Abstract
Pancreatic β-cell proliferation is infrequent in adult humans and is not increased in type 2 diabetes despite obesity and insulin resistance, suggesting the existence of inhibitory factors. Free fatty acids (FFAs) may influence proliferation. In order to test whether FFAs restrict β-cell proliferation in vivo, mice were intravenously infused with saline, Liposyn II, glucose, or both, continuously for 4 days. Lipid infusion did not alter basal β-cell proliferation, but blocked glucose-stimulated proliferation, without inducing excess β-cell death. In vitro exposure to FFAs inhibited proliferation in both primary mouse β-cells and in rat insulinoma (INS-1) cells, indicating a direct effect on β-cells. Two of the fatty acids present in Liposyn II, linoleic acid and palmitic acid, both reduced proliferation. FFAs did not interfere with cyclin D2 induction or nuclear localization by glucose, but increased expression of inhibitor of cyclin dependent kinase 4 (INK4) family cell cycle inhibitors p16 and p18. Knockdown of either p16 or p18 rescued the antiproliferative effect of FFAs. These data provide evidence for a novel antiproliferative form of β-cell glucolipotoxicity: FFAs restrain glucose-stimulated β-cell proliferation in vivo and in vitro through cell cycle inhibitors p16 and p18. If FFAs reduce proliferation induced by obesity and insulin resistance, targeting this pathway may lead to new treatment approaches to prevent diabetes.
β-Cell mass and insulin secretory function are both reduced in type 2 diabetes (1–3). Despite robust adaptive β-cell proliferation in some rodent strains, this phenomenon is variable, suggesting the existence of restraining influences (1). The signals driving adaptive β-cell proliferation remain poorly understood. Although existing models—obesity, insulin resistance, partial pancreatectomy, pregnancy, and hyperglycemia—share increased metabolic load on the β-cell, a common mechanism has not been identified (4). One potential link may be intracellular glucose metabolism, which is increased in hyperglycemic models but also drives β-cell proliferation in certain normoglycemic conditions (5–10).
Factors limiting adaptive β-cell proliferation are even less well understood. Free fatty acids (FFAs) exert toxic effects on β-cell survival and function and are predictive of progression to type 2 diabetes independently of insulin-mediated glucose uptake (11–16). Although it has been postulated that FFAs might stimulate β-cell proliferation in the context of obesity (16), other proliferation drivers, such as insulin resistance and hyperinsulinemia, are also present. In fact, FFAs may inhibit β-cell proliferation (17,18). Data remain discordant. In β-cell culture models, for example, FFAs are neutral or stimulate proliferation during nutrient-starvation, such as low glucose and serum starvation (19,20), whereas FFAs block proliferation and cause apoptosis in nutrient-stimulatory conditions (18,21). Studies addressing this question in vivo have mostly concluded that FFAs do not limit β-cell proliferation (22–25). However, no in vivo study has yet systematically evaluated the effect of high FFAs on β-cell proliferation in both control and stimulated conditions.
On the basis of work by others in rats (24,26,27), we previously developed a 4-day glucose infusion model in mice and showed that hyperglycemia stimulates both mouse and human β-cell proliferation in vivo (28–30). We have now used our infusion hyperglycemia model to test whether FFAs alter mouse β-cell proliferation in vivo in both basal and glucose-stimulatory conditions. Our findings illustrate a novel form of in vivo glucolipotoxicity: FFAs block glucose-mediated adaptive β-cell proliferation via induction of cell cycle inhibitors p16 and p18.
RESEARCH DESIGN AND METHODS
Surgical catheterization.
Mouse studies were approved by the University of Pittsburgh Institutional Animal Care and Use Committee. Mice were housed in controlled temperature, humidity, and 12-h light-dark cycle with free access to chow and water. Detailed protocols for surgical catheterization and blood sampling can be found in the online supplement to Alonso et al. (28). Ten- to twelve-week-old male C57BL/6J mice were anesthetized with inhaled 2% isoflurane, and microrenathane catheters (MRE-025; Braintree Scientific) were inserted into the left femoral artery and vein, tunneled subcutaneously to exit the skin at the upper back, taped to a wire attached to posterior cervical muscles (792500; A-M Systems), and connected to a 360° dual channel swivel (375/D/22QM; Instech). Catheter patency was maintained by continuous 7 μL/h infusion of sterile saline containing 20 units/mL unfractionated heparin (APP Pharmaceuticals) using a syringe pump (R99-EM; Razel Scientific Instruments).
Intravenous infusions.
Intravenous infusions were begun 3 days after catheterization (Fig. 1A). All blood samples were taken from the arterial catheter in unhandled, awake mice; infusions were via the venous catheter. Chow was provided throughout the experiment. Nonfasting morning arterial blood samples were taken at time 0, and at 8, 24, 48, 72, and 96 h. Glucose was measured on whole blood, plasma was frozen for future measurement of insulin, and RBCs were resuspended in 20 μL saline containing 100 units/mL heparin and reinfused. After the time 0 blood sample, the infusions were started: SAL (0.9% saline, 200 μL/h), LIP (Liposyn II 20%, 100 μL/h plus 0.9% saline, 100 μL/h), GLU (50% dextrose, 100 μL/h plus 0.9% saline, 100 μL/h), or L+G (Liposyn II, 100 μL/h plus 50% dextrose, 100 μL/h). All infusates contained heparin (2 units/h) and bromodeoxyuridine (BrdU, 100 μg/h). Immediately following infusion, mice were killed and organs dissected for histological analyses or islets isolated for molecular analyses.
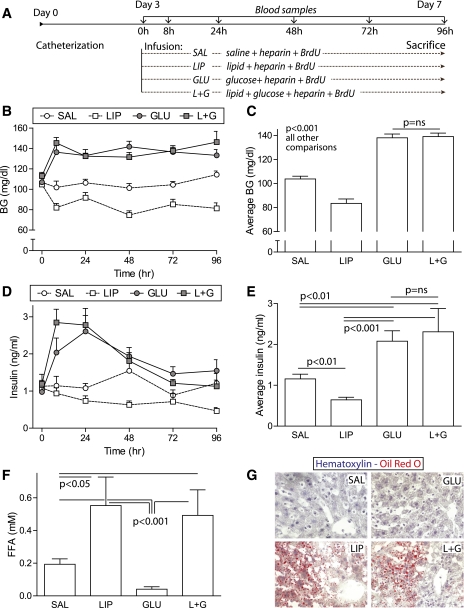
FIG. 1.
