Abstract
Objective
It is now recognized that climate change affects human health. The question is how to adapt. This article examines mainstreaming climate considerations into public health programs and the utility of climate change and health adaptation frameworks, using Ontario, Canada, as a case study.
Methods
A literature review identified climate change and health adaptation frameworks for comparison with the Ontario Public Health Standards. Key informant interviews gauged the extent to which climate change risks are currently considered in policy and planning.
Results
Ontario’s Public Health Standards already require many of the risk management activities identified in climate change and health adaptation frameworks. However, public health officials require additional information about linkages between climate change and health to manage risks.
Conclusions
Risk management activities such as population health assessments, surveillance and public education and outreach can address many key risks related to climate hazards when information about the risks, vulnerable populations and time scales is made available to health officials. The development, analysis and transfer of this information should be considered a priority at all levels within the public health sector.
Keywords: Climate change, Human health, Adaptation, Assessments, Policy, Environmental health
Introduction
Climate change impacts are being observed worldwide on human and natural systems, including water resources, forestry, food production, coastal areas, ecosystems, industry, settlements and human health (Intergovernmental Panel on Climate Change (IPCC) 2007; Stern 2006). Many recent publications have highlighted the health impacts of climate change on populations, as well as how these effects are expected to evolve as the climate continues to change. Potential impacts include more illnesses and deaths related to poor air quality, food shortages, water- and food-borne contamination, extreme weather events and changing patterns of diseases spread by animals, ticks and insects (Chiotti and Lavender 2008; Confalonieri et al. 2007; Haines et al. 2006; McMichael et al. 2006; Patz et al. 2005; Sequin and Clarke 2008). As evidence accumulates, there are increasing calls for public health decision makers to take preventative actions or “adaptations” (e.g., vulnerability assessments, surveillance, warning systems, public education and outreach) to reduce the health risks associated with climate change (Confalonieri et al. 2007; McMichael et al. 2008; Menne and Ebi 2006; World Health Organization 2005).
Climate change and health adaptation frameworks
A number of generic frameworks have been developed to assist decision makers and communities in preparing for the expected impacts of climate change in various sectors (Lim BS et al. 2005; Polsky et al. 2003; Smit and Wandel 2006). These frameworks have been instrumental in (1) raising awareness among decision makers in many climate-sensitive sectors about the need to view climate change as a risk management issue; (2) highlighting the respective roles of policy makers and program managers in planning for climate change impacts; (3) bringing to the forefront the need to establish institutional mechanisms for adaptation development; and (4) explicitly incorporating adaptation and climate change considerations into policies and programs designed to reduce risks. Recently, some researchers have developed climate change assessment and risk management frameworks specifically for health decision makers (Berry 2008; Kovats et al. 2003; Polsky et al. 2003).
The focus now is on “mainstreaming” climate change and health adaptation considerations and information into existing decision-making processes, rather than creating new policies or policy instruments (Dougherty and Elasha 2004; Smit and Wandel 2006). This entails incorporating information about climate-related health risks into existing risk management activities and integrating efforts among different health sector partners to develop coordinated responses (Berry 2008). To this end, knowledge is required about the expected risks to health (Künzli 2010), so that policies can be developed and public health systems can incorporate and act on this new information.
Public health risk management in Ontario
In Canada, each province has its own organizational structure, policy direction and set of priorities for delivering public health services. In Ontario, the local boards of health deliver public health programs and services based on the Ontario Public Health Standards (Government of Ontario 2008). The Ontario Public Health Standards represent minimum requirements for Ontario’s 36 boards of health, although many boards of health do provide additional programs and services beyond those stipulated in the standards. Population health and health promotion activities include key risk management activities related to assessing, planning, delivering, managing and evaluating public health programs and services. Several required programs and protocols relate to a number of climate-sensitive threats to health—infectious disease prevention and control, rabies prevention and control, vaccine preventable diseases, child health, food safety, water safety, health hazard prevention and management, and public health emergency preparedness (Fig. 1). No provisions specifically require assessments or monitoring of climate change health impacts, although the Ontario Public Health Standards state that the “…board of health shall increase public awareness of health risk factors associated with…climate change” (Government of Ontario 2008). For each program and protocol, generic risk management activities form the basis of efforts to protect health. As illustrated, the “foundational standards” include population health assessment, surveillance, research and knowledge exchange, and program evaluation.
