Abstract
The Internet has emerged as an important tool for the delivery of health promotion and disease prevention interventions. Our community-based participatory research (CBPR) partnership developed and piloted CyBER/testing, a culturally congruent intervention designed to promote HIV testing among men who have sex with men (MSM) within existing Internet chat rooms. Using a quasi-experimental, single-group study design, cross-sectional data were collected from chat room participants, known as “chatters,” at pretest (n=346) and post-test (n=315). Extant profile data also were collected to describe the demographics of the online population. The intervention significantly increased self-reported HIV testing among chatters overall, increasing rates from 44.5% at pretest to nearly 60% at post-test (p<.001). Furthermore, chatters who reported having both male and female sexual partners had nearly 6 times the odds of reporting HIV testing at post-test. Findings suggest that chat room-based HIV testing intervention may increase testing among MSM who may be difficult to reach in traditional physical spaces.
For many men who have sex with men (MSM), the Internet has emerged as an important tool for social networking and support, meeting friends and sexual partners, and building community (Bowen, Williams, Daniel, & Clayton, 2008; Nartz & Schoech, 2000; Rhodes, Hergenrather, Yee, & Ramsey, 2007; Silenzio, et al., 2009). The Internet may serve as an important tool in the development of social and sexual identity for some MSM. They may trust the sense of anonymity afforded by the Internet, and thus may be willing to engage in dialogue that they may not engage in publicly. These MSM may feel comfortable to share worries and experiences, brainstorm options, and learn from one another in a “virtual” safe space. There may be no other convenient safe space for many of these men (Bolding, Davis, Sherr, Hart, & Elford, 2004; Chiasson, et al., 2006; Rhodes, 2004).
However, seeking sex on the Internet has been found to be a risk factor for HIV and sexually transmitted disease (STD) infection among MSM (Coleman, et al., 2009; Klausner, Wolf, Fischer-Ponce, Zolt, & Katz, 2000; Rhodes, DiClemente, Cecil, Hergenrather, & Yee, 2002; Rosser, et al., 2009). MSM who seek sexual partners on the Internet tend to be more likely to report sex with both men and women (Elford, Bolding, Davis, Sherr, & Hart, 2004; Rhodes, et al., 2002), unprotected anal intercourse (Berry, Raymond, Kellogg, & McFarland, 2008; Garofalo, Herrick, Mustanski, & Donenberg, 2007; Rhodes, et al., 2002; Rosser, et al., 2009) more sexual partners (Horvath, Rosser, & Remafedi, 2008; Ogilvie, et al., 2008), and a history of STD infection (Rhodes, et al., 2002) when compared to those who meet one another in traditional physical spaces.
Since the beginning of the HIV epidemic in the US, MSM have been disproportionately affected by HIV, and it is recommended that sexually active MSM be tested for HIV annually (Centers for Disease Control and Prevention, Workowski, & Berman, 2006). Early detection of HIV infection through testing allows adequate monitoring and management of one’s health status, increases the likelihood of proper treatment initiation, and creates opportunities for education to prevent secondary transmission of HIV and improve sexual health (Mikolajczak, Hospers, & Kok, 2006; Weinhardt, Carey, Johnson, & Bickham, 1999). Data from the National HIV Behavioral Surveillance (NHBS) System found that among MSM ages 25–44, 92% reported ever being tested for HIV and 70.4% reported being tested in the previous 12 months (Sanchez, et al., 2006).
However, MSM who use Internet chat rooms for social and sexual networking (compared to other MSM) may be less likely to have been tested for HIV; we found 88% of MSM in chat rooms reported ever being tested for HIV and only 37% reported testing within previous 12 months (Rhodes, Hergenrather, Yee, & Ramsey, 2007). A clear need exists to develop and test innovative strategies that will increase testing among MSM at increased risk, including MSM who use the Internet for social and sexual networking.
Because evidence suggests that men who seek sexual partners on the Internet are at increased risk for HIV exposure and transmission through their risk behaviors (Benotsch, Kalichman, & Cage, 2002; Bolding, et al., 2004; Bull & McFarlane, 2000; McFarlane, Bull, & Rietmeijer, 2000; Moskowitz, Melton, & Owczarzak, 2009; Rhodes, et al., 2002), many community-based organizations (CBOs), AIDS service organizations (ASOs), and public health departments and clinics have responded by providing HIV education within existing chat rooms designed to facilitate social and sexual networking among MSM (Anderton & Valdiserri, 2005; Noar, Black, & Pierce, 2009; Ybarra & Bull, 2007). However, to our knowledge, outcomes from chat room-based HIV prevention intervention studies have not been reported previously.
Our community-based participatory research (CBPR) partnership proposed, developed, implemented, and evaluated a culturally congruent pilot intervention designed to promote HIV testing among MSM who seek male sexual partners within Internet chat rooms. The intervention, known as Cyber-Based Education and Referral/testing (CyBER/testing), was developed by a CBPR partnership whose members had broad experiences, perspectives, and skills. Blending these experiences, perspectives, and skills helped to ensure that CyBER/testing adhered to the norms of existing chat rooms while infusing sound science into the intervention and its evaluation.
We sought to describe the characteristics of chat room participants (“chatters”) who participated in the CyBER/testing intervention and evaluate the impact of the intervention on self-reported HIV testing rates using a quasi-experimental, pretest-post-test cross-sectional design.
Methods
CyBER/testing was an intervention that was developed, implemented, and evaluated by a CBPR partnership. CBPR is an approach to research that ensures full and equal participation by community members (including those affected by the issue being studied), organizational representatives, and academic researchers in all aspects of the research process. Much of the strength of CBPR comes from blending research and practice for the mutual benefit of all partners to effect community health (Cashman, et al., 2008; Israel, et al., 2003; Rhodes, Malow, & Jolly, 2010). Our partnership is committed to CBPR because blending lived experiences with sound science has potential to develop deeper understandings of phenomena and more relevant, and thus more likely impactful, interventions.
