and the more expensive three intervention arms (MI, FB, and MIFB) (Brown et al., 2011, unpublished data); thus, further CEA was not conducted for these outcomes (Drummond et al., 2005; Gold et al., 1996). Those other outcome measures were alcohol quantity and frequency, eBAC, the number of days during the past month on which the participant drank any alcohol, and the largest number of drinks consumed by a participant on a drinking day during the past month.
Analysis
Estimating costs.
Total fixed costs are the sum of training costs and computer equipment costs. Variable costs were calculated at the individual client level and comprise the value of the time spent by GAs conducting three interventions: MI, FB, and MIFB. The cost of any MI component was the product of the hours spent providing an intervention by a GA and the GA’s loaded wage rate. The cost of the FB component was driven by the time GAs spent overseeing the data entry by participants for feedback reports and was estimated similarly to the MI component. The inputs to the feedback report were taken from the baseline assessment; therefore, the estimate excluded time spent on the research-specific components of the assessment. Thus, the FB cost included the time GAs spent monitoring clients to collect data for the feedback report. Adjustments were made to the FB cost in cases where a GA monitored more than one client simultaneously. The cost estimate used in the main analysis assumed that the AO had zero cost because information gathered in the assessment was not used for any treatment given to the AO students. Feedback input costs only factor into treatment arms with feedback (FB, MIFB). In the sensitivity analyses, described below, we varied our assumptions about the time and cost of collecting data for the feedback report.
Estimating impact on costs.
The effect of the intervention on cost was estimated using multivariate regressions with the dependent variable as the cost of the intervention delivered. In addition to indicators for each intervention (with AO as the omitted reference category), the model included three covariates that were identified as significant and meaningful in the main outcomes analysis (Brown et al., 2011, unpublished data): gender, age at initial drinking, and high school drinking frequency.
Estimating impact on effectiveness.
The impact on effectiveness was estimated using the same approach, specification, and outcomes described in Brown et al. (2011, unpublished data). Robust regression was used to assess the association between binary indicators of MI, FB, and MIFB and changes in each outcome. The regression method accounted for outliers in the outcomes that otherwise skewed the mean. Analyses were completed in Stata Version 11.0 (StataCorp LP, College Station, TX).
Cost-effectiveness analysis.
The CEA consists of three main steps: calculating incremental cost-effectiveness ratios, deriving cost-effectiveness acceptability curves (CEACs), and estimating the expected value of perfect information (EVPI) (Barton et al., 2008; Fenwick et al., 2001). When calculating incremental cost-effectiveness ratios, a treatment arm was excluded from the cost-effective choice set if it (a) was both more expensive and less effective than the other interventions, or (b) had a higher incremental cost-effectiveness ratio than a more expensive treatment arm.
The incremental cost-effectiveness ratio expresses how much more would have to be paid to achieve a given improvement in the outcome when comparing two interventions. Every intervention included an assessment; therefore, the cost of the assessment did not factor into the incremental cost calculations. Importantly, having every arm include an assessment component meant the results could not be used to compare, for example, MIFB or AO with the costs and outcomes from having no assessment; thus, the current study cannot be used to determine whether assessment alone is cost-effective.
Because the incremental cost-effectiveness ratio is a ratio of two random variables, rather than using a standard error or confidence interval, sampling variability is shown via CEACs. CEACs show the probability that an intervention is cost-effective relative to the alternative interventions for a given willingness to pay for a unit change in the effectiveness outcome (Barton et al., 2008; Fenwick et al., 2001; Zarkin et al., 2008). Nonparametric bootstrap methods were used to calculate CEACs for changes in each effectiveness outcome. The EVPI uses some of the calculations from the CEACs to estimate the most that a provider should be willing to pay for future research that would eliminate any uncertainty as to which treatment is optimal (Barton et al., 2008; Fenwick et al., 2001; Koerkamp et al., 2006).
Sensitivity analysis.
Sensitivity analyses were conducted to see how changing the assumptions that were made in the analysis would affect the conclusions of the study. Two sources of variation in costs were explored. First, the cost per intervention per client was varied by 20% or more, which is an accepted precedent in the cost-effectiveness literature (Neighbors et al., 2010). Second, the time that GAs spent monitoring clients to obtain the inputs to the feedback report was omitted because these inputs were obtained during the baseline assessment.
Results
Table 1 presents the amount spent on fixed costs in 2009 dollars. Nearly 90% of the fixed costs were for training. The training cost per staff person (GA) was lower for the replacement GAs than for the initial training because replacement GAs received on-the-job training that displaced some formal training.
Table 1.
