Abstract
Background
American College of Cardiology/American Heart Association guidelines describe the perioperative evaluation as “a unique opportunity to identify patients with hypertension,” however factors such as anticipatory stress or medication noncompliance may induce a bias toward higher blood pressure, leaving clinicians unsure about how to interpret preoperative hypertension. Information describing the relationship between preoperative intake blood pressure and primary care measurements could help anesthesiologists make primary care referrals for improved blood pressure control in an evidence-based fashion. We hypothesized that the preoperative examination provides a useful basis for initiating primary care blood pressure referral.
Methods
We analyzed retrospective data on 2807 patients who arrived from home for surgery and who were subsequently evaluated within 6 months after surgery in the primary care center of the same institution. After descriptive analysis, we conducted multiple linear regression analysis to identify day-of-surgery (DOS) factors associated with subsequent primary care blood pressure. We calculated the sensitivity, specificity, and positive and negative predictive value of different blood pressure referral thresholds using both a single-measurement and a two-stage screen incorporating recent preoperative and DOS measurements for identifying patients with subsequently elevated primary care blood pressure.
Results
DOS systolic blood pressure (SBP) was higher than subsequent primary care SBP by a mean bias of 5.5mmHg (95% limits of agreement +43.8 to −32.8). DOS diastolic blood pressure (DBP) was higher than subsequent primary care DBP by a mean bias of 1.5mmHg (95% limits of agreement +13.0 to −10.0). Linear regression of DOS factors explained 19% of the variability in primary care SBP and 29% of the variability in DBP. Accounting for the observed bias, a two-stage SBP referral screen requiring preoperative clinic SBP≥140mmHg and DOS SBP≥146mmHg had 95.9% estimated specificity (95% CI 94.4 to 97.0) for identifying subsequent primary care SBP≥140mmHg and estimated sensitivity of 26.8% (95% CI 22.0 to 32.0). A similarly high specificity using a single DOS SBP required a threshold SBP≥160mmHg, for which estimated specificity was 95.2% (95% CI 94.2 to 96.1). For DBP, a presenting DOS DBP≥92mmHg had 95.7% specificity (95% CI 94.8 to 96.4) for subsequent primary care DBP≥90mmHg with a sensitivity of 18.8% (95% CI 14.4 to 24.0).
Conclusion
A small bias toward higher DOS blood pressures relative to subsequent primary care measurements was observed. DOS factors predicted only a small proportion of the observed variation. Accounting for the observed bias, a two-stage SBP threshold and a single-reading DBP threshold were highly specific though insensitive for identifying subsequent primary care blood pressure elevation.
Introduction
While it is widely assumed that because of anticipatory stress, or other factors such as medication noncompliance, preoperative day-of-surgery (DOS) blood pressure readings are elevated relative to the primary care setting, studies specifically comparing preoperative and subsequent primary care vital signs are lacking in the medical literature. This lack of published data persists despite strong evidence from the primary care literature that identification and better management of patients who have chronically elevated blood pressure carries a significant public health benefit in terms of reduced morbidity and mortality.2 Consistent with the recognized importance of appropriate blood pressure control, American College of Cardiology/American Heart Association guidelines have suggested that the perioperative examination is “a unique opportunity to identify patients with hypertension and initiate appropriate therapy.1”
Data characterizing the utility of preoperative blood pressure measurements for identifying subsequent primary care blood pressure elevation would therefore not only be of importance for public health, but also would provide an evidence base for current American College of Cardiology/American Heart Association recommendations. Literature on preoperative hypertension in anesthesiology has often focused either on perioperative risk modeling or on the issue of whether to cancel cases for severely elevated blood pressure.3 Although such questions are of great importance for the specialty, anesthesiologists regularly care for large numbers of mildly to moderately hypertensive patients in the perioperative period with little evidence to guide referral decisions.
The aims of the present study were thus to: 1) describe the relationship between initial DOS systolic and diastolic blood pressure (SBP and DBP) and subsequent primary care blood pressure, including identification of the mean bias and 95% limits of agreement, 2) identify independent DOS predictors of postoperative primary care blood pressure, and 3) assess the sensitivity, specificity, and positive and negative predictive value of a screen based on the initial DOS blood pressure measurement as well as a combined screen using both the DOS measurement and a recent presurgical evaluation for making referral decisions.
Methods
Formation of the database
Study investigators sought and received approval for creation of the Veterans Administration Perioperative Outcomes Research (VAPOR) database from the IRB of the Veterans Affairs (VA) Connecticut - West Haven Campus and the Human Investigations Committee at the Yale University School of Medicine. Both approvals included a waiver of the requirement of informed consent.
Patients were identified for inclusion in the VAPOR database if 1) their electronic medical record from the Veterans Health Information Systems and Technology Architecture (VISTA) database contained an Anesthesia Intraoperative Note from the period of June 2006 – December 2009, and 2) their vital signs (noninvasive blood pressure and heart rate) from the same day were obtained in the Ambulatory Procedures Unit (APU), the point of intake and evaluation for surgical patients arriving from home. This selection process excluded individuals who were inpatients before their surgery. For those patients who had more than one anesthetic, only their most recent encounter was brought into the dataset. These procedures identified 4159 unique anesthesia patients arriving from home for surgery.
For the entire cohort, vital signs assessments in the 6 months after surgery, marked by clinic location of measurement, were queried to identify assessments performed in the primary care center. Of these, the most proximate SBP, DBP, and heart rate for each patient from after the date of surgery were then included in the dataset. Primary care center vital signs within 183 days (6 months) following the date of surgery were found for 2812 patients, representing 68% of the ambulatory surgical cohort. The VISTA database was again queried to obtain vital sign measurements recorded at a preoperative evaluation within 30-days preceding the DOS.
Although the method of vital sign measurement was not dictated by this retrospective study, the general practice of the primary care center, the preoperative clinics, and the APU was for a nurse or nurse-assistant to measure blood pressure using an automated, noninvasive blood pressure cuff placed over the brachial artery with the patient in a sitting position.
Demographics including date of birth, gender, marital status, and self-identified race were included in the database. Due to the small numbers of self-identified race other than African-American or Caucasian, race was converted into a single dichotomous variable of black/not-black. Marital status was recoded as married or not married. The most proximate height and weight to the DOS were included in the dataset and converted to body mass index (BMI) as weight in kilograms divided by the square of the height in meters.
The cohort was classified by surgery type into a dichotomized variable of cardiothoracic/vascular surgery and all others on the basis of the APU intake classification. International Classification of Disease - 9 clinical modification (ICD-9 CM) diagnostic codes were used to classify comorbidities for each patient up to and including the DOS. Using the Veterans Aging Cohort Study (VACS)4–6 groupings, a history of the following comorbidities that were a priori suspected to affect the relationship between DOS and primary care vital signs were included in the dataset: alcoholism, anxiety disorder, atrial fibrillation, bipolar disorder, coronary artery disease, cerebrovascular disease (including stroke and transient ischemic attack), cocaine abuse, congestive heart failure, major depression, diabetes, drug abuse, hypertension, kidney disease, peripheral vascular disease, posttraumatic stress disorder, psychosis, schizoaffective disorder, and schizophrenia. The complete list of ICD-9 CM codes used to compile the above comorbidity classifications is available at the VACS website.7 In order to avoid a multiplicity of overlapping comorbid variables, some of the above VACS comorbidity groupings were consolidated into the following system-based variables: 1) Thought disorders were combined into a single psychotic disorder variable, 2) Drug and alcohol abuse were combined into a single substance abuse variable.