The history of this CBPR partnership, the application of partnership principles, and the adherence to CBPR in CyBER/M4M has been described previously (Rhodes, 2004; Rhodes, Hergenrather, Duncan, et al., 2010; Rhodes, Hergenrather, Duncan, et al, 2007; Rhodes, Hergenrather, Vissman, et al., In press). The partnership, which continues to evolve and reflects demographic trends, has existed for more than 9 years and has numerous studies designed to explore and/or reduce HIV risk. Members are mainly located in northwest and central North Carolina (NC), but membership is open to anyone or any organization committed to the partnership’s mission: “meeting HIV/AIDS prevention and care needs in NC through education, research, advocacy and support.” Members include lay community members and representatives from The Adam Foundation, Inc., AIDS Care Service, Inc., Chatham Social Health Council, Club Odyssey (a gay dance club), Forsyth Technical Community College, Guilford County Public Health Department, NC Pride, Inc., Triad Health Project, the University of NC Gillings School of Global Public Health, and Wake Forest University School of Medicine, among others.
CyBER/testing originated from a previous intervention study entitled Cyber-Based Education and Referral/Men for Men (CyBER/M4M), which was conceived, conducted, and evaluated by the partnership. CyBER/M4M was designed to increase awareness and reduce HIV risks among men who seek male sexual partners in existing chat rooms (Rhodes, Hergenrather, Ramsey, et al., 2007). CyBER/testing, however, focused on the promotion of HIV testing within one chat room designed for MSM social and sexual networking. It built on the lessons learned from CyBER/M4M. These lessons included: (1) many chatters find sexual partners in chat rooms and meet in person for sex; (2) many chat rooms seem to attract men who are not “out” about their sexual orientation; (3) chatters want information about, and access, to testing services; (4) because most chatters are online for priorities other than to participate in health promotion and disease prevention interventions, an Internet intervention must be focused (e.g., HIV testing promotion as opposed to broad HIV education); (5) to be effective, interventionists must juggle multiple chats and understand and respect the online culture; and (6) chatters are not likely to download incentives like coupons or gift certificates for several reasons, such as not wanting to have physical evidence of being online and having limited printing facilities (e.g., printers without ink and/or paper).
Study Design
We used a quasi-experimental, single-group pretest-post-test study design to evaluate the effects of the CyBER/testing intervention to increase HIV testing rates among MSM. The intervention was implemented in a chat room providing social and sexual networking for MSM in northwestern NC within a catchment area of over 1.3 million people. This chat room was selected because partnership members wanted to limit intervention delivery to one chat room to focus the intervention. This study was designed to adhere to standards outlined in the user agreement, community guidelines, legal notices, and privacy policies of the chat room. Because an Internet chat room in San Francisco was bombarded with profanity and death threats following media reports that health officials traced a syphilis outbreak to chatters who met there (Rhodes, 2004), we do not provide the name of the chat room in order to maintain the safety of the chatters and ensure maintenance of the trust our partnership earned with them.
Implementation of the intervention took place February-July 2009. Human subject review and study oversight were provided by the Institutional Review Board (IRB) of Wake Forest University Health Sciences.
The CyBER/testing Intervention
The CyBER/testing intervention was based on natural helping (Eng, Rhodes, & Parker, 2009) and implemented by a trained interventionist. The interventionist, a 29-year-old man, was selected because he was part of the local gay community and had an intimate understanding of the online and geographic MSM communities. He had an “insider’s” knowledge of how these communities identify; communicate with one another; network socially and sexually online and in person; and cope with homophobia, homonegativity, stigma, guilt, and fear of discovery and disease.
Given that our partnership had data indicating that a substantial percentage of chatters identify as bisexual and heterosexual (Rhodes, et al., 2002; Rhodes, Hergenrather, et al., 2010; Rhodes, Hergenrather, Yee, & Ramsey, 2007), his knowledge of and participation in various communities of MSM (both self-identifying and non-self-identifying as gay and African American, Latino, and white) helped to further ensure that the intervention was culturally congruent.
The interventionist had personal characteristics that were relevant to the study, including a sense of humor, high self-esteem, and being dedicated, respectful, and realistic. He was comfortable talking, and offering sound (and sex-positive) advice, about sensitive issues (e.g., sexual behavior, HIV, condoms, and HIV and STD testing) and remaining discreet. He also was proficient with accessing, evaluating, and interpreting Internet sexual health resources.
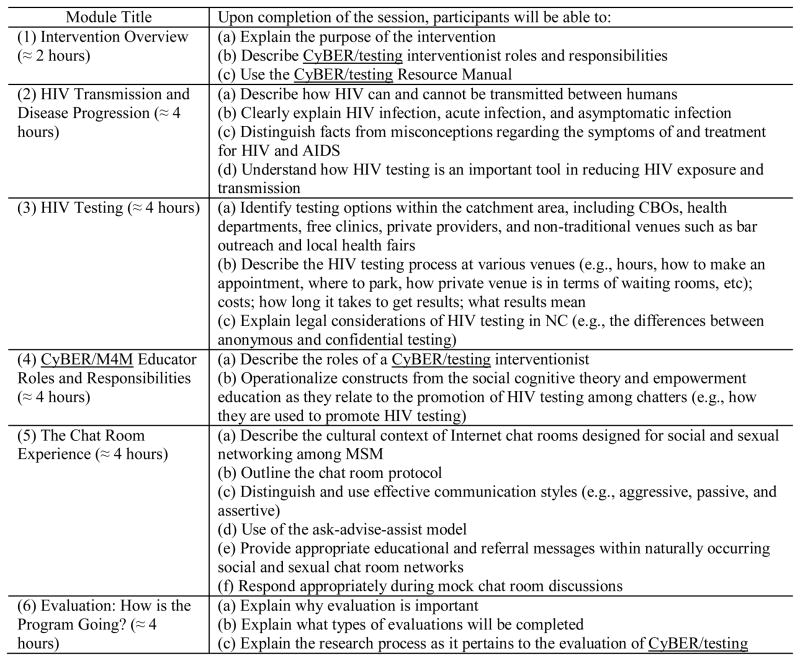
The interventionist training, outlined in Figure 1, included six didactic, interactive, and skills building modules that were included in a comprehensive CyBER/testing Intervention Training Manual. The training introduced the intervention and its approach, and covered HIV transmission and disease progression; testing options (including CBOs, health departments, free clinics, private providers, and non-traditional venues such as bar outreach and local health fairs) and processes (e.g., how to make an appointment, where to park, how private the testing venue is in terms of waiting rooms, how long it takes to get results, etc.) within the catchment area; the differences between anonymous and confidential testing; and interventionist roles and responsibilities.
