Abstract
Gastrointestinal stromal tumors (GISTs) are known to be poorly responsive to conventional chemotherapy and historically considered resistant to radiotherapy. In the past the mainstay of GIST treatment was surgery, but the introduction of tyrosine kinase inhibitors (TKIs) imatinib and sunitinib marked the beginning of a new era in the treatment of GIST patients. To date, radiotherapy for GIST has not been administered in clinical practice except for limited palliative settings and there are no clear data on the administration of radiotherapy, alone or in combination with TKIs, with a purely cytoreductive intent. We describe the clinical case of a 48-year-old woman with metastatic GIST treated with external radiotherapy in a critical supraclavicular tumor localization progressively increasing in size with several symptoms and not responsive to systemic TKI therapies. We obtained an initial shrinkage of the mass and subsequent stabilization with an immediate and clear clinical benefit. Although the historical medical literature considered GISTs resistant to radiation therapy, our clinical case suggests this treatment may be appropriate in selected patients.
Key words: gastrointestinal stromal tumors, radiotherapy.
Introduction
Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal tumors of the gastrointestinal tract. They originate from the intestinal cell of Cajal, an intestinal pacemaker cell, and are usually characterized by specific abnormalities of the KIT and PDGFR-alpha (PGDFRA) receptors that represent the main oncogenic events and prime therapeutic targets.1–2
Tumor resection is the treatment of choice for localized disease. The risk of recurrence is identified evaluating the tumor mitotic index, size and site of origin.3 Although previously considered refractory to any treatment, GIST patients may now benefit from tyrosine kinase inhibitors imatinib and sunitinib that have revolutionized the natural history of these neoplasms.4–5 Other molecules have also been tested and new therapeutic agents are still under evaluation in these tumors.6–7
In the pre-imatinib era, conventional chemotherapic agents tested in GISTs showed very poor results.8 Moreover the impact of radiotherapy on GIST outcome is still unknown. GISTs are generally considered resistant to radiotherapy so this treatment does not play a prominent role in tumor management except in limited palliative settings.
Here, we describe the case of a 48-year-old woman with a complex history of multi-metastatic gastrointestinal stromal tumor since 2004 who developed a progressively increasing mass causing worsening symptoms and was successfully treated by radiotherapy.
Case Report
In September 2004 a 48-year-old woman underwent surgical resection of a uterine fibroma. In the course of the procedure, a large mass was detected in the ileum and resected. During abdominal cavity exploration many peritoneal nodules were found but they were not sampled or removed.The histology report specified gastrointestinal stromal tumor (GIST) of the ileum (maximum diameter: 18 cm, mitotic index: >10/50 HPF). Tumor genotyping with sequencing for mutations in KIT (exons 9, 11, 13 and 17) and PDGFRA (exon 18) disclosed a deletion c.1657-1674del (p.Tyr553_Lys558 del.) at exon 11 of the KIT gene. Treatment with imatinib 400 mg was then started with a good radiological response so the patient underwent a new surgical intervention and all the peritoneal localizations of GIST were resected (R0) 6 months after starting imatinib. Immunohistochemistry confirmed the diagnosis of GIST for all peritoneal nodules. Treatment with imatinib was continued and the patient was followed with periodic CT scans until October 2007 when a retroperitoneal mass of about 8 cm was detected. In November 2007 she underwent a third surgical intervention that was referred as complete resection of the retroperitoneal mass, positive for GIST with a high mitotic index (>10/50 HPF). In January 2008 the patient was referred to our institution. Considering the two relapses during imatinib treatment and the absence of signs of histological response to therapy, we increased the imatinib dose to 800 mg/day.
Unfortunately a new CT scan in July 2008 documented another peritoneal relapse so she started a second line treatment with sunitinib. No response to therapy was obtained. The patient was also enrolled in a clinical trial with nilotinib for 4 months and then she was treated with sorafenib off label but even these new agents failed to yield a clear benefit.
During the history of her disease, a CT scan disclosed a left supraclavicular mass of 14 mm suspected for GIST localization that progressively increased to 56 mm when it became deeply symptomatic with local pain and initial dysphagia (Figure 1A). Radiological imaging showed a mild compression of the jugular vein without a clear separating plane between the mass and the trachea. Because of symptoms development, a rapid increase in the size of the mass in 5 months and the lack of surgical options, we administered external beam radiotherapy combined with sorafenib at a dose of 400 mg/bid starting in October 2010. Cytoreductive radiation therapy was given at a fraction of 25×200 cGy with a total dose of 5000 cGy. The treatment was well-tolerated and the patient referred an early benefit from radiotherapy with a marked improvement of pain and a resolution of the dysphagia. The CT scan performed after the end of the radiotherapy showed a decrease in size of the supraclavicular mass from 56×39 mm to 44×31 mm (Figure 1B). Despite a systemic progression of disease, the radio-treated mass remained stable at the following radiological controls and she has had no further symptoms at this site.