Cohort VA pharmacy records for the six months preceding the DOS were queried to identify the presence or absence of a filled prescription for different classes of antihypertensive medication using VA drug class codes. The codes selected for analysis comprised the following drug classes: angiotensin converting enzyme-inhibitor, angiotensin II receptor blocker (ARB), antianginal, beta blocker, calcium channel blocker, loop diuretic, thiazide-type diuretic, and combination antihypertensive (pills containing multiple active drugs). Due to the small proportion of study patients taking ARBs, we consolidated angiotensin converting enzymeinhibitors and ARBs into a single variable.
Other variables that were brought into the database for consideration included the hour of day that the DOS blood pressure evaluation occurred as well as the number of days between the DOS evaluation and subsequent primary care evaluation.
Data Analyses
After creation of the VAPOR database, we performed an overall descriptive analysis comparing subjects who were subsequently evaluated in primary care with those who were not. Outliers from the primary care group in whom a blood pressure value exceeded the investigator-defined valid physiologic range (SBP>230mmHg, SBP<80mmHg, DBP>120mmHg, or DBP<30mmHg) were checked against the electronic medical record to consider exclusion from the dataset as possible clerical errors on the part of the entering clinician. Similar procedures were followed for outliers in heart rate (<30 beats/min or >180 beats/min) and BMI (<10 or >80). Subjects with an aberrant heart rate or BMI entry, with otherwise appropriate vital signs, were retained in the primary analysis of blood pressure changes. All descriptive data are presented as mean (SD) for normally distributed continuous variables, median (interquartile range) for nonnormally distributed continuous data, or number (percent) for categorical data as appropriate.
The following four sets of analyses were then conducted:
To ascertain the overall relationship between blood pressure measurements, DOS and subsequent primary care measurements were displayed on simple scatter plots. The Pearson’s correlation coefficient and a regression line with 95% confidence bands were calculated. The mean bias and 95% limits of agreement were also calculated and shown via Bland-Altman plots.
Multiple linear regression modeling was conducted to identify DOS factors that were independently associated with subsequent primary care SBP and DBP and to offer an overall estimate of the variation in subsequent primary care blood pressure that could be accounted for by the DOS factors contained in the database. One linear regression model was created using primary care SBP as the dependent variable, and a second model was created using primary care DBP as the dependent variable. For both models, DOS variables with suspected clinical relevance to subsequent primary care blood pressure were selected and considered for entry into the multiple linear regression models by first performing univariate linear regression analysis of the possible association of each independent variable with primary care SBP or DBP, respectively. In addition, we considered entering a term to test the interaction between atrial fibrillation and DOS heart rate, reasoning that increased heart rate among patients with a history of paroxysmal atrial fibrillation was more likely to be indicative of reversion to atrial fibrillation and an associated decrease in cardiac output and blood pressure. Only the subset of variables with p≤0.2 was retained for entry in the multiple linear regression models. Collinearity diagnostics were performed to assure adequate independence of these variables for multiple regression analysis. Final results are reported as β (95% CI) and p-value of the partial-F statistic for each independent variable with p<0.05 considered the threshold of statistical significance.
Because the decision to refer for blood pressure evaluation is fundamentally a dichotomous clinical decision point, we separated the postoperative primary care blood pressure values into “elevated” and “not elevated” categories based on a cutoff of 140mmHg or more for SBP and 90mmHg or more for DBP. This cutoff was based on criteria published in the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7).8 We then calculated the sensitivity, specificity, and positive and negative predictive value of two different DOS blood pressure thresholds for identifying patients with subsequently elevated primary care blood pressures. The first DOS threshold chosen was 140/90mmHg, in line with JNC 7 criteria. The second threshold chosen was 146/92mmHg. This threshold was selected after performance of the Bland-Altman analyses and was meant to incorporate the DOS bias seen in our data. All sensitivity and specificity calculations are reported as percent (95% CI).
Because of the excessive variability observed in any single blood pressure measurement, the JNC 7 suggests that decisions regarding the diagnosis and treatment of hypertension be based on at least two blood pressure measurements. To account for this recommendation, and keeping within the limitations of data available in our local VISTA database, we investigated the utility of a two-stage screen for identifying patients with elevated postoperative primary care blood pressure by analyzing a subset of patients who had blood pressure data available from a recent (within 30-days) preoperative evaluation. For this two-stage screen, we required that patients demonstrate elevated blood pressure at both time points. Sensitivity, specificity and positive and negative predictive value were calculated using 140/90mmHg thresholds for both the preoperative and DOS measurements and then using 140/90mmHg at the preoperative visit with 146/92mmHg as the DOS thresholds.
Results
The overall descriptive analysis comparing subjects who were subsequently evaluated in primary care (N=2812) with those who were not (N=1347) demonstrated that patients with follow-up in the primary care center tended to be older (mean of 66 vs. 61 years; p<0.001) and to have more comorbid illness than those without follow-up (p<0.001 for difference in prevalence of each comorbid condition with the exception of kidney disease which was not significantly different).
Of the 2812 subjects available for the analysis, the procedure for identifying outliers demonstrated 5 (0.18%) subjects who were felt to have erroneous blood pressure entries and were thus excluded, leaving 2807 subjects with valid blood pressures evaluated at the primary care center within 6 months after surgery, 1312 (47%) of whom had blood pressure measured at a preoperative evaluation within 30 days before surgery. Other outliers retained in the blood pressure analysis but removed from the relevant univariate linear regression models included 7 (0.25%) subjects with an aberrant heart rate entry and 12 (0.43%) subjects with an aberrant BMI entry. Data on marital status were unavailable for 3 (0.11%) subjects. A single self-identified race was unavailable for 238 (8.5%) subjects. A summary flow diagram of the database formation is illustrated in Figure 1, and a summary of descriptive variables for the 2807 subjects analyzed is shown in Table 1.
Figure 1.
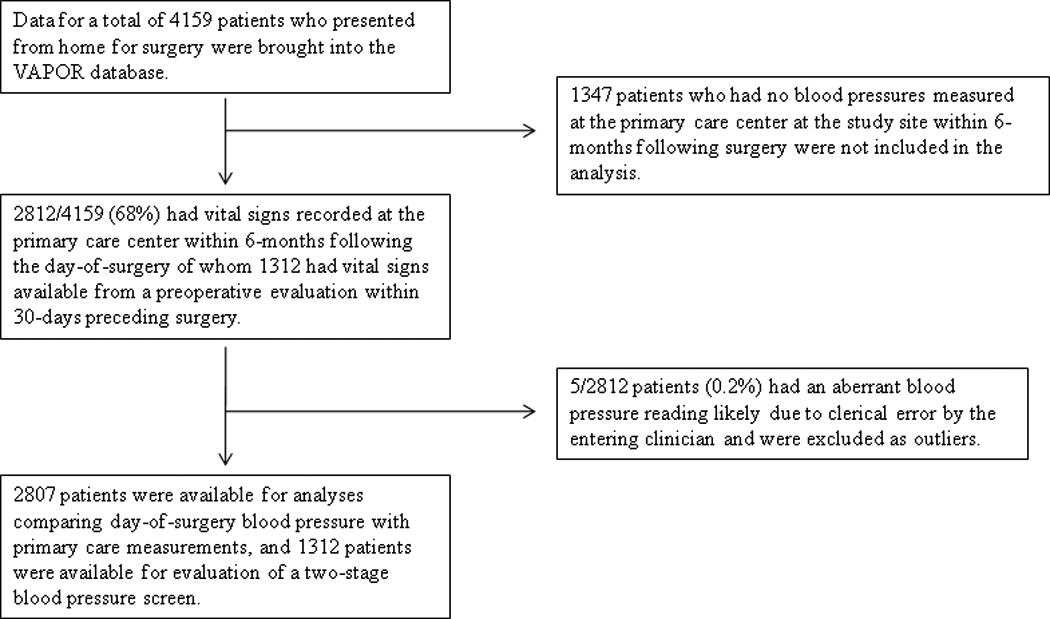
Flow Diagram of Patient Selection and Analysis
Table 1.
