Abstract
Objectives
To determine if the knowledge and awareness of "ventilator bundle" helped in the prevention of ventilator associated pneumonia and other outcome variables in the patients admitted to our AICU.
Design
A retrospective obsevational study from a pospectively collected data.
Participants
All the adult medical and surgical patients who were intubated and ventilated in our AICU from January to September in the year 2005 and 2006 were included in the study. During the period of October to December 2005 the critical care nurses and the staff were educated and made aware about the problem of VAP and the use of vrntilator bundle in helping to prevent this nososcomial infection. Patients who expired within 24 hrs of admission, who were transferred to tertiary care unit within 48hrs, and those who were diagnosed with pulmonary embolism or had gastrointestinal bleed prior to admission were excluded from this study.
Intervention
The concept of " ventilator bundle’ was introduced after educating the nursing staff, respiratory therapists and the medical personnel through group discussions and presentations in the infection control and staff development symposia. "Ventilator bundle "is a package of evidence -based interventions that include: (1) Elevation of patient’s head of bed to 30- 45 degrees; (2) Daily sedation vacation and daily assessment of readiness to extubation; (3) Peptic ulcer prophylaxis; (4) Deep vein thrombosis (DVT) prophylaxis.
Measurement
Demographic data was collected from the computer database. VAP was diagnosed when it met the (clinical non-invasive) diagnostic criteria. Incidence of VAP was calculated in the medical and surgical patients separately.
Results
Introducing the concept of "ventilator bundle" significantly reduced the incidence of VAP by 24.2% in the surgical patients and by 12% in the medical group. It significantly reduced the incidence of upper gastrointestinal bleed. The mean age of patients who developed VAP in 2006 was significantly higher in both the medical and the surgical groups. The length of stay decreased significantly in the surgical group, while it increased in the medical group. The mean duration of ventilation was reduced by 29.1% in the medical group and by 55.12% in the surgical group in those patients who developed VAP. In patients who did not develop VAP, the decrease of 9.9% in the mean duration of ventilation was seen in the surgical group while the mean duration of ventilation increased by 14.2% in the medical group.
Conclusions
Introducing the concept of "ventilator bundle" helped us to reduce the incidence of VAP, reduce the incidence of upper gastrointestinal bleed. It reduced the mean duration of ventilation in both the medical and surgical patients who developed VAP. The effect on decreasing the length of stay was seen in the surgical patients only.
Introduction
Preventing VAP is one of the important safety issues in critically ill patients receiving mechanical ventilation. In our effort to prevent this complication the concept of "Ventilator bundle "was introduced. This is based on the recommendations by Institute of health improvement.1
We conducted this retrospective study to determine the impact of this evidence based practice on improving patient safety and outcome.
Methods
Demographic data of all the adult medical and surgical patients who were intubated and ventilated in our AICU from January to September in the year 2005 and 2006 was collected from the data base. Patients who expired within 24 hrs of admission, who were transferred to tertiary care unit within 48 hrs, those who were diagnosed with pulmonary embolism at admission and those who had gastrointestinal bleed prior to admission were excluded from this study.
The educational activities were carried out during the months of October, November and December -2005. The nursing staff, respiratory therapists and the medical personnel were introduced to the concept of "Ventilator Bundle "through group discussions and presentations in the infection control and staff development symposiums.
Ventilator Bundle is a package of evidence based interventions.2
This includes the following recommendations which are to be followed as an all or none intervention.
Elevation of patient’s head of bed to 30-450
Daily sedation vacation and daily assessment of readiness to extubation.
Peptic ulcer prophylaxis.
Prophylaxis for (DVT) Deep vein thrombosis.
The nursing staff was empowered to check for the implementation of the bundle element on every patient every time.
VAP was diagnosed when it met the clinical non invasive diagnostic criteria.
(Modified CDC criteria).3
Presence of any two of the following was considered as diagnostic of VAP.
Significant heavy growth reported in the culture from tracheal aspirates.
Temp->380c or <350c
Development of progressive new infiltrate on X-ray.
Leucocytosis WBC > 10x 109 /L or leucopenia WBC <3x109 /L
Ten leucocytes per HPF in gram stain of tracheal aspirates.
Incidence of VAP was calculated in the medical and surgical sub-populations.
The data collected was analyzed for the incidence of VAP and the surrogate outcome.
The surrogate outcome measures that were analyzed were mean length of stay, mean duration of ventilation, and the incidence of gastrointestinal bleed.
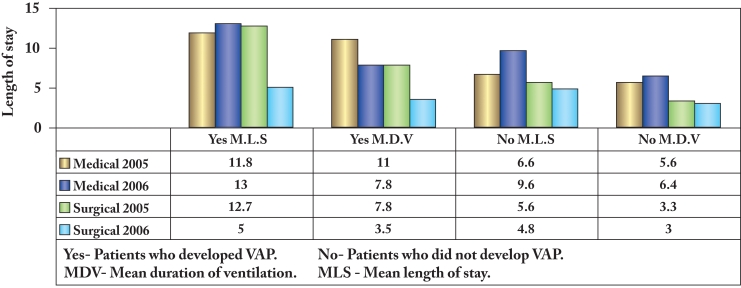
Graph: Comparative Outcome in the 2 years.