Fixed costs
| Cost category | Cost per trainee | Number trained | Total cost |
| Original staff | $2,580.45 | 3 | $7,741.35 |
| Replacement staff | $1,692.35 | 16 | $27,077.60 |
| Total staff training | – | 19 | $34,818.95 |
| Equipment cost | – | – | $4,995.06 |
| Total fixed cost | – | – | $39,814.01 |
Notes: All costs are in 2009 U.S. dollars.
Table 2 presents the average amount of GA time spent on the interventions and the cost per intervention (in 2009 dollars), broken into the intervention activities. With regard to time per intervention, both feedback activities—assisting and monitoring the clients while completing the feedback portion of the assessment and preparing the feedback report—took approximately the same amount of time for the two interventions that used feedback. The motivational interviews took slightly longer for the MIFB group (M = 38.05 minutes) than for the MI-only group (M = 33.27 minutes). The total staff time for the FB (M= 34.93 minutes) and MI-only (M = 33.27 minutes) groups are similar, with the FB group taking a mean of 1.66 minutes longer. The MIFB group took the longest at a mean of 72.60 minutes of staff time, which is consistent with this intervention requiring time preparing and reporting feedback and time delivering a motivational interview session.
Table 2.
Time and cost per intervention, M (SD)
| Activity | Time per intervention, in min. |
Cost per interventiona |
||||
| FB (n = 170) | MI (n = 165) | MIFB (n = 154) | FB (n = 170) | MI (n = 165) | MIFB (n = 154) | |
| Monitoring participant | 16.60 | – | 15.86 | $8.24 | – | $7.87 |
| (5.73) | – | (6.33) | (2.84) | – | (3.14) | |
| Preparing feedback report | 18.33 | – | 18.70 | $9.10 | – | $9.28 |
| (9.10) | – | (9.57) | (4.52) | – | (4.75) | |
| Conducting MI | – | 33.27 | 38.05 | – | $16.51 | $18.88 |
| – | (9.83) | (10.66) | – | (4.88) | (5.29) | |
| Total | 34.93‡ | 33.27‡ | 72.60*† | $17.33‡ | $16.51‡ | $36.03*† |
Notes: Min. = minutes; FB = feedback only; MI = motivational interviewing; MIFB = motivational interviewing with feedback. FB vs. MI: 333 df. FB vs. MIFB: 322 df. MI vs. MIFB: 317 df.
Cost per intervention is in 2009 U.S. dollars.
p < .01 vs. FB (t test);
p < .01 vs. MI only (t test);
p < .01 vs. MIFB (t test).
With regard to cost, MI was the cheapest intervention at $16.51, with FB only slightly higher at $17.33. The cost of MIFB ($36.03) is roughly twice the cost of FB and MI. The difference in cost between FB and MI was not statistically significant. The costs of FB and MI were statistically significantly different from MIFB at the 1% level of significance.
The results of the CEA are shown in Table 3. The changes in effectiveness associated with each treatment are displayed in data columns 3 and 5. The estimates are the change in the average weighted predicted outcome between baseline and the 3-month follow-up, controlling for gender, age at initial alcohol use, and high school drinking frequency in a robust regression. There was no predicted change in average drinks per drinking occasion between baseline and the 3-month follow-up for AO. FB had an average weighted predicted decrease of 0.36 drinks per drinking occasion, MI had an average weighted predicted decrease of 0.29 drinks per drinking occasion, and MIFB had an average weighted predicted decrease of 0.77 drinks per drinking occasion. For the change in heavy drinking days, AO had the smallest average weighted predicted decrease in heavy drinking days between baseline and the 3-month follow-up (1.29), and FB (1.48) and MI (1.35) had decreases slightly larger than AO. MIFB had the largest average weighted predicted decrease (1.85) in heavy drinking days.
Table 3.
Cost-effectiveness analysis
| Treatment | Mean cost (C) | Decrease in average drinks |
Decrease in heavy drinking days |
||
| Mean effectiveness (E) | ICER (∆C/∆E) | Mean effectiveness (E) | ICER (∆C/∆E) | ||
| AO | $– | −0.003 | – | 1.288 | – |
| (0.024) | (0.039) | ||||
| MI | $16.51 | 0.286 | Economically | 1.354 | Economically |
| (0.38) | (0.023) | dominated | (0.040) | dominated | |
| FB | $17.33 | 0.360 | Economically | 1.475 | Economically |
| (0.46) | (0.022) | dominated | (0.040) | dominated | |
| MIFB | $36.03 | 0.769 | $47.04 | 1.848 | $64.34 |
| (0.56) | (0.026) | (0.044) | |||
Notes: Standard error of estimate in parentheses. All costs are in 2009 U.S. dollars. An economically dominated intervention either is more expensive and less effective than another or has a higher calculated incremental cost-effectiveness ratio (ICER) than the next most expensive. Economically dominated interventions were removed from consideration in the analysis. AO = assessment only; MI = motivational interviewing; FB = feedback only; MIFB = motivational interviewing with feedback.
