Abstract
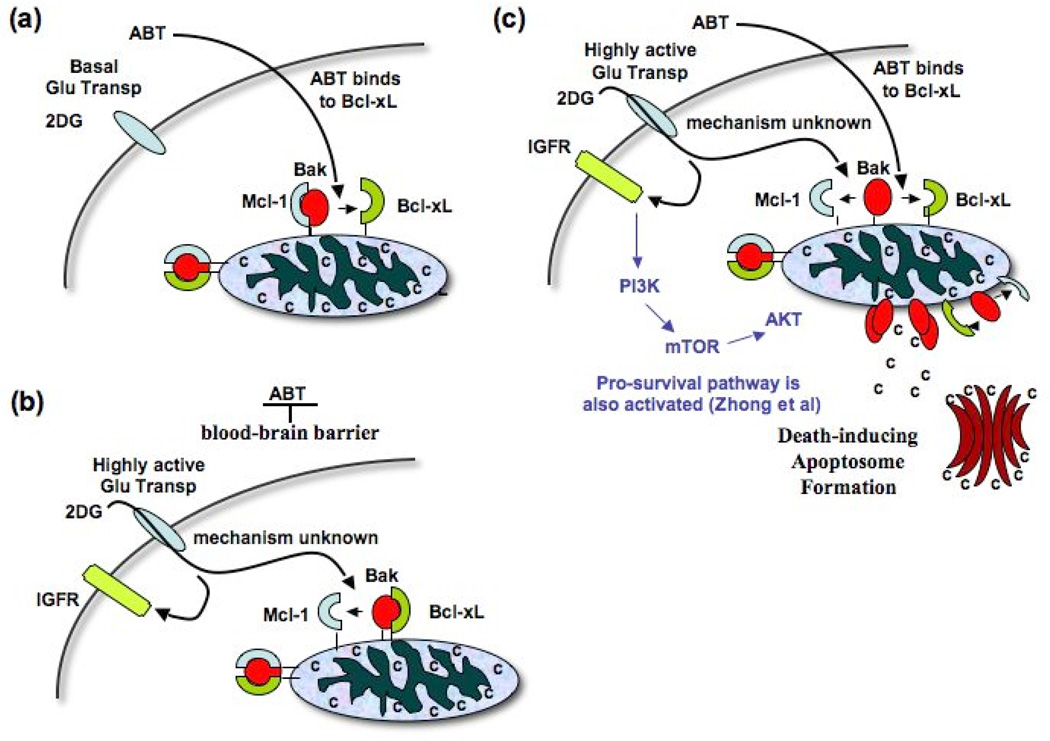
Since each cancer is a heterogeneous mix of cancer cells at different stages of development, we are faced with trying to treat many different diseased cells all at once. An authentic approach is to build a genomic and proteomic profile of a patient, identify the target oncogenes and prescribe the combination of targeted drugs tailored for that patient. However, there are many practical problems with this personalized medicine approach: (1) cancers often generate treatment-resistant phenotypes, (2) the treatment could be enormously expensive, and (3) most of the targeted drugs have not been developed yet. We propose a different approach: therapies that combine 2-deoxyglucose (2DG) with Bcl-2 antagonist such as ABT-263/737 (ABT). Pro-apoptotic protein Bak is normally sequestered by Mcl-1 and Bcl-xL. Only when Bak is released from both Mcl-1 and Bcl-xL, can it induce apoptosis. 2DG can prime highly glycolytic cells by dissociating Bak-Mcl-1 complex. Cells primed by 2DG are some brain cells and most cancer cells. ABT can bind to Bcl-xL, dissociating Bak-Bcl-xL complex, freeing Bak and inducing apoptosis. Since ABT cannot cross blood-brain barrier, only cells exposed to both agents are highly glycolytic cancer cells located outside the brain. Because ABT directly triggers apoptosis at the step very near the terminal point of apoptosis, 2DG-ABT combination therapies are applicable to many types of cancer at all stages of development, with little side effect.
