Abstract
Purpose
This systematic review updates one conducted in 2008 into extended scope practice (ESP) in physiotherapy in orthopedics.
Methods
A comprehensive open-ended search was conducted using electronic library data-bases and Google Scholar to identify any primary study design reporting on physiotherapists working in ESP roles within orthopedic settings. Studies were allocated to the National Health and Medical Research Council hierarchy of evidence, although only studies in levels I, II, or III_1 were critically appraised using a purpose-built critical appraisal tool. Information was extracted on the country of origin, ESP tasks, relevant training, patient types, health, process, and cost measures.
Results
1071 studies were identified, and twelve were included in the review (including diagnostic and evaluative research). The hierarchy of evidence ranged from II to IV, from which only two diagnostic studies met the criteria for critical appraisal. ESP tasks included injection therapy, removing k-wires, and requesting investigations. The education of ESP physiotherapists varied widely, and included formal and informal training. The positive outcomes of ESP initiatives were reported, in diagnostic ability, reduced costs and waiting times, and improved health outcomes.
Conclusion
Despite the positive results, the generally low level of evidence and the range of outcome measures reported, constrained clear conclusions regarding the health, process, and cost implications of ESP physiotherapy roles in orthopedic settings. The need for formalized, widely recognized training was highlighted, to give ESP physiotherapy roles credibility.
Keywords: extended scope practice, physiotherapy, orthopedics
Introduction
There are increasing reports, particularly from the United Kingdom (UK) and Australia, of implementation of extended scope of physiotherapy roles. A commissioned systematic review1 of the literature was undertaken to assist in determining the feasibility of introducing extended practice roles in physiotherapy within the Australian Capital Territory (ACT) Government Health Directorate and the ACT Department of Disability, Housing and Community Services (DHCS). This review found a lack of consensus regarding the definition of extended scope practice (ESP), although there was general agreement that it involved an expansion of traditional physiotherapeutic roles, in terms of diagnostics, management, and consultation. This review presented a working definition of ESP in physiotherapy:
“An ESP physiotherapist is a clinical specialist, who has the opportunity to develop and demonstrate expertise beyond the currently recognized scope of practice, including some aspect of job enhancement or expansion, involving the areas of extended therapeutics, diagnostics and practice consultation.”1
Lowe et al1 incorporated peer-reviewed and non-peer-reviewed publications, and grey literature. This review identified that while the majority of literature supported the potential usefulness of extending traditional roles in physiotherapy, there was a lack of information on quantifiable outcomes, particularly in terms of clinical efficacy, safety, and cost reductions or benefits. The literature presented in the 2008 review focused on organizational issues, such as patient waiting times, re-referral rates, and the appropriateness of referrals made by the ESP physiotherapist.
Lowe et al’s1 review examined ESP physiotherapy roles within emergency departments (EDs) and orthopedic outpatient clinics, although the potential for ESP in cardiorespiratory, obstetrics and gynecology, and neurology settings was recognized. The aim of this review is to update Lowe et al’s1 review regarding extension of scope of physiotherapy activities in orthopedic settings.
Material and methods
Research questions
The research questions for this review were:
How is ESP practiced in orthopedic outpatients?
What training and supervision is reported for ESP physiotherapists in orthopedic outpatients?
What is the evidence of effectiveness of ESP physio-therapy roles in orthopedics in terms of processes, cost containment, and health outcomes?
How does the literature identified in this review build on the findings of the Lowe et al1 review in terms of ESP physiotherapists working in orthopedic outpatients?
Search strategy
Inclusion/exclusion criteria
Types of studies
All study designs were eligible for inclusion. Literature had to be available in English, in full text, and published in peer-reviewed journals.
Publication dates of studies
No start or end date was set, following the search strategy reported in Lowe et al.1
Search criteria
A PICO (participants, interventions, comparison, outcome measure) approach was used to search library databases, in which there was no defined comparison.