Intravenous lipid infusion elevated FFA levels in both basal and hyperglycemic conditions. A: Timeline: mice with femoral artery and vein catheters received continuous intravenous 4-day infusions of 0.9% saline, Liposyn II, 50% glucose, or Liposyn II plus 50% glucose. Arterial blood was sampled daily. B and C: Glucose infusion elevated blood glucose (BG) levels consistently to moderate levels; coinfusion of lipid did not alter the degree of hyperglycemia (n = 26–34). D and E: Glucose infusion transiently elevated plasma insulin levels; coinfusion of lipid did not alter the degree of hyperinsulinemia (n = 13–15). F: Lipid infusion increased plasma FFA levels to a similar degree with and without coinfusion of glucose (n = 7–13). G: Oil Red O stain of liver showed end-organ lipid deposition in mice receiving intravenous Liposyn II. Data are mean ± SEM; P values by ANOVA. ns, nonsignificant. (A high-quality digital representation of this figure is available in the online issue.)
Biochemical assays.
Blood glucose was measured using an Ascencia XL glucometer. Plasma insulin was measured by radioimmunoassay (Linco sensitive rat insulin RIA kit; Millipore). FFAs were measured by colorimetric assay (Roche) on terminal blood samples obtained by cardiac puncture into prechilled tubes on ice.
Histological analyses.
Pancreata were fixed in Bouin’s fixative for 4 h and paraffin embedded. TUNEL, BrdU, and cyclin D2 staining were performed as described (28). For Oil Red O, livers were frozen in optimal cutting temperature compound; 10 μm cryosections were fixed in formalin, rinsed in 60% isopropanol, stained 15 min with 0.3% Oil Red O in 60% isopropanol, and hematoxylin counterstained. For proliferating cell nuclear antigen (PCNA) and Ki67 staining, paraffin sections were blocked in 1% BSA/5% goat serum/0.1% triton X-100, incubated overnight at 4°C with anti-PCNA (1:500; Santa Cruz Biotechnology) or anti-Ki67 (1:200; Neomarkers) and anti-insulin (1:500, Dako), incubated 30 min with secondary antibodies, and mounted with Hoechst. The number of β-cells quantified was as follows: 2,147 ± 116 (BrdU), 1,814 ± 144 (TUNEL), 1,675 ± 147 (PCNA), and 1,970 ± 204 (Ki67). Microscopy was performed using an Olympus Fluoview confocal microscope or an Olympus Provis microscope.
Islet experiments.
Islets were isolated by ductal collagenase injection and Ficoll separation (28). For immunoblot, islets were washed in PBS containing 100 nmol/L sodium orthovanadate immediately after isolation and frozen for future analysis. For islet cell culture experiments, trypsinized islet cells were plated on glass coverslips in RPMI containing 10% FBS and penicillin/streptomycin (islet medium) containing 5.5 mmol/L glucose. Dispersed islet cells were cultured for 72 h in islet medium containing 2 mmol/L or 15 mmol/L glucose, with either 0.5% BSA or 0.4 mmol/L FFAs conjugated to 0.5% BSA (19); BrdU was added for the final 24 h.
Cultured insulinoma cell experiments.
Rat insulinoma (INS-1) cells (kindly provided by Doris Stoffers, University of Pennsylvania) were cultured in INS-1 medium: RPMI with 10% FBS, 11 mmol/L glucose, 10 mmol/L HEPES, 2 mmol/L l-glutamine, 1 mmol/L sodium pyruvate, penicillin/streptomycin, and 50 μmol/L β-mercaptoethanol. For proliferation analyses, INS-1 cells were plated on coverslips, then cultured for 24 h in INS-1 medium containing 2 or 11 mmol/L glucose and 0.5% BSA or 0.4 mmol/L linoleic, oleic, or palmitic acid, or a mixture containing 7:2:1 linoleic:oleic:palmitic acid, all conjugated to 0.5% BSA. BrdU was added for the final hour of culture; cells fixed in 4% paraformaldehyde were immunostained for BrdU and Hoechst as above except antigen retrieval was by DNAse. For immunoblots, INS-1 cells were cultured in INS-1 medium with 0.5% BSA or BSA-conjugated FFAs for 24 h. For small interfering RNA (siRNA) experiments, siRNA pools (Dharmacon) targeting rat p16 or p18 were applied at 100 nmol/L for 24 h prior to proliferation assay or immunoblot.
Immunoblots.
Whole islets or INS-1 cells were sonicated in lysis buffer containing 125 mmol/L Tris pH 6.8, 2% SDS, 1 mmol/L dithiothreitol, 20 μg/mL 4-Amidinophenylmethanesulfonyl fluoride hydrochloride (APMSF), and protease inhibitors; separated by SDS-PAGE; transferred to nitrocellulose; and blocked in 5% milk/PBS Tween. Antibodies include cyclin D2 (Neomarkers), p16, p18, p21 (Santa Cruz Biotechnology), p27 (BD Pharmingen), tubulin (Calbiochem), anti-mouse and anti-rabbit (Jackson ImmunoResearch). Data were collected on film by ECL or ECL+ (Amersham Pharmacia Biotech).
Statistical analyses.
Data are expressed as mean ± SE. All statistical analyses were performed using Prism (GraphPad Software). P values were calculated by two-tailed Student t test when two groups were compared, by one-way ANOVA with Newman-Keuls post hoc analysis when more than two groups were compared, using log-transformed data when Bartlett test showed P < 0.01 for the variance among groups to be unequal, or by linear regression when two continuous variables were tested for interaction. P < 0.05 was considered significant.
RESULTS
Lipid infusion increases circulating FFAs in basal and glucose-stimulated conditions.
To test whether FFAs alter glucose-stimulated β-cell proliferation, mice were intravenously infused continuously for 4 days (Fig. 1A) with saline (SAL), Liposyn II (LIP), glucose (GLU) or Liposyn II and glucose (L+G). Glucose infusion resulted in a moderate, sustained elevation in blood glucose (Fig. 1B), to a degree previously shown to stimulate β-cell proliferation (28). Although infusion of lipid alone (LIP) reduced blood glucose, coinfusion of lipid with glucose (L+G) did not alter blood glucose relative to glucose alone (GLU). Comparison of average blood glucose over the 4-day infusion (Fig. 1C) showed that GLU and L+G mice had similar average circulating glucose levels, significantly higher than SAL and LIP mice.
Plasma insulin levels were transiently elevated in GLU and L+G mice relative to SAL and LIP mice (Fig. 1D). Average insulin levels over the 4-day infusion were significantly higher in GLU and L+G mice than SAL controls (Fig. 1E). Average plasma insulin levels did not differ between GLU and L+G mice.
Lipid infusion increased plasma FFA levels equivalently in LIP and L+G mice to levels higher than those measured in SAL and GLU mice (Fig. 1F). Hepatic steatosis was readily apparent in LIP and L+G mice, confirming lipid delivery to tissues (Fig. 1G). Therefore, continuous intravenous infusion of lipids successfully elevated FFA levels under control and glucose-stimulated conditions.