Introduction
Genotoxin-based DNA damaging agents and cell cycle inhibitors cause damage to DNA, activating checkpoints and inducing apoptosis in nearly all of the proliferating cells. Even though severe side effects are associated with these therapies, they are the most effective therapies in early stages of cancer. However, as cancer progresses, cancer cells accumulate more mutations, abrogating checkpoint functions and apoptosis-inducing programs, making them resistant to genotoxin-based treatments. More recently developed “targeted” therapies use drugs that inhibit specific gene or mutated gene products whose activities are important in cancer development and growth in particular types of cancer. Generally they are less toxic, yet their effects can be very dramatic, shrinking tumors within days. However, there are many practical problems with this approach. For example, inactivating one oncogene with its many variants may not be possible with just one targeted drug (1). Moreover, choosing just one oncogene in a complex cancer genome to inactivate and eliminate a heterogeneous population of cancer cells is very difficult and it may not be always possible. Even when the right choice is made, showing dramatic tumor regression initially, there are numerous incidents of cancer returning within a few years, in forms highly resistant to the original therapy (2). To move beyond these limitations, therapies using a combination of targeted drugs are being envisioned as the best approach (2). However, to choose the right combination, the genomic and proteomic profile of each patient’s cancer may be required, raising the cost (see Micael Stratton’s comments in (3)). Furthermore, many of these targeted drugs are not even developed yet, making this personalized medicine approach impractical (3). Lastly, even with the combination of targeted drugs, cancer could still generate treatment-resistant cells by activating an alternate pathway.
We propose a different approach; search for a cancer therapy that is applicable to many cancer types at different stages of development. We believe this can be done by targeting cancer cells with 2DG because they are highly glycolytic (4). Since 2DG also sensitizes cancer cells to Bcl-2 antagonists such as ABT (5), addition of a Bcl-2 antagonist to 2DG-treated cells mechanically activates Bak, circumventing the usual signal transduction cascades required for Bak activation. Thus the combination could selectively induce apoptosis for cells with high glucose transporter activities. Indeed, 2DG-ABT can induce apoptosis in many cancer cell-lines derived from many cancer types. It also eliminated p53 defective, PTEN deleted, highly metastasized cancer cells grafted onto nude mice (5), for which the standard chemotherapies and some targeted therapies had not worked. In this article, the molecular mechanisms of 2DG-ABT combination therapies and possible improvements will also be discussed.
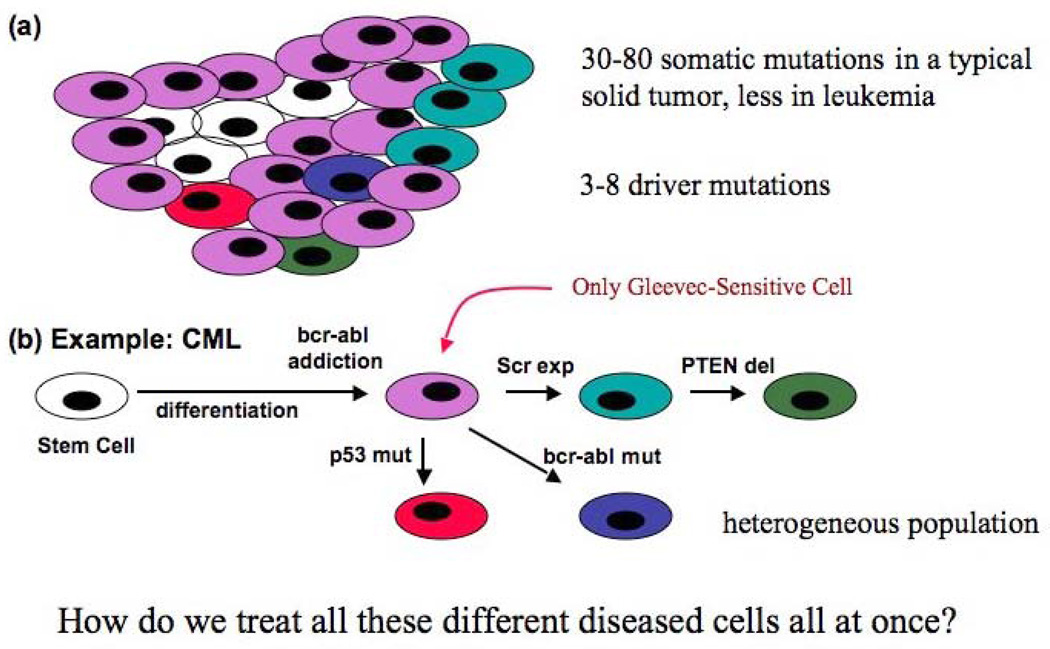
The Complexity of Cancer
Incoming analyses from The Cancer Genome Atlas Project already suggest enormous complexity of the cancer genome. For example, a typical solid tumor contains 30–80 somatic mutations (6). Many researchers are actively engaged with making annotations to each mutant gene. Some are the expected standard mutations found in many cancer types, while others are unique to particular cancer types. Some are so-called driver mutations, causally implicated in oncogenesis, while others are passenger mutations, hitchhikers on a clonal expansion, and some are totally unknown (6). The findings confirm that cancer is indeed a genetic disease. The typical etiology of the disease is that it progresses slowly, accumulating one mutation at time. But there seems to be no fixed schedule, nor a pre-set path. A cancer cell could develop an unexpected mutation that could drive it in a separate direction from the rest. Thus a tumor mass could contain a heterogeneous population of cancer cells at many different stages of development from which it might proceed in all sorts of directions (7). Thus each cancer is unique in its own way, defined by its own set of mutations (Fig. 1a). The challenge for cancer therapy is to find a way to treat all these diseased cells all at once.