Types of participants (P)
Participants were defined as physiotherapists working in an extended scope capacity, with patients with orthopedic conditions, in non-emergency situations. If the study involved non-orthopedic conditions and the physiotherapy management was not reported separately, the study was excluded.
Types of activities/interventions (I)
Any activity or intervention provided by a physiotherapist working in an ESP capacity was reported. For the purpose of this review, extension of scope activities referred to activities which are an extension of the agreed scope of physiotherapy practice in Australia, or stated extension of physiotherapy scope of practice relevant to another country. We used the following definitions for this purpose.
Advanced scope of practice – “A role that is within currently recognized scope of practice for that profession, but that through custom and practice has been performed by other professions. The advanced role would require additional training, competency development, as well as significant clinical experience and formal peer recognition. This role describes the depth of practice”.2
Extended scope of practice – “A role that is outside the currently recognized scope of practice and requires legislative change. Extended scope of practice requires some method of credentialing following additional training, competency development, and significant clinical experience. Examples include prescribing, injecting, and surgery. This role describes the breadth of practice”.2
Types of comparison interventions (C)
There was no defined comparison intervention.
Types of outcome measures (O)
Any process, cost, or health outcome was included. Such measures may include, but are not limited to, waiting times, referral rates, suitability of referrals, percentage of patients who were managed entirely by the ESP physiotherapist, and diagnostic ability of the ESP physiotherapists.
Search methods for identification of studies
All available electronic library databases were searched, using a composite and comprehensive set of search terms which were modified as required, for application to specific databases (OvidSP and Ebsco Host) and Google Scholar. See Appendix 1 for details.
Appendix 1.
Scoping search for physiotherapists ESP in Orthopedics and Emergency Department
| Databases | Search terms |
|---|---|
| Google scholar | Physiotherapy + ESP + ortho |
| EBSCO Host Academic Search Premier, AgeLine, CINAHL, eBook Collection (EBSCOhost), Education Research Complete, E-Journals, ERIC, Health Business Elite, Health Source–Consumer Edition, Health Source: Nursing/Academic Edition, SPORTDiscus |
Physiotherap* OR “physical therap*” AND “Extended scope” OR “extended practice” OR ESP AND Orthopaedic* OR orthopedic* Physiotherap* OR “physical therap*” AND “Extended scope” OR “extended practice” OR ESP AND Emergency OR urgent Physiotherap* OR “physical therap*” AND “Extended scope” OR “extended practice” OR ESP AND Bone OR muscle physiotherap* OR “physical therap*” AND “Extended scope” OR “extended practice” OR ESP AND Musculoskelet* |
| OvidSP | Physiotherap* OR “physical therap*” AND “Extended scope” OR “extended practice” OR ESP AND Orthopaedic* OR orthopedic* Physiotherap* OR “physical therap*” AND “Extended scope” OR “extended practice” OR ESP AND Emergency OR urgent Physiotherap* OR “physical therap*” AND “Extended scope” OR “extended practice” OR ESP AND Bone OR muscle Physiotherap* OR “physical therap*” AND “Extended scope” OR “extended practice” OR ESP AND Musculoskelet* |
Abbreviation: ESP, extended scope practice.
Data collection and analysis
Selection of studies
Titles and abstracts of papers identified in the search were screened for relevance and duplicates removed, before full texts were viewed to determine suitability for inclusion.
Hierarchy of evidence
The hierarchy of evidence of each included study was determined according to the National Health and Medical Research Council (NHMRC) Hierarchy of Evidence.3
Assessment of risk of bias in included studies
Lowe et al’s1 review indicated that a range of study designs may be identified from this search. The potential for risk of bias in the included studies was determined initially by the allocation to the hierarchy of evidence. If studies of Levels I, II, or III_1 were identified, critical appraisal of methodological quality would be undertaken using purpose-built key criteria relevant to the area (nonbiased selection of subjects, nonbiased allocation into treatment groups, and comparison with Gold Standard processes/outcomes). We assumed that the inherent methodological bias in the lower hierarchy studies was likely to distort the believability of any findings.
