Abstract
Background
extended spectrum β-lactamase (ESBL) producing gram negative bacilli are becoming a growing problem worldwide with difficulties in designing a national formulary for empirical treatment of gram negative sepsis.
Objectives
In this study, we investigated the in vitro activity of Carbapenems, Pipracillin-Tazobactam, Ciprofloxacin alone or in combination with aminoglycosides against ESBL-producing strains isolated from clinical samples.
Methods
Three hundred and one ESBL-producing Escherichia coli and K. pneumoniae strains isolated from clinical samples were investigated. Isolates were screened initially for ESBL production using an automated system. All ESBL isolates were further confirmed using the double-disk diffusion method.
Results
The overall Piperacillin-Tazobactam susceptibility was 57.9 (64.4% E. coli and 43.6% Klebsiella pneumoniae). Only 29.6% of ESBLs (24.9% E. coli and 39.6% Klebsiella pneumoniae) were ciprofloxacin susceptible. 98.1% E. coli and 93.1% of Klebsiella pneumoniae were susceptible to Piperacillin-Tazobactam plus Amikacin combination. 73.7% E. coli and 61.4% of Klebsiella pneumoniae were susceptible to Piperacillin-Tazobactam plus Gentamicin combination. 96.7% E. coli and 91.1% of Klebsiella pneumoniae were susceptible to Ciprofloxacin plus Amikacin combination. 41.2% E. coli and 51.5% of Klebsiella pneumoniae were susceptible to Ciprofloxacin plus Gentamicin combination.
Conclusion
ESBLs have high resistance profile against Piperacillin/Tazobactam and Ciprofloxacin. The ESBLs from Oman have similar resistantce pattern as those reported from UK and USA. This resistance decreases when these drugs are combined with Amikacin. All ESBLs are susceptible to Carbapenems. However, carbepenam overuse can lead to emergence of carbapenems resistant gram negative bacilli and ESBLs. Combination of Amikacin plus Piperacillin/Tazobactam is a feasible empirical therapy for ESBLs
Keywords: extended spectrum β-lactamases (ESBLs), empirical therapy, combination therapy
Introduction
There is a worldwide increase in antimicrobial resistance where most of the most of Gram-negative pathogens are becoming resistant to first-line antibiotics.1 While there are many mechanisms for antimicrobial resistance among Gram-negative pathogens, the production of extended spectrum β-lactamases (ESBLs) is well documented.2 ESBLs were first recognized among Klebsiella pneumoniae and Serratia marcescens isolates in Germany in 1983 shortly after the introduction of extended spectrum cephalosporins, such as ceftazidime.2 By definition, ESBLs are molecular class A or D β-lactamases, which are able to hydrolyze oxyimino cephalosporins at a rate equal to or higher than 10% of that for benzylpenicillin, have an active-site serine, and generally are inhibited by β-lactamase inhibitors such as clavulanic acid, sulbactam, or tazobactam.3
Class A ESBLs belong to three types and these are SHV with more than 60 varieties recognized so far on the basis of unique combinations of amino acid replacements, TEM with more than 135 TEM enzymes currently known, and CTX-M with 40 CTX-M enzymes known so far.4 Other uncommon class A ESBLs are BES-1, GES-1, GES-2, IBC-1, IBC-2, PER-1, SFO-1, TLA-1, VEB-1 and VEB-2.5 There are at least 12 ESBLs belonging to the OXA type (class D).5 Infections caused by ESBLs pose serious challenges to clinicians; because they are resistant to a broad range of β-lactamases, including third-generation cephalosporins, nosocomial infections caused by these organisms complicate therapy and limit treatment options. Moreover, patients infected with ESBLs may have a higher mortality rate and may require longer hospitalization as they are generally sicker and receive more antibiotics than patients who are not infected with ESBL-producing strains.6
In this study, we investigated the in vitro activity of Carbapenems (Imipenem and Meropenem), Pipracillin-Tazobactam, Ciprofloxacin alone or in combination with aminoglycosides against ESBL-producing strains isolated from clinical samples.