Figure 1. Every tumor is unique in its own way. Graphic representation of a heterogeneous tumor cell population.
a, A typical solid tumor contains many cancer cells with different genomic contents (represented by different colours). b, An example of CML cells with different genomic contents. Cancer stem cells for CML are known to express bcr-abl, yet are insensitive to the bcr-abl inhibitor Gleevec, thus not addicted to bcr-abl. Exactly how CML cells become addicted to bcr-abl is not known. In this graphic depiction, there is only one cell sensitive to Gleevec.
Targeted Therapies
Based on a phenomenon called oncogenic addiction, in which a specific cancer type becomes dependent on the activities of just one oncoprotein for its growth and survival (8), targeted therapies deploy a specific inhibitor for this oncoprotein for treatment. The oncogene addiction model gained credence when Gleevec, a specific inhibitor of bcr-abl, successfully treated chronic myeloid leukemia (CML) with remarkable efficacy; 5-year incidence-free survival rates reached over 90% in most studies (9). However, Gleevec could not eliminate CML completely because it could not eliminate the cancer stem cell population (10), forcing treatment to be open-ended. Gleevec was also ineffective in treating CML in blast crisis. Thus, Gleevec seems to be effective only at an intermediate stage, suggesting that oncogenic addiction in CML is limited to a particular stage of development.
Gleevec was also ineffective against acute myeloid leukemia (AML) even though it frequently expresses the bcr-abl protein. In treating AML and CML in blast crisis, Gleevec usually caused very rapid cancer regression, only to have cancer return within a short period of time in treatment-resistant forms (11). One reason for the resistance to Gleevec in CML and AML is the expression of Src family of kinases that can substitute for bcr-abl (12). Mutation in the Gleevec-binding region of bcr-abl is thought to be another reason for the generation of Gleevec-resistant cancer cells. Since p53 is required for Gleevec-induced apoptosis, mutation in p53 could also make CML cells resistant (13) (Fig. 1b). The scenario is remarkably similar to the treatment history of many targeted drugs (2), including that of PLX4032, a specific B-RAF inhibitor, used to treat metastasized melanomas. In the majority of cases, PLX4032 induced rapid, near complete regression of tumors within a few weeks. However, in 100% of the cases, cancer came back within a year in PLX4032-resistant forms (14).
Generally, there are three ways that cancer can become resistant to a targeted therapy:
Mutations in the targeted oncogene, which make them resistant to the specific targeted drugs. Examples: Gleevec-resistant mutations in bcr-abl genes were found in Gleevec-insensitive CML samples (1), and Tarceva-resistant mutations in ERBB3 were found in Tarceva insensitive patients (2).
Expression of proteins that make the targeted protein redundant. Example: COT expression and N-RAS and PDGFRb upregulation were found in PLX4032-resistant melanomas cells (reviewed in (15)), and over-expression of Lyn, a member of Src kinase family, was found in Gleevec-insensitive CML samples (16)
Loss of apoptosis-inducing programs that may be needed when a targeted oncogene is inactivated. Example: Loss of p53 makes CML cells resistant to Gleevec-induced apoptosis (13).
These mutations may have been present in a small number of cells in the initial tumor ass, or they may have developed during the pro-longed treatment. Trying to remedy the situation, more targeted drugs were developed in some cases. A new drug targeting a different region of the same oncogene was found effective in Gleevec resistant CML patients (11).