Overall Descriptive Characteristics of the Cohort
| Variable | Valid N | Mean (SDa) or Number positive (%) |
|
|---|---|---|---|
| DEMOGRAPHIC: | Age (years) | 2807 | 66.0 (13.7) |
| Female | 2807 | 134 (4.8%) | |
| African-American | 2569 | 328 (12.8%) | |
| Married | 2804 | 1150 (41.0%) | |
| Body-Mass Index (kg/m2) | 2795 | 29.2 (5.8) | |
| DAY OF SURGERY VITALS: | Systolic BPb (mmHg) | 2807 | 135.2 (18.3) |
| Diastolic BPb (mmHg) | 2807 | 75.2 (10.4) | |
| Heart Rate (beats/min) | 2803 | 71.7 (13.1) | |
| POSTOPERATIVE PRIMARY CARE VITALS: | Systolic BPb (mmHg) | 2807 | 129.7 (17.4) |
| Diastolic BPb (mmHg) | 2807 | 73.8 (12.0) | |
| Heart Rate (beats/min) | 2805 | 75.0 (14.3) | |
| SURGERY TYPE: | Cardiothoracic or Vascular Surgery | 2807 | 280 (10.0%) |
| COMORBID DIAGNOSIS: | Anxiety Disorder | 2807 | 556 (19.8%) |
| Atrial Fibrillation | 2807 | 337 (12.0%) | |
| Cerebrovascular Disease | 2807 | 448 (16.0%) | |
| Coronary Artery Disease | 2807 | 1063 (37.9%) | |
| Congestive Heart Failure | 2807 | 300 (10.7%) | |
| Diabetes | 2807 | 862 (30.7%) | |
| Hypertension | 2807 | 2224 (79.2%) | |
| Kidney Disease | 2807 | 210 (7.5%) | |
| Major Depression | 2807 | 591 (21.1%) | |
| Peripheral Vascular Disease | 2807 | 750 (26.7%) | |
| Posttraumatic Stress Disorder | 2807 | 470 (16.7%) | |
| Psychotic Disorder | 2807 | 502 (17.9%) | |
| Substance Abuse | 2807 | 676 (24.1%) | |
| ANTIHYPERTENSIVE DRUG CLASS: | Beta Blocker | 2807 | 826 (29.4%) |
| Calcium Channel Blocker | 2807 | 477 (17.0%) | |
| Anti-anginal | 2807 | 137 (4.9%) | |
| ACE-Inhibitor/ARBc | 2807 | 752 (26.8%) | |
| Loop Diuretic | 2807 | 232 (8.3%) | |
| Thiazide Diuretic | 2807 | 411 (14.6%) | |
| Combination pill | 2807 | 91 (3.2%) |
SD=Standard Deviation,
BP=Blood Pressure,
ACE=angiotensin converting enzyme, ARB=angiotensin II receptor blocker
The 2807 included subjects, demonstrated a mean (SD) DOS SBP of 135.2mmHg (18.3) and DBP of 75.2mmHg (10.4). The 1347 patients lost to follow-up demonstrated a mean (SD) DOS SBP of 134.3mmHg (17.3) and DBP of 76.3mmHg (10.1).
For the 2807 included subjects, scatter plots illustrated a highly significant linear relationship between the initial DOS blood pressure and subsequent primary care measurement with a large amount of variation present along the range of values (scatter plots available as Supplementary Figures 1 and 2 in supplemental digital content). Quantitatively, the Pearson’s correlation coefficient for SBP was 0.41 (95% CI 0.37 to 0.44), and for DBP it was 0.48 (95% CI 0.45 to 0.51). Bland-Altman plots of the difference between paired values (bias) plotted against their mean demonstrated a mean bias of +5.5mmHg for DOS SBP above primary care SBP with 95% limits of agreement of +43.7 mmHg to −32.8mmHg (Figure 2). For DBP, DOS measurement demonstrated a mean bias of +1.5mmHg above primary care DBP with 95% limits of agreement of +13.0 mmHg to −10.0 mmHg (Figure 3).
Figure 2.
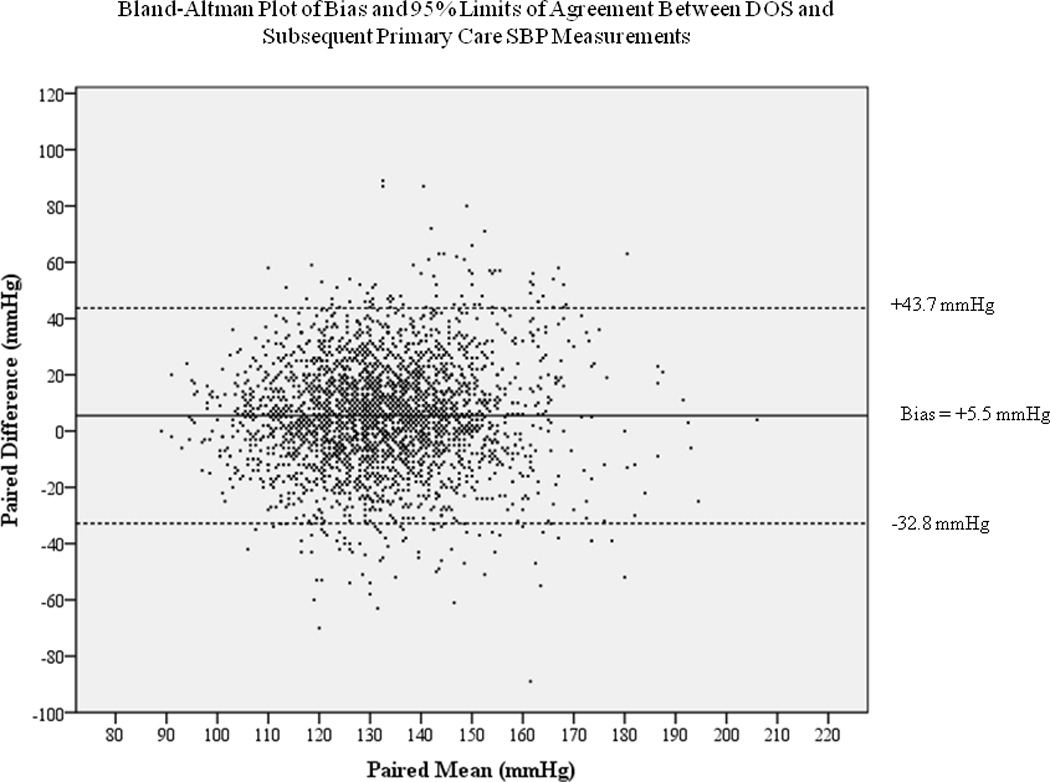
Bland-Altman plot demonstrating the mean bias (solid line) and 95% limits of agreement (dotted lines) of systolic blood pressure measurements on the day of surgery compared with those measured at a subsequent primary care visit. Positive bias represents a higher day of surgery reading. The 95% limits of agreement represent 1.96 times the standard deviation of the bias.