Because AO is the least expensive intervention, it has no incremental cost; AO is also the least effective treatment option in bringing about change in both outcomes. MIFB is the most expensive treatment option and is the most effective option for both study outcomes. MI and FB are not in the cost-effective choice set for both study outcomes, leaving only AO and MIFB for incremental cost-effectiveness ratio calculations. Going from AO to MIFB costs $47.04 for a one-drink decrease in average drinks per drinking occasion and $64.34 for a 1-day decrease in the number of heavy drinking days in the past 30 days.
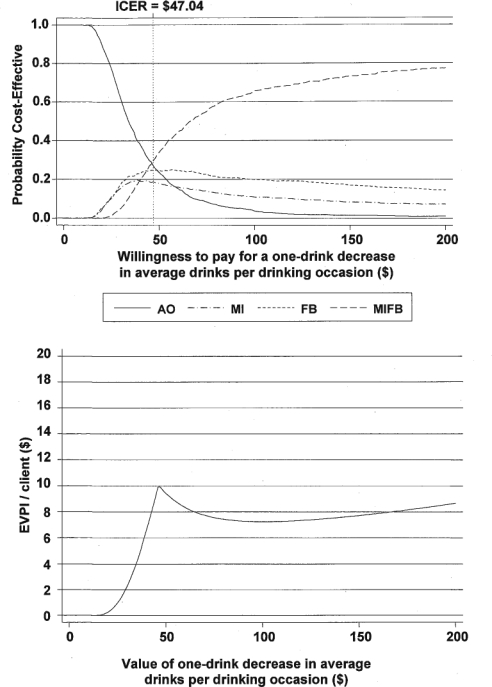
If the university would pay up to $47 for a one-drink reduction in average drinks per drinking episode, AO has the highest probability of being cost-effective relative to the other three interventions (Figure 1 [top chart]). Above the $47 value, MIFB has the highest probability of being cost-effective, and as a change in average drinks is increasingly valued, the probability that MIFB is cost-effective approaches .80. MI and FB have low probabilities of being cost-effective over the full range of values of changes in average drinks.
Figure 1.
Cost-effectiveness acceptability curves and expected value of perfect information (EVPI) for changes in average drinks per drinking occasion. ICER = incremental cost-effectiveness ratio; AO = assessment only; MI = motivational interviewing; FB = feedback only; MIFB = motivational interviewing with feedback.
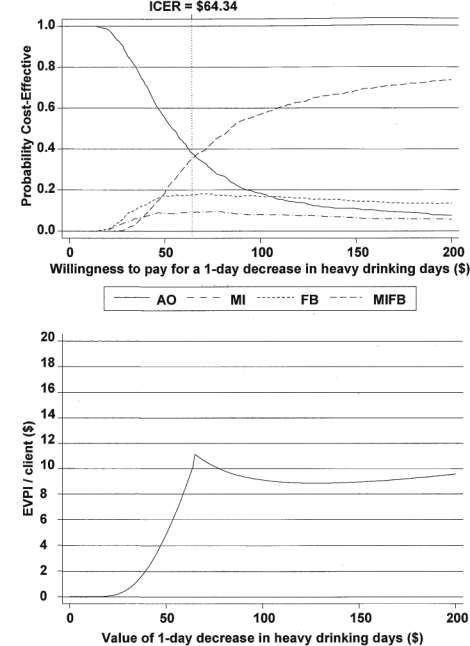
For heavy drinking days, AO has the highest probability of being cost-effective relative to the alternative interventions as long as the university was willing to pay only up to $64 for one less heavy drinking day (Figure 2 [top chart]). MIFB has the highest probability of being cost-effective above a value of $64, with that probability approaching .75 as willingness to pay increases. Again, MI and FB have low probabilities of being cost-effective over the full range of values of changes in average drinks.
Figure 2.
Cost-effectiveness acceptability curves and expected value of perfect information (EVPI) for changes in heavy drinking days. ICER = incremental cost-effectiveness ratio; AO = assessment only; MI = motivational interviewing; FB = feedback only; MIFB = motivational interviewing with feedback.