Elevated FFAs do not increase β-cell death in vivo in the context of mild hyperglycemia.
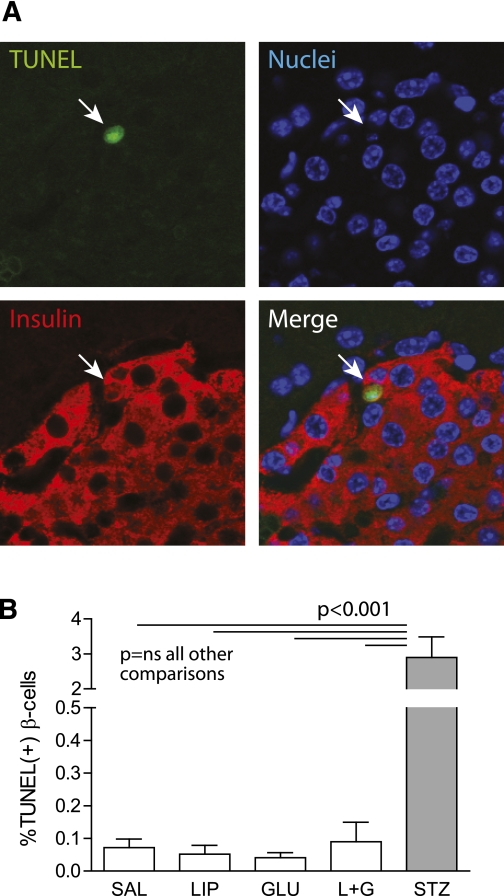
Decades of work from multiple investigators has produced incontrovertible evidence that FFAs cause β-cell death in vitro when glucose levels are also elevated (11). To determine whether 4-day infusion of lipids and glucose increased β-cell death in vivo, sections from pancreata obtained after infusion were analyzed for cell death by TUNEL staining (Fig. 2A). Although cell death was readily detectable in positive control sections, cell death was rare in L+G sections and was not increased over the other groups (Fig. 2B).
FIG. 2.
Four days of elevated FFAs did not increase β-cell death in vivo. Pancreas sections obtained after 4-day infusion were stained for TUNEL (green), insulin (red), and Hoechst (blue). A: Positive control sections obtained by injecting a mouse with streptozotocin 50 mg/kg i.p. and killing them 16 h later showed readily detectable TUNEL staining. B: Elevated FFAs did not increase β-cell TUNEL staining in either basal (LIP) or mildly hyperglycemic (L+G) conditions (n = 7–11). Data are mean ± SEM; P values by ANOVA. (A high-quality digital representation of this figure is available in the online issue.)
FFAs block glucose-stimulated β-cell proliferation in vivo in mice.
β-Cell proliferation was measured using histochemistry on pancreas sections after infusion (Fig. 3A and B). To learn whether elevating FFAs altered β-cell proliferation under basal conditions, LIP and SAL mice were compared. Cells costained for insulin and BrdU were present at similar frequency in sections from LIP and SAL mice, suggesting that, under basal conditions, elevation of FFAs neither increased nor decreased cumulative β-cell proliferation (Fig. 3C).
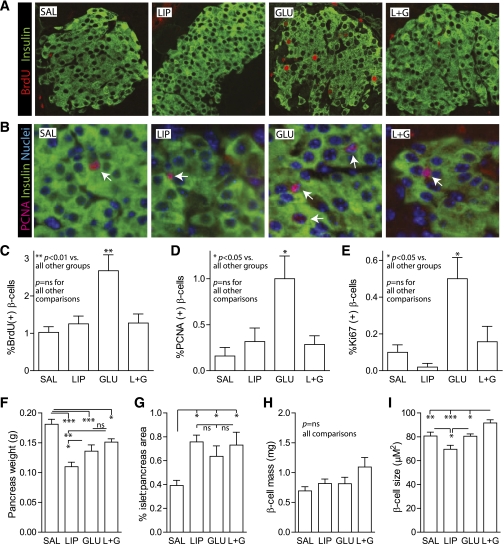
FIG. 3.
FFAs blocked glucose-stimulated β-cell proliferation in vivo in mice. A and B: Pancreas sections obtained after infusion were immunostained for insulin (green) and BrdU (red) (A) or for insulin (green), PCNA (red), and Hoechst (blue) (B). C–E: Quantification of β-cell BrdU (C), PCNA (D), and Ki67 (E) staining confirmed that glucose increased proliferation (GLU vs. SAL). Elevated FFAs did not alter basal proliferation (LIP vs. SAL) but blocked glucose-stimulated (L+G vs. GLU) proliferation. F–H: β-Cell mass, the product of pancreas weight (F) and % islet area (G) was not statistically different in any of the groups (H). I: The cross-sectional area of individual β-cells was reduced in LIP mice and increased in L+G mice. Data are mean ± SEM; P values by ANOVA. ns, nonsignificant. *P < 0.05; **P < 0.01; ***P < 0.001. (A high-quality digital representation of this figure is available in the online issue.)
As expected (28), moderate continuous 4-day hyperglycemia increased β-cell proliferation in GLU mice (Fig. 3C). To determine whether FFAs alter proliferation under glucose-stimulatory conditions, L+G mice were compared with GLU mice. As measured by BrdU incorporation, β-cell proliferation was lower in L+G mice than GLU mice (Fig. 3C), equivalent to SAL and LIP controls, despite having similar blood glucose and plasma insulin levels to GLU mice (Fig. 1B–E). These data suggest that circulating FFAs have antiproliferative effects on β-cells under glucose-stimulatory conditions in vivo.
To confirm the antiproliferative effect of lipid infusion in vivo, β-cell replication was measured by immunostaining for cell-cycle indicators PCNA and Ki67. These markers measure proliferation at the time of death rather than cumulatively over the 4-day infusion. For both PCNA and Ki67, the percent β-cells immunoreactive for both proliferation and insulin was not different between SAL and LIP mice, but was significantly higher in GLU mice than L+G mice, confirming that lipid infusion did not alter β-cell proliferation under basal conditions but blocked glucose-induced proliferation (Fig. 3D and E). Over the 4-day infusion, β-cell mass was not significantly altered in any of the groups (Fig. 3F–H); intriguingly, the cross-sectional area of individual β-cells was smaller in LIP mice and larger in L+G mice (Fig. 3I).
FFAs block glucose-stimulated β-cell proliferation in vitro.