Results
Table 1: shows that the mean age of the patients who developed VAP in 2006 was higher (72.2 yrs) (+13 yrs) in the medical group and (+1yr) in the surgical group, but the difference did not achieve statistical significance.(p>0.05).
Table 1. Mean age of the Patients.
| Medical 2005 | Surgical 2005 | Medical 2006 | Surgical 2006 | |
|---|---|---|---|---|
| Mean age of pt developing VAP | 59.2 | 56.0 | 72.20 | 57.0 |
| Mean age of pt not developing VAP | 57.1 | 38.7 | 61.0 | 33.2 |
| Range | 18-100 | 21-86 |
VAP: Ventilator Associated Pneumania
Table 2: shows that the incidence of VAP reduced by 24.2%. in the surgical and by 12% in the medical group.
Table 2. Incidence of Ventilator Associated Pneumania and outcome measures:
| Before –2005 Jan- August |
After 20006 Jan - August |
|||||||
|---|---|---|---|---|---|---|---|---|
| Medical N=23 |
Surgical N = 12 |
Medical N=22 |
Surgical N =11 |
|||||
| VAP / No VAP | Y | N | Y | N | Y | N | Y | N |
| Number of patients | 8 | 15 | 4 | 8 | 5 | 17 | 1 | 10 |
| Mean length of stay | 11.8 | 6.6 | 12.7 | 5.6 | 13.0 | 9.6 | 5.0 | 4.8 |
| Mean duration of ventilation | 11.0 | 5.6 | 7.8 | 3.3 | 7.8 | 6.4 | 3.0 | 3.5 |
| Incidence of fresh upper GIT bleed (Coffee ground aspirate) | 7/23 (30.43%) | 1/12 (8.3%) | 1/22 (4.54%) | 0/11 (0%) | ||||
| Incidence of VAP | 34.78% | 33.33% | 22.72% | 9.09% | ||||
VAP: Ventilator Associated Pneumania
The reduction in the incidence of upper gastrointestinal bleed was significant in both the groups (p<0.05).
The mean length of stay in the patients who developed VAP decreased in the surgical group by 7.1 days, but in contrast the length of stay increased in the medical group by 1.2days.
In the group which did not develop VAP a similar finding was observed but the decrease in the mean length of stay in surgical patients was less (0.6days), while the medical patients had an increase stay of 3 days.
Medical patients had higher mean duration of ventilation as compared to the surgical patients both before and after the implementation of the bundle.
The mean duration of ventilation decreased (4.3 days) in the surgical group as compared to 3.2 days in the medical group.
Discusion
Nizwa hospital AICU admits an average of 240 patients per year, a mixture of surgical and medical patients.
Audit reported a 36% incidence of VAP in our AICU. Most studies3,4 have reported a varied incidence from 17-30%, depending upon the diagnostic criteria used in diagnosing VAP. The reported incidence of VAP is higher in academic institutions.5
Studies have shown that the risk of VAP increases with the increase in the duration of mechanical ventilation.3,4
VAP is a subset of nosocomial pneumonia seen to develop in patients who are intubated and ventilated.
The pathogenesis of VAP commences in most cases with the bacteria entering the trachea during initial intubation, during subsequent reintubations or via the leakage around the tracheal tube cuff.6
The organisms responsible are multiresistant and require a higher broad spectrum antibiotic for at least 2 weeks for cure.
Thus this results in longer length of stay and prolonged use ventilator support.
There is always a threat to the other patients of getting this infection as a result of cross contamination through the hands of the health care workers.
Thus it results in increase in the burden to the health care costs and the ICU resources.7 It can even result in septic shock &death.
Various studies have increasingly shown that the use of ventilator bundle is successful in reducing the incidence of VAP.2,8,9
In our study we attempted to analyze the effectiveness of the implementation of ventilator bundle.
The incidence of VAP decreased by 12.06%and 24.2% in the medical and surgical sub-populations respectively in the year 2006 (table-1) after the bundle was implemented.
In both the groups the common risk factor was intubation and ventilation.
The difference of more than 5% decrease in the surgical group as compared to medical group could be attributed to the higher prevalence of co-morbidities, poor pre-VAP status in the medical group and the higher mean age of this population.
Age and other co-morbidities are independent risk factors for the development of VAP in critically ill patients.3 As seen in table 1, relatively elderly population had VAP after the bundle was implemented.
The graph shows that In the medical sub-population in our ICU, the length of stay did not decrease, but rather increased (+1 days) and more so (+3 days) in the patients who did not develop VAP.
This is contrary to our expectation. In addition to various social reasons, one of the reasons we could attribute to the increased length of stay were, the non-availability of bed in the High dependency unit. Various other factors also impact the length of stay in the intensive care unit and it will not be appropriate to abandon this bundle.