Fig. 1.
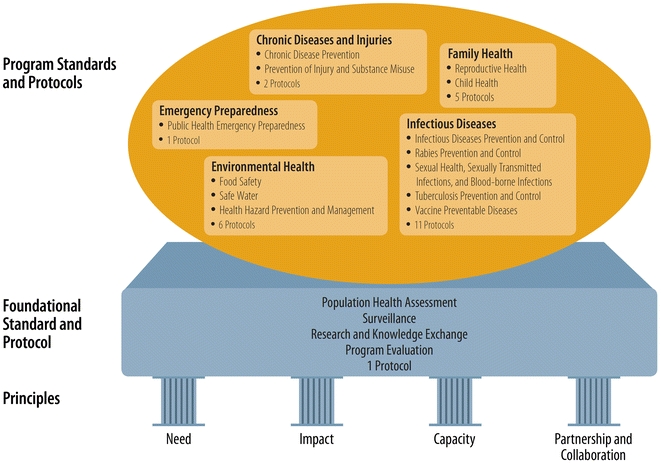
Ontario Public Health Standards: relationship between the principles, foundational standard, and program standards. Source: Government of Ontario 2008
In Canada, the risk management approach is well accepted and understood by the public health community, and several risk management frameworks exist to direct the activities of public health officials (Health Canada 2003). The question therefore is whether health sector officials can actually benefit from the frameworks proffered by climate change adaptation researchers, and if so, in what ways. In this article, the utility of climate change and health adaptation frameworks to support the development of adaptation measures in Ontario is examined by comparing them with the Ontario Public Health Standards. The results from a key informant survey of public health officials across Canada about climate-related health issues are presented to further analyze the utility of the frameworks and to identify other requirements for addressing climate-related health risks.
Methods
Two methods were used for the analysis. (1) A literature review was conducted to select climate change and health adaptation frameworks that could be compared with the Ontario Public Health Standards. The purpose was to identify similarities and differences among the frameworks for assessing climate-related health vulnerabilities and adaptation options. (2) Thirty semi-structured key informant interviews were conducted among local health authorities in Canada. The purpose was to identify awareness levels, key activities and allocated resources related to climate change and health.
Comparison of climate change and health adaptation frameworks and the Ontario Public Health Standards
A systematic literature search reviewed electronic databases, reference lists, books and reports (both published and grey literature) on the topic of climate change and adaptation, with a specific focus on health. Domestic and international sources were included; international ones when they had a Canadian component or provided a theoretical or methodological basis related to the health impacts of climate change. Keyword content and title searches for literature from all years to 2008 were examined. Examples of searched keywords included climate change and human health, climate change adaptation, climate change frameworks, extreme weather, impacts of global warming, adaptation policies and climate change mainstreaming. Retrieved articles were scanned for information on the actions needed to increase the capacity to manage health risks associated with a changing climate. Two frameworks were selected for the comparison with the Ontario Public Health Standards based on their comprehensiveness and the fact that they were specifically designed for the health sector—Kovats et al. (2003) (Fig. 2) and Berry (2008) (Fig. 3).
Fig. 2.