Figure 3.
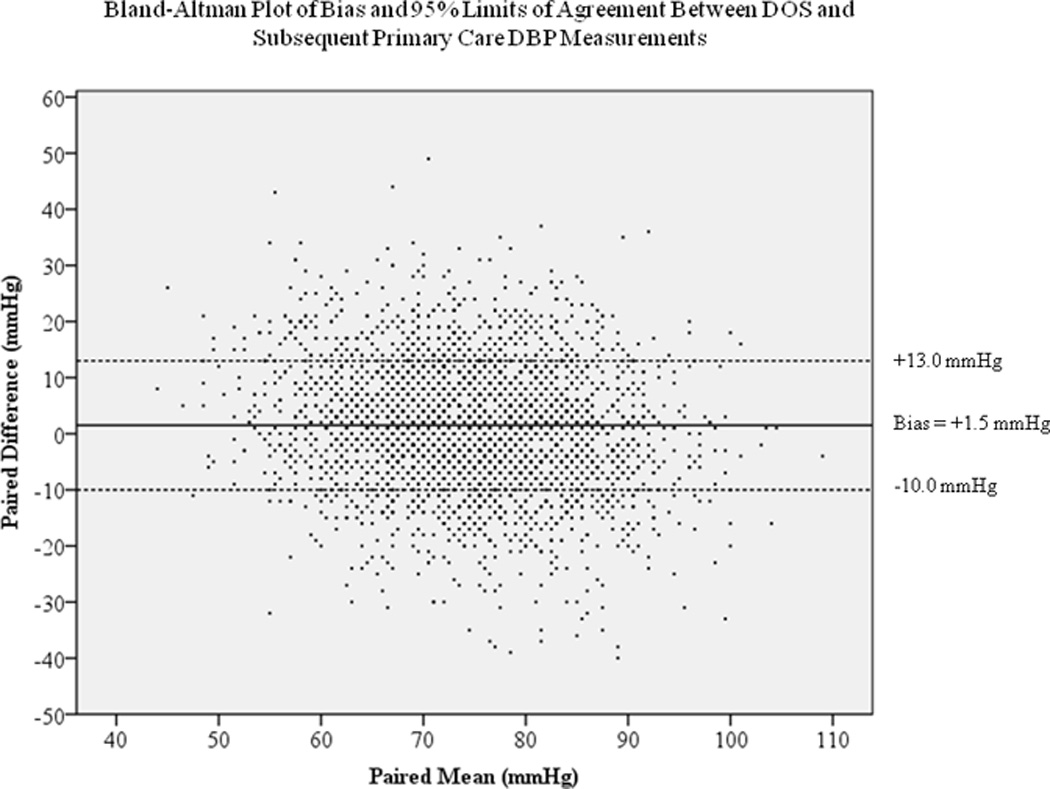
Bland-Altman plot demonstrating the mean bias (solid line) and 95% limits of agreement (dotted lines) of diastolic blood pressure measurements on the day of surgery compared with those measured at a subsequent primary care visit. Positive bias represents a higher day of surgery reading. The 95% limits of agreement represent 1.96 times the standard deviation of the bias.
Univariate linear regression results of DOS variables available in the dataset are shown in Table 2. For primary care SBP as the dependent variable, 25 DOS factors demonstrated univariate linear associations surpassing the p≤0.2 threshold. High collinearity was observed between atrial fibrillation and the heart rate × atrial fibrillation interaction term. After determining that the interaction term was insignificant in an alternative model, it was dropped from the final model, leaving the remaining 24 variables to be included in the multiple linear regression. The final SBP model demonstrated six variables with a statistically significant association with primary care SBP at the p≤0.05 level (Table 3). For primary care DBP as the dependent variable, 29 DOS parameters met the p≤0.2 threshold (Table 2). As with the SBP model, the heart rate × atrial fibrillation interaction term was again dropped from the final primary care DBP model because of both its collinearity with atrial fibrillation and its insignificance when included in an alternative model. The final DBP model demonstrated nine variables that retained significant associations with primary care DBP at the p≤0.05 level (Table 4). The overall R2 for the SBP model was 0.19 and for the DBP model was 0.29, leaving a large percentage of the variation in both subsequent SBP and DBP unexplained by the DOS variables in our models.
Table 2.
| Primary Care SBP as Dependent Variable |
Primary Care DBP as Dependent Variable |
|||||||
|---|---|---|---|---|---|---|---|---|
| Independent Variable | Beta | 95% CI of Beta |
Entered in Multivariable Model |
Beta | 95% CI of Beta |
P- value |
Entered in Multivariable Model |
|
| Age | 0.13 | 0.08, 0.18 | <0.001 | * | −0.25 | −0.29, −0.22 | <0.001 | * |
| Male gender | 4.79 | 1.78, 7.81 | 0.002 | * | 0.97 | −1.10, 3.05 | 0.36 | |
| African-American | 2.34 | 0.31, 4.36 | 0.02 | * | 3.87 | 2.49, 5.25 | <0.001 | * |
| Married | 1.14 | −0.17, 2.45 | 0.09 | * | −0.68 | −1.58, 0.22 | 0.14 | * |
| BMId | 0.28 | 0.17, 0.39 | <0.001 | * | 0.17 | 0.09, 0.24 | <0.001 | * |
| Days to Primary Care Evaluation | 0 | −0.02, 0.01 | 0.56 | 0.01 | −0.002, 0.02 | 0.12 | * | |
| DOS Systolic BP | 0.39 | 0.35, 0.42 | <0.001 | * | 0.09 | 0.07, 0.12 | <0.001 | * |
| DOS Diastolic BP | 0.32 | 0.26, 0.38 | <0.001 | * | 0.55 | 0.51, 0.59 | <0.001 | * |
| DOS Heart Rate | −0.01 | −0.06, 0.04 | 0.65 | 0.20 | 0.17, 0.23 | <0.001 | * | |
| Hour of Day of DOS BP | 0.24 | −0.02, 0.50 | 0.07 | * | 0.13 | −0.05, 0.31 | 0.16 | * |
| Cardiothoracic or Vascular Surgery | −1.48 | −3.63, 0.67 | 0.18 | * | −4.03 | −5.50, −2.56 | <0.001 | * |
| Anxiety Disorder | −2.05 | −3.66, −0.43 | 0.01 | * | 1.76 | 0.65, 2.87 | 0.002 | * |
| Atrial Fibrillation | −2.11 | −4.09, −0.13 | 0.04 | * | −3.86 | −5.21, −2.50 | <0.001 | * |
| Atrial Fibrillation X Heart Rate | −0.03 | −0.06, −0.001 | 0.04 | * | −0.05 | −0.07, −0.03 | <0.001 | * |
| Cerebrovascular Disease | 0.19 | −1.57, 1.95 | 0.83 | −4.97 | −6.17, −3.77 | <0.001 | * | |
| Congestive Heart Failure | −3.27 | −5.35, −1.18 | 0.002 | * | −5.74 | −7.15, −4.32 | <0.001 | * |
| Coronary Artery Disease | −1.33 | −2.66, −0.004 | 0.05 | * | −5.23 | −6.12, −4.33 | <0.001 | * |
| Diabetes | 2.91 | 1.51, 4.30 | <0.001 | * | −3.22 | −4.17, −2.26 | <0.001 | * |
| Hypertension | 7.57 | 6.01, 9.14 | <0.001 | * | −1.41 | −2.50, −0.32 | 0.01 | * |
| Kidney Disease | −0.54 | −2.99, 1.91 | 0.67 | −5.69 | −7.36, −4.02 | <0.001 | * | |
| Major Depression | −3.6 | −5.18, −2.03 | <0.001 | * | 1.41 | 0.32, 2.49 | 0.01 | * |
| Peripheral Vascular Disease | −0.32 | −1.77, 1.14 | 0.67 | −4.87 | −5.85, −3.89 | <0.001 | * | |
| Posttraumatic Stress Disorder | −3.8 | −5.52, −2.08 | <0.001 | * | 2.02 | 0.83, 3.20 | 0.001 | * |
| Psychotic Disorder | −3.03 | −4.70, −1.35 | <0.001 | * | 0.70 | −0.45, 1.86 | 0.23 | |