Applying Personalized Medicine to Cancer Treatment
When we examined the single-agent efficacies of already developed targeted drugs, except for one example (Gleevec), they had all failed to extend life significantly. In many cases, targeted drugs did not even inhibit all variants of oncogenes they are targeting (1). Compounding the problem is the cancer’s ability to develop an alternative signaling pathway, making them independent of the targeted oncogene. Combining targeted drugs may certainly improve the efficacy, but for the combination to be effective, each patient’s cancer genomic profile needs to be built. And even then, that is not a guarantee of success since targeted drugs may not inhibit all the possible variant of the targeted oncogene (1), or cancer may activate alternative pathways for its survival (15, 16). In short, we would not expect to know a priori, how cancer responds to a particular targeted drug and how they might possibly become resistant to them, unless we have build significant experience with particular targeted drugs applied to particular cancer types. Thus it is our view that applying personalized medicine approach to treat cancer would face many obstructs. Hence, searching for another approach that activates the body’s natural cell-death pathways makes sense.
Inducing Apoptosis in Cancer Cells
In healthy individuals, unwanted cells and cells that threaten our wellbeing are killed by inducing apoptosis-activating programs. Genotoxin-based therapies target all proliferating cells, inducing apoptosis through activation of cell cycle checkpoint and genomic surveillance programs. Thus, even though genotoxin-based therapies cause many side effects, unlike targeted therapies in which only specific cancer types can be treated, they can be applied to many cancer types at an early stage of development. Rapidly dividing cancer cells are also under pressure to compromise cell cycle checkpoint and genomic surveillance programs, the same programs that are intermediary for genotoxin-induced apoptosis. As cancer progresses and accumulates more mutations, it seems natural that it becomes more resistant to genotoxin-based therapies. Therefore, to effectively treat advanced cancers, a different approach is needed.
Another approach would be to directly activate apoptosis at the most critical juncture in the apoptotic pathway. This would be the step in which Bak or Bax are oligomerized, forming mitochondrial outer membrane pores through which cytochrome c can escape to start the apoptotic cascade. The step is often referred as the point of no return (17). Expression of BH3-only proteins such as tBid or BimS or transfection of BH3 peptides can activate Bak/Bax and induce apoptosis in cancer cells. They can also induce apoptosis in normal healthy cells (18). Thus, there would be substantial side effects with this approach. However, Bcl-2 antagonists, such as ABT-263 or ABT-737 (ABT), could induce mitochondria-dependent apoptosis in only a limited set of cancer cells such as leukemia cells and some small cell lung carcinomas, yet leaving most of the normal healthy cells intact.
The vast potential of ABT became apparent when we realized that by pre-incubating cancer cells with deoxyglucose, we could induce apoptosis in a variety of cancer types at submicromolar concentration of ABT (5). Furthermore, when deoxyglucose was injected into animals, it predominantly accumulated in cancer cells. Thus we discovered a way to target cancer cells in animals by simply injecting deoxyglucose before the injection of ABT.
Deoxyglucose-ABT Combination Therapy
Except for post-mitotic cells such as neurons and muscle cells, every cell in the body retains the capacity for self-sacrifice through the apoptotic program. Pro-apoptotic protein Bak is normally sequestered by Mcl-1 and Bcl-xL. Only when Bak is released from both Mcl-1 and Bcl-xL, can it form oligomers on the mitochondrial outer membranes through which cytochrome c can escape, thus initializing apoptosis. BH3 proteins such as tBid or BimS or BH3 peptides such as SAHB can disrupt Bak’s association to both Mcl-1 and Bcl-xL, thus freeing Bak and releasing cytochrome c (19, 20). However, forced expression of tBid or BimS, or peptide transfection of SAHB can also harm healthy cells (18). On the other hand, deoxyglucose is efficiently taken-up by cancer cells and some brain cells, disrupting the Bak-Mcl-1 association and priming only these cells for Bcl-2 antagonists-induced apoptosis. When cells primed by deoxyglucose are treated with ABT, the Bak-Bcl-xL association is lost, inducing Bak oligomerization and apoptosis (Fig 2). Even though deoxyglucose can potentially prime brain cells for ABT-induced apoptosis, because ABT cannot cross blood-brain barrier (21, 22), they are not targeted by the combination therapy (Fig. 2). Since the combination of deoxyglucose and Bcl-2 antagonist induces rapid apoptosis through protein-effector activation of mitochondria, it leaves little room for interference by a cancer cell’s highly active mutagenic programs. Cancer cells resistant to 2DG-ABT combination therapies are either cancer cells in chronic phase, cells defective in the intrinsic pathway of apoptosis, or cells expressing P-glycoprotein, which can exclude ABT from entering cancer cells.