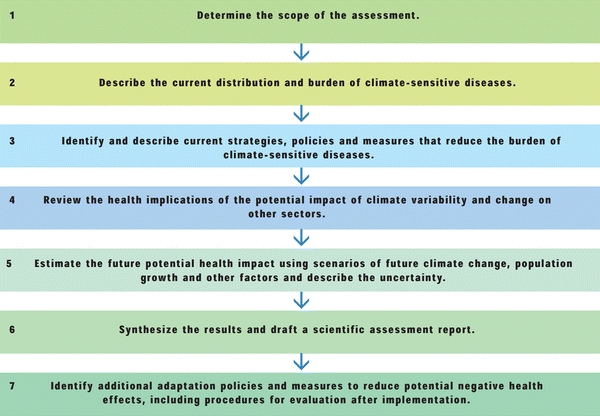
Steps in assessing vulnerability and adaptation to the health impacts of climate change. Source: Kovats et al. 2003
Fig. 3.
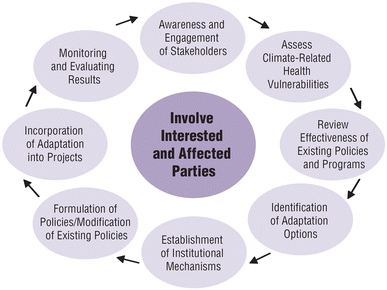
Framework for climate change adaptation development and implementation in the health sector. Source: Berry 2008
The framework proposed by Kovats et al. (2003) focuses on the steps and methods for assessing human health vulnerability to climate change. The framework proposed by Berry (2008) builds on the work of Kovats et al. (2003) by providing information on the steps to be considered when developing adaptation options to complement existing policies, institutional structures and processes (Fig. 3). Furthermore, it corresponds broadly to the key steps of standard risk management frameworks that are employed in the health sector in Canada. Basic steps include early and continuous engagement of stakeholders and other sectors, identifying adaptation options, modifying or establishing institutional mechanisms, formulating or modifying policies, incorporating adaptation into programs and projects, and monitoring and evaluating the results.
Key informant interviews with public health officials in Canada
To gauge the degree to which climate change risks are currently considered in policy and planning, 30 semi-structured key informant interviews were conducted in cities of various sizes across Canada in 2006, including eight interviews in Ontario (Canadian Public Health Association 2006). Senior public health officials from the largest city of each province were interviewed, and, based on their recommendations, follow-up interviews were conducted with other health professionals to collect further information (Fig. 4).
Fig. 4.
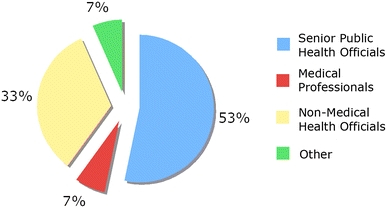
Breakdown of interviewees by professional role. Source: Canadian Public Health Association 2006
The survey instrument (Table 1) was designed to examine the extent to which public health officials (or organizations) are aware of climate change risks to health, are integrating such risks into their policies and planning, are able to respond to multiple health vulnerabilities and have identified key indicators or factors for enhancing adaptive capacity.
Table 1.
Informant interview survey instrument
| Question 1.0 | Do you believe that weather and climate have a significant impact on the health of people in your community? |
| Question 2.0 | Do you feel that climate change will increase risks to the health of people in your geographic jurisdiction? If YES, in what ways? |
| Question 2.1 | Has climate change been identified as a potential current or future public health issue for your geographical jurisdiction? |
| Question 3.0 | What are you currently doing to protect population health from the specific climate-related health risks that you have identified as of concern to your organization in question 2.0? |
| Question 3.1 | Do you find it necessary within the next 10 years to take new actions, or to expand current efforts, to reduce climate-related risks to health in your geographical jurisdictions? If YES, what actions? Why do you find it necessary? If NO, why do you find it unnecessary? |
| Question 3.2 | Do you use climate-related information (e.g., information about extreme weather events, warmer temperatures) in planning and program development activities at your organization? If YES, please give examples. |
| Question 4.0 | Do particular challenges exist in your efforts to reduce the health risks identified as a concern to your organization in question 2.0? |
Source: Canadian Public Health Association 2006
Results
Comparison of climate change adaptation and health frameworks and the Ontario Public Health Standards
Table 2 shows the comparative analysis of the two selected frameworks and the Ontario Public Health Standards. Considerable overlap exists between the activities required by the Ontario Public Health Standards and the steps in Kovats et al. (2003) and Berry (2008).