Data extraction and management
Extracted data was entered into a purpose-built Microsoft Excel sheet. Extracted data included the country of origin, research question, level of evidence, study design, patient types, ESP tasks, clinic type, a range of service delivery issues if and when reported (other health professionals involved in service delivery, appointment duration, methods of obtaining patients, training, protocols, supervision/accountability), and cost, health, and process outcome measures.
Data analysis
Data was analyzed descriptively, by considering the history and design of the available research, the processes by which, and the environments within which, ESP physiotherapists worked, the activities they undertook in the workplace (and how/if these activities were monitored/supervised), contexts of work, and any reported outcomes.
Results
Description of studies
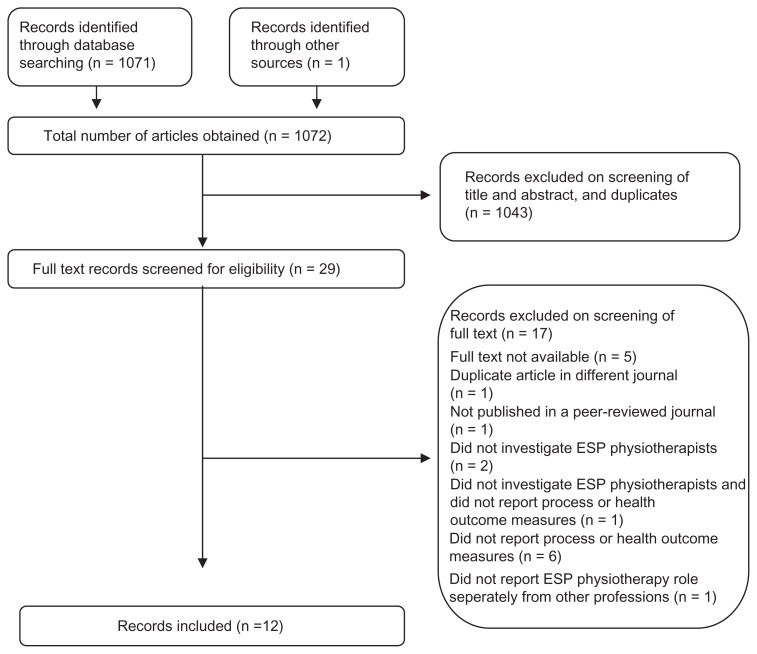
One thousand and seventy-one studies were identified in the search. The ACT Government Health Directorate identified one additional, recently published study4 which was not yet library-indexed. This study was relevant and was included in the review. One thousand and forty-three studies were excluded as they were duplicates or were not relevant to the review, based on the title and abstract. Five studies were not published as full text, and a further twelve studies were excluded as not being relevant, upon screening the full text. One of these had been duplicate-published in two different journals, and another was not published in a peer-reviewed journal. The reasons for excluding the other studies are included in the consort diagram (Figure 1). Twelve studies were therefore included in the study.
Figure 1.
Consort diagram.
Abbreviation: ESP, extended scope practice.
Study designs and levels of evidence
Table 1 reports the author, country, type of research question, the hierarchy of evidence, and the design of the study. Two types of research questions were reported, evaluation and diagnostic, with the highest hierarchy found in the diagnostic studies (two Level II studies). The most common evaluation designs were Levels III_2 and III_3. The studies in italics were found in the 2008 review, the normal font studies were those which had been published subsequently.
Table 1.