Figure 1.
The CyBER/testing intervention training modules and abbreviated learning objectives
The interventionist also was trained in social cognitive theory (Bandura, 1994) and empowerment education (Freire, 1973) and how constructs were to be operationalized and used during intervention implementation. For example, because a chatter may be hesitant to enter a health department and ask for an HIV test, the interventionist was trained to increase the chatter’s self-efficacy through identifying and then reducing perceived barriers (e.g., perceptions that the testing process is not confidential, that one will be “judged” by testing staff, that it costs to be tested, etc.)
Because empowerment education posits that individuals must experience the process of learning and critical reflection to “get to” action (Eng, et al., 2005), triggers were used to promote critical consciousness. For example, the interventionist applauded pre-ejaculation withdrawal during “barebacking” (i.e., insertive sex without a condom) as a method of harm minimization, but asked how confident the chatter (who reported this behavior) was that he was not HIV infected. This one-on-one discussion mentioned that guidelines suggest that sexually active MSM get tested annually for HIV and the risks that not knowing one’s status has on both one’s own disease progression and the health of one’s partners. Because community chat room norms and expectations may contribute to risk, raising consciousness about how these factors contribute to risk among individual chatters, others in their sexual networks (both male and female), and MSM communities is best facilitated by a community insider – the interventionist.
The CBPR partnership chose the social cognitive theory and empowerment education after engaging in a multiple step intervention development process as previously described (Rhodes, Hergenrather, Duncan, et al, 2007). Briefly, this process consisted of multiple steps, including the introduction of health behavior theory to members of the CBPR partnership. This introduction allowed the CBPR partnership to appreciate the mechanisms used in existing interventions to promote change in knowledge, attitudes, and/or behaviors and to make informed decisions about the theories that should be infused into this intervention, blended with the real lived experiences of gay men and MSM and the experiences of CBPR partners.
The training also included effective communication and application of the ask-advise-assist model (Whitlock, Orleans, Pender, & Allan, 2002) within the cultural context of chat rooms. The training included opportunities for mock chat room discussions to build interventionist’s proficiency and self-efficacy in the information and the application of the theories to promote HIV testing. The interventionist also was trained in research, including study design, human subjects protection, and data collection. Training was held at the Triad Health Project offices and at Wake Forest University School of Medicine. The interventionist was provided a CyBER/testing Resource Manual to assist him in implementation.
Biweekly intervention meetings were held to allow the research team, which included members of the CBPR partnership, to gauge study progress, problem solve, and ensure that the intervention was implemented according to protocol.
Intervention Implementation
The interventionist was employed by and located at the Triad Health Project and implemented the intervention from his office computer. The CBPR partnership decided that the interventionist would not implement the intervention from his home, home computer, or offsite laptop; this ensured that CyBER/testing was implemented during consistent hours and according to protocol, and that Triad Health Project resources were readily available for referral.
During the six-month implementation phase, the intervention was delivered typically 9AM-5PM Monday-Friday in a chat room that CBPR partners knew to facilitate social and sexual networking among local MSM (Rhodes, Hergenrather, Duncan, et al., 2010). We chose these days because we had evidence from our CyBER/M4M intervention that a majority of chatters who are online on Friday and Saturday also are online during other times during the week. Our partnership selected the schedule after weighing what we currently know about chatters with an eye on intervention reach, what was realistic given the scope and goals of the pilot study, and what mirrored common practice within CBOs, ASOs, and health departments and clinics.
The interventionist entered the chat room, which was an existing room designed for social and sexual networking among MSM within the catchment area. Every 30 minutes, he posted various standardized triggers about HIV testing and his availability to provide information and answer questions about testing within the public chat room. He did not privately “instant-message” (commonly known and referred to as “IM”) other chatters until they instant-messaged him. Our partnership chose this approach to be respectful of the cultural context of the chat room. Chatters were in the chat room for social and sexual networking, not to be inundated with HIV testing messages.
In both the public chat room and through private instant-messaging, the interventionist built trust with chatters through ongoing dialogue that was related to HIV testing; answered questions about testing locations and the processes of testing; referred chatters to other resources (online and in the physical community); explained HIV infection, acute infection, and asymptomatic infection; and engaged in discussions about the importance of knowing one’s HIV serostatus, resources for those who are seropositive (including medical resources and AIDS drug assistance programs [ADAP]), personal responsibility, and HIV-related stigma. The interventionist announced non-traditional testing opportunities as he learned about them. For example, he promoted local health fairs that included HIV testing, bar-based testing nights, and other HIV testing initiatives.
Also to build and maintain trust and his role as a member of the online community, the interventionist chatted about what chatters were doing over the weekend, movies they had seen, and what chatters wanted in a sexual partner. The interventionist was careful to maintain his interventionist role but when appropriate flirted and joked with, and teased, chatters. He did not enter the chat room as a chatter during non-intervention hours.
The interventionist also referred chatters to an online video that the CBPR partnership scripted and produced that highlighted diverse HIV testing experiences through vicarious learning. The video was available on a partner organization’s website and is currently available at: http://www.youtube.com/watch?v=qL8dQLLrLs0. In the video, three gay friends of differing socio-cultural backgrounds and levels of “outness” about their sexual orientation shared their experiences getting tested at a public health department, a local ASO, and a primary care provider’s office.
Data Collection
Two types of data were collected: cross-sectional pretest-post-test, and extant profile data.
