Abstract
Catecholamine signaling pathways in the peripheral and central nervous systems (PNS, CNS, respectively) utilize catechol-O-methyltransferase (COMT) as a major regulatory enzyme responsible for deactivation of dopamine (DA), norepinephrine (NE) and epinephrine (E). Accordingly, homeostasis of COMT gene expression is hypothesized to be functionally linked to regulation of autonomic control of normotensive vascular events. Recently, we demonstrated that morphine administration in vitro resulted in decreased cellular concentrations of COMT-encoding mRNA levels, as compared to control values. In contrast, cells treated with E up regulated their COMT gene expression. In sum, these observations indicate a potential reciprocal linkage between end product inhibition of COMT gene expression by E and morphine. Interestingly, the observed effects of administered E on COMT gene expression suggest an enhancement of its own catabolism or, reciprocally, a stimulation morphine biosynthesis.
Keywords: endogenous morphine, catecholamines, epinephrine, catechol-O-methyltransferase
A “morphinergic” signaling pathway in endothelial cells
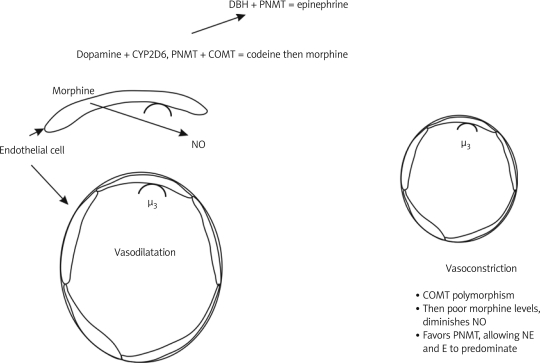
We have recently demonstrated a functional regulatory pathway in vascular endothelial cells driven by endogenous, chemically authentic, morphine, its cognate opiate alkaloid-selective µ3 and µ4 receptors and constitutive nitric oxide (NO) production and release [1–5]. Because NO/cyclic guanosine monophosphate (cGMP) signaling events have been well established as potent regulators of vasodilatation, it appears likely that populations of endothelial cells are also entrained as physiological regulators of normal vascular tone. Accordingly, µ3 and µ4 opiate receptors may represent important potential therapeutic targets for restoring normotensive vascular tone in hypertensive syndromes [1–5].
The presence of chemically authentic morphine has been demonstrated in vascular endothelial cells obtained from human atria [5] and human white blood cells (WBC), which also express µ3 and µ4 opiate receptors [1, 6], and several human cancer cell lines [1, 2, 5, 7, 8]. We have therefore hypothesized that µ3 and µ4 opiate receptors coupled to constitutive NO expression are tonically activated by low levels of endogenously expressed, chemically authentic morphine [5], a contention that is consistent with the presence of low levels of circulating morphine in human plasma [9–11]. Provocatively, we have also characterized a functionally competent µ3/µ4 receptor/NO-coupled regulatory pathway in human multilineage progenitor cells (MLPC) [12], thereby suggesting a fundamental role of morphine/NO-coupled developmental processes.
One of the key physiological roles of the “morphinergic”/NO-coupled regulatory pathway appears to be the homeostatic maintenance of normal vascular tone, which can only be achieved by intimate association of the vascular endothelium with circulating leukocytes. Endogenous morphine derived from defined cellular sources and circulating in plasma appears to provide an important caretaker role in promoting coordinated, on demand, vasomotor responsiveness, to diverse physiological stimuli.
Shared “morphinergic”/catecholamine biosynthetic enzymes
Based on recent elucidations of key functional components of “morphinergic” signaling pathways, it is likely that variations in gene expression of key enzymes of the morphine biosynthetic pathway may have profound effects on human health, especially in immune and vascular tissues [13]. Furthermore, the establishment of dopamine (DA) as a requisite intermediate precursor molecule in the morphine biosynthetic pathway suggest that perturbations of these biosynthetic enzymes will significantly effect human behavioral responses to cognitive and physiological stressors [13–18].