Figure 2. Signaling pathways in 2DG-ABT induced apoptosis.
a, Most normal healthy cells outside the brain are not affected by 2DG-ABT combination. b, Brain cells have higher glucose-uptake. However, ABT-263 is prevented from entering the brain by the blood-brain barrier. c, In cancer cells, deoxyglucose (2DG) is carried across the plasma membrane by the active glucose transporter (Glu Transp). It activates multiple signal transduction cascades, possibly phosphorylating Mcl-1/Bak, resulting in the dissociation of the Bak-Mcl-1 complex. ABT-263/737 (ABT) is membrane permeable, crosses the plasma membrane and binds to Bcl-xL, causing dissociation of the Bak-Bcl-xL complex, freeing Bak. Bak oligomerizes, creating pores on the mitochondrial outer membrane through which cytochrome c is released, crossing the point of no return. Cytochrome c triggers assembly of death-executioner apoptosomes, causing cell death. The model is a simplified version of the one found in (5). Note that deoxyglucose also triggers a PI3K-mTOR-AKT pro-survival pathway by activating IGFR.
Our tissue culture studies and cancer-bearing mice showed that the deoxyglucose-ABT combination induced apoptosis in a variety of cell lines. The combination therapy effectively treated difficult-to-treat cancer cells xenografted onto nude mice (5). We are now trying to initiate a clinical trial for the combination. Since both deoxyglucose and ABT-263 are already in Phase II clinical trials, we do know about the safety of these agents. The only known side effects of ABT-263 are mild lymphopenia and reversible thrombopenia. The only concern we have had in using the combination in a clinical trial was with deoxyglucose since it could effect brain function, and unlike mice or rats brains, human brain seems much more delicate and needs more attention. As it turns out, deoxyglucose was used to treat stress-related disorders and schizophrenic patients (23–25), generating enough information to establish the pharmacological dose for deoxyglucose.
Physiological effects of deoxyglucose
The amounts of deoxyglucose used in the 2DG-ABT combination in tissue culture cells was 0.4X that of glucose in the media. Deoxyglucose primed various cell lines and primary culture cells for ABT-induced apoptosis not through ATP insufficiency (intracellular ATP levels declined less than 10% in 8 hours), nor through activating ER stress, but by activating signal transduction cascades, possibly phosphorylating Mcl-1 and dissociating the Bak-Mcl-1 complex (5).
In our mice experiments, we used 0.5 g/kg deoxyglucose mixed with the same amount of glucose, applied by peritoneal injection, and observed no obvious harmful effects. In the past animal studies, 0.25–2 g/kg deoxyglucose was applied by peritoneal injection (see (5) and references within)or 50–250 mg/kg of deoxyglucose intravenously (26) to mice and rats. No harmful effects were observed either. In one article, 250 mg/kg deoxyglucose actually reduced the progression of the kindling in a rat kindling model of temporal lobe epilepsy (27).
In past human clinical studies, 30–250 mg/kg deoxyglucose has been used to treat stress and psychiatric disorders (23–25), and prostate cancer (28), and glioma patients (26, 29, 30). When 40 mg/kg deoxyglucose was administered intravenously to fasting patients in one study, plasma norepinephrine levels increased by 80%, raising glucose levels by 44%, suggesting that the regulatory mechanisms can maintain a normal supply of glucose in the presence of 40 mg/kg deoxyglucose (25). When doses exceeding 300mg/kg were administered in another study, however, two out of six patients became very restless and could not complete the treatment regiment, though no significant changes in the vital parameters were observed even at this dose (29, 30).
With the clinical trials for the combination therapy, the same ratio of 0.4 glucose/deoxyglucose used for the tissue culture and mice studies (5) should be maintained. Since normal blood glucose concentration is usually maintained between 4.4–6.1 mM in humans and mice, a concentration of 1.76 mM deoxyglucose in the blood is indicated for clinical trials of the combination therapy. Thus 40–50 mg/kg of deoxyglucose applied orally or intravenously would be sufficient for most adults, allowing the dose of deoxyglucose to stay within pharmacological parameters.
