Abstract
The presence of false negative nuclear stress test in the settings of positive electrocardiographic changes is a very unusual phenomenon and is usually secondary to balanced ischemia of the myocardial segments evaluated by SPECT-TL. We present a case of an 81-year old post-menopausal female who presented to her primary care physician for evaluation of a 6-week dyspnea on exertion and was referred to our institution for exercise stress test with Thallium SPECT with the objective of ruling out coronary artery disease and identifying possible areas of myocardial ischemia. The resting electrocardiogram was unremarkable and stress test evaluation was made. The patient was admitted to the cardiac care unit and coronary artery bypass grafting was successfully performed. The presence of false negative nuclear stress test in the settings of positive electrocardiographic changes is a very unusual phenomenon and is usually secondary to balanced ischemia of the myocardial segments evaluated by SPECT-TL. Patients undergoing stress tests with these characteristics should undergo careful evaluation and a high level of suspicion should be adopted for further diagnostic assessment of coronary artery disease.
Key words: false negative stress testing, balanced ischemia.
Introduction
Nuclear imaging with stress myocardial perfusion techniques, mostly single-photon emission computed tomography with radioisotopes such as Thallium (SPECT-TL) and techniciam-99m, has become the preferred modality for the non-invasive evaluation of ischemic heart disease. This diagnostic method plays a particularly important role in the identification of ischemic territories and myocardial viability assessment.1 Its sensitivity (85–90%) has been reported to be affected by different factors such as lesion characteristics and exercise test performance.2 Reports of false negative myocardial perfusion scintigraphy tests have been well described in the literature. They have been associated with different factors such as location of the lesions in the left circumflex artery or bifurcation areas, lesions with mild atherosclerotic burden producing non-obstructive coronary heart disease, single vessel compromise, the use of antianginal agents prior to the test or low levels of exercise leading to low myocardial oxygen consumption not sufficient to achieve diagnostic thresholds during stress test evaluation.3 Similarly, some cases of false negative Thallium scans can be explained by the use of certain agents such as caffeine or low molecular weight heparin before the test. However, this has only been related to stress tests with dipyridamole and the most likely explanation is an interaction with the adenosine receptor antagonist.4,5
Cases of false negative ECG during exercise stress test in patients with coronary artery disease later confirmed by positive nuclear studies and coronary angiogram have often been described. However, false negative SPECT-Tl studies associated with balanced ischemia are less commonly seen and different theories have been proposed to explain this phenomenon. We present a case of a truly positive electrocardiographic stress test with a false negative nuclear scan in a patient with multivessel coronary artery disease, a very unusual phenomenon which is rarely seen and which has had very few reports in the medical literature.
Case Report
We present a case of an 81-year old post-menopausal female with a past medical history of hypertension and dyslipidemia, the latter managed with non-pharmacological treatment. Her outpatient pharmacological regimen consisted of mlodipine and hydrochlorothiazide for blood pressure control and aspirin for primary cardiovascular prevention. She presented to her primary care physician for evaluation of a 6-week dyspnea on exertion and she was referred to our institution for exercise stress test with Thallium SPECT with the objective of ruling out coronary artery disease and identifying possible areas of myocardial ischemia. The patient denied any other complaints including chest pain, palpitations, fatigue, orthopnea, dizziness or cough. There were no other risk factors for cardiovascular disease, such as history of diabetes mellitus, known prior cardiovascular events, smoking history or family history of premature cardiovascular disease. At presentation the patient's exercise tolerance was minimal due to the shortness of breath described above.