Cross-sectional Brief Assessment Data
Cross-sectional baseline pretest data were collected in January 2009 and post-test data were collected in August 2009 from chatters who were recruited from the chat room. To increase the number of chatters who would consent to, and participate in, the assessment, our partnership decided to use a very brief online assessment. Previous research that had been validated by partnership members suggested that chatters were not likely to participate in an assessment that competed with their priorities in the chat room: social and sexual networking (Rhodes, 2004; Rhodes, Bowie, & Hergenrather, 2003). Thus, the pretest assessment included seven items that assessed (1) the chatter’s age in years, (2) what county he lived in, and whether he had: (3) been tested for HIV in the previous 12 months, (4) sex with men and/or women, (5) ever seen the interventionist (by alias) in the chat room, (6) ever chatted with the interventionist, and (7) taken the online assessment before. The post-test assessment included an eighth item to assess whether the chatter had seen the online video. The assessment was not designed to measure theoretical constructs given the need to keep the assessment brief. Response options used binary or drop-down lists to expedite completion and reduce respondent burden.
Using an alias that differed from the alias he used as the interventionist, the interventionist recruited chatters to complete the assessment by posting instant messages in the public room. Typical messages included: “I am doing a survey on this website. Please help me out and take this QUICK & ANONYMOUS Survey on Men’s Health. We are using these questions for a study to help men with health education. The link is [URL address]. IT IS ONLY 7 QUESTIONS! IT TAKES LESS THAN 1 MINUTE TO DO! Your participation is appreciated. If anyone has any questions about this survey, feel free to ask me.”
To ensure participant safety, Internet Protocol (IP) addresses were not collected; no data were stored on users’ computers (e.g., cookies); no personally identifying information was collected by the assessment; Internet provider logs were not stored; data were encrypted in transfer (although no personally identifying information existed) using Secure Sockets Layer (SSL), a protocol designed secure communications on an insecure network such as the Internet; and data were saved on a secured server space using a secure site certificate from GeoTrust.
Extant Profile Data
Because chat room interventions may reach chatters who never interact with the interventionist or complete the assessment, we collected publicly available published profile data of chatters who were in the chat room during a typical implementation week. In this chat room, available profile data included age, geographic location, sexual orientation, race/ethnicity, HIV status, and level of “outness” about one’s sexual orientation.
During five consecutive weeks in April and early May 2009, profile data were collected on one weekday sequentially, Monday through Friday. To illustrate, on Monday of week one, rather than implementing the intervention, the interventionist collected the profiles of each chatter that entered the room during typical intervention implementation hours. During week two, he collected profiles on Tuesday; on week three, he collected profiles on Wednesday. This collection continued until profiles were collected for each day of a typical week. Data from these profiles were entered into an excel spreadsheet. We used these data to describe the types of chatters who would have potentially been exposed to the intervention in the public chat room.
Data Analysis
Brief assessment extant profile data were imported into SPSS 11.5 (Chicago, IL) for analysis. We used univariate analyses to describe characteristics of those who were in the chat room during typical intervention implementation hours using frequencies, percentages, and means, using the extant profile data. Bivariate analyses (t-tests for continuous variables and Chi-squared or Fisher’s Exact tests for categorical variables) were used to identify differences between the pretest-post-test cross-sectional samples by age, gender of sexual partners, and having seen and chatted with the interventionist. Logistic regression was performed to test for differences in HIV testing rates between pretest and post-test and to calculate odds ratios (ORs) and 95% confidence intervals (CI). One-way ANOVA and Chi-squared tests were performed to test differences among pretest, post-test, and profile data. A two-sided p-value <0.05 was considered to be statistically significant.
Results
Chatter Characteristics: Profile Data
During extant profile data collection during intervention implementation, the chat room had 761 chatters, one of whom self-identified as female; all of whom reported being sexually active. After eliminating the female chatter and duplicate aliases, 509 unique chatters were identified. The mean age of these 509 chatters was 37.1 (standard deviation [SD]=10.9) with a range 18–78 years. Nearly three-quarters of the sample of chatters reported living in a 16-county catchment area served by the Triad Health Project. Slightly over 50% self-identified as gay; nearly 20% self-identified as bisexual; and the remaining one quarter did not report sexual identity. The majority of the sample self-identified as White/European; and 1.6% reported being HIV positive. See Table 1 for additional chatter profile data.
Table 1.
Chat room profile data (N=509)
| Characteristic | Mean (±SD) or n (%) |
|---|---|
| Age in years | 37.1 (±10.9) Range 18–78 |
| Location | |
| Within the 16 county catchment area (Alamance, Chatham, Davison, Forsyth, Guilford, Davie, Rowan, Randolph, Montgomery, Moore, Lee, Iredell, Rockingham, Stokes, Surry, Yadkin Counties) | 364 (71.5) |
| Outside NC | 41 (8.1) |
| Undisclosed | 27 (5.3) |
| Sexual orientation | |
| Gay | 295 (58.0) |
| Bisexual | 91 (17.8) |
| Undisclosed | 123 (24.2) |
| Race/ethnicity | |
| African/African American/Black | 15 (3.0) |
| Asian/Pacific Islander | 3 (0.6) |
| Latino | 9 (1.8) |
| Mixed race/ethnicity | 12 (2.4) |
| White/European | 363 (71.3) |
| Undisclosed | 106 (20.8) |
| HIV status | |
| HIV+ | 8 (1.6) |
| Undisclosed | 115 (22.6) |
| Outness | |
| Undisclosed | 392 (77.0) |
| Not out at all | 22 (4.3) |
| Not out at work | 6 (1.2) |
| To some people | 45 (8.8) |
| To all but family | 3 (0.6) |
| Totally | 37 (7.3) |
Cross-sectional Data
Table 2 presents comparisons of participant characteristics between each cross-sectional sample. Mean age of the participants in the baseline assessment (n=346) and the post-test assessment (n=315) was 37.2 and 36.9 years, respectively. There were no significant differences by age or sexual partner type (i.e., men and/or women). Predictably, few participants reported seeing or chatting with the interventionist in the pretest, while at post-test, nearly two-thirds reported seeing the interventionist online (n=197) and one-third reported chatting with the interventionist (n=112).