Country, type of research question, level of evidence, and study design
| Study | Country | Type of research question | Level of evidence | Study design |
|---|---|---|---|---|
| Blackburn et al6 | Australia | Evaluation | III_3 | Observational: retrospective cohort |
| Dickens et al12 | UK | Diagnostic | II | Observational: prospective cohort/agreement (between disciplines) |
| Gardiner and Turner13 | UK | Diagnostic | II | Observational: retrospective audit accuracy (disciplines with surgical findings) |
| Harrison et al7 | UK | Evaluation | III_3 | Observational: retrospective audit |
| Hattam14 | UK | Diagnostic | III_2 | Observational: validation of triage decision with case notes |
| Hattam and Smetham5 | UK | Intervention | III_2 | Intervention: quasi-experimental |
| Heywood8 | UK | Evaluation | III_3 | Observational: retrospective cohort |
| Maddison et al9 | UK | Intervention | III_3 | Observational: over time comparisons |
| Moloney et al10 | Ireland | Intervention | IV | Position paper about training and measurement |
| Morris et al4 | Australia | Intervention | III_2 | Intervention: quasi-experimental |
| Oakes15 | UK | Diagnostic | III_2 | Observational: retrospective validation of triage decisions using case notes |
| Rabey11 | UK | Evaluation | III_3 | Observational: retrospective cohort/descriptive |
Note: Studies in italics were found in the 2008 review; the normal font studies were those which had been published subsequently.
The literature base, which consisted of two Level III_2 intervention studies,4,5 six lower (III_3 and IV) hierarchy intervention studies,6–11 and four diagnostic,12–15 is reported in Table 1. Two of the diagnostic studies13,14 had the highest level of hierarchy of literature identified in the search.
Morris et al4 investigated the effectiveness of physiotherapists working in a telephone triage role, which is considered within scope. However one of the management options for patients in this study was attending a multidisciplinary clinic in which an ESP physiotherapist was being trained and supervised. The extracted data for this review reports only on the ESP management component of this study.
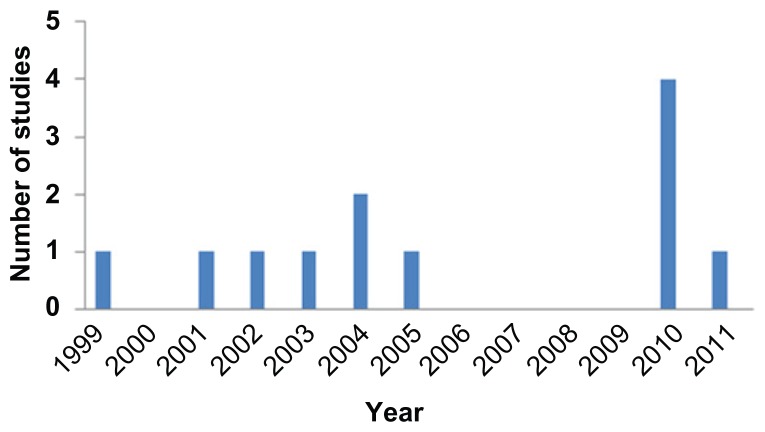
Included studies were published from 1999 to 2011, as indicated in Figure 2. There has been no clear improvement in the bias inherent in study designs used or the types of studies published (eg, intervention, diagnostic), over this time period.
Figure 2.
Graph of the number of included studies per year.
Critical appraisal
The relevant critical appraisal scores are reported in Table 2. Only two studies12,13 were eligible for critical appraisal. Both were diagnostic studies which used non-biased selection of subjects, however only Gardiner and Turner13 made comparisons with a Gold Standard.
Table 2.
Critical appraisal
| Study | Non-biased selection of subjects | Non-biased allocation into treatment groups | Comparison with Gold Standard processes/outcomes |
|---|---|---|---|
| Dickens et al12 | Yes | NA (no treatment groups, all patients seen by two physiotherapists and consultant) | No (decisions of each health provider were recorded, and the surgeon had final say) |
| Gardiner and Turner13 | Yes | NA (no treatment groups) | Yes (arthroscopy) |
Note: Studies in italics were found in the 2008 review.