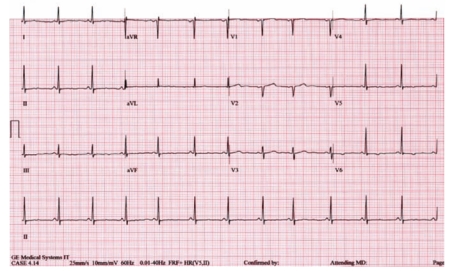
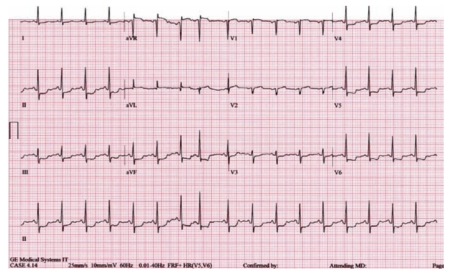
The resting electrocardiogram was unremarkable as shown in Figure 1. The patient presented for stress test evaluation following the standard protocol for nuclear imaging established in our institution. This included a one-day test with rest/stress phases with 99m-sestamibi infusion followed by myocardial perfusion imaging with SPECT. The stress protocol followed for this case included exercise treadmill and the heart rate achieved was 140 beats per minute which was 101% of her maximal predicted heart rate, with a maximal blood pressure of 160/90 mmHg during peak exercise. At that level of exercise, after approximately about 4 min the electrocardiogram showed ST-segment depression of 2 mm in leads I, II, V5 and V6 with concomitant ST-segment elevation of 1 mm in aVR; however, the patient remained symptom free during the entire test (Figure 2). The patient's calculated Duke treadmill score (−10), carries a 64% probability of significant CHD, a 47% probability of severe CHD and a 28% 5-year mortality.6–8 The exercise protocol was, therefore, stopped and the patient was taken to the nuclear laboratory to complete SPECT imaging.
Figure 1.
Baseline electrocardiography.
Figure 2.
ST-segment depression in leads I, II, V5, V6 and ST-segment elevation in lead aVR.
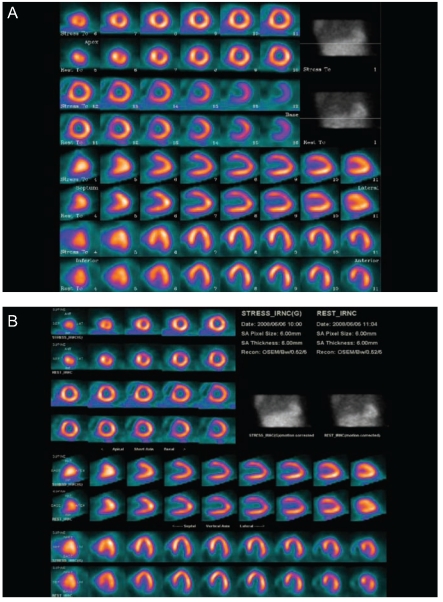
Myocardial perfusion imaging was performed both at rest and immediately after discontinuation of the exercise treadmill phase and standardized imaging integration software (Myovation™, General Electric Healthcare Technologies, Milwaukee, Wisconsin, USA) was used to gate and reconstruct the planimetric images for results to be interpreted. Tomographic imaging of the different segments and myocardial segments and walls were completely normal and did not show any apparent defects in perfusion in any territory at rest or at stress (Figures 3A and B) with no significant wall motion abnormalities, no transient ischemic dilatation and a left ventricular systolic ejection fraction of 54%. However, given the markedly positive electrocardiogram during peak exercise and the patient's clinical presentation, she was taken to the cardiac catheterization laboratory for angiographic evaluation. Cardiac catheterization showed triple vessel coronary artery disease with 95% stenosis on the distal left main, 40% stenosis of the mid segment of the right coronary artery, 75% stenosis of the mid segment of the left anterior descending coronary artery and 70% stenosis of the distal segment of the left circumflex coronary artery (Figure 4A and B). The patient was admitted to the cardiac care unit and coronary artery bypass grafting was successfully performed.
Figure 3.
(A) Planar images-eCToolBox. (B) Planar images-MYOVATION.
Figure 4.