In Figure 1, at low valuations of a change in average drinks, the decision maker is very likely to adopt AO. Thus, additional information is unlikely to change the decision about adopting AO, and the EVPI is zero (bottom chart). As outcomes become more highly valued, the decision maker is willing to pay more to achieve the outcome, and he or she is also willing to finance research that reduces the uncertainty regarding which treatment is more cost-effective. The peak EVPI of $10 per student around a value of the outcome of $45 occurs when there is the least certainty about whether to adopt or reject MIFB based on current evidence (the probability any treatment is cost-effective is between .20 and .30). As the valuation of the change in average drinks increases beyond $47, the EVPI decreases initially and then increases as the probability that MIFB is cost-effective gradually levels off at about .80. The EVPI for the change in heavy drinking days follows a similar pattern (see bottom chart in Figure 2).
Sensitivity analysis
The first sensitivity analysis examined the effect of increasing/decreasing costs by 20%. The results indicated that because the proportional change in costs was the same across interventions, their relative rankings by cost did not change, and AO and MIFB remain the only treatments in the cost-effective choice set. The incremental cost-effectiveness ratios from AO to MIFB in each of these analyses increased or decreased by 20%, and the CEAC was shifted right or left.
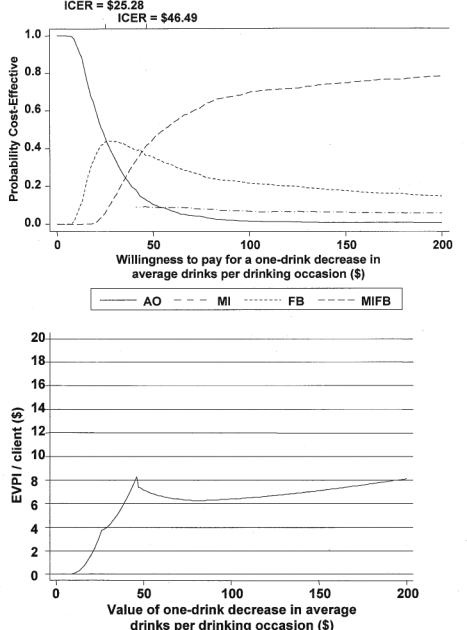
The sensitivity analysis in which the GAs’ time monitoring clients was set to zero reduced the mean costs of FB and MIFB. This analysis changed the interventions in the cost-effective choice set from the main analysis for average drinks but not to a great degree for heavy drinking. The difference between the impact on the outcomes can be explained by heavy drinking being less sensitive to changes in costs. For both outcomes, AO, FB, and MIFB were now in the cost-effective choice set, whereas in the main analysis FB did not appear in this choice set. For average drinking days, the range of valuations over which FB could be considered optimal is sizeable (Figure 3). For valuations between ∼$25 and ∼$46, FB had a high probability of being optimal. Below a valuation of $25 for this outcome, AO has the highest probability of being cost-effective, and, above a valuation of $46, MIFB has the highest probability of being cost-effective. For heavy drinking, the range of valuations over which FB could be considered optimal was negligible; for the sake of brevity, this Figure is omitted. The EVPI for this sensitivity analysis follows a similar trend to the main analysis (see Figure 3).
Figure 3.
Cost-effectiveness acceptability curves and expected value of perfect information (EVPI) for the change in average drinks per drinking occasion with adjusted feedback input costs. ICER = incremental cost-effectiveness ratio; AO = assessment only; MI = motivational interviewing; FB = feedback only; MIFB = motivational interviewing with feedback.
Discussion
This study found that combining MI and FB as a single intervention (MIFB) when delivered by a GA in a college counseling service setting was cost-effective at reducing average number of drinks per drinking day and heavy episodic drinking among students. This intervention was compared with three other study arms: MI alone, FB alone, and no intervention (AO). The analysis demonstrates the cost in dollars of using MIFB to get a one-unit improvement when compared with the next best alternative, FB. The results thus indicated that using MIFB cost $47 to gain one less drink per average drinking occasion and $64 to gain 1 less day of heavy episodic drinking in a 30-day period.
To our knowledge, there is no published study that conducts an economic evaluation of brief interventions to reduce drinking among students to which these results can be compared. However, more broadly, Neighbors et al. (2010) recently conducted an economic evaluation of motivational interventions among youth in an emergency department. The costs of that study can be compared with our findings (however, that study does not use the same outcomes as our study; therefore, the cost-effectiveness findings are not directly comparable). That study found that the comparable labor cost of the intervention was about $68 per client. Our study found that the cost per intervention using MIFB was about $36, which is therefore just over half as expensive. Staff in the two studies spent approximately the same amount of time on the interventions. In Neighbors et al., average staff time per intervention was estimated retrospectively by experts and totaled 1 hour and 22 minutes, including 30 minutes of direct intervention time. In our study, we used staff logs to estimate time per intervention and found the average time spent on MIFB was 1 hour and 12 minutes, including 38 minutes of direct intervention time. The cost differences between the two studies are therefore likely driven by staff pay. Neighbors et al. report using trained masters-level social workers as staff, whereas we used trained graduate students.