The antiproliferative effects of lipid infusion on β-cells could result indirectly from effects on other tissues and could result from mediators other than FFAs. To find out whether FFAs have the capacity to block glucose-stimulated β-cell proliferation directly, primary mouse islet cells were cultured in low (2 mmol/L) or high (15 mmol/L) glucose with BSA control or high glucose in the presence of BSA-conjugated FFAs. The FFA mixture, engineered to mimic the fatty acid content of Liposyn II, contained a 7:2:1 ratio of linoleic, oleic, and palmitic acids. β-Cell proliferation was readily detectable and was more frequent in high glucose (Fig. 4A). Quantification confirmed that glucose increased primary β-cell proliferation (Fig. 4B). Importantly, treatment with the FFA mixture blocked glucose-stimulated β-cell proliferation in vitro, confirming that FFAs exert antiproliferative effects directly on primary islet cell cultures.
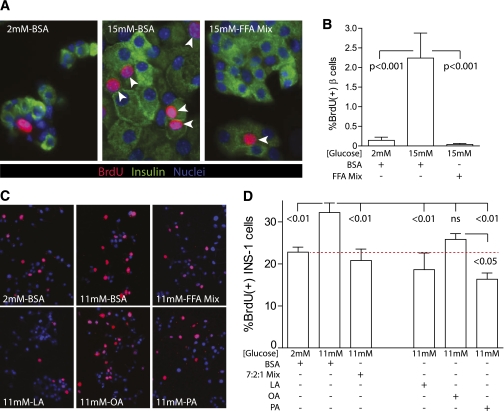
FIG. 4.
Linoleic acid and palmitic acid inhibit β-cell proliferation in vitro. A: Primary mouse islet cells were cultured for 72 h in low (2 mmol/L) or high (15 mmol/L) glucose in the presence of either BSA control or a FFA mixture designed to mimic the components of Liposyn II (7:2:1 linoleic:oleic:palmitic acids) conjugated to BSA; proliferation was measured by immunostaining for BrdU (red), insulin (green), and Hoechst (blue). B: Quantification showed that glucose increased β-cell proliferation; glucose-induced proliferation was blocked by addition of FFAs (n = 7–10). C and D: INS-1 cells cultured for 24 h with BSA or FFAs also showed that the FFA mixture blocked glucose-induced proliferation. Culturing INS-1 cells with the individual components of the FFA mixture indicated that both linoleic and palmitic acids blocked proliferation in high glucose; the reduction by oleic acid was nonsignificant (n = 4–5). Mean ± SEM; P values by ANOVA. (A high-quality digital representation of this figure is available in the online issue.)
FFAs might act on other cell types within primary islet cell cultures, such as other endocrine cells or fibroblasts, which could send secondary antiproliferative signals to the β-cell. To determine whether FFAs act directly on β-cells, a β-cell–derived transformed cell line (INS-1) was cultured in low or high glucose with BSA control or FFA mixture, and proliferation was measured (Fig. 4C). Basal proliferation was frequent in this cell line. However, glucose significantly increased proliferation above baseline, and again, the FFA mixture blocked the glucose-dependent increase in proliferation (Fig. 4D).
To learn which component of the FFA mixture exerted antiproliferative effects on β-cells, INS-1 cells were cultured in high glucose with each of the individual component FFAs. Quantification revealed that both linoleic and palmitic acids blocked proliferation in high glucose; the reduction by oleic acid treatment was nonsignificant (Fig. 4D). Therefore, FFAs, specifically linoleic and palmitic acids, act directly on the β-cell to block glucose-induced proliferation.
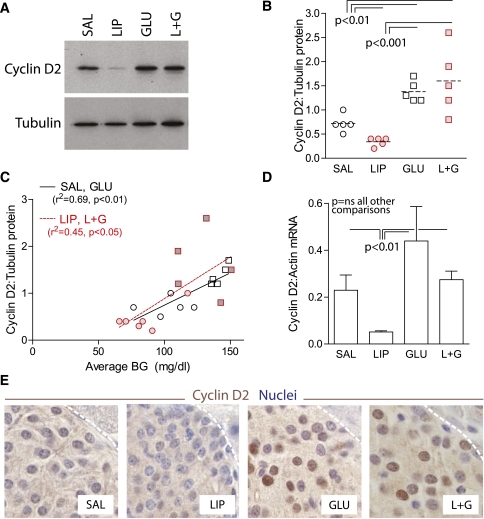
FFAs do not prevent glucose-mediated induction of islet cyclin D2 protein.
Cyclin D2, an important regulator of rodent β-cell proliferation (31–35), is upregulated and relocates to the nucleus in response to hyperglycemia (28). We hypothesized that FFAs might interfere with glucose-mediated cyclin D2 protein induction or nuclear localization. To determine whether FFAs blocked the increase in cyclin D2 expression in islets in response to hyperglycemia in vivo, islets were isolated after 4-day infusion and subjected to immunoblot. Unexpectedly, although islet cyclin D2 levels were lower in LIP mice than SAL controls, cyclin D2 protein upregulation in GLU mice was unaffected by coinfusion of lipid (Fig. 5A and B). When islet cyclin D2 protein expression by immunoblot was analyzed in the context of prevailing average blood glucose levels during infusion in mice without lipid exposure (SAL or GLU), a significant positive correlation was observed (Fig. 5C). Supporting the concept that FFAs did not alter glucose induction of islet cyclin D2 protein, a similar positive correlation between blood glucose and cyclin D2 expression was observed in mice with lipid exposure (LIP or L+G; Fig. 5C). As observed previously (28), the increase in cyclin D2 by hyperglycemia appeared to be mediated posttranslationally, since cyclin D2 mRNA was not significantly increased in GLU mice relative to SAL mice (Fig. 5D). Although lipid infusion reduced cyclin D2 mRNA levels under low-glucose conditions, lipids did not significantly lower cyclin D2 mRNA expression under glucose-stimulatory conditions. In sum, elevating FFA levels in vivo did not prevent glucose-mediated induction of cyclin D2 protein.
FIG. 5.
FFAs did not prevent glucose-mediated induction of islet cyclin D2 protein in vivo. A and B: Immunoblot of islets isolated after 4-day infusion showed that cyclin D2 protein was increased by hyperglycemia with or without elevated FFAs; data are quantified (B); n = 5–6. One point was excluded from the LIP group on the basis of abnormally high blood glucose (BG) in this mouse. C: A positive correlation was observed between islet cyclin D2 expression by immunoblot and average blood glucose during the preceding 4-day infusion, both in the absence (SAL and GLU; open symbols) and presence (LIP and L+G; shaded symbols) of FFAs. D: Islet cyclin D2 mRNA was not induced by glucose infusion, and there was no effect of coinfusion of lipids, although cyclin D2 mRNA levels were significantly lower in islets isolated from mice infused with lipid alone (n = 3–4). E: Immunostaining of pancreas sections after infusion showed that coinfusion of lipid did not prevent nuclear accumulation of cyclin D2 induced by glucose. Data are mean ± SEM; P values by ANOVA. ns, nonsignificant. (A high-quality digital representation of this figure is available in the online issue.)