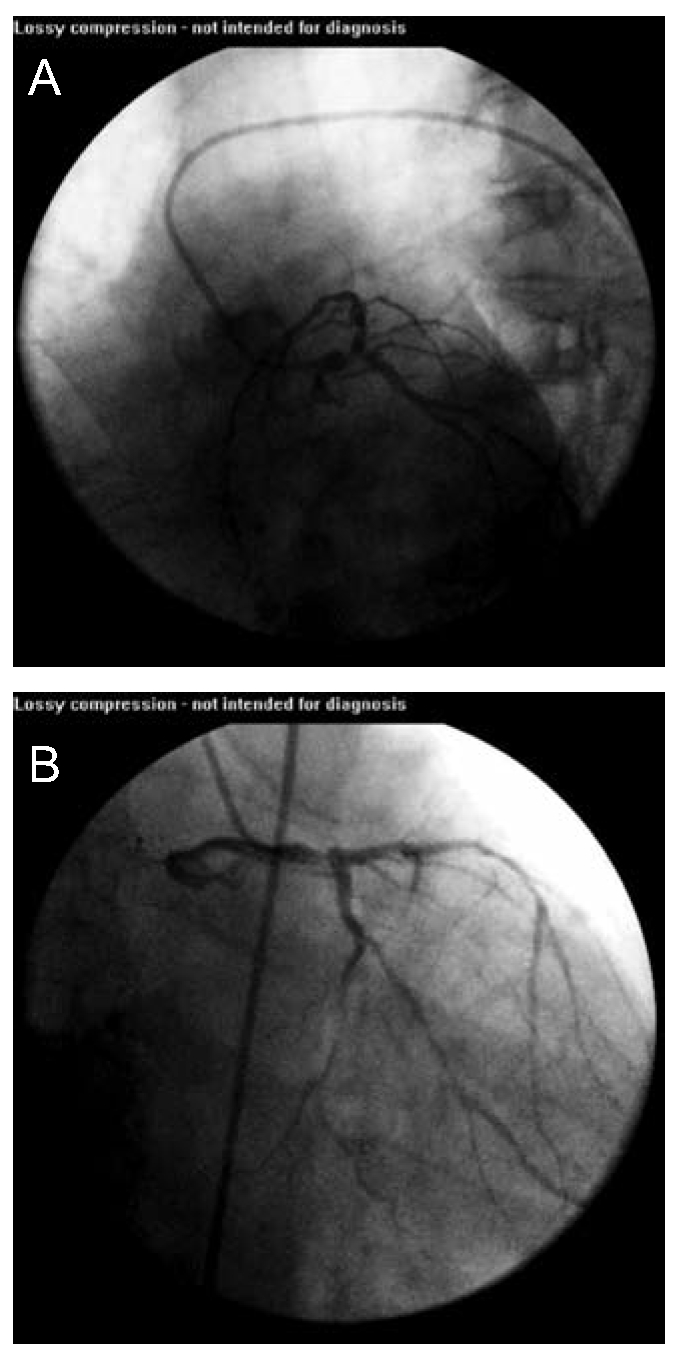
(A) LAO caudal projection showing severe distal left main disease. (B) RAO caudal projection showing severe distal left main disease.
Discussion
Exercise stress testing is a common screening tool for the non-invasive evaluation of patients with suspected coronary heart disease.8 In the last few decades, the combination of electrocardiographic evaluation with imaging techniques such as echocardiography or nuclear scintigraphy has improved the diagnostic accuracy of the stress test. The overall sensitivity and specificity of exercise ECG testing is approximately 65–68% and 72–77% respectively9–11 while Thallium SPECT provides a sensitivity of 81.9% with a specificity of 96.0% for the evaluation of the extension of myocardial ischemia based on comparisons performed with pathology specimens.12
False negative results in patients undergoing electrocardiographic stress test with exercise have been reported and they are often secondary to submaximal exercise stress testing, mild to moderate stress-induced ischemia, single vessel coronary artery disease (CAD) and electrical cancellation of the ischemic vectors. This last phenomenon, which has been associated to multi-vessel disease, has been attributed to a process called ischemic ST-segment counterpoise. This is basically the cancellation of the ischemic ST-segment vectors, secondary to severe ischemia that is homogenously distributed and that involves segments of the myocardium that are opposite to each other.13 This agrees with previous data showing that Thallium scans are more sensitive to detect multivessel coronary artery disease than the exercise stress test, especially in patients with a prior history of myocardial infarction in which the distribution of the ischemic vectors might play a similar role.14 Similarly, it has been reported that positive Thallium scans can identify 75% of the patients with false negative electrocardigraphic exercise tests and 82% of the patients with positive ECG exercise tests.15 A study of 15 symptomatic patients demonstrated that myocardial perfusion imaging after the combination of dipyridamole and low level exercise can help to identify individuals with true ischemic segments with false negative electrocardiographic stress test and non-diagnostic Thallium scans secondary to sub-maximal exercise during the test.16
Our patient had markedly positive electrocardiographic changes but a false negative SPECT-TL. While she achieved adequate exercise levels during the stress test, factors such as inadequate myocardial effort during peak exercise were unlikely to explain the negative nuclear study and despite having intermediate pre-test probability of CAD,17 she was found to have severe disease. The literature reports similar cases with multi-vessel coronary disease presenting as false negative scans and true positive electrocardiographic exercise test confirmed by coronary angiogram.18–20 The exact incidence of this phenomenon has not yet been accurately described and a clear etiology behind this process is not completely understood. Despite this, the estimated frequency of false negatives of SPECT-TL has been reported to be around 11% and, according to some series, the ability of this phenomenon to correctly localize the ischemic region and calculate the extent of myocardial involvement can be as low as 20% in patients with triple vessel disease.21 In a recent sub-analysis of the J-ACCESS study, 293 out of a total of 2,383 patients undergoing exercise testing with myocardial perfusion imaging were noted to have ischemic electrocardiographic changes with no reversible abnormalities.22