Previously published studies have established catechol-O-methyltransferase (COMT) as a key player in the morphine biosynthetic pathway responsible for enzymatic conversion of tetrahydropapveroline (THP) to the methylated intermediate precursor molecule (S)-reticuline [13, 16, 19]. Additionally, polymorphisms in other genes involved in “morphinergic” and catecholamine metabolic pathways, including tyrosine hydroxylase, DOPA decarboxylase, dopamine β-hydroxylase, and monoamine oxidase have not been as well studied as COMT in terms of their effects on human health [14–18, 20–25]. The most studied COMT polymorphism is termed val/met 158. This polymorphism has a methionine substituted for a valine at amino acid 158 [26]. Ongoing studies are attempting to establish a link between this polymorphism and behavior [27]. The effect of this polymorphism is a lowering of the activity of COMT and thus a slower metabolism of DA [26, 28].
Figure 1.
Human vascular endothelial cells contain the µ3/µ4 opiate receptor subtype coupled to NO release, leading to vasodilatation. Furthermore, vascular endothelial cells appear to express endogenous morphine, indicating an autonomous autocrine/paracrine signaling pathway. Well established polymorphisms of the COMT gene are predicted to result in significant alterations in morphine biosynthesis (discussed above). Alterations of COMT enzyme activity will effectively result in diminished cellular concentrations of endogenous morphine with coordinate reductions of NO signaling events, a compounded endpoint promoting enhanced vasoconstriction. Second, alterations of COMT enzyme activity will effectively diminish catecholamine metabolism, with resultant enhancement of NE and E pressor activity via α-adrenergic receptor activation
Recently we examined the effect of morphine exposure on COMT gene expression in cancer cells [29, 30]. Morphine administration was observed to decrease cellular concentrations of COMT-encoding mRNA in a time-dependent manner, thereby suggesting a negative feedback regulatory process. Interestingly, administration of E at 10–9M to colonicadenocarcinoma cells at for 24 h was observed to produce a 1.6 fold increase in levels of COMT-encoding mRNA [30]. In sum, these observations indicated a potential reciprocal linkage between end product inhibition of COMT gene expression by E and morphine. Interestingly, the observed effects of administered E on COMT gene expression suggest an enhancement of its own catabolism or, reciprocally, a stimulation morphine biosynthesis.
Dopamine is a requisite intermediate precursor molecule in the morphine biosynthetic pathway [13, 19, 31]. The intimate and interactive coupling of “morphinergic” to dopaminergic behavioral processes provide a cogent window of understanding additive behavioral processes. For example, initial speculation as to the existence and potential physiological role of endogenous morphine were made over 30 years ago by prominent researchers in the field of alcohol abuse, not opiate abuse, who advanced the hypothesis that the reinforcing or additive effects of ethanol were functionally linked to the cellular effects of DA derived isoquinoline alkaloids, notably the tetrahydroisoquinoline salsolinol [32–34] and the benzylisoquinoline morphine precursor tetrahydropapaveroline (THP) [35–37]. Recognition of tetrahydroisoquinolines, THP, and endogenous morphine as active principles of alcohol abuse was inherently linked to their normal presence in dopaminergic neurons, enhanced cellular expression following chronic ethanol intake [37–42], and concentration-dependent disregulation of DA metabolism and/or dopaminergic signaling in mesolimbic/mesocortical areas such as the nucleus accumbens and the ventral tegmental area traditionally associated with reward and reinforcement of ethanol intake [15, 16, 43–51]. The causal relationship and functional association of CNS expression of tetrahydroisoquinoline and benzylisoquinoline alkaloids to alcohol abuse remains controversial despite anatomical, physiological, pharmacological, and behavioral evidence linking dopaminergic and opioidergic systems in limbic areas associated with reinforcement of ethanol intake behaviors [17, 21, 52–56].