Possible improvements on the combination therapy
Is deoxyglucose an ideal agent targeting cancer cells? The answer is no. Deoxyglucose activates insulin-like growth factor receptor (IGFR), which activates the PI3K-mTOR-AKT pro-survival pathway (Fig 2b) (see (5) and references within). Thus in many cases, having deoxyglucose in the medium actually reduces the efficacy of chemotherapeutics, including the 2DG-ABT combination. Furthermore, the long-term treatment of deoxyglucose could reduce the cellular concentration of ATP enough to arrest the cell cycle, making certain genotoxins less effective. Of course, this negative effect of deoxyglucose is also an opportunity to improve the 2DG-ABT combination therapy. The 2DG-ABT combination might actually be enhanced by adding a PI3K kinase inhibitor (5). PI3K kinase inhibitors tend to have adverse side effects. Because a new class of safer and more effective PI3K inhibitors is now being developed, it is anticipated that we could add a PI3K inhibitor to an already very effective 2DG-ABT combination.
The combination of deoxyglucose and ABT successfully induced apoptosis in many cancer cell lines derived from a variety of cancer types such as leukemia, hepatocarcinoma, lung, breast, prostate, and cervical cancer (5). It also induced apoptosis efficiently at many stages of cancer development, including p53 mutated PTEN-depleted hormone-independent highly metastasized prostate cancer. Cancer cells resistant to 2DG-ABT combination therapies are either cancer cells in chronic phase, cells defective in the intrinsic pathway of apoptosis, or cells expressing P-glycoprotein, which can exclude ABT from entering cancer cells. Unfortunately, over 90% of pancreatic cancer cells express P-glycoprotein (31).
The combination treatment of cancer-bearing mice was very effective against tumor xenograft from hormone-independent highly metastasized chemo-resistant human prostate cancer cells. Even though the animal studies were efficacious, precautionary measures should be considered when applied to patients. First, since the combination treatment could cause lymphopenia and thrombopenia (5), hematopoietic stem cells should be collected and saved before the combination therapy, for autologous transplant later. Second, since people taking metformin for treatment of diabetes are known to have highly elevated glucose uptake in their bowels (32), the use of metformin might need to be interrupted during the 2DG-ABT combination therapy. Once we take these and possibly other precautionary measures, the combination therapy may provide a safe and effective alternative to genotoxin-based cancer therapies. Thus we may have found a simple solution to a very complex problem.
References
- 1.Shah NP, Nicoll JM, Nagar B, Gorre ME, Paquette RL, Kuriyan J, et al. Multiple BCR-ABL kinase domain mutations confer polyclonal resistance to the tyrosine kinase inhibitor imatinib (STI571) in chronic phase and blast crisis chronic myeloid leukemia. Cancer Cell. 2002 Aug;2(2):117–125. doi: 10.1016/s1535-6108(02)00096-x. [DOI] [PubMed] [Google Scholar]
- 2.Kaiser J. Combining targeted drugs to stop resistant tumors. Science. 2011 Mar 25;331(6024):1542–1545. doi: 10.1126/science.331.6024.1542. [DOI] [PubMed] [Google Scholar]
- 3.Frederick R. Sequencing Cancer Genomes: Targeted Cancer Therapies. ScienceMagazine video http://video.sciencemag.org/featured/850053254001/1. Science. 2011 doi: 10.1126/science.331.6024.1539-b. [DOI] [PubMed] [Google Scholar]
- 4.Warburg O. On respiratory impairment in cancer cells. Science. 1956 Aug 10;124(3215):269–270. [PubMed] [Google Scholar]