Our case represents this phenomenon catalogued as balanced ischemia in which the radiotracer uptake by the different myocardial regions becomes homogenously distributed secondary to globalized hypoperfusion in all the segments of the myocardium. The principle of nuclear imaging techniques to detect ischemic areas is based on the fact that significant differences, defined as 15–20%, in myocardial perfusion between different regions are identified as reversible defects within the cardiac muscle when exposed to stress.23 The quantification of the radiotracer's distribution could demonstrate global reduction in the uptake, but Thallium assessment is based on relative differences in the signal density between myocardial territories. Therefore, the presence of uniformly distributed ischemic burden in all the myocardial regions evaluated by SPECT-TL can lead to false negative results.24 In our case, the associated SPECT-TL indicated homogeneous perfusion of the heart both at stress and rest phases without significant differences relative to the washout or redistribution phases, and was interpreted as normal.
In general, a positive electrocardiographic test with a negative TL in patients with suspected coronary artery disease in whom doubts about the diagnosis are raised usually requires further evaluation with more invasive techniques. In our patient, despite the negative TL and because of case history and the strongly positive ECG, the patient underwent cardiac catheterization. This was also based on previous studies demonstrating the prognostic value of ST changes during exercise stress test. Colby et al. highlighted the importance of caution when interpretating the ST changes seen during exercise stress test. They found that the degree of exercise-induced ST depression did not correlate with perfusion defects in the exercise-induced Thallium-201. Arguably, this might not be true with ischemic ECG response to intravenous adenosine administration and normal perfusion on SPECT, as it was shown that these patients, and particularly women, are at low risk of cardiovascular events, even after long-term follow up.25 However, patients presenting with strongly positive electrocardiographic changes during exercise tests, especially at early stages of the Bruce protocol with low levels of oxygen consumption (low Mets or low heart rate), warrant a careful and more thorough evaluation for coronary disease, even in the setting of negative nuclear studies as they have been identified to have a higher risk of myocardial ischemia.26 Similarly, in terms of diagnostic and prognostic implications, vasodilator perfusion SPECT share similar characteristics with exercise stress testing.
Another theory behind the presence of false negative SPECT-TL with a truly positive electrocardiogram during peak exercise has been proposed by Madias et al.19 These authors suggested that the cardiac apex is responsible for the truly positive electrocardiographic changes in cases of global ischemia, like the one presented here. They proposed that the apical myocardial wall segment, which is also ischemic and able to generate ST segment deviations, is not cancelled by any vector coming from a muscular structure as there is not really a myocardial segment opposite to the apex that could generate ischemic ST vectors cancelling the apical one. This issue might be perhaps overcome with the use of dipyridamole Tl-201 gated myocardial perfusion imaging in order to detect the presence of stunting myocardium by wall motion abnormalities induced by ischemia, as proposed by some authors.27,28
Conclusions
The presence of false negative nuclear stress test in the settings of positive electrocardiographic changes is a very unusual phenomenon and is usually secondary to balanced ischemia of the myocardial segments evaluated by SPECT-TL. This is perhaps explained by a process in which the ischemic apical segment is spared from electrocardigraphic vectors cancelling the ST segment changes. Patients undergoing stress tests with these characteristics should undergo careful evaluation and a high level of suspicion should be adopted for further diagnostic assessment of coronary artery disease.