This link is equally important when considering animal behavior. It can be surmised that the DA component modulates excitatory states, including rage, whereas the morphinergic component offers calming action associated with relaxation and reward. This association may also explain the calming effect following excitatory emotional states. Moreover, in this scenario of DA synthesis coming before that of morphine one would predict excitation would precede the calm, which may be associated with morphine signaling. Furthermore, this coupling may also explain the fact that within various relaxation techniques an excitatory stress component emerges physiologically before relaxation sets in [21–23, 48, 57]. The link between catecholamine and morphine metabolism promises to be the subject of future investigations given its significance in biomedicine. This link is critical in offering a novel explanation for idiopathic hypertension via identification of physiological deficits in vascular endothelial “morphinergic”/NO/catecholamine-coupled signaling events. Investigation of the potential involvement of COMT and its genetic polymorphisms in metabolic/pathophysiological states represents an area for intense biomedical research advancement.
References
- 1.Cadet P, Mantione KJ, Stefano GB. Molecular identification and functional expression of mu3, a novel alternatively spliced variant of the human mu opiate receptor gene. J Immunol. 2003;170:5118–23. doi: 10.4049/jimmunol.170.10.5118. [DOI] [PubMed] [Google Scholar]
- 2.Zhu W, Cadet P, Baggerman G, Mantione KJ, Stefano GB. Human white blood cells synthesize morphine: CYP2D6 modulation. J Immunol. 2005;175:7357–62. doi: 10.4049/jimmunol.175.11.7357. [DOI] [PubMed] [Google Scholar]
- 3.Stefano GB, Hartman A, Bilfinger TV, et al. Presence of the mu3 opiate receptor in endothelial cells: coupling to nitric oxide production and vasodilation. J Biol Chem. 1995;270:30290–3. doi: 10.1074/jbc.270.51.30290. [DOI] [PubMed] [Google Scholar]
- 4.Cadet P, Bilfinger TV, Fimiani C, Peter D, Stefano GB. Human vascular and cardiac endothelia express mu opiate receptor transcripts. Endothelium. 2000;7:185–91. doi: 10.3109/10623320009165316. [DOI] [PubMed] [Google Scholar]
- 5.Zhu W, Bilfinger TV, Baggerman G, Goumon Y, Stefano GB. Presence of endogenous morphine and morphine 6 glucuronide in human heart tissue. Int J Mol Med. 2001;7:419–22. [PubMed] [Google Scholar]
- 6.Cadet P, Mantione K, Bilfinger TV, Stefano GB. Real-time RT-PCR measurement of the modulation of Mu opiate receptor expression by nitric oxide in human mononuclear cells. Med Sci Monit. 2001;7:1123–8. [PubMed] [Google Scholar]
- 7.Boettcher C, Fellermeier M, Boettcher C, Drager B, Zenk MH. How human neuroblastoma cells make morphine. Proc Natl Acad Sci U S A. 2005;102:8495–500. doi: 10.1073/pnas.0503244102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Poeaknapo C, Schmidt J, Brandsch M, Dräger B, Zenk MH. Endogenous formation of morphine in human cells. Proc Nat Acad Sci U S A. 2004;101:14091–6. doi: 10.1073/pnas.0405430101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brix-Christensen V, Tonnesen E, Sanchez RG, Bilfinger TV, Stefano GB. Endogenous morphine levels increase following cardiac surgery as part of the antiinflammatory response? Int J Cardiol. 1997;62:191–7. doi: 10.1016/s0167-5273(97)00229-5. [DOI] [PubMed] [Google Scholar]