To find out whether FFA exposure might block proliferation by preventing cyclin D2 from relocalizing to the nucleus in response to hyperglycemia, pancreas sections from infused mice were immunostained for cyclin D2 (Fig. 5E). In fact, cyclin D2 protein was readily detectible in islet nuclei from L+G mice, suggesting that FFAs did not block nuclear localization, but might, instead, act downstream of cyclin D2 to reduce proliferation.
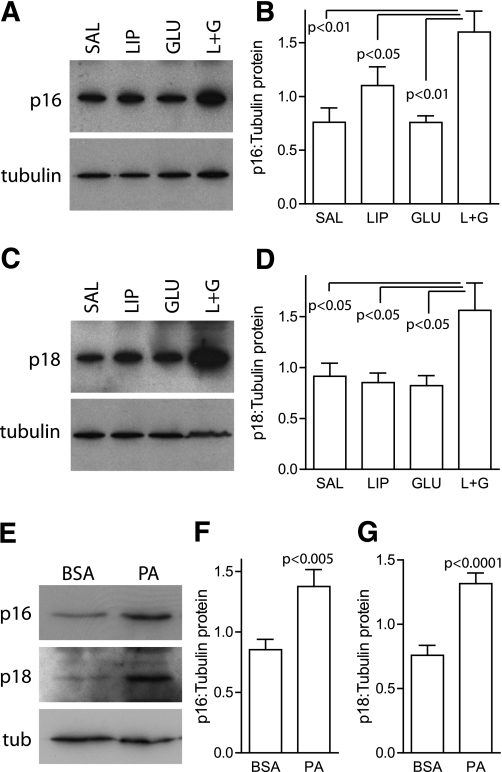
FFAs increase β-cell expression of cell cycle inhibitors p16 and p18, both in vivo and in vitro.
D-cyclins bind to and activate cyclin-dependent kinase (Cdk) -4 and -6, which regulate entry into the G1-S transition of the cell cycle (36,37). Cell cycle inhibitors act downstream of D-cyclins to block cell cycle progression; both cyclin inhibitory protein/kinase inhibitory protein (Cip/Kip) inhibitors p21/p27 and INK4 family members p16/p18 are known to regulate proliferation in β-cells (31,38–43). We hypothesized that FFAs might block proliferation by inducing expression of cell cycle inhibitors. Immunoblot of islets isolated after infusion showed that neither p21 nor p27 were significantly induced in L+G islets (data not shown). However, both p16 (Fig. 6A and B) and p18 (Fig. 6C and D) were significantly induced at the protein level in islets isolated from L+G mice, relative to all other groups. To confirm that FFAs increase cell cycle inhibitor expression in β-cells directly, INS-1 cells were treated with fatty acids and subjected to immunoblot. Although the linoleic:oleic:palmitic mixture did not increase expression of either p16 or p18, possibly because of a protective effect of oleate in INS-1 cells, treatment with palmitic acid alone induced both p16 and p18 protein expression (Fig. 6E–G). Therefore, the antiproliferative effect of FFAs in vivo and in vitro may be mediated by induction of cell cycle inhibitors p16 and p18, which act to block the cell cycle downstream of D-cyclins.
FIG. 6.
Cell cycle inhibitors p16 and p18 are induced in β-cells by FFAs in combination with high glucose. Islets isolated after infusion showed increased expression of p16 (A) (n = 5–6; data are quantified [B]) and p18 (C) (n = 5–6; data are quantified [D]), only in mice infused with both lipids and glucose. E–G: INS-1 cells cultured with glucose and BSA control or BSA-conjugated palmitic acid had increased expression of both p16 and p18 by immunoblot (E); data are quantified (F–G), n = 12–13. Data are mean ± SEM; P values by ANOVA (B and D) and by t test (F–G).
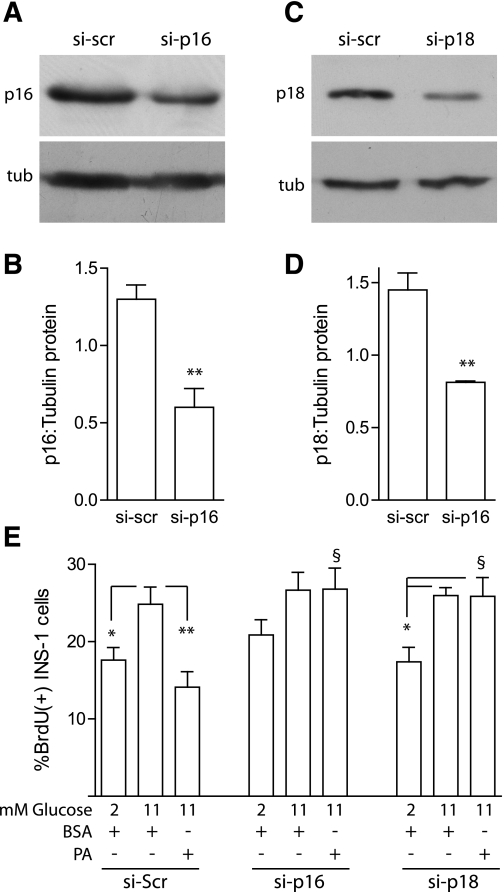
Both p16 and p18 are required for the antiproliferative effect of FFAs.
To find out whether either p16 or p18 was required for FFAs to block proliferation, a knockdown approach was used. INS-1 cells treated with siRNA directed against either p16 (Fig. 7A and B) or p18 (Fig. 7C and D) showed a modest but significant knockdown of each inhibitor relative to scrambled control siRNA. When INS-1 cell proliferation was measured in the presence of scrambled siRNA, glucose-induced proliferation was blocked by palmitic acid (Fig. 7E) as seen in prior experiments (Fig. 4D). Intriguingly, knockdown of either p16 or p18 completely eliminated the antiproliferative effect of palmitic acid in INS-1 cells, suggesting that both p16 and p18 may be required for FFAs to block β-cell proliferation.
FIG. 7.
Both p16 and p18 are required for the antiproliferative effects of FFAs. By immunoblot, INS-1 cells treated with siRNA directed against p16 (si-p16; A and B) or p18 (si-p18; C and D) had reduced expression of the targeted proteins relative to siRNA targeting nonspecific sequence (si-scr), n = 3–4. E: INS-1 cells treated with scramble siRNA again showed that palmitic acid blocked proliferation in high glucose, but knockdown of either p16 or p18 rescued the antiproliferative effects of palmitic acid. Mean ± SEM; P values by t test (C and D) and by ANOVA (E). *P < 0.05; **P < 0.01; §P < 0.01 vs. si-Scr 11 mmol/L-PA. tub, tubulin.