In addition to describing the trade-off between spending on interventions and improving outcomes, the analysis also provides insight into which interventions should be adopted, depending on how much the decision maker is willing to pay. In the current study, the probability that MIFB was optimal was highest if the decision maker was willing to pay more than ∼$45 to achieve a one-drink decrease in average drinks per drinking occasion, or more than ∼$67 to achieve a 1-day decrease in heavy episodic drinking days. Up to these thresholds, AO had the highest probability of being optimal of all study arms. This finding does not necessarily mean that universities on tight budgets should adopt AO. Budget restrictions affect the ability to pay but not necessarily willingness to pay. Moreover, cost-effectiveness analysis can only ever assess interventions relative to one another. Because doing no assessment at all was not a study arm, AO cannot be said to be better or worse than doing no assessment. Future research is needed to determine both the decision makers’ willingness to pay to reduce drinking and whether AO is an effective and cost-effective intervention.
Sensitivity analyses that quantify the impact of varying key assumptions demonstrated that the specific allocation of resources to deliver interventions can be important. For example, the results showed that whether GAs supervised clients completing forms made a difference to which intervention is most cost-effective. The sensitivity analysis findings also demonstrate how accurate measurement and assumptions in deriving costs for cheap interventions, such as FB, can be crucial to the inferences that decision makers might make.
The EVPI also describes how results are influenced by uncertainty by combining the probability that a decision is optimal with the value of the consequences of that decision. The findings indicate that the maximum value of conducting future research to reduce the uncertainty rises quite rapidly as willingness to pay is increased up to the point at which MIFB becomes the optimal intervention. Thereafter, the value of future research increases slowly.
The findings of the current study are perhaps particularly significant because college students are a key target population of federally funded efforts to reduce drinking (NIAAA, 2011). Moreover, this study focuses on freshmen, a group of college students that is of particular concern (Arnett, 2005; Bachman et al., 1997; White and Jackson, 2004/2005). Addressing heavy drinking among students early in their college career could help protect against heavy drinking later in their college career, and hence consequent harm to overall academic performance. At the participating college, which is a state-funded institution, budgets for faculty hires are based on student course load. As an approximation, having 18 students enrolled in a course at this college secures one full-time faculty position. Thus, minimizing student dropout through poor academic performance or other consequences of drinking may have budgetary implications for the university. This issue is of particular concern when large state deficits mean public universities are instituting hiring freezes.
The study has at least three potential limitations. First, the data are from only one college, and thus the findings cannot necessarily be applied to other institutions of higher education or to noncollegiate settings. Other settings will likely vary with regard to the social/cultural norms toward alcohol consumption, the demographic characteristics of the target population, and the staff and other resources administering the screening and intervention. Results should be replicated before widespread decisions about allocating intervention and education resources are made. Second, the outcome measures examined are temporally and conceptually proximate to the intervention. They focus on drinking, which is intended to be directly affected by the intervention, and the interventions are short and aimed at a nondependent population; therefore, outcomes are examined in the near term, at 3 months. Many outcomes are excluded, such as drinking and driving (Neighbors et al., 2010) and postgraduation employment. There is debate in the literature on the economic evaluation of alcohol interventions as to the appropriate long-term outcome measure (Sindelar et al., 2004). Third, the analysis is a cost-effectiveness analysis and not a cost-utility or cost-benefit analysis. Outcomes that could be used to convert into quality-adjusted life years were not included in the study. Many studies measure outcomes in natural units (e.g., number of drinking days) rather than as a composite (e.g., quality-adjusted life years) or monetized measure (e.g., dollars) (Barbosa et al., 2010). Victimization among women is one example of a relevant outcome that is difficult to monetize. A study using the current study’s interventions among female students found reduced episodes of victimization in MIFB compared with AO (Clinton-Sherrod et al., 2011). Given the temporal nature of heavy drinking in underage drinkers, it would be difficult to accurately quantify the long-term cost savings of reductions in alcohol use for this study’s population based on changes in these near-term outcomes.