- 10.Liu Y, Bilfinger TV, Stefano GB. A rapid and sensitive quantitation method of endogenous morphine in human plasma. Life Sci. 1996;60:237–43. doi: 10.1016/s0024-3205(97)89478-7. [DOI] [PubMed] [Google Scholar]
- 11.Bilfinger TV, Kushnerik V, Bundz S, Liu Y, Stefano GB. Evidence for morphine downregulating immunocytes during cardiopulmonary bypass in a porcine model. Int J Cardiol. 1996;53:S39–46. doi: 10.1016/0167-5273(96)02574-0. [DOI] [PubMed] [Google Scholar]
- 12.Cadet P, Mantione KJ, Zhu W, Kream RM, Sheehan M, Stefano GB. A functionally coupled mu3-like opiate receptor/nitric oxide regulatory pathway in human multi-lineage progenitor cells. J Immunol. 2007;179:5839–44. doi: 10.4049/jimmunol.179.9.5839. [DOI] [PubMed] [Google Scholar]
- 13.Kream RM, Stefano GB. De novo biosynthesis of morphine in animal cells: an evidence-based model. Med Sci Monit. 2006;12:RA207–19. [PubMed] [Google Scholar]
- 14.Fricchione G, Zhu W, Cadet P, et al. Identification of endogenous morphine and a mu3-like opiate alkaloid receptor in human brain tissue taken from a patient with intractable complex partial epilepsy. Med Sci Monit. 2008;14:CS45–9. [PubMed] [Google Scholar]
- 15.Kream RM, Stefano GB. Homeopathic ethanol. Med Sci Monit. 2008;14:SC11–3. [PubMed] [Google Scholar]
- 16.Mantione KJ, Cadet P, Zhu W, et al. Endogenous morphine signaling via nitric oxide regulates the expression of CYP2D6 and COMT: autocrine/paracrine feedback inhibition. Addict Biol. 2008;13:118–23. doi: 10.1111/j.1369-1600.2007.00072.x. [DOI] [PubMed] [Google Scholar]
- 17.Stefano GB, Stefano JM, Esch T. Anticipatory stress response: a significant commonality in stress, relaxation, pleasure and love responses. Med Sci Monit. 2008;14:RA17–21. [PubMed] [Google Scholar]
- 18.Zhu W, Esch T, Kream RM, Stefano GB. Converging cellular processes for substances of abuse: endogenous morphine. Neuro Endocrinol Lett. 2008;29:63–6. [PubMed] [Google Scholar]
- 19.Stefano GB, Kream RM. Endogenous morphine synthetic pathway preceded and gave rise to catecholamine synthesis in evolution. Int J Mol Med. 2007;20:837–41. [PubMed] [Google Scholar]
- 20.Haavik J, Blau N, Thony B. Mutations in human monoamine-related neurotransmitter pathway genes. Hum Mutat. 2008;29:891–902. doi: 10.1002/humu.20700. [DOI] [PubMed] [Google Scholar]
- 21.Kream RM, Stefano GB. Endogenous morphine and nitric oxide coupled regulation of mitochondrial processes. Med Sci Monit. 2009;15:RA263–8. [PubMed] [Google Scholar]
- 22.Stefano GB, Esch T, Kream RM. Xenobiotic perturbation of endogenous morphine signaling: paradoxical opiate hyperalgesia. Med Sci Monit. 2009;15:RA107–10. [PubMed] [Google Scholar]
- 23.Stefano GB, Kream RM, Esch T. Revisiting tolerance from the endogenous morphine perspective. Med Sci Monit. 2009;15:RA189–98. [PubMed] [Google Scholar]
- 24.Zhu W, Stefano GB. Comparative aspects of endogenous morphine synthesis and signaling in animals. Ann N Y Acad Sci. 2009;1163:330–9. doi: 10.1111/j.1749-6632.2008.03623.x. [DOI] [PubMed] [Google Scholar]
- 25.Gu Y, Yun L, Tian Y, Hu Z. Association between COMT gene and Chinese male schizophrenic patients with violent behavior. Med Sci Monit. 2009;15:CR484–9. [PubMed] [Google Scholar]
- 26.Syvanen AC, Tilgmann C, Rinne J, Ulmanen I. Genetic polymorphism of catechol-O-methyltransferase (COMT): correlation of genotype with individual variation of S-COMT activity and comparison of the allele frequencies in the normal population and parkinsonian patients in Finland. Pharmacogenetics. 1997;7:65–71. doi: 10.1097/00008571-199702000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Lachman HM. Does COMT val158met affect behavioral phenotypes: yes, no, maybe? Neuropsychopharmacology. 2008;33:3027–9. doi: 10.1038/npp.2008.189. [DOI] [PubMed] [Google Scholar]