DISCUSSION
These studies describe a new form of in vivo lipotoxicity: inhibition of glucose-stimulated β-cell proliferation. If FFAs restrict β-cell proliferation in response to other stimuli, such as obesity and insulin resistance, this process could influence β-cell mass accrual and type 2 diabetes risk. This finding could also be relevant to type 1 diabetes; when immune-protective tools become sufficiently developed to pursue β-cell regenerative treatments, the elevated FFAs that occur with acute insulin insufficiency could impair the β-cell proliferative response to treatment.
Strengths of this study include the use of a carefully controlled intravenous infusion system to directly assess the impact of elevating FFAs under basal and proliferation-stimulatory conditions in vivo, in vitro studies to verify that FFAs act directly on the β-cell, and the novel identification of two cell cycle inhibitors required for the antiproliferative effect. Our infusion system allows manipulation of a single variable in an in vivo setting; interventions such as genetic alteration or diet-induced obesity introduce multiple variables. Although it is not yet known whether the mechanism of adaptive β-cell proliferation in response to hyperglycemia is similar to obesity or insulin resistance, various parallels, such as increased insulin secretory load on the β-cell, downstream signals such as insulin receptor substrate 2 and cyclin D2, and a role for intracellular glucose metabolism in obesity-related proliferation, suggest areas of potential overlap (4,7,10,28,35).
Although an antiproliferative effect of FFAs on β-cells has been hypothesized for a decade (17) and was observed in vitro (18,21), in vivo evidence to date has not supported this hypothesis (22–25). An interesting distinction raised by our data set is the difference between basal- and proliferation-stimulated settings. Our findings suggest that FFAs do not alter basal proliferation, but prevent glucose-stimulated proliferation. Several experiments have observed a proproliferative effect of FFAs on β-cells under basal nutrient conditions, both in vitro (19,20) and in vivo (24). In our experiments, glucose and insulin levels were lower in LIP mice than SAL mice, possibly due to reduced chow intake and lower overall caloric and carbohydrate load in this group, raising the possibility that a proproliferative effect of lipids in the basal state was counteracted by an antiproliferative effect of hypoglycemia, hypoinsulinemia, or undernutrition.
Several studies have examined the effect of elevated lipids on β-cell proliferation in rats; however, none allows direct comparison of stimulated proliferation without and with elevated FFAs. One important study found robust β-cell mass recovery after pancreatectomy in Zucker fatty rats, which have elevated plasma lipids (22). However, β-cell proliferation was not increased by pancreatectomy, and islet neogenesis was thought to be responsible for the β-cell mass expansion, limiting conclusions regarding the effect of FFAs on β-cell proliferation. Three studies have measured β-cell proliferation in rats after intravenous infusion of lipids. In one, lipid effects on proliferation were examined only in the unstimulated state (24). In the second, cyclical glucose exposure did not induce proliferation, preventing conclusions regarding the effect of cyclical FFA exposure on stimulated proliferation (25). In the third study, lipids were continuously coinfused with glucose into 2- or 6-month-old rats for 72 h (23). Intriguingly, β-cell proliferation in L+G rats was equivalent to saline controls at 2 months of age, similar to our present mouse data, but was increased relative to saline controls at 6 months of age. Since a glucose-alone control was not presented, effects of coinfusion of lipid on glucose-stimulated proliferation cannot be inferred. Therefore, our study is the first to isolate lipids as a variable and compare in vivo stimulated β-cell proliferation in low and high FFA states.
Acute elevation of FFAs causes insulin resistance (rev. in 15); insulin resistance is a potent stimulus for β-cell proliferation (35). Although we have not measured insulin sensitivity in this study, the antiproliferative effect of FFAs cannot be related to changes in peripheral insulin resistance, because the effect occurs when β-cells are exposed to FFAs in culture and because insulin resistance would be expected to increase rather than decrease β-cell proliferation. The intriguing hypothesis that FFAs might induce insulin resistance at the level of the β-cell, and thereby block a proliferative effect of insulin, remains to be tested. Since the proliferative effect of glucose requires glucose metabolism (8), the observed negative impact of lipids on glucose-induced proliferation may be related to the metabolic impact of FFAs, which includes inhibition of glucose oxidation (16,44).
At first glance, an antiproliferative effect of FFAs seems inconsistent with the marked proproliferative effect of high-fat diet exposure. However, overnutrition is associated with other potent proliferation drivers (4). Elevated circulating FFA levels are not a consistent feature of early, compensated high-fat diet exposure, since insulin potently suppresses lipolysis (45). Teleogically, one might predict no evolutionary pressure to expand β-cell mass in the setting of high FFAs, which would occur during nutrient deprivation on a hunter-gatherer diet.
β-Cell death was not increased by combined hyperglycemia and FFAs in vivo in our model. This may be due to the degree of hyperglycemia, which is lower than glucose concentrations used to elicit glucolipotoxicity in vitro (11), or to the timing. The deleterious effects of FFAs on β-cells vary with exposure duration (11); 4 days represents an intermediate duration which may produce different effects than either acute or chronic exposure.
How FFAs increase expression of INK4 family cell cycle inhibitors remains unknown; however, the observation that genomic polymorphisms near the p16 locus predict risk of type 2 diabetes adds importance to our finding (46). Peroxisome proliferator–activated receptors, nuclear receptors activated by lipids, increase p16 expression in mesenchymal cells (47). Intriguingly, p16 is a primary mediator of senescence, and senescence was observed in β-cells after prolonged high-fat diet exposure (48). On the other hand, after 8 weeks of high-fat diet, at a time when obesity- or insulin resistance–mediated β-cell proliferation was markedly increased, islet p16 levels were reduced (49). Future studies are needed to dissect the mechanisms of the antiproliferative effect of FFAs.
Surprisingly, knockdown of either p16 or p18 was sufficient to relieve proliferation repression by FFAs, suggesting that both are required for the antiproliferative effect. We speculate that signaling downstream of p16 and p18 interacts in such a way that reduction of one disallows action of the other, resulting in the apparent requirement for both. Intriguingly, glucose-stimulated proliferation lost statistical significance in INS-1 cells after p16 knockdown, suggesting a possible basal suppression of proliferation in low glucose by p16. Based on the modest increase in INK4 expression by palmitate and the modest reduction by siRNA, it seems that relatively small changes in cellular INK4 content are able to significantly influence the rate of proliferation. In mice, loss of either p16 or p18 is compensated by the presence of the other, as measured by islet cell proliferation under basal conditions (50). Future experiments will determine whether both p16 and p18 are required for the antiproliferative effect of FFAs in β-cells in vivo.
In conclusion, modest elevations of FFAs and glucose cause in vivo glucolipotoxicity with respect to adaptive β-cell proliferation. If FFAs also restrict proliferation in response to obesity and insulin resistance, this may be an important mechanism driving failure of β-cell mass expansion in prediabetes. A logical extension of our findings is to speculate that the antiproliferative effect of FFAs might represent the elusive connection between p16 and genetic risk of type 2 diabetes. It is our hope that this work leads to therapeutic interventions that expand β-cell mass to prevent diabetes.