Figure 1.
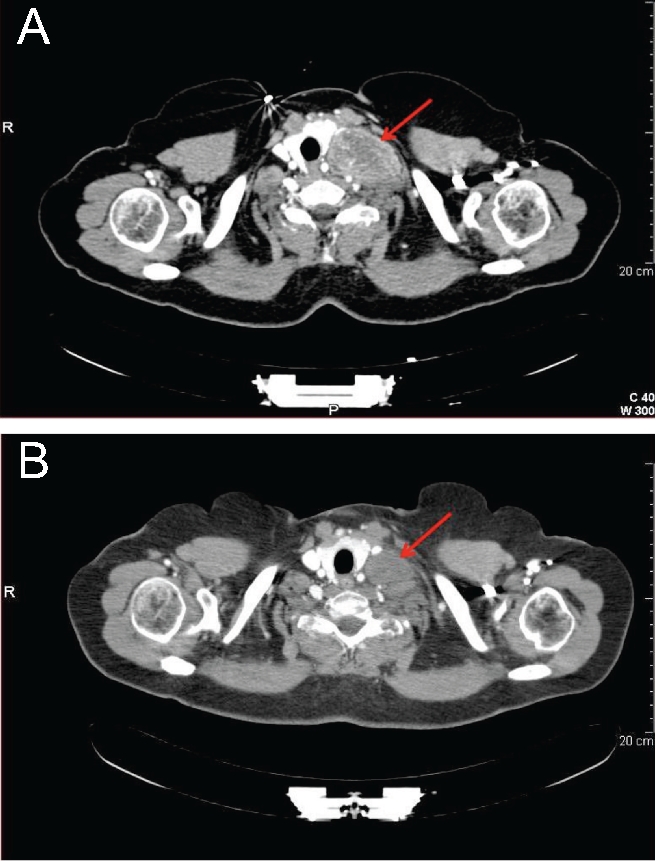
(A) Supraclavicular localization of GIST before radiotherapy. (B) Supraclavicular localization of GIST after radiotherapy
Discussion
We described a case of an unusual metastatic localization of GIST not responsive to systemic treatments and successfully controlled by external beam radiotherapy.
The advent of tyrosine kinase inhibitors has revolutionized the treatment of GIST clearly marking two periods in the history of these tumors: the pre- and the post- imatinib era. So, the main treatments of GIST are surgery, in case of localized disease and responding metastatic lesions, and medical therapies with TKIs inhibitors for not resectable and metastatic GISTs. Conventional treatments like chemotherapy and radiotherapy were quickly outclassed by target therapies due to the huge differences in their efficacy.8
Radiation therapy was historically considered to have minimal activity in these tumors. The main reason for the scant use of radiation therapy in GIST is that the pattern of metastasis in the liver and peritoneum involves fields too large to be amenable to radiation therapy.9 In 2002, Dematteo et al. reported that radiotherapy may have some role in the palliation of patients with bleeding from peritoneal recurrence or with painful disease localizations.8 Literature reports on radiation therapy in GISTs are limited to palliation of bone metastases, often in association with biphosphonates.10–11
In fact, radiotherapy in the management of GIST patients is currently restricted to symptomatic palliation and has not clearly been investigated with a purely cytoreductive intent.8,10–11 In 2001 Shioyama et al.12 described a case of a retroperitoneal GIST treated with primary radiotherapy (5100 cGy) but also with arterial chemotherapy and immunotherapy (OK432). No change in tumor size was reported on early computed tomography whereas CT scan at long-term follow-up revealed a marked decrease of tumor size. The only recent experience of radiotherapy in association with imatinib with a potentially curative intent was described by Ciresa et al.13 in a patient with GIST of the rectum who obtained a complete pathological response. To our knowledge, no data are available on radiotherapy in esophageal GISTs.
In the adjuvant setting, Pollock et al. reported on a case of adjuvant postoperative radiotherapy in a rectal GIST treated by incomplete surgical resection.14 They performed radiation therapy due to the risk of local recurrence after a subtotal resection. The patient was reported to be disease-free two years after the end of postoperative radiotherapy.