- 28.Kunugi H, Nanko S, Ueki A, et al. High and low activity alleles of catechol-O-methyltransferase gene: ethnic difference and possible association with Parkinson's disease. Neurosci Lett. 1997;221:202–4. doi: 10.1016/s0304-3940(96)13289-4. [DOI] [PubMed] [Google Scholar]
- 29.Mantione K, Kream RM, Stefano GB. Variations in critical morphine biosynthesis genes and their potential to influence human health. Neuro Endocrinol Lett. 2010;31:9. [PubMed] [Google Scholar]
- 30.Mantione KJ, Zhu W, Kream RM, Esch T, Stefano GB. Regulation of the transcription of the catechol-O-methyltransferase gene by morphine and epinephrine. Activitas Nervosa Superior Rediviva. 2010;52:51–6. [Google Scholar]
- 31.Stefano GB, Bianchi E, Guarna M, et al. Nicotine, alcohol and cocaine coupling to reward processes via endogenous morphine signaling: the dopamine-morphine hypothesis. Med Sci Monit. 2007;13:RA91–102. [PubMed] [Google Scholar]
- 32.Davis VE, Walsh MJ. Alcohol, amines and alkaloids: a possible biochemical basis for alcohol addiction. Science. 1970;167:1005–7. doi: 10.1126/science.167.3920.1005. [DOI] [PubMed] [Google Scholar]
- 33.Davis VE, Walsh MJ, Yamanaka Y. Augmentation of alkaloid formation from dopamine by alcohol and acetaldehyde in vitro. J Pharmacol Exp Ther. 1970;174:401–12. [PubMed] [Google Scholar]
- 34.Yamanaka Y, Walsh MJ, Davis VE. Salsolinol, an alkaloid derivative of dopamine formed in vitro during alcohol metabolism. Nature. 1970;227:1143–4. doi: 10.1038/2271143a0. [DOI] [PubMed] [Google Scholar]
- 35.Halushka PV, Hoffmann PC, Davis VE, Walsh MJ. Alcohol addiction and tetrahydropapaveroline. Science. 1970;169:1104–6. doi: 10.1126/science.169.3950.1104. [DOI] [PubMed] [Google Scholar]
- 36.Walsh MJ, Davis VE, Yamanaka Y. Tetrahydropapaveroline: an alkaloid metabolite of dopamine in vitro. J Pharmacol Exp Ther. 1970;174:388–400. [PubMed] [Google Scholar]
- 37.Weiner H. Relationship between 3,4-dihydroxyphenylacetaldehyde levels and tetrahydropapaveroline formation. Alcohol Clin Exp Res. 1978;2:127–31. doi: 10.1111/j.1530-0277.1978.tb04712.x. [DOI] [PubMed] [Google Scholar]
- 38.Collins MA, Hannigan JJ, Weiner C. Effects of catecholic tetrahydroisoquinolines on endogenous catecholamines. Curr Alcohol. 1979;5:53–9. [PubMed] [Google Scholar]
- 39.Turner AJ, Baker KM, Algeri S, Erigerio A, Garattini S. Tetrahydropapaveroline: formation in vivo and in vitro in rat brain. Life Sci. 1974;14:2247–57. doi: 10.1016/0024-3205(74)90106-4. [DOI] [PubMed] [Google Scholar]
- 40.Weiner H. Possible steady-state concentrations of tetrahydroisoquinolines in brain after the consumption of ethanol. Fed Proc. 1981;40:2082–5. [PubMed] [Google Scholar]
- 41.Zhu W, Mantione K, Kream RM, Stefano GB. Alcohol-, nicotine-, and cocaine-evoked release of morphine from human white blood cells: substances of abuse actions converge on endogenous morphine release. Med Sci Monit. 2006;12:BR350–4. [PubMed] [Google Scholar]
- 42.Zhu W, Mantione KJ, Casares FM, et al. Alcohol-, nicotine, and cocaine-evoked release of morphine from invertebrate ganglia: Model system for screening drugs of abuse. Med Sci Monit. 2006;12:BR155–61. [PubMed] [Google Scholar]