ACKNOWLEDGMENTS
This work was supported by National Institutes of Health grants HL063767 (C.P.O.), DK067351 and DK077096 (A.G.-O.), DK076562 and DK046204 (L.C.A.), and by American Diabetes Association grant 7-11-BS-04 (L.C.A.).
No potential conflicts of interest relevant to this article were reported.
J.P., D.H., R.S., and M.A. performed the experiments. L.C.R. efficiently organized the mouse infusion room. B.Z. catheterized the mice. C.P.O. and A.G.-O. contributed to discussion and revised the manuscript. L.C.A. conceived and directed the experiments, contributed to data collection, and wrote and revised the manuscript.
The authors thank Andrew Stewart, Rupangi Vasavada, Don Scott, and Robert O’Doherty, from the University of Pittsburgh, for their thoughtful input.
Footnotes
J.P., D.H., and R.S. contributed equally to this work.
See accompanying commentary, p. 560.
REFERENCES
- 1.Butler AE, Janson J, Bonner-Weir S, Ritzel R, Rizza RA, Butler PC. Beta-cell deficit and increased beta-cell apoptosis in humans with type 2 diabetes. Diabetes 2003;52:102–110 [DOI] [PubMed] [Google Scholar]
- 2.Lorenzo C, Wagenknecht LE, Rewers MJ, et al. Disposition index, glucose effectiveness, and conversion to type 2 diabetes: the Insulin Resistance Atherosclerosis Study (IRAS). Diabetes Care 2010;33:2098–2103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ritzel RA, Butler AE, Rizza RA, Veldhuis JD, Butler PC. Relationship between beta-cell mass and fasting blood glucose concentration in humans. Diabetes Care 2006;29:717–718 [DOI] [PubMed] [Google Scholar]
- 4.Sachdeva MM, Stoffers DA. Minireview: Meeting the demand for insulin: molecular mechanisms of adaptive postnatal beta-cell mass expansion. Mol Endocrinol 2009;23:747–758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hosokawa H, Hosokawa YA, Leahy JL. Upregulated hexokinase activity in isolated islets from diabetic 90% pancreatectomized rats. Diabetes 1995;44:1328–1333 [DOI] [PubMed] [Google Scholar]
- 6.Liu YQ, Han J, Epstein PN, Long YS. Enhanced rat beta-cell proliferation in 60% pancreatectomized islets by increased glucose metabolic flux through pyruvate carboxylase pathway. Am J Physiol Endocrinol Metab 2005;288:E471–E478 [DOI] [PubMed] [Google Scholar]
- 7.Terauchi Y, Takamoto I, Kubota N, et al. Glucokinase and IRS-2 are required for compensatory beta cell hyperplasia in response to high-fat diet-induced insulin resistance. J Clin Invest 2007;117:246–257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Porat S, Weinberg-Corem N, Tornovsky-Babaey S, et al. Control of pancreatic β cell regeneration by glucose metabolism. Cell Metab 2011;13:440–449 [DOI] [PubMed] [Google Scholar]
- 9.Weir GC, Bonner-Weir S. A dominant role for glucose in beta cell compensation of insulin resistance. J Clin Invest 2007;117:81–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu YQ, Jetton TL, Leahy JL. Beta-Cell adaptation to insulin resistance. Increased pyruvate carboxylase and malate-pyruvate shuttle activity in islets of nondiabetic Zucker fatty rats. J Biol Chem 2002;277:39163–39168 [DOI] [PubMed] [Google Scholar]
- 11.Poitout V, Robertson RP. Glucolipotoxicity: fuel excess and beta-cell dysfunction. Endocr Rev 2008;29:351–366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Charles MA, Eschwège E, Thibult N, et al. The role of non-esterified fatty acids in the deterioration of glucose tolerance in Caucasian subjects: results of the Paris Prospective Study. Diabetologia 1997;40:1101–1106 [DOI] [PubMed] [Google Scholar]
- 13.Paolisso G, Tataranni PA, Foley JE, Bogardus C, Howard BV, Ravussin E. A high concentration of fasting plasma non-esterified fatty acids is a risk factor for the development of NIDDM. Diabetologia 1995;38:1213–1217 [DOI] [PubMed] [Google Scholar]
- 14.Milburn JL, Jr, Hirose H, Lee YH, et al. Pancreatic beta-cells in obesity. Evidence for induction of functional, morphologic, and metabolic abnormalities by increased long chain fatty acids. J Biol Chem 1995;270:1295–1299 [DOI] [PubMed] [Google Scholar]
- 15.Samuel VT, Petersen KF, Shulman GI. Lipid-induced insulin resistance: unravelling the mechanism. Lancet 2010;375:2267–2277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prentki M, Madiraju SR. Glycerolipid metabolism and signaling in health and disease. Endocr Rev 2008;29:647–676 [DOI] [PubMed] [Google Scholar]
- 17.Rhodes CJ. IGF-I and GH post-receptor signaling mechanisms for pancreatic beta-cell replication. J Mol Endocrinol 2000;24:303–311 [DOI] [PubMed] [Google Scholar]
- 18.Cousin SP, Hügl SR, Wrede CE, Kajio H, Myers MG, Jr, Rhodes CJ. Free fatty acid-induced inhibition of glucose and insulin-like growth factor I-induced deoxyribonucleic acid synthesis in the pancreatic beta-cell line INS-1. Endocrinology 2001;142:229–240 [DOI] [PubMed] [Google Scholar]
- 19.González-Pertusa JA, Dubé J, Valle SR, et al. Novel proapoptotic effect of hepatocyte growth factor: synergy with palmitate to cause pancreatic beta-cell apoptosis. Endocrinology 2010;151:1487–1498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brelje TC, Bhagroo NV, Stout LE, Sorenson RL. Beneficial effects of lipids and prolactin on insulin secretion and beta-cell proliferation: a role for lipids in the adaptation of islets to pregnancy. J Endocrinol 2008;197:265–276 [DOI] [PubMed] [Google Scholar]
- 21.Maedler K, Oberholzer J, Bucher P, Spinas GA, Donath MY. Monounsaturated fatty acids prevent the deleterious effects of palmitate and high glucose on human pancreatic beta-cell turnover and function. Diabetes 2003;52:726–733 [DOI] [PubMed] [Google Scholar]
- 22.Delghingaro-Augusto V, Nolan CJ, Gupta D, et al. Islet beta cell failure in the 60% pancreatectomised obese hyperlipidaemic Zucker fatty rat: severe dysfunction with altered glycerolipid metabolism without steatosis or a falling beta cell mass. Diabetologia 2009;52:1122–1132 [DOI] [PubMed] [Google Scholar]