Tasks
ESP physiotherapy management tasks were variously reported as injection therapy,5,7,13 or removal of plaster of Paris and k-wires.10 ESP physiotherapists were permitted to request further investigations such as radiographs,5,7,8,10,11,13 and blood tests.8,11,13 Referrals could be made by ESP physiotherapists to other allied health professionals,5,13,15 or medical professionals.5–8,11,13–15 More specifically, the medical referrals could be to orthopedics,5–8,11,14 rheumatology,8 or pain clinics.8 In some cases, the ESP physiotherapist may list patients for surgery.13,15
ESP physiotherapists did not universally have complete autonomy in performing these tasks. Some had to have X-ray requests ‘signed off ’ by a medical consultant10 and others had to discuss referrals, surgery listings, and requests for radiological investigations with the medical consultant, although the medical consultant was not required to assess the patient.13 Harrison et al7 reported that difficult cases could be discussed with medical practitioners in the orthopedic clinic, should the ESP physiotherapist require additional support.
Protocols were developed in some cases to assist the ESP physiotherapist to conduct the extension of scope tasks.6,8,10 These included protocols for the first physiotherapy appointment,6 examination and assessment, and for requesting further investigations and managing fractures.8 These were developed by physiotherapy and orthopedic staff,6 or ESP physiotherapists and nurse practitioners10 and were based on the orthopedic consultants’ examination, assessment, and management processes.8,10
Multidisciplinary approach
The included studies highlighted the multidisciplinary mechanisms of activities in which ESP physiotherapists engaged. They were reported to work alongside other physiotherapists5,12 and orthopedic staff including consultants, and various specialist registrars.7,13
Patient referrals
In most cases, patients were referred to an orthopedic clinic by a medical doctor (usually a general practitioner [GP]).6,7,9–13 In some cases the referrals were screened by the orthopedic surgeon6,7,10 or by the ESP physiotherapist.9,11 Direct GP referrals were reported by Hattam and Smetham,5 while in a military setting, referrals were accepted from senior physiotherapists (military and civilian), medical officers, and civilian medical practitioners.8
A range of patients were seen by ESP physiotherapists, as reported in Table 3.
Table 3.
Patient types
| Study | Patient types |
|---|---|
| Blackburn et al6 | Low back pain (including discogenic, degenerative disease, spinal canal stenosis, spondylolisthesis) |
| Dickens et al12 | Knee conditions excluding confirmed fracture, previous knee surgery, severe osteoarthritis, or referral from another consultant |
| Gardiner and Turner13 | Internal derangement of the knee |
| Harrison et al7 | Shoulder problems (including impingement, rotator cuff tear, osteoarthritis, and adhesive capsulitis) |
| Hattam14 | Knee, shoulder, lumbar, and other sites |
| Hattam and Smetham5 | Lower limb, upper limb, and spinal |
| Heywood8 | Spinal |
| Maddison et al9 | Acute and chronic back pain, soft tissue injury, osteoarthritis, arthritis, connective tissue disease |
| Moloney et al10 | Uncomplicated fractures |
| Morris et al4 | Orthopedic patients |
| Oakes15 | Shoulder problems (impingements, muscle tears and imbalance, adhesive capsulitis, fractured clavicle, glenohumeral joint osteoarthritis and stability, and spinal referred) |
| Rabey11 | Knee and lumbar spine disorders |
Note: Studies in italics were found in the 2008 review; the normal font studies were those which had been published subsequently.
Training
The ESP physiotherapists had a variety of training, and years of experience. Consequently, it is difficult to recommend a standard approach for identifying suitable candidates. For instance, Gardiner and Turner13 stated that the ESP physiotherapists had additional training in requesting investigations and performing injection therapy, although no details regarding the training were reported. In addition, while Dickens et al12 stated that the ESP physiotherapists had, on average, 5 years of experience as a senior orthopedic physiotherapist, Hattam and Smetham5 reported that their ESP physiotherapists had extensive postgraduate training, including a Diploma in Injection Therapy, over 10 years of experience working in musculoskeletal physiotherapy, and had attained a fellowship of the Society of Orthopedic Medicine. The physiotherapists in the study conducted by Blackburn et al6 had a minimum of a Masters in Musculoskeletal Physiotherapy, in addition to at least 12 years of experience in the musculoskeletal area. It is unclear in most instances whether the training reported in these studies was required prior to taking on the ESP role or whether it was provided to describe the physiotherapists who worked in this area.