Table 2.
Comparative analysis of the two climate change and health adaptation frameworks and the Ontario Public Health Standards
| Framework steps | Kovats et al. (2003) | Berry (2008) | Ontario Public Health Standards (Government of Ontario 2008) |
|---|---|---|---|
| Engagement of stakeholders | Yes | Yes | Yes |
| Identification of burden of climate-related illness or injury | Yes | Yes | Partial |
| Identification of vulnerable populations | Yes | No | Yes |
| Projection of future health impacts from climate change | Yes | No | No |
| Assessment of the effectiveness of programs and activities to reduce climate-related health risks | Yes | Yes | Yes |
| Identification and prioritization of policy and program options to meet health needs | Yes | Yes | Yes |
| Establishment of policy mechanisms | No | Yes | Yes |
| Tailoring and implementation of programs and policies | No | Yes | Yes |
| Surveillance and monitoring | Partial | Partial | Partial |
| Knowledge exchange and raising awareness of climate-related health risks | Partial | Partial | Yes |
The Ontario Public Health Standards do not explicitly call for surveillance and monitoring of climate change health impacts, as is advocated for in the adaptation frameworks. However, they provide an institutional mechanism with generic program requirements that are able to manage climate-related risks. Therefore public health officials in Ontario do not require additional guidance, although specific information on how to integrate findings from climate scenarios and models to understand future risks and vulnerabilities (Kovats et al. 2003) would benefit these activities. The findings from the interviews of Canadian public health authorities suggest that climate change adaptations have yet to be implemented in many regions across Canada (Canadian Public Health Association 2006). This suggests that factors other than institutional mechanisms are necessary for public health authorities to address climate change impacts. Elements identified as being essential for implementing climate change adaptation measures into public health policy and programs include additional resources, increased awareness and climate specific information about risks to health (Fussel and Klein 2004).
Key informant interviews with public health officials in Canada
The key informant interviews revealed a broad awareness of climate change and related health issues. All respondents indicated that weather and climate do have a significant impact on health; most (76%) believed that climate change will increase risks to health in their jurisdictions (Canadian Public Health Association 2006). However, about half (54%) indicated that climate change had not been identified as a current or future public health issue in their jurisdictions. Respondents who did report that climate change was considered an important public health issue in their jurisdiction also indicated that it was not considered a high priority (Canadian Public Health Association 2006). Key challenges in addressing climate-related health risks included a lack of resources, a lack of prioritization of climate impacts on public health and a lack of adequate knowledge about potential linkages between climate change and health (Canadian Public Health Association 2006). Many identified that climate-related information pertaining to extreme weather warnings, air quality reports, West Nile virus surveillance and monitoring for flooding is used in planning and program development. However, most said they did not have adequate knowledge to make informed decisions about whether they need to take new actions, or extend current efforts, within the next 10 years. When identifying the various challenges faced in reducing climate-related health risks, the respondents did not identify a lack of tools or frameworks for managing risks (Canadian Public Health Association 2006).
Overall results
The comparative analysis and key informant interviews suggest that regular population health assessments and risk management activities by local public health units in Ontario can address many risks related to climate hazards and emergencies, when information about such risks is made available to health officials. Many activities identified in the Ontario Public Health Standards mirror those proposed by the climate change and health adaptation frameworks. The overlap between these standards and the frameworks therefore suggests that public health practices in Ontario are theoretically able to accommodate many of the proposed climate considerations and adaptation strategy development measures. For example, emergency management activities—such as planning and preparedness for weather-related emergencies, which are expected to increase in frequency and severity with climate change (Intergovernmental Panel on Climate Change (IPCC) 2007)—flow directly from the hazards identification phase within the Ontario Public Health Standards. What is needed is information about increased health risks associated with climate change.