Table 2.
Characteristics of participants in each cross-sectional sample (N=661)
| Characteristic | Pretest (n= 346) | Post-test (n=315) | P |
|---|---|---|---|
| Mean age in years | 37.2 (±11.3); range 17–65 | 36.9 (±11.8); range 18–65 | .7 |
|
| |||
| Sex | .5 | ||
| With men | 272 (78.6%) | 255 (81.0%) | |
| With men and women | 74 (21.4%) | 60 (19.0%) | |
|
| |||
| Seen the interventionist in the chat room | 22 (6.4%) | 197 (62.5%) | <.001 |
|
| |||
| Chatted with the interventionist | 4 (1.2%) | 112 (35.6%) | <.001 |
Table 3 presents HIV testing percentages, the ORs, 95% CIs, and significance levels between pretest and post-test. Chatters in the post-test had significantly higher rates of HIV testing than chatters in the pretest (p<0.001). Using the pretest sample as the referent group, chatters had an increased odds of reporting HIV testing at post-test (OR=1.8; 95% CI=1.4, 2.5). Furthermore, examining subgroups of chatters, chatters who reported only male sexual partners had an increased odds of reporting HIV testing within the past 12 months (OR=1.4; 95% CI=1.1, 2.0). Chatters who reported both male and female sexual partners had an increased odds of reporting HIV testing within the past 12 months (OR=5.7; 95% CI=2.6, 12.6).
Table 3.
HIV testing between participants in each cross-sectional sample (N=661)
| Characteristic | Pretest (n= 346) | Post-test (n=315) | OR (95% CI) | P |
|---|---|---|---|---|
| Tested for HIV during the past 12 months | 154 (44.5%) | 187 (59.4%) | 1.8 (1.4, 2.5) | <.001 |
| Among chatters reporting only male partners | 141 (51.8%) | 154 (60.4%) | 1.4 (1.1, 2.0) | .04 |
| Among chatters reporting male and female partners | 13 (17.6%) | 33 (55.0%) | 5.7 (2.6, 12.6) | <.001 |
Profile and Cross-sectional Data Comparisons
To determine how representative the chatters who completed the assessment were to the larger online community of chatters, we compared the two common variables from the profile data with both the pretest and post-test data: age and sexual partner type (i.e., men and/or women). There were no significant differences across the three samples by age (p=0.93) and partner type (p=0.12).
Discussion
Findings from this quasi-experimental, pretest-post-test cross-sectional study suggest that a chat room-based intervention among MSM has promise as an approach to increase HIV testing within this population. At pretest, 45% of all chatters reported having had an HIV test while at post-test nearly 60% reported having had an HIV test. Among chatters who reported having sex with both men and women, the difference was even more profound with about 18% reporting having had an HIV test at pretest and 55% reporting having had an HIV test at post-test. Thus, after the intervention, chatters who reported having sex with both men and women had nearly six times the odds of reporting being tested for HIV. This finding is particularly important given that MSM who have sex with both men and women are difficult to reach for participation in traditional HIV prevention interventions. These MSM may not be exposed to venue-based prevention efforts (e.g., gay bar or community based), disclose risks to healthcare providers, or identify with gay-focused prevention messages (Flores, Bakeman, Millett, & Peterson, 2009; Lauby & Milnamow, 2009; Rhodes, Hergenrather, Yee, & Ramsey, 2007; Shoptaw, et al., 2009).
We do not know with certainty how similar those who completed the brief assessment are to other chatters in the room. It has been suggested that chatters who participate in online assessments may be at less risk, relatively, than those who do not participate in online assessments (Rhodes, Hergenrather, Yee, Knipper, et al., 2007; Ross, et al., 2000); however, when comparing those who completed the brief assessment to the extant profile data, no differences existed between the groups in terms of mean age or sexual partner type.
The Use of CBPR
Much of the success of this intervention and its evaluation is attributable to the CBPR approach used. The impetus for this study came from members within the community who wanted to harness the strengths of the Internet and the existing social networks within chat rooms. The study design and methods were developed by CBPR partnership using a negotiation and consensus building approach to decision making. For example, although more comprehensive data would have supported the evaluation of this intervention, partnership members knew that a tradeoff between comprehensiveness and potential success of collecting data was necessary. A longer assessment would not have been completed by chatters who may have benefited from the intervention but been unlikely to commit the time (and distraction from their primary reasons for being in the chat room) to complete a longer assessment. This type of negotiation is typical within CBPR and illustrates one of many key roles community partners play in ensuring research is feasible and meaningful.
The CyBER/testing intervention itself was developed, refined, and implemented by the partnership based on lessons learned from the original CyBER/M4M intervention (Rhodes, Hergenrather, Duncan, et al., 2007). Because the intervention was implemented within an existing chat room for social and sexual networking among MSM, partners were careful to ensure that the interventionist was well trained but also that the interventionist had characteristics of a natural helper. The interventionist neither received an official reprimand from the host of the chat room nor was removed from the room. He followed the community norms, just as any interventionist would in a bar, adult bookstore public sex setting, or in partnership with a soccer league, as examples. In fact, when an occasional chatter accused the interventionist of being an Internet robot or “bot” (e.g., a software application that runs automated tasks over the Internet), other chatters defended the interventionist and his right to be online in the chat room. Because he was a community insider, he gained the trust and support of regular chatters.
An outcome that we had not foreseen was the role of the interventionist as a community advocate. Although he was trained to offer advice about where to get tested to meet the needs and reduce concerns of the chatters, he also built trust with local HIV testing staff. He was able to provide staff with insights into the challenges and barriers to testing that chatters identified and expressed online. The role of the community advocate in natural helping is important but often neglected as communities have individual-level change needs that may supersede systems change (Eng & Young, 1992; Rhodes, Hergenrather, Bloom, et al., 2009).