Moloney et al10 examined aspects of implementation of a clinical specialist physiotherapist role, including their training, in a fracture clinic over a 6-month period. The initial 2 months was spent entirely in training. This continued over the next 4 months whilst patients were being treated. Training in the first 2 months included shadowing orthopedic consultants and registrars, other ESPs, and plaster technicians in fracture clinics. In addition, the physiotherapists attended a recognized X-ray interpretation course, in-house courses including Radiation Protection Regulations, and they had ongoing access to study days, special interest groups, and ESP conferences. They had scheduled time to draft protocols and guidelines, and review medico-legal issues. During the third month, the physiotherapist continued to shadow consultants and registrars, and had a limited number of patients to review, from each of the permanent orthopedic consultants, in addition to having discussions with the consultant about patient management. Shadowing and management discussions continued in the final 3 months, in addition to the consultant assessing competency via the physiotherapist’s notes, as well as the ESP writing-up selected case histories for review.
Evidence to support the effectiveness of ESP physiotherapists
The high hierarchy studies reported positive results regarding the effectiveness and efficiency of management provided by the ESP physiotherapist. The outcome measures varied between studies.
Hattam14 reported on the nature of referrals made by ESP physiotherapists. He reported that 16.5% referrals were for investigations, 27.6% were for further investigation, and 55.9% were for surgery. Seventy-four percent of patients referred for surgery were deemed suitable for a surgical referral, 79% had an operable lesion, and 69.5% accuracy reported in determining whether surgery was required. Overall, 70.6% of referrals to consultants were considered appropriate.
Diagnostic accuracy
Two high-hierarchy diagnostic studies compared the ESP physiotherapist’s diagnosis with consultants’ or surgical findings. Dickens et al12 investigated the diagnosis made by a consultant and two ESP physiotherapists, on the basis of a non-invasive assessment. Following this, participants were referred for conservative treatment or arthroscopy, based upon discussion between the three professionals, in which the consultant had the final say. The accuracy of this diagnosis was determined by comparing it to arthroscopy results. If the patient improved with conservative treatment, the consultant’s decision was considered to be correct, regardless of the views of the ESP physiotherapists. They found that the consultant’s initial diagnosis was correct for 92% of patients, while 84% and 80% agreement was reported for the two ESP physiotherapists involved in the study, respectively.
Gardiner and Turner13 compared the orthopedic team, doctors, and ESP physiotherapist’s diagnoses with arthroscopy findings (n = 128). The ESP physiotherapist’s diagnosis agreed with the arthroscopy findings for 52% of patients, compared with 40% and 37% agreement for the orthopedic team and doctors, respectively. Furthermore, the ESP physiotherapist identified that the patient had an operable condition 100% of the time, in comparison with 79% achieved by doctors.
Waiting times
Only two high-hierarchy studies reported waiting times associated with implementing an ESP physiotherapy role. Hattam and Smetham5 reported that the average waiting time to see the ESP physiotherapist was 32 working days (range 4–87 days), compared with the orthopedic waiting times which were over 11 months. However, the quasi-experimental design of this study attenuates the believability of the finding.
Morris et al4 triaged some orthopedic patients to a multidisciplinary clinic, which included an orthopedic surgeon, a rheumatologist, and an ESP physiotherapist. Prior to the implementation of this service, the median time on the waiting list for an orthopedic appointment was 25.1 months (IQR: 24.3–31.3) compared with the time waiting for a triage telephone call, followed by some form of management (6.6 months [IQR: 5.8–7.5 months]). This represented a significant decrease in waiting time.
Costs
Harrison et al7 in the UK compared the cost of an orthopedic appointment with an ESP physiotherapy appointment. The ESP physiotherapy appointment was cheaper at £11 (compared with £16 for an orthopedic appointment).
Morris et al,4 in an Australian study, reported the cost of an ESP physiotherapist as AU$58.03/hour compared with a salaried specialist (AU$128.76/hour). The average cost of an appointment at the multidisciplinary clinic was AU$52.59. Via this clinic, 21 patients were discharged prior to having an orthopedic appointment resulting in a decrease in costs of approximately 48%.