Discussion
Some studies have identified general health risks related to climate change for people living in Ontario (Abelsohn et al. 2008; Carty et al. 2004; Chiotti et al. 2002; Chiotti and Lavender 2008). However, information is lacking about the direct and indirect climate-mediated processes involved at local scales within the time frames needed to inform decision making (Tamerius et al. 2007). Challenges exist in the development of new knowledge about the expected impacts of climate change on health given the very complex causal sources and pathways and intertwined interactions between them (Forastiere 2010; Xun et al. 2010). Once current or near-term health risks related to climate variability are identified, activities to protect health before, during and after a health emergency can be adopted. The Ontario Public Health Standards can address existing diseases that are being exacerbated by climate change (e.g., Lyme disease) through current surveillance and public education and outreach activities. In this regard, the standards require “…the board of health shall work with community partners to improve public knowledge of infectious diseases of public health importance and infection prevention and control practices…” (Government of Ontario 2008). Given that the requirements in Ontario already provide direction for addressing many health concerns that are climate sensitive, new processes or risk management steps are not required in order to mainstream climate change.
In order to mainstream climate change concerns, public health decision making requires information about climate-related health risks to inform existing risk management activities. These activities, such as population health assessment, surveillance and public education and outreach can only account for climate factors if information on climate-related risks is available to public health practitioners and researchers (e.g., what are the climate hazards and associated health impacts, where will they occur, when will they occur and who will be most affected?). For example, while it is known that extreme heat can impact morbidity (Green et al. 2010) and mortality (Sequin and Clarke 2008), assessments of heat-health vulnerabilities require projections of the future frequency and severity of extreme heat events, information related to the geographical variation in exposure to extreme heat, identification of vulnerable populations and identification of actual temperature and morbidity/mortality thresholds. If such information is not available to be considered in the assessment step of existing frameworks, important risks to human health cannot be mainstreamed. Public health interventions that may be implemented to reduce climate change impacts on health within relevant time scales (5–10 years) need to be identified through assessments (Ortíz Bultó et al. 2008). However, information in these time scales about projected risks to health is often not available to decision makers.
The need in Canada for better understanding of health risks associated with climate change, as reported in the key informant interviews, is also reflected in resolutions or declarations passed by the Canadian Public Health Association (2001), the World Health Organization (World Health Organization Department of Communications May 22, 2009) and the World Medical Association (World Medical Association 2010); these call for more research into the health impacts of climate change. A lack of information about risks was also identified as a major barrier to public health adaptation in a recent survey of local health departments in the United States (Balbus et al. 2008). The development, analysis and transfer of knowledge among local, provincial, federal and international health authorities showing how climate change might impact the health of local populations is critical for facilitating adaptation efforts in the health sector, and should be made a priority area of collaborative efforts in the future (Ebi 2008; Yohe and Ebi 2005). At the national level, Health Canada has completed a country-wide assessment of health vulnerabilities to climate change impacts that can help inform the development of needed adaptations by health authorities at local and regional levels (Sequin and Clarke 2008). Moreover, new knowledge is being developed at the national level on climate-related health risks pertaining to extreme heat events (Health Canada 2011), vector-borne diseases and challenges faced by northern populations (Government of Canada 2009; Health Canada 2009).
Conclusions
A key finding of this study is that a strong foundation for developing and implementing adaptive actions to protect health already exists through current public health requirements and activities in Ontario. Existing risk management practices can be applied to reduce some climate-related risks, such as air pollution, extreme weather events, infectious diseases (e.g., Lyme disease), and water and food contamination. Thus, the current risk management practices already allow for the mainstreaming of most climate-related health risks. There is no need to implement or adopt separate climate change and health adaptation frameworks, particularly given limited resources and competing demands faced by public health officials. For this reason, frameworks that advocate, or propose, new climate change risk management processes and procedures for reducing health risks, will have limited applicability for public health and emergency management decision makers in Ontario and other provinces in Canada, as well as in other countries with similar risk management systems in place. However, countries and regions with less comprehensive population health assessment, surveillance and public education and outreach activities may benefit more from the guidance provided by the adaptation frameworks examined here.