- 5.Yamaguchi R, Janssen E, Perkins G, Elisman M, Kitada S, Reed JC. Efficient elimination of cancer cells by deoxyglucose-ABT-263/737 combination therapy. PLoS ONE. 2011 Sep 19;6(9):e24102. doi: 10.1371/journal.pone.0024102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stratton MR, Campbell PJ, Futreal PA. The cancer genome. Nature. 2009 Apr 9;458(7239):719–724. doi: 10.1038/nature07943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bertucci F, Birnbaum D. Reasons for breast cancer heterogeneity. J Biol. 2008;7(2):6. doi: 10.1186/jbiol67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weinstein IB, Joe A. Oncogene addiction. Cancer Res. 2008 May 1;68(9):3077–3080. doi: 10.1158/0008-5472.CAN-07-3293. discussion 3080. [DOI] [PubMed] [Google Scholar]
- 9.Druker BJ, Guilhot F, O'Brien SG, Gathmann I, Kantarjian H, Gattermann N, et al. Five-year follow-up of patients receiving imatinib for chronic myeloid leukemia. N Engl J Med. 2006 Dec 7;355(23):2408–2417. doi: 10.1056/NEJMoa062867. [DOI] [PubMed] [Google Scholar]
- 10.Stuart SA, Minami Y, Wang JY. The CML stem cell: evolution of the progenitor. Cell Cycle. 2009 May 1;8(9):1338–1343. doi: 10.4161/cc.8.9.8209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Talpaz M, Shah NP, Kantarjian H, Donato N, Nicoll J, Paquette R, et al. Dasatinib in imatinib-resistant Philadelphia chromosome-positive leukemias. N Engl J Med. 2006 Jun 15;354(24):2531–2541. doi: 10.1056/NEJMoa055229. [DOI] [PubMed] [Google Scholar]
- 12.Dai Y, Rahmani M, Corey SJ, Dent P, Grant S. A Bcr/Abl-independent, Lyn-dependent form of imatinib mesylate (STI-571) resistance is associated with altered expression of Bcl-2. J Biol Chem. 2004 Aug 13;279(33):34227–34239. doi: 10.1074/jbc.M402290200. [DOI] [PubMed] [Google Scholar]
- 13.Wendel HG, de Stanchina E, Cepero E, Ray S, Emig M, Fridman JS, et al. Loss of p53 impedes the antileukemic response to BCR-ABL inhibition. Proc Natl Acad Sci U S A. 2006 May 9;103(19):7444–7449. doi: 10.1073/pnas.0602402103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bollag G, Hirth P, Tsai J, Zhang J, Ibrahim PN, Cho H, et al. Clinical efficacy of a RAF inhibitor needs broad target blockade in BRAF-mutant melanoma. Nature. 2010 Sep 30;467(7315):596–599. doi: 10.1038/nature09454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McMahon M. Parsing out the complexity of RAF inhibitor resistance. Pigment Cell Melanoma Res. 2011 Apr;24(2):361–365. doi: 10.1111/j.1755-148X.2010.00824.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Donato NJ, Wu JY, Stapley J, Gallick G, Lin H, Arlinghaus R, et al. BCR-ABL independence and LYN kinase overexpression in chronic myelogenous leukemia cells selected for resistance to STI571. Blood. 2003 Jan 15;101(2):690–698. doi: 10.1182/blood.V101.2.690. [DOI] [PubMed] [Google Scholar]
- 17.Green DR, Amarante-Mendes GP. The point of no return: mitochondria, caspases, and the commitment to cell death. Results Probl Cell Differ. 1998;24:45–61. doi: 10.1007/978-3-540-69185-3_3. [DOI] [PubMed] [Google Scholar]
- 18.Wang K, Yin XM, Chao DT, Milliman CL, Korsmeyer SJ. BID: a novel BH3 domain-only death agonist. Genes Dev. 1996 Nov 15;10(22):2859–2869. doi: 10.1101/gad.10.22.2859. [DOI] [PubMed] [Google Scholar]
- 19.Korsmeyer SJ, Wei MC, Saito M, Weiler S, Oh KJ, Schlesinger PH. Pro-apoptotic cascade activates BID, which oligomerizes BAK or BAX into pores that result in the release of cytochrome c. Cell Death Differ. 2000 Dec;7(12):1166–1173. doi: 10.1038/sj.cdd.4400783. [DOI] [PubMed] [Google Scholar]