One avenue for future research on this topic is to address the above limitations. Further study is needed to examine combinations of MI and FB in other sites of higher education. If short-term improvement in drinking is also established elsewhere, research should assess whether that then affects long-term drinking and other correlated behaviors, such as drinking and driving, graduation from college, employment, and chronic health problems. If the findings from this study are borne out elsewhere, analyses should also examine whether results should be stratified by certain characteristics of students and the degree to which costs or effectiveness differ according to more refined differences in intervention (e.g., length of MI protocol, content of the feedback report).
Acknowledgments
We thank Brian McMillen for his help in obtaining cost estimates and comments on the article, the graduate assistants participating in this study, the host university, and Carolina Barbosa for comments on the article.
Footnotes
This research was supported by National Institute on Alcohol Abuse and Alcoholism Grant AA014374.
References
- Agostinelli G, Brown JM, Miller WR. Effects of normative feedback on consumption among heavy drinking college students. Journal of Drug Education. 1995;25:31–40. doi: 10.2190/XD56-D6WR-7195-EAL3. [DOI] [PubMed] [Google Scholar]
- Arnett JJ. The developmental context of substance use in emerging adulthood. Journal of Drug Issues. 2005;35:235–253. [Google Scholar]
- Bachman JG, Wadsworth KN, O’Malley PM, Johnston LD, Schulenberg J. Smoking, drinking, and drug use in young adulthood: The impacts ofnew freedoms and new responsibilities. Mahwah, NJ: Lawrence Erlbaum; 1997. [Google Scholar]
- Baer JS, Kivlahan DR, Blume AW, McKnight P, Marlatt GA. Brief intervention for heavy-drinking college students: 4-year follow-up and natural history. American Journal of Public Health. 2001;91:1310–1316. doi: 10.2105/ajph.91.8.1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbosa C, Godfrey C, Parrott S. Methodological assessment of economic evaluations of alcohol treatment: What is missing? Alcohol and Alcoholism. 2010;45:53–63. doi: 10.1093/alcalc/agp067. [DOI] [PubMed] [Google Scholar]
- Barton GR, Briggs AH, Fenwick EAL. Optimal cost-effectiveness decisions: the role of the cost-effectiveness acceptability curve (CEAC), the cost-effectiveness acceptability frontier (CEAF), and the expected value of perfection information (EVPI) Value in Health. 2008;11:886–897. doi: 10.1111/j.1524-4733.2008.00358.x. [DOI] [PubMed] [Google Scholar]
- Broskowski A, Smith S. Estimating the cost of preventive services in mental health and substance abuse under managed care (DHHS Pub. No. SMA-02-3617R) Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration; 2001. Retrieved from http://store.samhsa.gov/shin/content//SMA02-3617R/SMA02-3617R.pdf. [Google Scholar]
- Brown JM, Bender RH, Cowell AJ, Orr WA, Rae Olmsted K. Motivational interviewing to reduce drinking among a sample of freshmen college students. Unpublished manuscript. 2011 [Google Scholar]
- Carey KB, Scott-Sheldon LAJ, Elliott JC, Bolles JR, Carey MP. Computer-delivered interventions to reduce college student drinking: A meta-analysis. Addiction. 2009;104:1807–1819. doi: 10.1111/j.1360-0443.2009.02691.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clinton-Sherrod M, Morgan-Lopez AA, Brown JM, McMillen BA, Cowell A. Incapacitated sexual violence involving alcohol among college women: The impact of a brief drinking intervention. Violence Against Women. 2011;17:135–154. doi: 10.1177/1077801210394272. [DOI] [PubMed] [Google Scholar]
- Coffield AB, Maciosek MV, McGinnis JM, Harris JR, Caldwell MB, Teutsch SM, Haddix A. Priorities among recommended clinical preventive services. American Journal of Preventive Medicine. 2001;21:1–9. doi: 10.1016/s0749-3797(01)00308-7. [DOI] [PubMed] [Google Scholar]
- Collins SE, Carey KB, Sliwinski MJ. Mailed personalized normative feedback as a brief intervention for at-risk college drinkers. Journal of Studies on Alcohol. 2002;63:559–567. doi: 10.15288/jsa.2002.63.559. [DOI] [PubMed] [Google Scholar]