| Substance Abuse | −1.8 | −3.83, −0.23 | 0.08 | * | 4.08 | 2.69, 5.47 | <0.001 | * |
| Beta Blocker | 0.93 | −0.49, 2.34 | 0.20 | * | −2.43 | −3.40, −1.47 | <0.001 | * |
| Calcium Channel Blocker | 5.20 | 3.49, 6.90 | <0.001 | * | −1.28 | −2.46, −0.10 | 0.03 | * |
| Anti-anginal | −2.36 | −5.35, 0.63 | 0.12 | * | −6.11 | −8.15, −4.07 | <0.001 | * |
| ACE-Inhibitor or ARBe | 2.5 | 1.05, 3.95 | 0.001 | * | −2.12 | −3.12, −1.12 | <0.001 | * |
| Loop Diuretic | −0.46 | −2.80, 1.88 | 0.70 | −5.44 | −7.03, −3.84 | <0.001 | * | |
| Thiazide Diuretic | 5.45 | 3.64, 7.26 | <0.001 | * | 0.97 | −0.29, 2.22 | 0.13 | * |
| Combination pill | 0.47 | −3.17, 4.10 | 0.8 | 0.36 | −2.14, 2.86 | 0.78 | ||
DOS=day of surgery,
SBP=systolic blood pressure,
DBP=diastolic blood pressure,
BMI=Body-Mass Index,
ACE=angiotensin converting enzyme, ARB=angiotensin II receptor blocker.
Table 3.
Multiple Linear Regression Model of DOSa Parameters Associated with Primary Care Systolic Blood Pressure
| Primary Care SBPb as Dependent Variable (R2=0.19) | |||
|---|---|---|---|
| Independent Variable | Beta | 95% CI of Beta | P-value |
| Age | 0.02 | −0.04, 0.08 | 0.50 |
| Male gender | 0.57 | −2.43, 3.57 | 0.71 |
| African-American | 0.47 | −1.44, 2.37 | 0.63 |
| Married | 0.29 | −0.99, 1.56 | 0.66 |
| BMIc | 0.22 | 0.11, 0.33 | <0.001 |
| DOS SBP | 0.35 | 0.31, 0.39 | <0.001 |
| DOS DBPd | 0.01 | −0.07, 0.08 | 0.87 |
| Hour of Day of DOS Measurement | 0.21 | −0.04, 0.46 | 0.11 |
| Cardiothoracic or Vascular Surgery | −1.35 | −3.45, 0.76 | 0.21 |
| Anxiety | 0.28 | −1.42, 1.97 | 0.75 |
| Atrial Fibrillation | −0.46 | −2.50, 1.59 | 0.66 |
| Congestive Heart Failure | −3.74 | −5.94, −1.54 | 0.001 |
| Coronary Artery Disease | −1.58 | −3.08, −0.07 | 0.04 |
| Diabetes | 1.02 | −0.43, 2.47 | 0.17 |
| Hypertension | 3.24 | 1.42, 5.06 | <0.001 |
| Major Depression | −1.49 | −3.29, 0.30 | 0.10 |
| Post Traumatic Stress Disorder | −1.37 | −3.25, 0.50 | 0.15 |
| Psychotic Disorder | −1.16 | −2.93, 0.61 | 0.20 |
| Substance Abuse | 1.84 | −0.29, 3.97 | 0.09 |
| Beta Blocker | 0.20 | −1.27, 1.66 | 0.79 |
| Calcium Channel Blocker | 1.49 | −0.21, 3.19 | 0.09 |
| Anti-anginal | −1.74 | −4.69, 1.22 | 0.25 |
| ACE Inhibitor or ARBe | −0.43 | −1.95, 1.09 | 0.58 |
| Thiazide Diuretic | 2.37 | 0.54, 4.21 | 0.01 |
DOS=day of surgery,
SBP=systolic blood pressure,
BMI= body mass index,
DBP=diastolic blood pressure,
ACE=angiotensin converting enzyme, ARB=angiotensin II receptor blocker.
Table 4.
Multiple Linear Regression Model of DOSa Parameters Associated with Primary Care Diastolic Blood Pressure
| Primary Care DBPb as Dependent Variable (R2=0.29) | |||
|---|---|---|---|
| Independent Variable | Beta | 95% CI of Beta | P-value |
| Age | −0.14 | −0.18, −0.10 | <0.001 |
| African-American | 1.07 | −0.16, 2.30 | 0.09 |
| Married | 0.55 | −0.27, 1.37 | 0.19 |
| BMIc | 0.08 | 0.01, 0.15 | 0.04 |
| Days to Primary Care Evaluation | 0.003 | −0.01, 0.01 | 0.42 |
| DOS SBPd | −0.001 | −0.03, 0.03 | 0.950 |
| DOS DBP | 0.45 | 0.40, 0.50 | <0.001 |
| DOS Heart Rate | 0.07 | 0.04, 0.10 | <0.001 |
| Hour of DOS Measurement | 0.10 | 0.26, 0.96 | 0.23 |
| Cardiothoracic or Vascular Surgery | −1.32 | −2.68, 0.04 | 0.06 |
| Anxiety | 0.66 | −0.42, 1.74 | 0.23 |
| Atrial Fibrillation | 0.90 | −0.41, 2.22 | 0.18 |
| Cerebrovascular Disease | −1.85 | −2.98, −0.71 | 0.001 |
| Congestive Heart Failure | −1.02 | −2.49, 0.45 | 0.17 |
| Coronary Artery Disease | −0.92 | −1.90, 0.07 | 0.07 |
| Diabetes | −0.98 | −1.93, −0.04 | 0.04 |
| Hypertension | 0.05 | −0.75, 0.85 | 0.90 |
| Kidney Disease | −2.15 | −3.71, −0.59 | 0.01 |
| Major Depression | −0.55 | −1.67, 0.57 | 0.33 |
| Peripheral Vasular Disease | −0.53 | −1.53, 0.46 | 0.29 |
| Post Traumatic Stress Disorder | −0.43 | −1.62. 0.77 | 0.48 |
| Substance Abuse | 1.39 | 0.05, 2.74 | 0.04 |
| Beta Blocker | −0.23 | −1.18. 0.72 | 0.63 |
| Calcium Channel Blocker | −0.11 | −1.21, 0.98 | 0.84 |
| Anti-anginal | −1.28 | −3.18, 0.63 | 0.19 |
| ACE Inhibitor or ARBe | −1.11 | −2.09, −0.13 | 0.03 |
| Loop Diuretic | −0.23 | −1.82, 1.36 | 0.78 |
| Thiazide Diuretic | 0.78 | −0.40, 1.96 | 0.19 |
DOS=day of surgery,
DBP=diastolic blood pressure,
BMI= body mass index,
SBP=systolic blood pressure,
ACE=angiotensin converting enzyme, ARB=angiotensin II receptor blocker.