References
- 1.Marzullo P, et al. Imaging of myocardial viability: a head-to-head comparison among nuclear, echocardiographic, and angiographic techniques. Am J Card Imaging. 1993;7:143–51. [PubMed] [Google Scholar]
- 2.Fleischmann KE, et al. Exercise echocardiography or exercise SPECT imaging? A meta-analysis of diagnostic test performance. JAMA. 1998;280:913–20. doi: 10.1001/jama.280.10.913. [DOI] [PubMed] [Google Scholar]
- 3.Fujimoto S, et al. Study of the predictors and lesion characteristics of ischemic heart disease patients with false negative results in stress myocardial perfusion single-photon emission tomography. Circ J. 2006;70:297–303. doi: 10.1253/circj.70.297. [DOI] [PubMed] [Google Scholar]
- 4.Smits P, et al. False-negative dipyridamolethallium-201 myocardial imaging after caffeine infusion. J Nucl Med. 1991;32:1538–41. [PubMed] [Google Scholar]
- 5.Hofman MS, et al. False-negative myocardial perfusion scintigraphy possibly as a result of administration of low-molecular-weight heparin. Clin Nucl Med. 2007;32:70–2. doi: 10.1097/01.rlu.0000249403.93884.93. [DOI] [PubMed] [Google Scholar]
- 6.Gulati M, et al. Prognostic value of the duke treadmill score in asymptomatic women. Am J Cardiol. 2005;96:369–75. doi: 10.1016/j.amjcard.2005.03.078. [DOI] [PubMed] [Google Scholar]
- 7.Ho KT, et al. Long-term prognostic value of Duke treadmill score and exercise thallium-201 imaging performed one to three years after percutaneous transluminal coronary angioplasty. Am J Cardiol. 1999;84:1323–7. doi: 10.1016/s0002-9149(99)00565-2. [DOI] [PubMed] [Google Scholar]
- 8.Mark DB, et al. Exercise treadmill score for predicting prognosis in coronary artery disease. Ann Intern Med. 1987;106:793–800. doi: 10.7326/0003-4819-106-6-793. [DOI] [PubMed] [Google Scholar]
- 9.Detrano R, et al. Exercise-induced ST segment depression in the diagnosis of multi-vessel coronary disease: a meta analysis. J Am Coll Cardiol. 1989;14:1501–8. doi: 10.1016/0735-1097(89)90388-4. [DOI] [PubMed] [Google Scholar]
- 10.Gianrossi R, et al. Exercise-induced ST depression in the diagnosis of coronary artery disease. A meta-analysis. Circulation. 1989;80:87–98. doi: 10.1161/01.cir.80.1.87. [DOI] [PubMed] [Google Scholar]
- 11.Garber AM, Solomon NA. Cost-effectiveness of alternative test strategies for the diagnosis of coronary artery disease. Ann Intern Med. 1999;130:719–28. doi: 10.7326/0003-4819-130-9-199905040-00003. [DOI] [PubMed] [Google Scholar]
- 12.Nagashima J, et al. [Evaluation of thallium-201 myocardial emission computed tomography based on a comparison with postmortem findings] Radioisotopes. 1986;35:631–5. doi: 10.3769/radioisotopes.35.12_631. [DOI] [PubMed] [Google Scholar]
- 13.Madias JE, Mahjoub M, Valance J. The paradox of negative exercise stress ECG/positive thallium scintigram. Ischemic ST-segment counterpoise as the underlying mechanism. J Electrocardiol. 1996;29:243–8. doi: 10.1016/s0022-0736(96)80087-2. [DOI] [PubMed] [Google Scholar]
- 14.Ahmadpour H, et al. Thallium 201 exercise scintigraphy for detection of multivessel coronary artery disease after transmural myocardial infarction. J Natl Med Assoc. 1984;76:1193–200. [PMC free article] [PubMed] [Google Scholar]
- 15.Hakki AH, et al. Implications of normal exercise electrocardiographic results in patients with angiographically documented coronary artery disease. Correlation with left ventricular function and myocardial perfusion. Am J Med. 1983;75:439–44. doi: 10.1016/0002-9343(83)90345-5. [DOI] [PubMed] [Google Scholar]