Methods
We have investigated a total of 301 ESBL-producing Escherichia coli and K. pneumoniae strains isolated from clinical samples. These strains were collected over a period of two years from July 2005 to July 2007 from patients attending Sultan Qaboos University Hospital. Isolates were screened initially for ESBL production using an automated system "Phoenix Identification and Susceptibility System" (by Becton Dickinson, USA, Sparks, MD, USA). It relies on the growth response to selected expanded-spectrum cephalosporins. This test is composed of five wells, each containing a cephalosporin alone or in combination with clavulanic acid (cefpodoxime, ceftazidime, ceftazidime with clavulanic acid, cefotaxime with clavulanic acid and ceftriaxone with clavulanic acid). In this system, the results are also interpreted through a computerized system.7 All identified ESBL isolates were further confirmed using the Clinical and Laboratory Standards Institute (CLSI) approved double-disk diffusion method,8 which is based on a synergistic increase of inhibition zone of ceftazidime and cefotaxime when they are combined with clavulanate. The test is considered positive when the increase of inhibition zone is (≥5 mm).7,9,10 Susceptibility results for all ESBL isolates against Ciprofloxacin, Cefepime and Piperacillin-Tazobactam have been tested using the Phoenix Identification and Susceptibility System (Becton Dickinson Biosciences, Sparks, MD). The data analysis and results of antibiotic combinations were conducted using SPSS software.
Results
There was 100% correlation between the BDPhoenix ESBL identification system and the CLSI double disk diffusion confirmatory test. All the 301 isolates were susceptible to Carbapenem (Imipenem & Meropenem). The overall Piperacillin-Tazobactam susceptibility was 57.9% (64.4% E. coli and 43.6% Klebsiella pneumoniae). Only 29.6% of ESBLs (24.9% E. coli and 39.6% Klebsiella pneumoniae) were ciprofloxacin susceptible. Cefepime susceptibility was found in 8.7% (9.1% E. coli and 0.99% Klebsiella pneumoniae). The overall Gentamicin susceptibility was 38.2% (38.3% E. coli and 37.6% Klebsiella pneumoniae. 94% of ESBLs were susceptible to Amikacin (95.2% E. coli and 90.1% Klebsiella pneumoniae). 98.1% E. coli and 93.1% of Klebsiella pneumoniae were susceptible to Piperacillin-Tazobactam plus Amikacin combination. 73.7% E. coli and 61.4% of Klebsiella pneumoniae were susceptible to Piperacillin-Tazobactam plus Gentamicin combination. 96.7% E. coli and 91.1% of Klebsiella pneumoniae were susceptible to Ciprofloxacin plus Amikacin combination. 41.2% E. coli and 51.5% of Klebsiella pneumoniae were susceptible to Ciprofloxacin plus Gentamicin combination.
Discussion
In our study there was 100% correlation between the BDPhoenix ESBL identification system and the CLSI double disk diffusion confirmatory test, the same result was previously reported by Enno Stürenburg et al., where 100% specificity and 100% susceptibility of ("Phoenix Identification and susceptibility system" by Becton Dickinson) in ESBL detection was proved.11 All our isolates were 100% susceptible to Carbapenems (Table 1). It is known that the most successful antibiotic treatment for ESBLs are carbapenems.12 They are considered the drugs of choice for any serious infections caused by ESBLs.13
Table 1. Susceptibility of ESBLs to different antibiotics.