The findings also indicate that risk management systems must be informed by adequate information about climate-related health risks for public health authorities to mainstream climate change concerns and take needed actions to protect at-risk populations. Other research has also indicated that adaptation efforts within and outside of Canada require a better understanding of current and geographically specific risks from climate-related hazards, and projected risks due to climate change in time scales relevant to public health decision makers (Haines et al. 2004; Berry 2008; Menne and Ebi 2006). In this regard, Huntingford et al. (2007) call for the development of multidisciplinary research teams which enhance collaboration between climate modelers and the health community to provide this information. What is needed is more information, including case studies and community examples that aid public health officials in their efforts to obtain, analyze and integrate findings from climate scenarios and models to gauge future impacts on health. Climate change can only be mainstreamed into health sector activities when such information is available and incorporated into existing public health risk management activities, as well as decision-making processes or standards (e.g., local population health assessments, surveillance, public education and outreach).
Given the critical role of information about climate-related health risks, future research and program development efforts to support greater mainstreaming would benefit from investigation of the most effective and efficient ways to provide this information to governmental and non-governmental authorities charged with protecting citizens from environmental and climate-related health risks. The complexity and uncertainty inherent in understanding climate-related health risks means that investigation into best practices for knowledge development, translation and transfer among researchers, decision makers and other stakeholders is required (Balbus et al. 2008). The findings here also strongly support the call by the World Health Organization for countries to take immediate measures to strengthen existing public health systems to reduce current impacts on health from climate extremes and to prepare for future climate change (World Health Organization 2005). Robust population health assessments, surveillance and public education and outreach activities, in particular, are key to protecting populations by mainstreaming climate change considerations into existing activities.
Acknowledgments
The authors are grateful to two anonymous referees for their constructive comments. Further comments, provided by Barry Smit, Mark Pajot, Eric Crighton and officials at the Ontario Ministry of Health and Long-Term Care are gratefully acknowledged.
Conflict of interest
The authors, Kaila-Lea Clarke and Peter Berry, declare that they have no competing interests.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- Abelsohn A, Rachlis V, Rosen D, Kasperski MJ (2008) Addressing the Health Effects of Climate Change: Family Physicians Are Key. The Ontario College of Family Physicians, Toronto. http://www.ocfp.on.ca/local/files/EHC/Addressing%20the%20Health%20Effects%20of%20Climate%20Change%20Family%20Physicians%20are%20Key%20April%207%202008.pdf. Accessed 1 July 2011
- Balbus J, Ebi K, Finzer L, Malina C, Chadwick A, McBride D, Chuk M, Maibach E (2008) Are we ready: preparing for the public health challenges of climate change. Environmental Defence. http://www.edf.org/documents/7846_AreWeReady_April2008.pdf. Accessed 1 July 2011
- Berry P. Vulnerabilities, adaptation and adaptive capacity in canada. In: Séguin J, editor. Human health in a changing climate: a canadian assessment of vulnerabilities and adaptive capacity. Ottawa: Health Canada; 2008. pp. 367–448. [Google Scholar]