- 16.Verzijlbergen JF, et al. Inadequate exercise leads to suboptimal imaging. Thallium-201 myocardial perfusion imaging after dipyridamole combined with low-level exercise unmasks ischemia in symptomatic patients with non-diagnostic thallium-201 scans who exercise submaximally. J Nucl Med. 1991;32:2071–8. [PubMed] [Google Scholar]
- 17.Gibbons RJ, et al. ACC/AHA 2002 guideline update for exercise testing: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines) Circulation. 2002;106:1883–92. doi: 10.1161/01.cir.0000034670.06526.15. [DOI] [PubMed] [Google Scholar]
- 18.Madias JE. Falsely negative thallium-201 scintigram associated with truly positive exercise electrocardiogram: the case of the globally balanced myocardial ischemia. Cardiology. 2006;105:22–4. doi: 10.1159/000088292. [DOI] [PubMed] [Google Scholar]
- 19.Madias JE, Knez P, Win MT. True-positive exercise electrocardiogram/false-negative thallium-201 scintigram: a proposal of a mechanism for the paradox. Clin Cardiol. 2000;23:625–9. doi: 10.1002/clc.4960230815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lesser JR, et al. Balanced myocardial ischaemia: a case of “normal” stress Tc99 sestamibi scan and diagnosis. Heart. 2005;91:e53–e53. doi: 10.1136/hrt.2004.049916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Svane B, Bone D, Holmgren A. Coronary angiography and thallium-201 single photon emission computed tomography in multiple vessel coronary artery disease. Acta Radiol. 1990;31:325–32. [PubMed] [Google Scholar]
- 22.Takehana K, et al. Clinical significance of ischemic electrocardiographic changes during stress myocardial perfusion imaging: sub-analysis of the J-ACCESS study. Ann Nucl Med. 2010;24:215–24. doi: 10.1007/s12149-010-0346-1. [DOI] [PubMed] [Google Scholar]
- 23.Aarnoudse WH, Botman KJ, Pijls NH. False-negative myocardial scintigraphy in balanced three-vessel disease, revealed by coronary pressure measurement. Int J Cardiovasc Intervent. 2003;5:67–71. doi: 10.1080/14628840310003244. [DOI] [PubMed] [Google Scholar]
- 24.Sharir T, et al. Identification of severe and extensive coronary artery disease by postexercise regional wall motion abnormalities in Tc-99m sestamibi gated single-photon emission computed tomography. Am J Cardiol. 2000;86:1171–5. doi: 10.1016/s0002-9149(00)01206-6. [DOI] [PubMed] [Google Scholar]
- 25.Hage FG, Heo J, Iskandrian AE. Adenosine-induced ST segment depression with normal perfusion. Cardiol J. 2009;16:121–6. [PubMed] [Google Scholar]
- 26.Colby J, et al. Hemodynamic, angiographic and scintigraphic correlates of positive exercise electrocardiograms: emphasis on strongly positive exercise electrocardiograms. J Am Coll Cardiol. 1983;2:21–9. doi: 10.1016/s0735-1097(83)80372-6. [DOI] [PubMed] [Google Scholar]
- 27.Hung GU, Chen CP, Yang KT. Incremental value of ischemic stunning on the detection of severe and extensive coronary artery disease in dipyridamole Tl-201 gated myocardial perfusion imaging. Int J Cardiol. 2005;105:108–10. doi: 10.1016/j.ijcard.2004.11.018. [DOI] [PubMed] [Google Scholar]
- 28.Kumar SP, Movahed A. Importance of wall motion analysis in the diagnosis of left main disease using stress nuclear myocardial perfusion imaging. Int J Cardiovasc Imaging. 2003;19:219–24. doi: 10.1023/a:1023606223940. [DOI] [PubMed] [Google Scholar]