Health outcomes
Health outcomes were rarely reported. While Harrison et al7 reported that Constant–Murley shoulder scores (which evaluate function, range of motion and pain) improved on average by 40 points, and that no patient had a decrease in their score, no comparison was made with other forms of management. Dickens et al12 reported that all patients who received conservative physiotherapy management improved. The focus of this study was determining agreement between the diagnosis made by an orthopedic consultant and ESP physiotherapist. Hence, this management was unlikely to involve any ESP techniques.
Discussion
Only one additional study8 published within the dates of the Lowe et al1 review, was included in this review. Since 2008, only six more studies have been published which reported processes and/or outcome measures related to physiotherapists working in ESP roles in orthopedic settings. However, the low levels of evidence and poor methodological quality of these studies mean that the evidence base regarding the effectiveness of physiotherapists working in extension of scope practice in orthopedics has not changed since Lowe et al’s1 review. Consequently, no conclusions can be drawn regarding the effectiveness of the management of orthopedic patients by physiotherapists working in extended scope roles. The studies provide some evidence that the introduction of such roles may decrease waiting times and costs, and that some patients who had been referred to the orthopedic clinic may not require further medical management following management by an ESP physiotherapist. Perhaps the most important aspect of this review was the finding that ESP physiotherapists’ ability to diagnose some musculoskeletal conditions, and accurately identify patients requiring surgery, was comparable to that of orthopedic (medical) consultants.
What constitutes extended scope of orthopedic practice for physiotherapists remains unclear. This is possibly due to the difference in traditional physiotherapy roles in different countries and even different work settings. This, therefore, constrains the differentiation between traditional physiotherapy skills (within scope), advanced physiotherapy skills (at the margins of scope), and extended scope of practice. Due to the large number of studies from the UK, the information presented is most relevant to ESP physiotherapy roles in that country. Although this may give an indication of the benefits of developing such roles elsewhere, research specific to the health service delivery processes in each country will need to be conducted to ensure that the same benefits are obtained elsewhere. This is corroborated by a recent commentary paper16 which highlights the need for establishing a business case prior to introducing ESP physiotherapy intervention, to ensure that significant impact on service delivery will occur. Furthermore, all studies were conducted in specific hospital settings, sometimes with only one ESP physiotherapist involved, which limits the generalizability and clinical utility of the results. Each ESP physiotherapist was likely to have different work experiences, different training both within the hospital and more formal settings, different protocols and varying levels of support, and contact with others in the orthopedic team.
There are persistent evidence gaps to support the wide-spread implementation of ESP physiotherapy roles. The positive results reported in some studies, however, indicate that further research would be of benefit. This research should aim to use high quality study designs, and investigate the ESP physiotherapy roles on a large scale, potentially over a variety of sites, and different physiotherapists. The training provided to ESP physiotherapists, the decision-making protocols they use, and support of others within the multidisciplinary team should be clearly reported so that the reproducibility of the health service delivery processes can be replicated elsewhere, should positive results be obtained. While process measures such as waiting times form the majority of the reported evidence, cost and health outcomes should also be considered in future studies to demonstrate that management provided by ESP physiotherapists is cost effective, beneficial, and safe for patients.
Conclusion
This review found that research into ESP physiotherapy roles in orthopedics has not considerably improved in quality or volume since the last systematic review1 was conducted in 2008. There is still no clarity on definitions of ESP roles (sufficient to distinguish them from traditional or advanced practice), and the available research continues to be of lower hierarchy, threatened by bias and sitespecific. The lack of standardized training underpinning ESP physiotherapy practice is evident, despite the country of origin of the research, and there are large differences in autonomy in decision-making. The literature suggests that ESP physiotherapists may be comparable with medical doctors in terms of clinical decision-making pertaining to patients with orthopedic conditions, and there are indications that ESP physiotherapy services may improve the efficiency of outpatient management pathways for orthopedic patients.