Furthermore, while the CBPR partnership has been building its research capacities and experiences, this study contributed to the development of research capacities and experiences among staff at Triad Health Project specifically. These staff members are newer members to the partnership, and this type of study not only may have made an appreciable difference in terms of HIV testing among MSM considered to be difficult to find and reach for HIV prevention but also nurtured trust among CBPR partners and further developed the critical thinking and research skills of staff at Triad Health Project. Similarly, academic researchers increased their ability to “think outside the box” to ensure that the intervention had high ecological validity (Devieux, et al., 2005).
Limitations
There are several limitations that should be acknowledged. First, this study design was cross sectional and findings should be interpreted with caution; however, these promising findings warrant a more rigorous study design. Future studies may choose a stronger design by comparing multiple intervention and comparison chat rooms longitudinally, or add additional time points with or without treatment to assess intervention effects over time. It would be useful to include multiple interventionists in subsequent studies to increase generalizability.
Second, because of the potential of alternate explanations for increased HIV testing among MSM such as a new public awareness campaign, we interviewed local and state level health department representatives who reported that no new initiative was implemented during the CyBER/testing intervention implementation. Furthermore, post hoc analyses indicated that two groups of chatters – those who reported having seen and those who reported having chatted with the interventionist online – were more likely to report being tested at post-test than those who did not report having seen or chatted with the interventionist (p<.001). Chatters who reported having seen (versus those who reported not having seen) the online video were no more likely to report being tested at post-test (p=.09).
Although our previous research was successful reaching African American chatters (Rhodes, Hergenrather, Duncan, et al., 2010; Rhodes, Hergenrather, Yee, Knipper, et al., 2007), this intervention did not reach these chatters. Extant profile data indicated that only 3% of the chatters who were online during implementation hours self-identified as African American/Black. Further research is needed to determine whether African American MSM are in the chat room at other times or whether these MSM are using other site hosts. Online trends change rapidly, and many African American MSM in our catchment areas use two additional Internet site hosts for social and sexual networking. One site does not offer “in real time” chat; rather, chatters communicate by electronic-mail (e-mail). Research is needed to explore how to utilize e-mail communications for intervention implementation while being culturally congruent and not targeting individual chatters with unwelcomed messages. The second site offers “in real time” chat but does not have rooms delineated by geographic locations. Instead rooms are national; thus, targeting chatters with local information may be difficult (Rhodes, Hergenrather, Vissman, et al., In press). Similarly, we have found low levels of chat room use among Latino MSM (Rhodes, Yee, & Hergenrather, 2006).
Furthermore, we implemented this intervention during limited hours. Although we had support for our intervention implementation time period, further exploration is needed to determine whether the intervention missed some chatters (e.g., chatters who were not online during intervention implementation).
Finally, the validity of online profile data is not clear. Chatters may present themselves in a socially desirable manner. However, extant profile data did not differ significantly from the cross-sectional brief assessment data.
Implications for Practice
Some CBOs, ASOs, and health departments and clinics have responded to sexual risk among MSM who use chat rooms for sexual networking by implementing chat room-based interventions to reduce the risk of exposure to and transmission of HIV and other STDs. However, this is the first study of which we are aware to provide preliminary evidence that an Internet-based, natural helping intervention based on social cognitive theory and empowerment education is feasible, appropriate for use to reach MSM, and most importantly, can be effective. This type of intervention also may reach MSM who are less likely to be reached through traditional outreach, such as outreach in gay bars, because they may be less likely to identify as gay and thus be less likely found in gay venues.
The intervention did not require recruitment to or implementation of a standardized program that is not authentic to the lived experiences of MSM at risk; rather, CyBER/testing was implemented within the existing structure of the chat room and thus reached MSM, who have been identified as at risk, “where they are” without a burdensome enrollment process or their having to participate in an intense intervention. The commitment for participation by MSM was minimal, and the intervention was designed to “demystify” HIV testing and link MSM to existing HIV testing services.
Staff from CBOs, ASOs, and health departments and clinics who want to implement such an intervention can benefit from knowing that this type of intervention is feasible and may meet the health promotion and disease prevention needs of members of a hard-to-reach and potentially at-risk community. Our partnership saw this research as step in building trust and developing capacity to engage in CBPR, while determining whether a chat room-based intervention could increase HIV testing. To reduce health disparities among some of the most vulnerable communities, we must act creatively, developing new partnerships, building trust through incremental research steps, and utilizing mixed frameworks to improve community health, and more rigorous studies are needed to further demonstrate the efficacy of this type of intervention.