| E. coli (%) | K. pneumonia (%) | Overall ESBLs (%) | |
|---|---|---|---|
| Carbapenem | 100 | 100 | 100 |
| Piperacillin-Tazobactam | 64.4 | 43.6 | 57.9 |
| Ciprofloxacin | 24.9 | 39.6 | 29.6 |
| Cefepime | 9.1 | 0.99 | 8.7 |
| Gentamicin | 38.3 | 37.6 | 38.2 |
| Amikacin | 95.2 | 90.1 | 94 |
ESBL: Extended Spectrum Beta - Lactamase
Piperacillin-Tazobactam susceptibility was variable and demons-trated as 64.4% for E. coli and 43.6% for K. pneumoniae (Table 1). This is comparable to ESBL susceptibility reported from Europe for Piperacillin-Tazobactam (72.5% E. coli and 38.6% Klebsiella pneumoniae)14 (Table 2). Similar susceptibility was reported in USA (80.0% for E. coli and 42.1% for Klebsiella pneumoniae)14 (Table 2). The overall susceptibility of ESBLs to piperacillin/tazobactam is only 57.9% (Table 1). This low susceptibility makes piperacillin/tazobactam not a good choice as empirical therapy if suspicion of ESBL is high. However, we found that the some isolates resistant to piperacillin/tazobactam were susceptible to gentamicin and amikacin; and the combined susceptibility to both piperacillin/tazobactam plus an aminoglycoside is additive where piperacillin/tazobactam covers the isolates resistant to aminoglycoside and the aminoglycosides covers the isolates resistant to piperacillin/tazobactam, for example combination of piperacillin/tazobactam plus gentamicin increases the susceptibility to 73.7% against E. coli and 61.4% against K. pneumoniae (Table 3). The susceptibility is further enhanced if the piperacillin/tazobactam was added with amikacin (susceptibility is 98.1% against E. coli and 93.1% against K. pneumoniae) (Table 3).
Table 2. ESBL susceptibility in Oman, Europe & USA.
| Oman | Europe14 | USA14 | ||||
|---|---|---|---|---|---|---|
| E. coli | K. pneumoniae | E. coli | K. pneumoniae | E. coli | K. pneumoniae | |
| Pip-Taz | 64.4% | 43.6% | 72.5% | 38.6% | 80.0% | 42.1% |
| Cip | 24.9% | 39.6% | 20.2% | 57.5 | 20% | 36.8 |
Pip-Taz: Piperacillin/Tazobactam; Cip: Ciprofloxacin. Europe & USA results adopted from Herman Goossensa et al.14
Table 3. Susceptibility of ESBLs to Antibiotic Combination.
| E. coli | K. pneumoniae | |
|---|---|---|
| Pip-Taz + AK | 98.1 | 93.1 |
| Pip-Taz + GN | 73.7 | 61.4 |
| CIP + AK | 96.7 | 91.1 |
| CIP + GN | 41.2 | 51.5 |
Pip-Taz: Piperacillin-Tazobactam; CIP: Ciprofloxacin; Cefe: Cefepime; GN: Gentamicin; AK: Amikacin
Ciprofloxacin has very low activity against ESBLs, only 29.6% of ESBLs are susceptible (24.9% E. coli and 39.6% K. pneumoniae). These results are comparable to those in Europe (20.2% E. coli and 57.5% K. pneumoniae) (Table 3), similar results were also found in USA (20% E. coli and 36.8% K. pneumoniae)14 (Table 2). Combination of Ciprofloxacin plus Gentamicin improves the susceptibility to (41.2% for E. coli and 51.5% for K. pneumoniae). Amikacin boosts the susceptibility of Ciprofloxacin to (96.7% for E. coli and 91.1% for Klebsiella pneumoniae). Cefepime has very poor activity against ESBLs producing strains; the susceptibility to Cefepime was 9.1% in E. coli and 0.99% in K. pneumoniae.
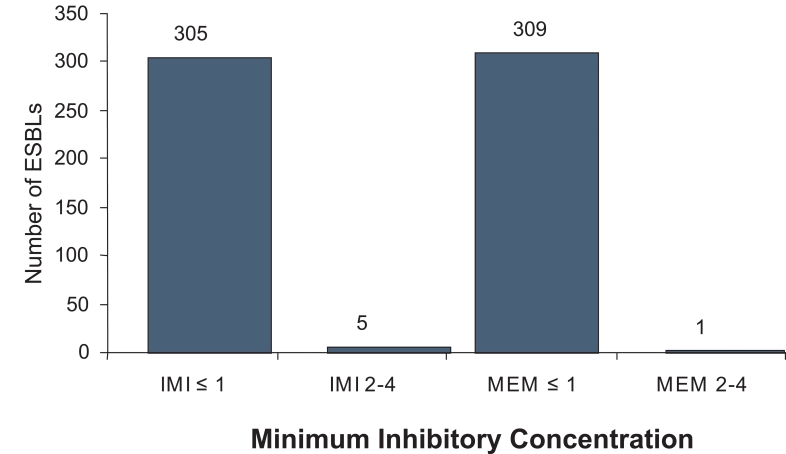
It is very clear that Carbapenems are the best empirical therapy for suspected ESBL producing strains. However, repeated exposure to crabapenem has its own cost in terms of emergence of other multi-resistant organisms e.g. Pseudomonas aeruginosa and Acinetobacter spp.15 Even though, Robert and coworkers have not detected any increase in carbapenem resistance despite continued use of meropenem and imipenem.16 The other concern regarding overuse of carbapenem is the emergence of ESBLs tolerant to Carbapenems. Babini and Livermore have seen that of 1% of the ESBL-producing K. pneumoniae have decreased susceptibility to meropenem with high MIC values.17 Kizirgil and coworkers have reported that 5.3% of ESBLs were associated with elevated MICs at 2-4mg/ml of meropenem.18 In this study 98.4% of ESBLs were susceptible to Imipenem with MIC of ≤1µg/ml and 99.7% susceptible to Meropenem with MIC of ≤1µg/ml (Figure 1). The concern about emergence of Carbapenems resistant gram negative bacilli and ESBLs should encourage physicians to look for other alternatives for the empirical treatment of ESBLs.