- Canadian Public Health Association (2006) Snapshot of adaptation and response capacity to climate change in public health. Prepared for Health Canada, Ottawa
- Carty P, Crabbé P, Krewski D (2004) A risk management approach to climate change and health impacts in eastern Ontario. Prepared for Health Canada, Ottawa
- Chiotti Q, Lavender B. Ontario. In: Lemmen D, Warren F, Lacroix J, Bush E, editors. From impacts to adaptation: Canada in a changing climate 2007. Ottawa: Government of Canada; 2008. pp. 127–274. [Google Scholar]
- Chiotti Q, Morton I, Maarouf A (2002) Toward and adaptation action plan: climate change and health in the Toronto–Niagara region. Prepared for the Climate Change Action Fund, Natural Resources Canada, Ottawa
- Confalonieri U, Menne B, Akhtar R, Ebi KL, Hauengue M, Kovats RS, Revich B, Woodward A. Human health. In: Parry M, Canziani O, Palutikof J, van der Linden P, Hanson C, editors. Climate Change 2007: impacts, adaptation and vulnerability. Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge: Cambridge University Press; 2007. pp. 391–431. [Google Scholar]
- Dougherty B, Elasha BO (2004) Mainstreaming adaptation into national development plans. Second AIACC Africa and Indian Ocean Island Regional Workshop. University of Senegal, Dakar. http://www.aiaccproject.org/meetings/Dakar_04/Dakar_Final.pdf Accessed 1 July 2011
- Ebi KL. Healthy people 2100: modeling population health impacts of climate change. Clim Change. 2008;88:5–19. doi: 10.1007/s10584-006-9233-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forastiere F. Climate change and health: a challenge for epidemiology and public health. Int J of Public Health. 2010;55:83–84. doi: 10.1007/s00038-009-0096-9. [DOI] [PubMed] [Google Scholar]
- Fussel H, Klein R. Conceptual frameworks of adaptation to climate change and their application to human health. PIK Report No. 91. Potsdam: Potsdam Institute for Climate Impact Research; 2004. [Google Scholar]
- Government of Canada (2009) Canada’s action on climate change. http://www.climatechange.gc.ca/default.asp?lang=En&n=76935E93-1. Accessed 1 July 2011
- Government of Ontario (2008) The Ontario Public Health Standards: guidelines for the provision of mandatory health programs and services by the Minister of Health and Long-Term Care
- Green R, Basu R, Malig B, Broadwin R, Kim Je, Ostro B. The effect of temperature on hospital admissions in nine California counties. Int J Public Health. 2010;55:113–121. doi: 10.1007/s00038-009-0076-0. [DOI] [PubMed] [Google Scholar]
- Haines A, Kuruvilla S, Borchet M. Bridging the implementation gap between knowledge and action for health. B World Health Organ. 2004;82:724. [PMC free article] [PubMed] [Google Scholar]
- Haines A, Kovats RS, Campbell-Lendrum D, Corvalan C. Climate change and human health: impacts, vulnerability and mitigation. Lancet. 2006;367:2102–2109. doi: 10.1016/S0140-6736(06)68933-2. [DOI] [PubMed] [Google Scholar]
- Health Canada . Health Canada decision-making framework for identifying, assessing and managing health risks. Ottawa: Health Canada; 2003. [Google Scholar]
- Health Canada . Climate Change and Health Adaptation in Northern First Nations and Inuit Communities Program: 2010–2011 funding application guide. Ottawa: Health Canada; 2009. [Google Scholar]
- Health Canada . Extreme heat events guidelines: technical guide for health care workers. Ottawa: Health Canada; 2011. [Google Scholar]
- Huntingford C, Hemming D, Gash JHC, Gedney N, Nuttall PA. Impact of climate change on health: what is required of climate modellers? Trans R Soc Trop Med Hyg. 2007;101:97–103. doi: 10.1016/j.trstmh.2006.11.001. [DOI] [PubMed] [Google Scholar]
- Intergovernmental Panel on Climate Change (IPCC) (2007) Climate change 2007: synthesis report. In: Core Writing Team, Pachauri RK, Reisinger A (eds) Contribution of working groups I, II and III to the fourth assessment report of the intergovernmental panel on climate change. IPCC, Geneva, Switzerland, p 104