References
- Anderton JP, Valdiserri RO. Combating syphilis and HIV among users of internet chatrooms. Journal of Health Communication. 2005;10:665–671. doi: 10.1080/10810730500269007. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social cognitive theory and the exercise over HIV infection. In: DiClemente RJ, Peterson JL, editors. Preventing AIDS: Theories and Methods of Behavioral Intervention. New York, NY: Plenum Press; 1994. pp. 25–59. [Google Scholar]
- Benotsch EG, Kalichman S, Cage M. Men who have met sex partners via the Internet: prevalence, predictors, and implications for HIV prevention. Archives of Sexual Behavior. 2002;31:177–183. doi: 10.1023/a:1014739203657. [DOI] [PubMed] [Google Scholar]
- Berry M, Raymond HF, Kellogg T, McFarland W. The Internet, HIV serosorting and transmission risk among men who have sex with men, San Francisco. AIDS. 2008;22:787–789. doi: 10.1097/QAD.0b013e3282f55559. [DOI] [PubMed] [Google Scholar]
- Bolding G, Davis M, Sherr L, Hart G, Elford J. Use of gay Internet sites and views about online health promotion among men who have sex with men. AIDS Care. 2004;16:993–1001. doi: 10.1080/09540120412331292453. [DOI] [PubMed] [Google Scholar]
- Bowen AM, Williams ML, Daniel CM, Clayton S. Internet based HIV prevention research targeting rural MSM: feasibility, acceptability, and preliminary efficacy. Journal of Behavioral Medicine. 2008;31:463–477. doi: 10.1007/s10865-008-9171-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bull SS, McFarlane M. Soliciting sex on the Internet: what are the risks for sexually transmitted diseases and HIV? Sexually Transmitted Diseases. 2000;27:545–550. doi: 10.1097/00007435-200010000-00008. [DOI] [PubMed] [Google Scholar]
- Cashman SB, Adeky S, Allen AJ, 3rd, Corburn J, Israel BA, Montano J, et al. The power and the promise: working with communities to analyze data, interpret findings, and get to outcomes. American Journal of Public Health. 2008;98:1407–1417. doi: 10.2105/AJPH.2007.113571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Workowski KA, Berman SM Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2006. MMWR Recommendations and Reports. 2006;55(RR-11):1–94. [PubMed] [Google Scholar]
- Chiasson MA, Parsons JT, Tesoriero JM, Carballo-Dieguez A, Hirshfield S, Remien RH. HIV behavioral research online. Journal of Urban Health. 2006;83:73–85. doi: 10.1007/s11524-005-9008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman E, Horvath KJ, Miner M, Ross MW, Oakes M, Rosser BR. Compulsive sexual behavior and risk for unsafe sex among Internet using men who have sex with men. Archives of Sexual Behavior. doi: 10.1007/s10508-009-9507-5. (In press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devieux JG, Malow RM, Rosenberg R, Jean-Gilles M, Samuels D, Ergon-Perez E, et al. Cultural adaptation in translational research: field experiences. Journal of Urban Health. 2005;82(2 Suppl 3):iii82–91. doi: 10.1093/jurban/jti066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elford J, Bolding G, Davis M, Sherr L, Hart G. Web-based behavioral surveillance among men who have sex with men: a comparison of online and offline samples in London, UK. Journal of Acquired Immune Deficiency Syndromes. 2004;35:421–426. doi: 10.1097/00126334-200404010-00012. [DOI] [PubMed] [Google Scholar]
- Eng E, Moore KS, Rhodes SD, Griffith D, Allison L, Shirah K, et al. Insiders and outsiders assess who is “the community”: Participant observation, key informant interview, focus group interview, and community forum. In: Israel BA, Eng E, Schulz AJ, Parker E, editors. Methods for Conducting Community-Based Participatory Research for Health. San Francisco, CA: Jossey-Bass; 2005. pp. 77–100. [Google Scholar]
- Eng E, Rhodes SD, Parker EA. Natural helper models to enhance a community’s health and competence. In: DiClemente RJ, Crosby RA, Kegler MC, editors. Emerging theories in Health Promotion Practice and Research. Vol. 2. San Francisco, CA: Jossey-Bass; 2009. pp. 303–330. [Google Scholar]
- Eng E, Young R. Lay health advisors as community change agents. Family and Community Health. 1992;15:24–40. [Google Scholar]
- Flores SA, Bakeman R, Millett GA, Peterson JL. HIV risk among bisexually and homosexually active racially diverse young men. Sexually Transmitted Diseases. 2009;36:325–329. doi: 10.1097/OLQ.0b013e3181924201. [DOI] [PubMed] [Google Scholar]
- Freire P. Education for critical consciousness. New York, NY: Seabury Press; 1973. [Google Scholar]
- Garofalo R, Herrick A, Mustanski BS, Donenberg GR. Tip of the iceberg: Young men who have sex with men, the Internet, and HIV risk. American Journal of Public Health. 2007;97:1113–1117. doi: 10.2105/AJPH.2005.075630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvath KJ, Rosser BR, Remafedi G. Sexual risk taking among young internet-using men who have sex with men. American Journal of Public Health. 2008;98:1059–1067. doi: 10.2105/AJPH.2007.111070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Israel BA, Schulz AJ, Parker EA, Becker AB, Allen AJ, Guzman R. Critical issues in developing and following community based participatory research issues. In: Minkler M, Wallerstein N, editors. Community-Based Participatory Research for Health. San Francisco, CA: Jossey-Bass; 2003. pp. 53–76. [Google Scholar]
- Klausner JD, Wolf W, Fischer-Ponce L, Zolt I, Katz MH. Tracing a syphilis outbreak through cyberspace. Journal of the American Medical Association. 2000;284:447–449. doi: 10.1001/jama.284.4.447. [DOI] [PubMed] [Google Scholar]
- Lauby JL, Milnamow M. Where MSM have their first HIV test: differences by race, income, and sexual identity. American Journal of Men’s Health. 2009;3:50–59. doi: 10.1177/1557988307313465. [DOI] [PubMed] [Google Scholar]
- McFarlane M, Bull SS, Rietmeijer CA. The Internet as a newly emerging risk environment for sexually transmitted diseases. Journal of the American Medical Association. 2000;284:443–446. doi: 10.1001/jama.284.4.443. [DOI] [PubMed] [Google Scholar]
- Mikolajczak J, Hospers HJ, Kok G. Reasons for not taking an HIV-test among untested men who have sex with men: an Internet study. AIDS and Behavior. 2006;10:431–435. doi: 10.1007/s10461-006-9068-8. [DOI] [PubMed] [Google Scholar]
- Moskowitz DA, Melton D, Owczarzak J. PowerON: the use of instant message counseling and the Internet to facilitate HIV/STD education and prevention. Patient Education and Counseling. 2009;77:20–26. doi: 10.1016/j.pec.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nartz M, Schoech D. Use of the Internet for community practice: A Delphi study. Journal of Community Practice. 2000;8:37–59. [Google Scholar]