The regression results demonstrated that a prior diagnosis of congestive heart failure or coronary artery disease was independently associated with a lower primary care SBP when controlling for other DOS variables. The prior diagnosis of hypertension, thiazide diuretics, and increasing BMI were independently associated with higher primary care blood pressure when controlling for other DOS variables.
For analysis of the sensitivity, specificity, and positive and negative predictive value for different referral thresholds, 753 of 2807 patients seen postoperatively in primary care were classified as having elevated primary care SBP (SBP ≥ 140mmHg), and 276 were classified as having elevated primary care DBP (DBP ≥ 90mmHg). Table 5 reports the results using both the simple screen (based on a single DOS blood pressure reading) as well as a two-stage screen (based on a combined evaluation of preoperative and DOS measurements). A two-stage screen using a preoperative SBP ≥ 140mmHg combined with a DOS SBP ≥ 146mmHg would have resulted in a blood pressure referral rate of just under 10% of the cohort with an estimated sensitivity of 26.8% (95% CI 22.0 to 32.0) and an estimated specificity of 95.9% (95% CI 94.4 to 97.0). The estimated positive and negative predictive values of this two-stage screen were 67.7% (95% CI 58.9 to 75.7) and 80.2% (95% CI 77.8 to 82.4), respectively.
Table 5.
Prognostic Value of Single and Two-Stage Perioperative Blood Pressure Screens
| Single Blood Pressure Screen for Predicting Elevated Primary Care Blood Pressure | ||||||
|---|---|---|---|---|---|---|
| Referral Threshold (mmHg) |
Incidence of Referral (%) |
Sensitivity (95% CI) |
Specificity (95% CI) |
Positive Predictive Value (95% CI) |
Negative Predicitive Value (95% CI) |
|
| Systolic Blood Pressure Screen | DOS SBPa ≥ 140 | 1119/2807 (39.9%) | 62.5% (59.0, 66.0) | 68.5% (66.3, 70.5) | 42.1% (39.2, 45.1) | 83.3% (81.4, 85.0) |
| DOS SBP ≥ 146 | 766/2807 (27.3%) | 48.6% (45.0, 52.2) | 80.5% (78.8, 82.2) | 47.8% (44.2, 51.4) | 81.0% (79.3, 82.7) | |
| Diastolic Blood Pressure Screen | DOS DBPb ≥ 90 | 236/2807 (8.4%) | 25% (20.0, 30.5) | 93.4% (92.4, 94.3) | 29.2% (23.5, 35.5) | 91.9% (90.8, 93.0) |
| DOS DBP ≥ 92 | 162/2807 (5.8%) | 18.8% (14.4, 24.0) | 95.7% (94.8, 96.4) | 32.1% (25.0, 39.9) | 91.5% (90.4, 92.6) | |
| Two-Stage Blood Pressure Screen for Predicting Elevated Primary Care Blood Pressure | ||||||
| Systolic Blood Pressure Screen | Preoperative SBP ≥ 140 and DOS SBP ≥ 140 | 180/1312 (13.7%) | 32.7% (27.6, 38.1) | 92.4% (90.6, 94.0) | 58.3% (50.8, 65.6) | 80.9% (78.5, 83.2) |
| Preoperative SBP ≥ 140 and DOS SBP ≥ 146 | 127/1312 (9.7%) | 26.8% (22.0, 32.0) | 95.9% (94.4, 97.0) | 67.7% (58.9, 75.7) | 80.2% (77.8, 82.4) | |
| Diastolic Blood Pressure Screen | Preoperative DBP ≥ 90 and DOS DBP ≥ 90 | 31/1312 (2.4%) | 10.2% (5.4, 17.1) | 98.4% (97.5, 99.0) | 38.7% (21.9, 57.8) | 91.7% (90.1, 93.2) |
| Preoperative DBP ≥ 90 and DOS DBP ≥ 92 | 19/1312 (1.4%) | 8.5% (4.1, 15.0) | 99.2% (98.6, 99.7) | 52.6% (28.9, 75.6) | 91.6% (90.0, 93.1) | |
DOS=Day of Surgery; SBP=Systolic Blood Pressure;
DBP=Diastolic Blood Pressure
For DBP screening, a single DOS referral threshold DBP≥92mmHg would have led to a 5.8% referral rate with an estimated sensitivity of 18.8% (95% CI 14.4 to 24.0), an estimated specificity of 95.7% (95% CI 94.8 to 96.4), and estimated positive and negative predictive value of 32.1% (95% CI 25.0 to 39.9) and 91.5% (95% CI 90.4 to 92.6), respectively. Incorporation of a two-stage screen using preoperative DBP≥90mmHg and a DOS DBP≥92mmHg decreased estimated sensitivity to 8.5% (95% CI 4.1 to 15.0) with an estimated specificity of 99.2% (95% CI 98.6 to 99.7) and an increase in estimated positive and negative predictive value to 52.6% (95% CI 28.9 to 75.6) and 91.6% (95% CI 90.0 to 93.1), respectively.
After analysis of the above thresholds was performed, we conducted a post hoc analysis to identify what DOS SBP threshold would have been necessary to approximate a similar estimated specificity (>95%) to that approached by the more stringent two-stage SBP screen. Our analysis revealed that if a single DOS threshold were used without reference to other preoperative clinic measurements, an intake DOS SBP≥160mmHg achieved an estimated sensitivity and specificity of 16.5% (95% CI 13.9 to 19.3) and 95.2% (95% CI 94.2 to 96.1), with estimated positive and negative predictive values of 55.6% (95% CI 48.8 to 62.2) and 75.7% (95% CI 74.0 to 77.3), respectively.
Conclusions
The present analysis sought to examine the relationship between DOS and primary care blood pressure and to assess the evidence for anesthesiologist-initiated perioperative blood pressure referral. The mean bias in DOS SBP of +5.5mmHg may be lower than what is conventionally assumed, and the mean bias in DBP of +1.5mmHg is clinically trivial, perhaps even within the error of measurement of many blood pressure cuffs. Beyond these mean values, however, there was wide variability in blood pressures that remained unexplained in the multiple linear regression results.
In the analysis of potential blood pressure referral thresholds, we demonstrate that a single DOS SBP measurement performs modestly in discriminating patients with elevated primary care blood pressure in the 6 months after surgery. Consistent with this finding, the hypertension literature has recognized the need to avoid overdependence on a single reading to guide diagnosis or treatment of hypertension.9 With the implementation of a two-stage screen, however, we were able to demonstrate a procedure with more useful prognostic value. While insensitive, screening using a preoperative SBP ≥ 140mmHg combined with a DOS SBP ≥ 146mmHg (incorporating the observed DOS bias) would have resulted in an estimated specificity of 95.9% (95% CI 94.4 to 97.0) with a sensitivity of 26.8% (95% CI 22.0 to 32.0). More than two-thirds of patients who met this two-stage threshold were subsequently found to have elevated SBP at their primary care appointment while four of five patients not meeting the screening threshold were found not to have elevated primary care SBP. Because of the low sensitivity of this screen, many patients with elevated primary care SBP would have been missed by such a referral threshold, but the high estimated specificity and reasonable estimated positive predictive value offer support to anesthesiologists who are inclined to make primary care blood pressure referrals based on a two-stage preoperative blood pressure screen.