- Cowell AJ, Bray JW, Mills MJ, Hinde JM. Conducting economic evaluations of screening and brief intervention for hazardous drinking: Methods and evidence to date for informing policy. Drug and Alcohol Review. 2010;29:623–630. doi: 10.1111/j.1465-3362.2010.00238.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham JA, Wild TC, Cordingley J, Van Mierlo T, Humphreys K. Twelve-month follow-up results from a randomized controlled trial of a brief personalized feedback intervention for problem drinkers. Alcohol and Alcoholism. 2010;45:258–262. doi: 10.1093/alcalc/agq009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stod-dart GL. Methods for the economic evaluation of health care programmes. New York, NY: Oxford University Press; 2005. [Google Scholar]
- Fenwick E, Claxton K, Sculpher M. Representing uncertainty: The role of cost-effectiveness acceptability curves. Health Economics. 2001;10:779–787. doi: 10.1002/hec.635. [DOI] [PubMed] [Google Scholar]
- Gold MR, Siegel JE, Russell LB, Weinstein MC, editors. Cost effectiveness in health and medicine. New York, NY: Oxford University Press; 1996. [Google Scholar]
- Koerkamp BG, Myriam Hunink MG, Stijnen T, Weinstein MC. Identifying key parameters in cost-effectiveness analysis using value of information: A comparison of methods. Health Economics. 2006;15:383–392. doi: 10.1002/hec.1064. [DOI] [PubMed] [Google Scholar]
- Larimer ME, Cronce JM. Identification, prevention and treatment: A review of individual-focused strategies to reduce problematic alcohol consumption by college students. Journal of Studies on Alcohol, Supplement. 2002;14:148–163. doi: 10.15288/jsas.2002.s14.148. [DOI] [PubMed] [Google Scholar]
- Larimer ME, Cronce JM. Identification, prevention, and treatment revisited: Individual-focused college drinking prevention strategies 1999-2006. Addictive Behaviors. 2007;32:2439–2468. doi: 10.1016/j.addbeh.2007.05.006. [DOI] [PubMed] [Google Scholar]
- Latimer N, Guillaume L, Goyder E, Chilcott J, Payne N. Screening and brief interventions: Cost effectiveness review. Sheffield, England: ScHARR Public Health Collaborating Centre; 2009. [Google Scholar]
- McMillen BA, Hillis SM, Brown JM. College students’ responses to a 5/4 drinking question and maximum blood alcohol concentration calculated from a timeline followback questionnaire. Journal of Studies on Alcohol and Drugs. 2009;70:601–605. doi: 10.15288/jsad.2009.70.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people to change addictive behavior. New York, NY: Guilford Press; 1991. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. New York, NY: Guilford Press; 2002. [Google Scholar]
- Miller WR, Tonigan JS. Assessing drinkers’ motivations for change: The Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) Psychology of Addictive Behaviors. 1996;10:81–89. [Google Scholar]
- Murphy JG, Benson TA, Vuchinich RE, Deskins MM, Eakin D, Flood AM, Torrealday O. A comparison of personalized feedback for college student drinkers delivered with and without a motivational interview. Journal of Studies on Alcohol. 2004;65:200–203. doi: 10.15288/jsa.2004.65.200. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. What colleges need to know now: an update on college drinking research. NIH Publication No. 07–5010; 2007. Retrieved from http://www.niaaa.nih.gov/AboutNIAAA/NIAAASponsoredPrograms/Documents/1College_Bulletin-508_361C4E.pdf. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. College drinking: Changing the culture. 2011. Retrieved from http://www.collegedrinking-prevention.gov/NIAAACollegeMaterials/Default.aspx.
- Neighbors C, Larimer ME, Lewis MA. Targeting misper-ceptions of descriptive drinking norms: Efficacy of a computer-delivered personalized normative feedback intervention. Journal of Consulting and Clinical Psychology. 2004;72:434–447. doi: 10.1037/0022-006X.72.3.434. [DOI] [PubMed] [Google Scholar]
- Neighbors CJ, Barnett NP, Rohsenow DJ, Colby SM, Monti PM. Cost-effectiveness of a motivational intervention for alcohol-involved youth in a hospital emergency department. Journal of Studies on Alcohol and Drugs. 2010;71:384–394. doi: 10.15288/jsad.2010.71.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins HW. Surveying the damage: A review of research on consequences of alcohol misuse in college populations. Journal of Studies on Alcohol, Supplement. 2002;14:91–100. doi: 10.15288/jsas.2002.s14.91. [DOI] [PubMed] [Google Scholar]