The benefits in terms of decreased length of stay and decreased duration of ventilation were seen in the surgical group.
The decrease in the incidence of gastrointestinal bleeding was statistically significant in both the sub-populations in our unit. The administration of stress ulcer prophylaxis is controversial.
We had administered Ranitidine to all our patients.
Collard and colleagues8 had recommended the use of sucralfate rather than H2- antagonists for preventing bleeding. Cook and colleagues in their study3 had found a non-significant increase in the risk of VAP while a significant decrease in the gastrointestinal bleeding with ranitidine.
Minimizing the intubation time, semi recumbent positioning, and providing the prophylaxis for deep vein thrombosis are relatively uncontroversial measures for VAP prevention.
Further the general preventive measures of hand hygiene and circuit care are not a part of this bundle.
Awareness and education were the main focus in our unit for preventing VAP. We do not employ any special oscillatory beds or endotracheal tubes with provision of continuous subglottic secretions.
The limitations of our study are a small population studied and hence could not deduce statistical significance of the findings.
Further individual risk factors which predispose the patients to the development of VAP have not been considered.
The nurses were empowered and educated but the actual performance in the emergency hours was not documented.
Due to the non-availability of the quantitative methods of sampling, the laboratory method to establish the diagnosis of pneumonia is less rigorous.
The strength of the study is that so far separate subpopulations are not studied in the same intensive care unit.
This study would aim to direct our efforts to the patient subpopulation and help to determine the latent causes which prevent the effectiveness of this practice.
This in turn would help to determine alternative strategies to decrease the length of stay in the respective sub-populations.
Conclusion
Implementing the evidence based practice led to a decrease in the incidence of VAP in both surgical and medical sub-populations.
It helped to decrease mean length of stay and mean duration of ventilation in the surgical sub-population. This was clinically significant but not statistically significant.
It significantly reduced the incidence (p<0.05) of upper GI bleed in the population studied.
Incorporating this bundle in the AICU computer module will help in the continuity of its use and result in improving patient safety in the intensive care unit.
Acknowledgements
I would like to thank Dr Sunil Bhat (epidemiologist) for the statistical assistance and the nursing staff of our AICU for their help in data collection. I am indebted to the patients who put their care in our hands.
References
- 1.Institute for health care improvement. Implement the ventilator bundle. Available at http//www.ihi.org/IHI/Topics/crit care/intensive care/changes/implement the ventilator bundle.htm
- 2.Nolan T, Berwick DM. All-or-none measurement raises the bar on performance. JAMA 2006. Mar;295(10):1168-1170 10.1001/jama.295.10.1168 [DOI] [PubMed] [Google Scholar]
- 3.Cook DJ, Walter SD, Cook RJ, Griffith LE, Guyatt GH, Leasa D, et al. Incidence of and risk factors for ventilator-associated pneumonia in critically ill patients. Ann Intern Med 1998. Sep;129(6):433-440 [DOI] [PubMed] [Google Scholar]
- 4.Ibrahim EH, Tracy L, Hill C, Fraser VJ, Kollef MH. The occurrence of ventilator-associated pneumonia in a community hospital: risk factors and clinical outcomes. Chest 2001. Aug;120(2):555-561 10.1378/chest.120.2.555 [DOI] [PubMed] [Google Scholar]
- 5.Akça O, Koltka K, Uzel S, Cakar N, Pembeci K, Sayan MA, et al. Risk factors for early-onset, ventilator-associated pneumonia in critical care patients: selected multiresistant versus nonresistant bacteria. Anesthesiology 2000. Sep;93(3):638-645 10.1097/00000542-200009000-00011 [DOI] [PubMed] [Google Scholar]
- 6.Petring OU, Adelhøj B, Jensen BN, Pedersen NO, Lomholt N. Prevention of silent aspiration due to leaks around cuffs of endotracheal tubes. Anesth Analg 1986. Jul;65(7):777-780 10.1213/00000539-198607000-00013 [DOI] [PubMed] [Google Scholar]
- 7.Warren DK, Shukla SJ, Olsen MA, Kollef MH, Hollenbeak CS, Cox MJ, et al. Outcome and attributable cost of ventilator-associated pneumonia among intensive care unit patients in a suburban medical center. Crit Care Med 2003. May;31(5):1312-1317 10.1097/01.CCM.0000063087.93157.06 [DOI] [PubMed] [Google Scholar]
- 8.Collard HR, Saint S, Matthay MA. Prevention of ventilator-associated pneumonia: an evidence-based systematic review. Ann Intern Med 2003. Mar;138(6):494-501 [DOI] [PubMed] [Google Scholar]
- 9.Dodek P, Keenan S, Cook D, Heyland D, Jacka M, Hand L, et al. Canadian Critical Care Trials Group. Canadian Critical Care Society Evidence-based clinical practice guideline for the prevention of ventilator-associated pneumonia. Ann Intern Med 2004. Aug;141(4):305-313 [DOI] [PubMed] [Google Scholar]