- 43.Clow A, Stolerman IP, Murray RM, Sandler M. Ethanol preference in rats: increased consumption after intraventricular administration of tetrahydropapaveroline. Neuropharmacology. 1983;22:563–5. doi: 10.1016/0028-3908(83)90181-8. [DOI] [PubMed] [Google Scholar]
- 44.Duncan CC, Fernando PW. Effects of tetrahydropapaveroline in the nucleus accumbens and the ventral tegmental area on ethanol preference in the rat. Alcohol. 1991;8:87–90. doi: 10.1016/0741-8329(91)91314-r. [DOI] [PubMed] [Google Scholar]
- 45.Myers RD. Anatomical “circuitry” in the brain mediating alcohol drinking revealed by THP-reactive sites in the limbic system. Alcohol. 1990;7:449–59. doi: 10.1016/0741-8329(90)90031-7. [DOI] [PubMed] [Google Scholar]
- 46.Myers RD, Robinson DE. Tetrahydropapaveroline injected in the ventral tegmental area shifts dopamine efflux differentially in the shell and core of nucleus accumbens in high-ethanol-preferring (HEP) rats. Alcohol. 1999;18:83–90. doi: 10.1016/s0741-8329(99)00008-7. [DOI] [PubMed] [Google Scholar]
- 47.Sallstrom BS, Hill R, Kiianmaa K, Rommelspacher H. Effect of ethanol on (R)- and (S)-salsolinol, salsoline, and THP in the nucleus accumbens of AA and ANA rats. Alcohol. 1999;18:165–9. doi: 10.1016/s0741-8329(98)00080-9. [DOI] [PubMed] [Google Scholar]
- 48.Esch T, Stefano GB. The neurobiology of stress management. Neuro Endocrinol Lett. 2010;31:30. [PubMed] [Google Scholar]
- 49.Neri C, Ghelardini C, Sotak B, et al. Dopamine is necessary to endogenous morphine formation in mammalian brain in vivo. J Neurochem. 2008;106:2337–44. doi: 10.1111/j.1471-4159.2008.05572.x. [DOI] [PubMed] [Google Scholar]
- 50.Roy JR, Chakraborty S, Chakraborty TR. Estrogen-like endocrine disrupting chemicals affecting puberty in humans – a review. Med Sci Monit. 2009;15:RA137–45. [PubMed] [Google Scholar]
- 51.Atmanene C, Laux A, Glattard E, et al. Characterization of human and bovine phosphatidylethanolamine-binding protein (PEBP/RKIP) interactions with morphine and morphine-glucuronides determined by noncovalent mass spectrometry. Med Sci Monit. 2009;15:BR178–87. [PubMed] [Google Scholar]
- 52.Haber H, Roske I, Rottmann M, Georgi M, Melzig MF. Alcohol induces formation of morphine precursors in the striatum of rats. Life Sci. 1997;60:79–89. doi: 10.1016/s0024-3205(96)00597-8. [DOI] [PubMed] [Google Scholar]
- 53.McCoy JG, Strawbridge C, McMurtrey KD, Kane VB, Ward CP. A re-evaluation of the role of tetrahydropapaveroline in ethanol consumption in rats. Brain Res Bull. 2003;60:59–65. doi: 10.1016/s0361-9230(03)00018-2. [DOI] [PubMed] [Google Scholar]
- 54.Naoi M, Maruyama W, Nagy GM. Dopamine-derived salsolinol derivatives as endogenous monoamine oxidase inhibitors: occurrence, metabolism and function in human brains. Neurotoxicology. 2004;25:193–204. doi: 10.1016/S0161-813X(03)00099-8. [DOI] [PubMed] [Google Scholar]
- 55.Shearman GT, Herz A. Ethanol and tetrahydroisoquinoline alkaloids do not produce narcotic discriminative stimulus effects. Psychopharmacology (Berl) 1983;81:224–7. doi: 10.1007/BF00427266. [DOI] [PubMed] [Google Scholar]
- 56.Santamaria F, De SS, Montella S, et al. Nasal nitric oxide assessment in primary ciliary dyskinesia using aspiration, exhalation, and humming. Med Sci Monit. 2008;14:CR80–5. [PubMed] [Google Scholar]
- 57.Stefano GB, Fricchione GL, Slingsby BT, Benson H. The placebo effect and relaxation response: neural processes and their coupling to constitutive nitric oxide. Brain Res Rev. 2001;35:1–19. doi: 10.1016/s0165-0173(00)00047-3. [DOI] [PubMed] [Google Scholar]