- 20.Walensky LD, Kung AL, Escher I, Malia TJ, Barbuto S, Wright RD, et al. Activation of apoptosis in vivo by a hydrocarbon-stapled BH3 helix. Science. 2004 Sep 3;305(5689):1466–1470. doi: 10.1126/science.1099191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tagscherer KE, Fassl A, Campos B, Farhadi M, Kraemer A, Bock BC, et al. Apoptosis-based treatment of glioblastomas with ABT-737, a novel small molecule inhibitor of Bcl-2 family proteins. Oncogene. 2008 Nov 6;27(52):6646–6656. doi: 10.1038/onc.2008.259. [DOI] [PubMed] [Google Scholar]
- 22.Vogler M, Dickens D, Dyer MJ, Owen A, Pirmohamed M, Cohen GM. The B-cell lymphoma 2 (BCL2)-inhibitors, ABT-737 and ABT-263, are substrates for P-glycoprotein. Biochem Biophys Res Commun. 2011 May 6;408(2):344–349. doi: 10.1016/j.bbrc.2011.04.043. [DOI] [PubMed] [Google Scholar]
- 23.Breier A A.E. Bennett award paper. Experimental approaches to human stress research: assessment of neurobiological mechanisms of stress in volunteers and psychiatric patients. Biol Psychiatry. 1989 Sep;26(5):438–462. doi: 10.1016/0006-3223(89)90066-8. [DOI] [PubMed] [Google Scholar]
- 24.Mattson MP. Gene-diet interactions in brain aging and neurodegenerative disorders. Ann Intern Med. 2003 Sep 2;139(5 Pt 2):441–444. doi: 10.7326/0003-4819-139-5_part_2-200309021-00012. [DOI] [PubMed] [Google Scholar]
- 25.Elman I, Rott D, Green AI, Langleben DD, Lukas SE, Goldstein DS, et al. Effects of pharmacological doses of 2-deoxyglucose on plasma catecholamines and glucose levels in patients with schizophrenia. Psychopharmacology (Berl) 2004 Nov;176(3–4):369–375. doi: 10.1007/s00213-004-1890-y. [DOI] [PubMed] [Google Scholar]
- 26.Mohanti BK, Rath GK, Anantha N, Kannan V, Das BS, Chandramouli BA, et al. Improving cancer radiotherapy with 2-deoxy-D-glucose: phase I/II clinical trials on human cerebral gliomas. Int J Radiat Oncol Biol Phys. 1996 Apr 1;35(1):103–111. doi: 10.1016/s0360-3016(96)85017-6. [DOI] [PubMed] [Google Scholar]
- 27.Garriga-Canut M, Schoenike B, Qazi R, Bergendahl K, Daley TJ, Pfender RM, et al. 2-Deoxy-D-glucose reduces epilepsy progression by NRSF-CtBP-dependent metabolic regulation of chromatin structure. Nat Neurosci. 2006 Nov;9(11):1382–1387. doi: 10.1038/nn1791. [DOI] [PubMed] [Google Scholar]
- 28.Stein M, Lin H, Jeyamohan C, Dvorzhinski D, Gounder M, Bray K, et al. Targeting tumor metabolism with 2-deoxyglucose in patients with castrate-resistant prostate cancer and advanced malignancies. Prostate. 2010 Sep 15;70(13):1388–1394. doi: 10.1002/pros.21172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Singh D, Banerji AK, Dwarakanath BS, Tripathi RP, Gupta JP, Mathew TL, et al. Optimizing cancer radiotherapy with 2-deoxy-d-glucose dose escalation studies in patients with glioblastoma multiforme. Strahlenther Onkol. 2005 Aug;181(8):507–514. doi: 10.1007/s00066-005-1320-z. [DOI] [PubMed] [Google Scholar]
- 30.Dwarakanath BS, Singh D, Banerji AK, Sarin R, Venkataramana NK, Jalali R, et al. Clinical studies for improving radiotherapy with 2-deoxy-D-glucose: present status and future prospects. J Cancer Res Ther. 2009 Sep;5 Suppl 1:S21–S26. doi: 10.4103/0973-1482.55136. [DOI] [PubMed] [Google Scholar]
- 31.O'Driscoll L, Walsh N, Larkin A, Ballot J, Ooi WS, Gullo G, et al. MDR1/P-glycoprotein and MRP-1 drug efflux pumps in pancreatic carcinoma. Anticancer Res. 2007 Jul–Aug;27(4B):2115–2120. [PubMed] [Google Scholar]
- 32.Gontier E, Fourme E, Wartski M, Blondet C, Bonardel G, Le Stanc E, et al. High and typical 18F-FDG bowel uptake in patients treated with metformin. Eur J Nucl Med Mol Imaging. 2008 Jan;35(1):95–99. doi: 10.1007/s00259-007-0563-6. [DOI] [PubMed] [Google Scholar]