In the absence of a recent preoperative measurement and basing referral decisions on a single presenting DOS SBP measurement, we found that a threshold SBP ≥ 160mmHg achieved a similar estimated specificity to the two-stage screen. Estimated specificity was 95.2% (95% CI 94.2 to 96.1) but the estimated sensitivity was decreased to 16.5% (95% CI 13.9 to 19.3). Using a single-measurement DOS SBP ≥ 160mmHg screen in our dataset, more than half of referred patients indeed would have demonstrated elevated primary care SBP, and more than three of four patients not referred would have demonstrated normal primary care SBP. While a more reliable test would of course be desirable, the relatively benign nature of the proposed intervention may lead some clinicians to rely on a single-measurement threshold where preoperative numbers are not readily available. The decision to refer a patient to primary care based on such a measurement will no doubt depend on clinician and patient preferences as well as on the ease and expense of primary care referral within the particular health care system considered.
For DBP, the single reading and two stage referral thresholds all demonstrated high estimated specificity (93%–99%) with relatively low estimated sensitivity (25.0%–8.5%) across the different referral thresholds examined. Because elevated primary care DBP was relatively uncommon in our cohort, only a two-stage DBP screen incorporating the DOS bias reached an estimated positive predictive value of more than 50%. While all of our DBP thresholds were relatively insensitive, the high estimated specificity would offer support to anesthesiologists who favor primary care blood pressure referral based on elevated preoperative DBP measurements, particularly in populations with a relatively high prevalence of diastolic hypertension.
It should be emphasized that our study uses DOS blood pressures taken in the preoperative admitting area, generally by a nurse or nurse’s assistant. The bias toward higher blood pressure may be greater inside the operating room or when the blood pressure is taken by a physician. Given the heterogeneity of surgical procedures and anesthetic techniques, it also remains to be seen whether similar thresholds can be identified using hemodynamics from the operating room itself. The screening thresholds used in this study have the advantage of occurring before the introduction of the confounding factors that are encountered intraoperatively.
Several limitations to the present study should be noted. We did not track medication changes, medication adherence, or intervening visits to primary care doctors that occurred outside the VA system. It is possible that incorporating more detailed medication information or information from providers outside the VA system could further enhance the predictive value of DOS measurements. The lack of significance of the time between surgery and the follow-up primary care measurement in both multiple regression models suggests that unobserved doctor’s visits or medication changes were unlikely to have significantly changed the predictive ability of our DOS measurements.
Although the number of patients in our study was large, interpreting our findings to other groups of patients should be done cautiously. For example, generalizing our results to patients with absent or remote primary care relationships, to younger patients, or to female patients may be premature without studies specifically focused on such populations. Our retrospective approach to the study population necessitated that the members of the cohort had primary care data available for analysis. As could be expected, such patients tended to be older with more comorbidities than patients who lacked primary care data. Further studies may shed light on how DOS blood pressure measurements perform in populations with different comorbidity profiles. It is also of interest whether our findings may be generalized to other countries’ health care systems in which the fragmentation of primary care may be less pervasive.
In addition, future research is needed to clarify whether anesthesiologist-initiated referral improves long-term blood pressure control. Literature on smoking cessation has demonstrated that with a long-standing and modifiable health risk factor like tobacco use, additional brief interventions by health care providers including during the perioperative period, may be of benefit.10–14 However, it is possible that patients with difficult-to-control blood pressures or with poor medication compliance, even if correctly identified, would receive no benefit from primary care referral. Recent data from the anesthesiology literature may offer modest encouragement in this regard. In a large retrospective study, Wax et al. observed that patients who undergo case cancellations due to severe preoperative hypertension return for future surgery with significantly lower, albeit not normal, blood pressure.3 Evidence from the hypertension literature has shown that among hypertensive people, incremental decreases in SBP or DBP correspond to significant reductions in the risk of coronary heart disease and stroke even in the absence of complete blood pressure normalization.15 Still, Wax et al. made their observation only in relation to severely hypertensive patients, and their observation may have been enhanced by a regression-toward-the-mean phenomenon. Whether significantly lower blood pressures will result from primary care referral among the much more commonly seen population of patients with mild to moderate preoperative hypertension remains to be seen in future studies.
Additionally, the potential impact may be greater in patients who lack close primary care follow-up. In such patients without primary care follow-up, our own data demonstrate the potentially large public health impact. Revisiting the blood pressure data for the 1347 patients who were not seen within 6 months after surgery in the primary care center, we found that 92 (6.8%) had DOS SBP≥160mmHg. If referral were shown to be useful only in patients who lacked close primary care follow-up, the potential impact on public health and on long-term postoperative outcomes could still be significant.
In conclusion, our data demonstrate a small upward bias with wide variation in DOS intake blood pressure as compared to subsequent primary care measurements. The initial DOS SBP measurement, particularly when combined with a recent preoperative measurement, is insensitive but reasonably specific for predicting primary care hypertension. The initial DOS DBP measurement, after accounting for the small DOS bias, is also insensitive but reasonably specific for subsequently elevated primary care DBP. The summative message of the sensitivity and specificity data in this study is that while it is difficult to exclude high primary care blood pressure based on normal preoperative values, there are clinically plausible perioperative thresholds that when exceeded, provide a reasonable basis for initiating primary care blood pressure referral. Accordingly, our study provides evidence to support DOS intake blood pressure screening and thus adds to the growing body of literature suggesting a potential role of anesthesiologists as perioperative physicians who have the opportunity to make long-term improvements in patients’ health.
Supplementary Material
Scatter plot illustrating the linear relationship between systolic blood pressures from the day of surgery and subsequent primary care visits. SBP=systolic blood pressure. Pearson’s R = 0.41. The best fit line with 95% confidence bands is displayed.
Scatter plot illustrating the linear relationship between diastolic blood pressures from the day of surgery and subsequent primary care visits. DBP=diastolic blood pressure. Pearson’s R = 0.48. The best fit line with 95% confidence bands is displayed.
Acknowledgements
The authors wish to thank Dr. Fredrick K. Orkin, MD, MBA, SM; Adjunct Professor, Department of Anesthesiology, Yale University School of Medicine, New Haven, CT for his input on the manuscript; and the assistance with database management of Mr. Woody Levin, MS; Informatics Consultant at the VA Connecticut Healthcare System, West Haven, CT.
Funding: National Institutes of Health (NIH) T-32 Research Training Grant: T32 GM086287,
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Department of Veterans Affairs Attribution and Disclaimer
This material is based upon work supported in part by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
The authors declare no conflicts of interest.
DISCLOSURES:
Name: Robert B. Schonberger, MD, MA
Contribution: This author helped design the study, conduct the study, analyze the data, and write the manuscript.
Attestation: Robert B. Schonberger has seen the original study data, reviewed the analysis of the data, approved the final manuscript, and is the author responsible for archiving the study files.