Acknowledgment
The iCAHE team for conducting the search.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Lowe J, Prior M. A Systematic Review of the Literature on extended scope of practice physiotherapy: Physiotherapy extended scope of practice project. ACT Government Health Directorate: ACT Government; 2008. [Accessed January 11, 2012]. Available from: http://www.health.act.gov.au/c/health?a=sendfile&ft=p&fid=1301227758&sid= [Google Scholar]
- 2.APA. Position Statement: Scope of Practice. Australian Physiotherapy Association; Victoria: 2009. [Accessed November 21, 2011]. Available from: http://physiotherapy.asn.au/images/Document_Library/Position_Statements/2014%20scope%20of%20practice.pdf. [Google Scholar]
- 3.NHMRC NHMRC levels of evidence and grades for recommendations for developers of guidelines National Health and Medical Research Council. Australia Government; 2009. [Accessed January 23, 2012]. Available from: http://www.nhmrc.gov.au/_files_nhmrc/file/guidelines/evidence_statement_form.pdf. [Google Scholar]
- 4.Morris J, Grimmer-Somers K, Kumar S, et al. Effectiveness of a physiotherapy-initiated telephone triage of orthopedic waitlist patients. Patient Related Outcome Measures. 2011;2:151–159. doi: 10.2147/PROM.S2373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hattam P, Smetham A. Evaluation of an orthopaedic screening service in primary care. Clin Perform Qual Health Care. 1999;7(3):121–124. [PubMed] [Google Scholar]
- 6.Blackburn M, Cowan S, Cary B, Nall C. Physiotherapy-led triage clinic for low back pain. Aust Health Rev. 2009;33(4):663–670. doi: 10.1071/ah090663. [DOI] [PubMed] [Google Scholar]
- 7.Harrison J, Rangan A, Shetty A, Robinson C. Reducing waiting times: physiotherapy shoulder assessment clinic. Brit J Ther Rehabil. 2001;8:57–59. [Google Scholar]
- 8.Heywood J. Specialist physiotherapists in orthopaedic triage-the results of a military spinal triage clinic. J R Army Med Corps. 2005;151(3):152–156. doi: 10.1136/jramc-151-03-04. [DOI] [PubMed] [Google Scholar]
- 9.Maddison P, Jones J, Breslin A, et al. Improved access and targeting of musculoskeletal services in northwest wales: targeted early access to musculoskeletal services (teams) programme. BMJ. 2004;329(7478):1325–1327. doi: 10.1136/bmj.329.7478.1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moloney A, Dolan M, Shinnick L, Murphy M, Wallace L. A 6-month evaluation of a clinical specialist physiotherapist’s role in a fracture clinic. Physiother Ireland. 2009;30(1):8–15. [Google Scholar]
- 11.Rabey M. Orthopaedic physiotherapy practitioners: surgical and radiological referral rates. Clinical Governance. 2009;14(1):15–19. [Google Scholar]
- 12.Dickens V, Ali F, Gent H, Rees A. Assessment and diagnosis of knee injuries: the value of an experienced physiotherapist. Physiother. 2003;89:417–422. [Google Scholar]
- 13.Gardiner J, Turner P. Accuracy of clinical diagnosis of internal derangement of the knee by extended scope physiotherapists and orthopaedic doctors: retrospective audit. Physiother. 2002;88:153–157. [Google Scholar]
- 14.Hattam P. The effectiveness of orthopaedic triage by extended scope physiotherapists. Clinical Governance. 2004;9:244–252. [Google Scholar]
- 15.Oakes H. Orthopaedic shoulder clinic diagnosis and treatment plan audit. Clinical Governance. 2009;14(2):126–133. [Google Scholar]
- 16.Gilmore LG, Morris JH, Murphy K, Grimmer-Somers K, Kumar S. Skills escalator in allied health: a time for reflection and refocus. J Healthcare Leadership. 2011;3:53–58. [Google Scholar]