Figure 1.
Carbapenem MIC level for ESBLs.
We have demonstrated clearly that Piperacillin/Tazobactam combination with Amikacin has almost similar activity against ESBL producing E. coli (98.1%), to that of Imipenem (98.4%) and Meropenem (99.7%). Piperacillin/Tazobactam combination with Amikacin activity against K. pneumoniae (93.1%) is also not far behind that of Imipenem. Ciprofloxacin in combination with Amikacin has an activity against ESBLs (96.7% for E. coli and 91.1% for K. pneumoniae) comparable to that of Imipenem. The recommendation of combination therapy with Amikacin plus either Piperacillin/Tazobactam or Ciprofloxacin in infections caused by ESBLs is an alternative to Carbapenems as empirical therapy when ESBL infection is suspected.
Conclusion
ESBLs have high resistance profile against Piperacillin/Tazobactam and Ciprofloxacin. The ESBLs from Oman have similar resistance patterns as those reported from United Kingdom and United State of America. This resistance decreases when these drugs are combined with Amikacin. All ESBLs are susceptible to Carbapenems. However, Carbepenam overuse can lead to emergence of carbapenems resistant gram negative bacilli and ESBLs. Combination of Amikacin plus Piperacillin/Tazobactam is a feasible empirical therapy for ESBLs.
References
- 1.Goldstein FW. Combating resistance in a challenging, changing environment. Clin Microbiol Infect 2007. Jun;13(Suppl 2):2-6 10.1111/j.1469-0691.2007.01721.x [DOI] [PubMed] [Google Scholar]
- 2.Kotapati S, Kuti JL, Nightingale CH, Nicolau DP. Clinical implications of extended spectrum β-lactamase (ESBL) producing Klebsiella species and Escherichia coli on cefepime effectiveness. J Infect 2005. Oct;51(3):211-217 10.1016/j.jinf.2005.01.005 [DOI] [PubMed] [Google Scholar]
- 3.Stürenburg E, Mack D. Extended-spectrum beta-lactamases: implications for the clinical microbiology laboratory, therapy, and infection control. J Infect 2003. Nov;47(4):273-295 10.1016/S0163-4453(03)00096-3 [DOI] [PubMed] [Google Scholar]
- 4.Sorlózano A, Gutiérrez J, de Dios Luna J, Oteo J, Liébana J, Soto MJ, et al. High presence of extended-spectrum β-lactamases and resistance to quinolones in clinical isolates of Escherichia coli. Microbiol Res 2007;162(4):347-354 10.1016/j.micres.2006.02.003 [DOI] [PubMed] [Google Scholar]
- 5.Jacoby GA, Munoz-Price LS. The new β-lactamases. N Engl J Med 2005. Jan;352(4):380-391 10.1056/NEJMra041359 [DOI] [PubMed] [Google Scholar]
- 6.Ramphal R, Ambrose PG. Extended-spectrum β-lactamases and clinical outcomes: current data. Clin Infect Dis 2006. Apr;42(Suppl 4):S164-S172 10.1086/500663 [DOI] [PubMed] [Google Scholar]
- 7.Drieux L, Brossier F, Sougakoff W, Jarlier V. Phenotypic detection of extended-spectrum beta-lactamase production in Enterobacteriaceae: review and bench guide. Clin Microbiol Infect 2008. Jan;14(Suppl 1):90-103 10.1111/j.1469-0691.2007.01846.x [DOI] [PubMed] [Google Scholar]
- 8.Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing. Wayne, PA: CLSI, 2005. [Google Scholar]