- 23.Fontés G, Zarrouki B, Hagman DK, et al. Glucolipotoxicity age-dependently impairs beta cell function in rats despite a marked increase in beta cell mass. Diabetologia 2010;53:2369–2379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Steil GM, Trivedi N, Jonas JC, et al. Adaptation of beta-cell mass to substrate oversupply: enhanced function with normal gene expression. Am J Physiol Endocrinol Metab 2001;280:E788–E796 [DOI] [PubMed] [Google Scholar]
- 25.Hagman DK, Latour MG, Chakrabarti SK, et al. Cyclical and alternating infusions of glucose and intralipid in rats inhibit insulin gene expression and Pdx-1 binding in islets. Diabetes 2008;57:424–431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bonner-Weir S, Deery D, Leahy JL, Weir GC. Compensatory growth of pancreatic beta-cells in adult rats after short-term glucose infusion. Diabetes 1989;38:49–53 [DOI] [PubMed] [Google Scholar]
- 27.Topp BG, McArthur MD, Finegood DT. Metabolic adaptations to chronic glucose infusion in rats. Diabetologia 2004;47:1602–1610 [DOI] [PubMed] [Google Scholar]
- 28.Alonso LC, Yokoe T, Zhang P, et al. Glucose infusion in mice: a new model to induce beta-cell replication. Diabetes 2007;56:1792–1801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Levitt HE, Cyphert TJ, Pascoe JL, et al. Glucose stimulates human beta cell replication in islets transplanted into NOD-SCID mice. Diabetologia 2011;54:572–582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yokoe T, Alonso LC, Romano LC, et al. Intermittent hypoxia reverses the diurnal glucose rhythm and causes pancreatic beta-cell replication in mice. J Physiol 2008;586:899–911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fatrai S, Elghazi L, Balcazar N, et al. Akt induces beta-cell proliferation by regulating cyclin D1, cyclin D2, and p21 levels and cyclin-dependent kinase-4 activity. Diabetes 2006;55:318–325 [DOI] [PubMed] [Google Scholar]
- 32.Georgia S, Bhushan A. Beta cell replication is the primary mechanism for maintaining postnatal beta cell mass. J Clin Invest 2004;114:963–968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kushner JA, Ciemerych MA, Sicinska E, et al. Cyclins D2 and D1 are essential for postnatal pancreatic beta-cell growth. Mol Cell Biol 2005;25:3752–3762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Peshavaria M, Larmie BL, Lausier J, et al. Regulation of pancreatic beta-cell regeneration in the normoglycemic 60% partial-pancreatectomy mouse. Diabetes 2006;55:3289–3298 [DOI] [PubMed] [Google Scholar]
- 35.Georgia S, Hinault C, Kawamori D, et al. Cyclin D2 is essential for the compensatory beta-cell hyperplastic response to insulin resistance in rodents. Diabetes 2010;59:987–996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cozar-Castellano I, Fiaschi-Taesch N, Bigatel TA, et al. Molecular control of cell cycle progression in the pancreatic beta-cell. Endocr Rev 2006;27:356–370 [DOI] [PubMed] [Google Scholar]
- 37.Rane SG, Dubus P, Mettus RV, et al. Loss of Cdk4 expression causes insulin-deficient diabetes and Cdk4 activation results in beta-islet cell hyperplasia. Nat Genet 1999;22:44–52 [DOI] [PubMed] [Google Scholar]
- 38.Cozar-Castellano I, Weinstock M, Haught M, Velázquez-Garcia S, Sipula D, Stewart AF. Evaluation of beta-cell replication in mice transgenic for hepatocyte growth factor and placental lactogen: comprehensive characterization of the G1/S regulatory proteins reveals unique involvement of p21cip. Diabetes 2006;55:70–77 [PubMed] [Google Scholar]
- 39.Elghazi L, Balcazar N, Blandino-Rosano M, et al. Decreased IRS signaling impairs beta-cell cycle progression and survival in transgenic mice overexpressing S6K in beta-cells. Diabetes 2010;59:2390–2399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Uchida T, Nakamura T, Hashimoto N, et al. Deletion of Cdkn1b ameliorates hyperglycemia by maintaining compensatory hyperinsulinemia in diabetic mice. Nat Med 2005;11:175–182 [DOI] [PubMed] [Google Scholar]
- 41.Chen H, Gu X, Su IH, et al. Polycomb protein Ezh2 regulates pancreatic beta-cell Ink4a/Arf expression and regeneration in diabetes mellitus. Genes Dev 2009;23:975–985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dhawan S, Tschen SI, Bhushan A. Bmi-1 regulates the Ink4a/Arf locus to control pancreatic beta-cell proliferation. Genes Dev 2009;23:906–911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Krishnamurthy J, Ramsey MR, Ligon KL, et al. p16INK4a induces an age-dependent decline in islet regenerative potential. Nature 2006;443:453–457 [DOI] [PubMed] [Google Scholar]
- 44.Pappan KL, Pan Z, Kwon G, et al. Pancreatic beta-cell lipoprotein lipase independently regulates islet glucose metabolism and normal insulin secretion. J Biol Chem 2005;280:9023–9029 [DOI] [PubMed] [Google Scholar]
- 45.Kim SP, Catalano KJ, Hsu IR, Chiu JD, Richey JM, Bergman RN. Nocturnal free fatty acids are uniquely elevated in the longitudinal development of diet-induced insulin resistance and hyperinsulinemia. Am J Physiol Endocrinol Metab 2007;292:E1590–E1598 [DOI] [PubMed] [Google Scholar]
- 46.Duesing K, Fatemifar G, Charpentier G, et al. Strong association of common variants in the CDKN2A/CDKN2B region with type 2 diabetes in French Europids. Diabetologia 2008;51:821–826 [DOI] [PubMed] [Google Scholar]
- 47.Gizard F, Amant C, Barbier O, et al. PPAR alpha inhibits vascular smooth muscle cell proliferation underlying intimal hyperplasia by inducing the tumor suppressor p16INK4a. J Clin Invest 2005;115:3228–3238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sone H, Kagawa Y. Pancreatic beta cell senescence contributes to the pathogenesis of type 2 diabetes in high-fat diet-induced diabetic mice. Diabetologia 2005;48:58–67 [DOI] [PubMed] [Google Scholar]
- 49.Tschen SI, Dhawan S, Gurlo T, Bhushan A. Age-dependent decline in beta-cell proliferation restricts the capacity of beta-cell regeneration in mice. Diabetes 2009;58:1312–1320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ramsey MR, Krishnamurthy J, Pei XH, et al. Expression of p16Ink4a compensates for p18Ink4c loss in cyclin-dependent kinase 4/6-dependent tumors and tissues. Cancer Res 2007;67:4732–4741 [DOI] [PubMed] [Google Scholar]