Name: Matthew M. Burg, PhD
Contribution: This author helped design the study, conduct the study, analyze the data, and write the manuscript.
Attestation: Matthew M. Burg has seen the original study data, reviewed the analysis of the data, and approved the final manuscript.
Name: Natalie Holt, MD, MPH
Contribution: This author helped design the study, conduct the study, analyze the data, and write the manuscript.
Attestation: Natalie Holt has seen the original study data, reviewed the analysis of the data, and approved the final manuscript.
Name: Carrie L. Lukens, PhD
Contribution: This author helped conduct the study, analyze the data, and write the manuscript.
Attestation: Carrie L. Lukens has seen the original study data, reviewed the analysis of the data, and approved the final manuscript.
Name: Feng Dai, PhD
Contribution: This author helped design the study, conduct the study, analyze the data, and write the manuscript.
Attestation: Feng Dai has seen the original study data, reviewed the analysis of the data, and approved the final manuscript.
Name: Cynthia Brandt, MD, MPH
Contribution: This author helped design the study, conduct the study, analyze the data, and write the manuscript.
Attestation: Cynthia Brandt has seen the original study data, reviewed the analysis of the data, and approved the final manuscript.
This manuscript was handled by: Franklin Dexter, MD, PhD
Contributor Information
Robert B. Schonberger, Department of Anesthesiology, Yale University School of Medicine, New Haven, CT.
Matthew M. Burg, Department of Veterans Affairs Medical Center, West Haven, CT (current affiliation: Department of Veterans Affairs Medical Center, West Haven, CT; Department of Internal Medicine, Yale University School of Medicine, New Haven, CT; Columbia University College of Physicians and Surgeons, New York, NY).
Natalie Holt, Anesthesiology Service, Department of Veterans Affairs Medical Center, West Haven, CT; Department of Anesthesiology, Yale University School of Medicine, New Haven, CT.
Carrie L. Lukens, Department of Veterans Affairs Medical Center, West Haven, CT.
Feng Dai, Yale Center for Analytical Sciences, Yale University School of Public Health, West Haven, CT.
Cynthia Brandt, Department of Veterans Affairs Medical Center, West Haven, CT; Department of Anesthesiology, Yale University School of Medicine, New Haven, CT.
References
- 1.Fleisher LA, Beckman JA, Brown KA, Calkins H, Chaikof EL, Fleischmann KE, Freeman WK, Froehlich JB, Kasper EK, Kersten JR, Riegel B, Robb JF. 2009 ACCF/AHA focused update on perioperative beta blockade incorporated into the ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: a report of the American college of cardiology foundation/American heart association task force on practice guidelines. Circulation. 2009;120:e169–e276. doi: 10.1161/CIRCULATIONAHA.109.192690. [DOI] [PubMed] [Google Scholar]
- 2.Grimm RH, Jr, Cohen JD, Smith WM, Falvo-Gerard L, Neaton JD. Hypertension management in the Multiple Risk Factor Intervention Trial (MRFIT). Six-year intervention results for men in special intervention and usual care groups. Arch Intern Med. 1985;145:1191–1199. [PubMed] [Google Scholar]
- 3.Wax DB, Porter SB, Lin H-M, Hossain S, Reich DL. Association of preanesthesia hypertension with adverse outcomes. J Cardiothorac Vasc Anesth. 2010;24:927–930. doi: 10.1053/j.jvca.2010.06.022. [DOI] [PubMed] [Google Scholar]
- 4.Goulet JL, Fultz SL, McGinnis KA, Justice AC. Relative prevalence of comorbidities and treatment contraindications in HIV-mono-infected and HIV/HCV-co-infected veterans. AIDS. 2005;19 Suppl 3:S99–S105. doi: 10.1097/01.aids.0000192077.11067.e5. [DOI] [PubMed] [Google Scholar]
- 5.Goulet JL, Fultz SL, Rimland D, Butt A, Gibert C, Rodriguez-Barradas M, Bryant K, Justice AC. Aging and infectious diseases: do patterns of comorbidity vary by HIV status, age, HIV severity? Clin Infect Dis. 2007;45:1593–1601. doi: 10.1086/523577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Justice AC, Lasky E, McGinnis KA, Skanderson M, Conigliaro J, Fultz SL, Crothers K, Rabeneck L, Rodriguez-Barradas M, Weissman SB, Bryant K, Team VP. Medical disease and alcohol use among veterans with human immunodeficiency infection: A comparison of disease measurement strategies. Med Care. 2006;44:S52–S60. doi: 10.1097/01.mlr.0000228003.08925.8c. [DOI] [PubMed] [Google Scholar]
- 7.Veterans Aging Cohort Study homepage. [Accessed April 28, 2011]; Available at: http://medicine.yale.edu/intmed/vacs/index.aspx.
- 8.Lenfant C, Chobanian AV, Jones DW, Roccella EJ. Joint National Committee on the Prevention DEaToHBP. Seventh report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7): resetting the hypertension sails. Hypertension. 2003;41:1178–1179. doi: 10.1161/01.HYP.0000075790.33892.AE. [DOI] [PubMed] [Google Scholar]
- 9.Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ. Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure R. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension. 2005;45:142–161. doi: 10.1161/01.HYP.0000150859.47929.8e. [DOI] [PubMed] [Google Scholar]
- 10.Gordon JS, Andrews JA, Albert DA, Crews KM, Payne TJ, Severson HH. Tobacco cessation via public dental clinics: results of a randomized trial. Am J Public Health. 100:1307–1312. doi: 10.2105/AJPH.2009.181214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thomsen T, Villebro N, Moller AM. Interventions for preoperative smoking cessation. Cochrane Database Syst Rev. 2010;7 doi: 10.1002/14651858.CD002294.pub3. CD002294. [DOI] [PubMed] [Google Scholar]
- 12.Warner DO. American Society of Anesthesiologists Smoking Cessation Initiative Task F. Feasibility of tobacco interventions in anesthesiology practices: a pilot study. Anesthesiology. 2009;110:1223–1228. doi: 10.1097/ALN.0b013e3181a5d03e. [DOI] [PubMed] [Google Scholar]
- 13.Warner DO, Klesges RC, Dale LC, Offord KP, Schroeder DR, Shi Y, Vickers KS, Danielson DR. Clinician-delivered Intervention to Facilitate Tobacco Quitline Use by Surgical Patients. Anesthesiology. 2011;114 doi: 10.1097/ALN.0b013e31820d868d. [DOI] [PubMed] [Google Scholar]
- 14.Warner DO, Klesges RC, Dale LC, Offord KP, Schroeder DR, Vickers KS, Hathaway JC. Telephone quitlines to help surgical patients quit smoking patient and provider attitudes. Am J Prev Med. 2008;35 Supp:S486–S493. doi: 10.1016/j.amepre.2008.08.032. [DOI] [PubMed] [Google Scholar]
- 15.Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. doi: 10.1136/bmj.b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Scatter plot illustrating the linear relationship between systolic blood pressures from the day of surgery and subsequent primary care visits. SBP=systolic blood pressure. Pearson’s R = 0.41. The best fit line with 95% confidence bands is displayed.
Scatter plot illustrating the linear relationship between diastolic blood pressures from the day of surgery and subsequent primary care visits. DBP=diastolic blood pressure. Pearson’s R = 0.48. The best fit line with 95% confidence bands is displayed.