- Ruger JP, Weinstein MC, Hammond SK, Kearney MH, Em-mons KM. Cost-effectiveness of motivational interviewing for smoking cessation and relapse prevention among low-income pregnant women: A randomized controlled trial. Value in Health. 2008;11:191–198. doi: 10.1111/j.1524-4733.2007.00240.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaus JF, Sole ML, McCoy TP, Mullett N, O’Brien MC. Alcohol screening and brief intervention in a college student health center: A randomized controlled trial. Journal of Studies on Alcohol and Drugs, Supplement. 2009;16:131–141. doi: 10.15288/jsads.2009.s16.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulenberg J, O’Malley PM, Bachman JG, Wadsworth KN, Johnston LD. Getting drunk and growing up: Trajectories of frequent binge drinking during the transition to young adulthood. Journal of Studies on Alcohol. 1996;57:289–304. doi: 10.15288/jsa.1996.57.289. [DOI] [PubMed] [Google Scholar]
- Sindelar JL, Jofre-Bonet M, French MT, McLellan AT. Cost-effectiveness analysis of addiction treatment: Paradoxes of multiple outcomes. Drug and Alcohol Dependence. 2004;73:41–50. doi: 10.1016/j.drugalcdep.2003.09.002. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB, Leo GI, Cancilla A. Reliability of a timeline method: Assessing normal drinkers’ reports of recent drinking and a comparative evaluation across several populations. British Journal of Addiction. 1988;83:393–402. doi: 10.1111/j.1360-0443.1988.tb00485.x. [DOI] [PubMed] [Google Scholar]
- Solberg LI, Maciosek MV, Edwards NM. Primary care intervention to reduce alcohol misuse: Ranking its health impact and cost effectiveness. American Journal of Preventive Medicine. 2008;34:143–152. doi: 10.1016/j.amepre.2007.09.035. [DOI] [PubMed] [Google Scholar]
- Tevyaw TO, Borsari B, Colby SM, Monti PM. Peer enhancement of a brief motivational intervention with mandated college students. Psychology of Addictive Behaviors. 2007;21:114–119. doi: 10.1037/0893-164X.21.1.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turrisi R, Larimer ME, Mallett KA, Kilmer JR, Ray AE, Mas-troleo NR, Montoya H. A randomized clinical trial evaluating a combined alcohol intervention for high-risk college students. Journal of Studies on Alcohol and Drugs. 2009;70:555–567. doi: 10.15288/jsad.2009.70.555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters ST. In praise of feedback: An effective intervention for college students who are heavy drinkers. Journal of American College Health. 2000;48:235–238. doi: 10.1080/07448480009599310. [DOI] [PubMed] [Google Scholar]
- Walters ST, Bennett ME, Miller JH. Reducing alcohol use in college students: A controlled trial of two brief interventions. Journal of Drug Education. 2000;30:361–372. doi: 10.2190/JHML-0JPD-YE7L-14CT. [DOI] [PubMed] [Google Scholar]
- Walters ST, Vader AM, Harris TR. A controlled trial of web-based feedback for heavy drinking college students. Prevention Science. 2007;8:83–88. doi: 10.1007/s11121-006-0059-9. [DOI] [PubMed] [Google Scholar]
- Walters ST, Vader AM, Harris TR, Field CA, Jouriles EN. Dismantling motivational interviewing and feedback for college drinkers: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2009;77:64–73. doi: 10.1037/a0014472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler H, Nelson TF. What we have learned from the Harvard School of Public Health College Alcohol Study: Focusing attention on college student alcohol consumption and the environmental conditions that promote it. Journal of Studies on Alcohol and Drugs. 2008;69:481–490. doi: 10.15288/jsad.2008.69.481. [DOI] [PubMed] [Google Scholar]
- Weingardt KR, Baer JS, Kivlahan DR, Roberts LJ, Miller ET, Marlatt GA. Episodic heavy drinking among college students: Methodological issues and longitudinal perspectives. Psychology of Addictive Behaviors. 1998;12:155–167. [Google Scholar]
- White HR, Jackson K. Social and psychological influences on emerging adult drinking behavior. Alcohol Research & Health. (2004/2005);28(4):182–190. Retrieved from http://pubs.niaaa.nih.gov/publications/arh284/182-190.pdf. [Google Scholar]
- White HR, Morgan TJ, Pugh LA, Celinska K, Labouvie EW, Pandina RJ. Evaluating two brief substance-use interventions for mandated college students. Journal of Studies on Alcohol. 2006;67:309–317. doi: 10.15288/jsa.2006.67.309. [DOI] [PubMed] [Google Scholar]
- Zarkin GA, Bray JW, Aldridge A, Mitra D, Mills MJ, Couper DJ, Cisler RA the COMBINE Cost-Effectiveness Research Group. Cost and cost-effectiveness of the COMBINE study in alcohol-dependent patients. Archives of General Psychiatry. 2008;65:1214–1221. doi: 10.1001/archpsyc.65.10.1214. [DOI] [PMC free article] [PubMed] [Google Scholar]