- Kovats S, Ebi K, Menne B. Methods of assessing human health vulnerability and public health adaptation to climate change. Geneva: World Health Organization, Health Canada, World Meteorological Association, United Nations Environment Programme; 2003. [Google Scholar]
- Künzli N. Climate changes health. Int J Public Health. 2010;55:77–78. doi: 10.1007/s00038-010-0123-x. [DOI] [PubMed] [Google Scholar]
- Lim BS E, Burton I, Malone EL, Huq S. Adaptation policy frameworks for climate change: developing strategies, policies and measures. Cambridge: Cambridge University Press; 2005. [Google Scholar]
- McMichael AJ, Woodruff RE, Hales S. Climate change and human health: present and future risks. Lancet. 2006;367:859–869. doi: 10.1016/S0140-6736(06)68079-3. [DOI] [PubMed] [Google Scholar]
- McMichael AJ, Neira M, Heymann DL. World Health Assembly 2008: climate change and health. Lancet. 2008;371:1895–1896. doi: 10.1016/S0140-6736(08)60811-9. [DOI] [PubMed] [Google Scholar]
- Menne B, Ebi KL. Climate change and adaptation strategies for human health. Darmstadt: Steinkopff Verlag; 2006. [Google Scholar]
- Ortíz Bultó PL, Pérez Rodríguez AE, Rivero Valencia A, Pérez Carreras A, Juan Ramón C, Lecha Estela LB (2008) La variabilidad y el cambio climático en Cuba: potenciales impactos en la salud humana. Revista Cubana de Salud Pública
- Patz JA, Campbell-Lendrum D, Holloway T, Foley JA. Impact of regional climate change on human health. Nature. 2005;438:310–317. doi: 10.1038/nature04188. [DOI] [PubMed] [Google Scholar]
- Polsky C, Schroter D, Pratt A (2003) Assessing vulnerabilities to the effects of global change: an eight-step approach. Research and Assessment Systems for Sustainability Program Discussion Paper 2003–05. Cambridge, MA: Environment and Natural Resources Program, Belfer Center for Science and International Affairs, Kennedy School of Government, Harvard University
- Sequin J, Clarke K-L. Introduction. In: Sequin J, editor. Human health in a changing climate: a Canadian assessment and adaptive capacity. Ottawa: Health Canada; 2008. [Google Scholar]
- Smit B, Wandel J. Adaptation, adaptive capacity and vulnerability. Global Environ Change. 2006;16:282–292. doi: 10.1016/j.gloenvcha.2006.03.008. [DOI] [Google Scholar]
- Stern N. The economics of climate change: the Stern review. Popul Dev Rev. 2006;32:793–798. doi: 10.1111/j.1728-4457.2006.00153.x. [DOI] [Google Scholar]
- Tamerius JD, Wise EK, Uejio CK, McCoy AL, Comrie AC. Climate change and human health: synthesizing environmental complexity and uncertainty. Stoch Environ Risk Assess. 2007;21:601–613. doi: 10.1007/s00477-007-0142-1. [DOI] [Google Scholar]
- World Health Organization Department of Communications (2009) World Health Assembly closes with resolutions on public health. http://www.who.int/mediacentre/news/releases/2009/world_health_assembly_20090522/en/index.html. Accessed 1 July 2011
- World Health Organization (2005) Health and climate change: the now and how a policy action guide. WHO Regional Office for Europe, Copenhagen http://www.euro.who.int/__data/assets/pdf_file/0003/95925/E87872.pdf. Accessed 1 July 2011
- World Medical Association (2010) WMA Declaration of Delhi on Health and Climate Change. http://www.wma.net/en/30publications/10policies/c5/
- Xun W, Khan A, Michael E, Vineis P. Climate change epidemiology: methodological challenges. Int J Public Health. 2010;55:85–96. doi: 10.1007/s00038-009-0091-1. [DOI] [PubMed] [Google Scholar]
- Yohe G, Ebi KL. Approaching adaptations: parallels and contrasts between the climate and health communities. In: Ebi KL, Smith J, Burton I, editors. Integration of public health with adaptation to climate change: lessons learned and new directions. London: Frances & Taylor; 2005. pp. 18–43. [Google Scholar]