The clinical case described herein shows that radiotherapy may have a role as a cytoreductive therapy in GISTs. We adopted this unusual approach in this particular site due to the onset of worsening symptoms and lack of therapeutic options in a progressive disease. The patient gained an early benefit from radiotherapy but the most impressive outcome was that the supraclavicular localization that had progressively increased before radiotherapy resulted decreased at the first CT scan after radiation treatment and this response has been maintained to date. We now suggest that radiotherapy should be considered as a treatment to obtain a cytoreductive effect or disease control in selected cases especially when systemic treatments are ineffective as in our GIST patient. The possibility of obtaining tumor shrinkage or disease stabilization by radiotherapy alone or in combination with TKIs could open new perspectives in the treatment of this neoplasm. While radiation therapy in soft tissue sarcomas is highly reported, its role in GIST management merits extensive investigation. Future research may well abolish the old concept of GISTs as not sensitive to radiation therapy.
References
- 1.Hirota S, Isozaki K, Moriyama Y, et al. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science. 1998;279:577–80. doi: 10.1126/science.279.5350.577. [DOI] [PubMed] [Google Scholar]
- 2.Corless CL, Fletcher JA, Heinrich MC. Biology of gastrointestinal stromal tumors. J Clin oncol. 2004;22:3813–25. doi: 10.1200/JCO.2004.05.140. [DOI] [PubMed] [Google Scholar]
- 3.Miettinen M, Lasota J. Gastrointestinal stromal tumors: pathology and prognosis at different sites. Semin Diagn Pathol. 2006;23:70–83. doi: 10.1053/j.semdp.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 4.Demetri GD, von Mehren M, Blanke CD, et al. Efficacy and safety of imatinib mesylate in advanced gastrointestinal stromal tumors. N Engl J Med. 2002;347:472–80. doi: 10.1056/NEJMoa020461. [DOI] [PubMed] [Google Scholar]
- 5.Demetri GD, van Oosterom AT, Garrett CR, et al. Efficacy and safety of sunitinib in patients with advanced gastrointestinal stromal tumour after failure of imatinib: a randomised controlled trial. Lancet. 2006;368:1329–38. doi: 10.1016/S0140-6736(06)69446-4. [DOI] [PubMed] [Google Scholar]
- 6.Reichardt P. Novel approaches to imatinib- and sunitinib-resistant GIST. Curr Oncol Rep. 2008;10:344–9. doi: 10.1007/s11912-008-0053-4. [DOI] [PubMed] [Google Scholar]
- 7.Reichardt P, Reichardt A, Pink D. Molecular targeted therapy of gastrointestinal stromal tumors. Curr Cancer Drug Targets. 2011;11:688–97. doi: 10.2174/156800911796191042. [DOI] [PubMed] [Google Scholar]
- 8.Dematteo RP, Heinrich MC, El-Rifai WM, et al. Clinical management of gastrointestinal stromal tumors: before and after STI-571. Hum Pathol. 2002;33:466–77. doi: 10.1053/hupa.2002.124122. [DOI] [PubMed] [Google Scholar]
- 9.D'Amato G, Steinert DM, McAuliffe JC, et al. Update on the biology and therapy of gastrointestinal stromal tumors. Cancer Control. 2005;12:44–56. doi: 10.1177/107327480501200106. [DOI] [PubMed] [Google Scholar]
- 10.Di Scioscio V, Greco L, Pallotti MC, et al. Three cases of bone metastases in patients with gastrointestinal stromal tumors. Rare Tumors. 2011;3:e17–e17. doi: 10.4081/rt.2011.e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tezcan Y, Koç M. Gastrointestinal stromal tumor of the rectum with bone and liver metastasis: a case study. Med Oncol. 2010 Oct 17; doi: 10.1007/s12032-010-9697-7. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 12.Shioyama Y, Yakeishi Y, Watanabe T, et al. Long-term control for a retroperitoneal metastasis of malignant gastrointestinal stromal tumor after chemoradiotherapy and immunotherapy. Acta Oncol. 2001;40:102–4. doi: 10.1080/028418601750071154. [DOI] [PubMed] [Google Scholar]
- 13.Ciresa M, D'Angelillo RM, Ramella S, et al. Molecularly targeted therapy and radio-therapy in the management of localized gastrointestinal stromal tumor (GIST) of the rectum: a case report. Tumori. 2009;95:236–9. doi: 10.1177/030089160909500217. [DOI] [PubMed] [Google Scholar]
- 14.Pollock J, Morgan D, Denobile J, et al. Adjuvant radiotherapy for gastrointestinal stromal tumor of the rectum. Dig Dis Sci. 2001;46:268–72. doi: 10.1023/a:1005581000712. [DOI] [PubMed] [Google Scholar]