- 9.Carter MW, Oakton KJ, Warner M, Livermore DM. Detection of extended-spectrum beta-lactamases in klebsiellae with the Oxoid combination disk method. J Clin Microbiol 2000. Nov;38(11):4228-4232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.M’Zali FH, Chanawong A, Kerr KG, Birkenhead D, Hawkey PM. Detection of extended-spectrum beta-lactamases in members of the family enterobacteriaceae: comparison of the MAST DD test, the double disc and the Etest ESBL. J Antimicrob Chemother 2000. Jun;45(6):881-885 10.1093/jac/45.6.881 [DOI] [PubMed] [Google Scholar]
- 11.Stürenburg E, Sobottka I, Feucht HH, Mack D, Laufs R. Comparison of BDPhoenix and VITEK2 automated antimicrobial susceptibility test systems for extended-spectrum beta-lactamase detection in Escherichia coli and Klebsiella species clinical isolates. Diagn Microbiol Infect Dis 2003. Jan;45(1):29-34 10.1016/S0732-8893(02)00481-9 [DOI] [PubMed] [Google Scholar]
- 12.Doménech-Sánchez A, Pascual A, Suárez AI, Alvarez D, Benedí VJ, Martínez-Martínez L. Activity of nine antimicrobial agents against clinical isolates of Klebsiella pneumoniae producing extended-spectrum β-lactamases and deficient or not in porins. J Antimicrob Chemother 2000. Nov;46(5):858-859 10.1093/jac/46.5.858 [DOI] [PubMed] [Google Scholar]
- 13.Paterson DL, Mulazimoglu L, Casellas JM, Ko WC, Goossens H, Von Gottberg A, et al. Epidemiology of ciprofloxacin resistance and its relationship to extended-spectrum β-lactamase production in Klebsiella pneumoniae isolates causing bacteremia. Clin Infect Dis 2000. Mar;30(3):473-478 10.1086/313719 [DOI] [PubMed] [Google Scholar]
- 14.Goossens H, Grabein B. Prevalence and antimicrobial susceptibility data for extended-spectrum β-lactamase- and AmpC-producing Enterobacteriaceae from the MYSTIC Program in Europe and the United States (1997-2004). Diagn Microbiol Infect Dis 2005. Dec;53(4):257-264 10.1016/j.diagmicrobio.2005.10.001 [DOI] [PubMed] [Google Scholar]
- 15.Rahal JJ, Urban C, Horn D, Freeman K, Segal-Maurer S, Maurer J, et al. Class restriction of cephalosporin use to control total cephalosporin resistance in nosocomial Klebsiella. JAMA 1998. Oct;280(14):1233-1237 10.1001/jama.280.14.1233 [DOI] [PubMed] [Google Scholar]
- 16.Masterton RG, Turner PJ. Trends in antimicrobial susceptibility in UK centres: the MYSTIC Programme (1997-2002). Int J Antimicrob Agents 2006. Jan;27(1):69-72 10.1016/j.ijantimicag.2005.09.011 [DOI] [PubMed] [Google Scholar]
- 17.Babini GS, Livermore DM. Antimicrobial resistance amongst Klebsiella spp. collected from intensive care units in Southern and Western Europe in 1997-1998. J Antimicrob Chemother 2000. Feb;45(2):183-189 10.1093/jac/45.2.183 [DOI] [PubMed] [Google Scholar]
- 18.Kizirgil A, Demirdag K, Ozden M, Bulut Y, Yakupogullari Y, Toraman ZA. In vitro activity of three different antimicrobial agents against ESBL producing Escherichia coli and Klebsiella pneumoniae blood isolates. Microbiol Res 2005;160(2):135-140 10.1016/j.micres.2004.10.001 [DOI] [PubMed] [Google Scholar]