- Noar SM, Black HG, Pierce LB. Efficacy of computer technology-based HIV prevention interventions: a meta-analysis. AIDS. 2009;23:107–115. doi: 10.1097/QAD.0b013e32831c5500. [DOI] [PubMed] [Google Scholar]
- Ogilvie GS, Taylor DL, Trussler T, Marchand R, Gilbert M, Moniruzzaman A, et al. Seeking sexual partners on the internet: a marker for risky sexual behaviour in men who have sex with men. Canadian Journal of Public Health. 2008;99:185–188. doi: 10.1007/BF03405470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD. Hookups or health promotion? An exploratory study of a chat room-based HIV prevention intervention for men who have sex with men. AIDS Education and Prevention. 2004;16:315–327. doi: 10.1521/aeap.16.4.315.40399. [DOI] [PubMed] [Google Scholar]
- Rhodes SD, Bowie DA, Hergenrather KC. Collecting behavioural data using the world wide web: considerations for researchers. Journal of Epidemiology and Community Health. 2003;57:68–73. doi: 10.1136/jech.57.1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD, DiClemente RJ, Cecil H, Hergenrather KC, Yee LJ. Risk among men who have sex with men in the United States: a comparison of an Internet sample and a conventional outreach sample. AIDS Education and Prevention. 2002;14:41–50. doi: 10.1521/aeap.14.1.41.24334. [DOI] [PubMed] [Google Scholar]
- Rhodes SD, Hergenrather KC, Bloom FR, Leichliter JS, Montaño J. Outcomes from a community-based, participatory lay health advisor HIV/STD prevention intervention for recently arrived immigrant Latino men in rural North Carolina, USA. AIDS Education and Prevention. 2009;21:104–109. doi: 10.1521/aeap.2009.21.5_supp.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD, Hergenrather KC, Duncan J, Vissman AT, Miller C, Wilkin AM, et al. A pilot intervention utilizing Internet chat rooms to prevent HIV risk behaviors among men who have sex with men. Public Health Reports, 125, Supplement. 2010;1:29–37. doi: 10.1177/00333549101250S105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD, Hergenrather KC, Vissman AT, Stowers J, Davis AB, Hannah A, Alonzo J, Marsiglia FF. Boys must be men, and men must have sex with women: A qualitative CBPR study to explore sexual risk among African Ameircna, Latino and white gya men and MSM. American Journal of Men’s Health. doi: 10.1177/1557988310366298. (In press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD, Hergenrather KC, Yee LJ, Knipper E, Wilkin AM, Omli MR. Characteristics of a sample of men who have sex with men, recruited from gay bars and internet chat rooms, who report methamphetamine use. AIDS Patient Care and STDS. 2007;21:575–583. doi: 10.1089/apc.2007.0002. [DOI] [PubMed] [Google Scholar]
- Rhodes SD, Hergenrather KC, Yee LJ, Ramsey B. Comparing MSM in the Southeastern United States who participated in an HIV prevention chat room-based outreach intervention and those who did not: how different are the baseline HIV-risk profiles? Health Education Research. 2007;23:180–190. doi: 10.1093/her/cym015. [DOI] [PubMed] [Google Scholar]
- Rhodes SD, Hergenrather KC, Duncan J, Ramsey B, Yee LJ, Wilkin AM. Using community-based participatory research to develop a chat room-based HIV prevention intervention for gay men. Progress in Community Health Partnerships: Research, Education, and Action. 2007;1:175–184. doi: 10.1353/cpr.2007.0013. [DOI] [PubMed] [Google Scholar]
- Rhodes SD, Malow R, Jolly C. An introduction to community-based participatory research (CBPR): A new and not-so-new approach to HIV prevention, care, and treatment. AIDS Education and Prevention. 2010;22:183–183. doi: 10.1521/aeap.2010.22.3.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD, Yee LJ, Hergenrather KC. A community-based rapid assessment of HIV behavioural risk disparities within a large sample of gay men in southeastern USA: a comparison of African American, Latino and white men. AIDS Care. 2006;18:1018–1024. doi: 10.1080/09540120600568731. [DOI] [PubMed] [Google Scholar]
- Ross MW, Tikkanen R, Mansson SA. Differences between Internet samples and conventional samples of men who have sex with men: implications for research and HIV interventions. Social Science and Medicine. 2000;51:749–758. doi: 10.1016/s0277-9536(99)00493-1. [DOI] [PubMed] [Google Scholar]
- Rosser BR, Miner MH, Bockting WO, Ross MW, Konstan J, Gurak L, et al. HIV risk and the internet: results of the Men’s INTernet Sex (MINTS) Study. AIDS and Behavior. 2009;13:746–756. doi: 10.1007/s10461-008-9399-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez T, Finlayson T, Drake A, Behel S, Cribbin M, Dinenno E, et al. Human immunodeficiency virus (HIV) risk, prevention, and testing behaviors - United States, National HIV Behavioral Surveillance System: men who have sex with men, November 2003-April 2005. MMWR Surveillance Summary. 2006;55:1–16. [PubMed] [Google Scholar]
- Shoptaw S, Weiss RE, Munjas B, Hucks-Ortiz C, Young SD, Larkins S, et al. Homonegativity, substance use, sexual risk behaviors, and HIV status in poor and ethnic men who have sex with men in Los Angeles. Journal of Urban Health. 2009;86(Suppl 1):77–92. doi: 10.1007/s11524-009-9372-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silenzio VM, Duberstein PR, Tang W, Lu N, Tu X, Homan CM. Connecting the invisible dots: reaching lesbian, gay, and bisexual adolescents and young adults at risk for suicide through online social networks. Social Science and Medicine. 2009;69:469–474. doi: 10.1016/j.socscimed.2009.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinhardt LS, Carey MP, Johnson BT, Bickham NL. Effects of HIV counseling and testing on sexual risk behavior: a meta-analytic review of published research, 1985–1997. American Journal of Public Health. 1999;89:1397–1405. doi: 10.2105/ajph.89.9.1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitlock EP, Orleans CT, Pender N, Allan J. Evaluating primary care behavioral counseling interventions: an evidence-based approach. American Journal of Preventive Medicine. 2002;22:267–284. doi: 10.1016/s0749-3797(02)00415-4. [DOI] [PubMed] [Google Scholar]
- Ybarra ML, Bull SS. Current trends in Internet- and cell phone-based HIV prevention and intervention programs. Current HIV/AIDS Reports. 2007;4:201–207. doi: 10.1007/s11904-007-0029-2. [DOI] [PubMed] [Google Scholar]