Abstract
Purpose
Both the antero-posterior and anterior approaches have been used for treating L5-S1 vertebral tuberculosis. However, no studies have compared the efficacy of the two methods in treating the disease.
Methods
The antero-posterior (AP group, 14 cases) and anterior (A group, 13 cases) approaches were performed on L5-S1 vertebral tuberculosis cases who were followed up for average of 25 months. Clinical and radiographic data were obtained from and compared between groups.
Results
Average operative time, blood loss and pre-operative, post-operative and last follow-up of lumbo-sacral angles for groups AP and A were 497 min vs 190 min, 980 ml vs 410 ml, 22.3° vs 20.6°, 29.8° vs 25.7° and 28.3° vs 23.6°, respectively. Averaged visual analogue scale (VAS) scores in groups AP and A, respectively, were 6.5 vs 6.0 points before surgery and 3.0 vs 2.8 points after surgery. Mean ODI scores were 60.2 vs 63.0 points before and 30.0 vs 28.5 points after the operation for groups AP and A, respectively. Six cases in the AP group and five in the A group who exhibited neurological symptoms recovered to American Spinal Injury Association (ASIA) grade E. The average hospitalisations of groups AP and A lasted for 21 and 15 days, respectively. Bony fusion was achieved in both groups, with an average fusion time of five and four months, respectively.
Conclusions
Both the antero-posterior and anterior approaches can effectively heal L5-S1 vertebral tuberculosis, but the average surgical time, blood loss and hospital stay following the anterior approach are prominently less than those following the antero-posterior approach.
Introduction
There is an increasing incidence of tuberculosis in developing countries. In China, there are 140,000 new cases each year. Spinal tuberculosis is the most common type of bone tuberculosis, which usually develops in the lumbar and lower thoracic spine. Lumbo-sacral tuberculosis is rare, accounting for only 2–3% of all spinal tuberculosis [1]. The therapeutic strategy for lumbo-sacral tuberculosis includes conservative and operative treatments, as with other types of spinal tuberculosis. Early diagnosis and timely conservative treatment can effectively heal lumbo-sacral tuberculosis [2]. In clinical research that reviewed 26 cases of lumbo-sacral spinal tuberculosis after an average follow-up of 20 years, both conservative and surgical treatment led to fusion in 26 cases. However, kyphosis associated trunk shortening occurred in all patients treated conservatively. They also had a higher incidence of back pain (54%) in pregnancy and a higher chance of Caesarean section (44%) [3]. Surgical treatment is required for patients who have progressive neurological functional disturbances, unstable or severely deformed spines, massive cold abscesses and who do not respond to conservative treatment [4]. Various surgical treatments have been performed on patients with lumbar tuberculosis [5–10]. However, there is a lack of clinical studies comparing the single-stage antero-posterior (AP) approach with the single-stage anterior (A) approach. Therefore, this study aimed to review and compare the therapeutic efficacy of the two approaches during an average follow-up of 25 months.
Materials and methods
Clinical data
This was a retrospective, clinical, comparative study. From February 1997 to December 2006, 27 cases of lumbo-sacral tuberculosis received surgical treatment. Surgery was performed on patients with neurological functional impairment (11 cases) and patients who did not respond well to conservative treatment (16 cases): 14 in the AP group and 13 in the A group. Every case was confirmed by computer tomography (CT)-guided biopsy. Patients receiving conservative treatment were excluded from our study. Study participants were followed up at 1, 3, 6, 12, 24 and 36 months post surgery for an average of 25 months. Three-dimensional CT and digital subtraction angiography were performed on all patients to reveal vertebrae damage and iliac vascular bifurcation. Patients who had <1/3 remaining of the affected vertebrae (L5–S1) and an iliac vascular bifurcation that was too low (below the L5–S1 intervertebral space or the S1 vertebrae), were all assigned to the AP group [4, 11, 12], as it is difficult to fix the plate in these situations. Conversely, the combination of the anterior and posterior approaches can overcome these unfavourable conditions: the pedicle screw system in the posterior approach has the advantage of maintaining stability of the affected vertebrae; in the anterior approach, the bone or mesh cage can implanted into the L5–S1 space, even if there is a low iliac vascular bifurcation and only 1/3 of the affected vertebra remains.
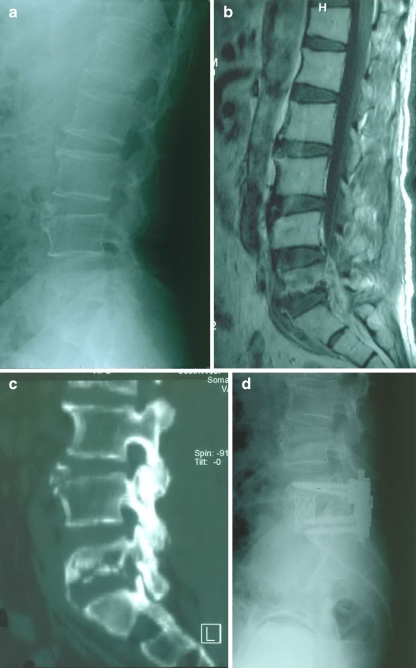
Detailed patient information for both groups and levels of involvement are showed in Table 1. In the AP group, X-ray and CT/magnetic resonance imaging (MRI) revealed vertebral body damage, intervertebral space narrowing and paravertebral abscess formation in all patients (Fig. 1a, b, c). Ten cases were complicated by an anterior sacro-iliac abscess. All patients underwent a single stage, posterior pedicle-screw fixation combining anterior debridement with an autogenous iliac bone graft (Fig. 1d).
Table 1.
Information on the patients and their level of involvement
| Sex | AP group | A group |
|---|---|---|
| Male | 10 | 8 |
| Female | 4 | 5 |
| Mean age | 36 (18-65) | 40 (20-63) |
| Number of affected vertebrae | 14 | 13 |
| L5 | 4 | 2 |
| S1 | 1 | 3 |
| L5-S1 | 9 | 8 |
| Course of disease (month) | 7.5 (5-12) | 6.8 (4-14) |
AP anteroposterior, A anterior
Fig. 1.
a Pre-operative lateral radiography of a 59-year-old man with L5 tuberculosis who had severe low back pain despite conservative treatment. b Sagittal magnetic resonance imaging showed moderate destruction of the L5 vertebral body and a prevertebral cold abscess extending caudally to S1. c Sagittal computed tomography showed destruction of the L5 vertebral body and sequestrum. d Post-operative lateral radiography, showing pedicle screw fixation with the mesh placed anteriorly. Fusion was seen at 36 months postoperatively, and a transverse connector was placed for additional stability
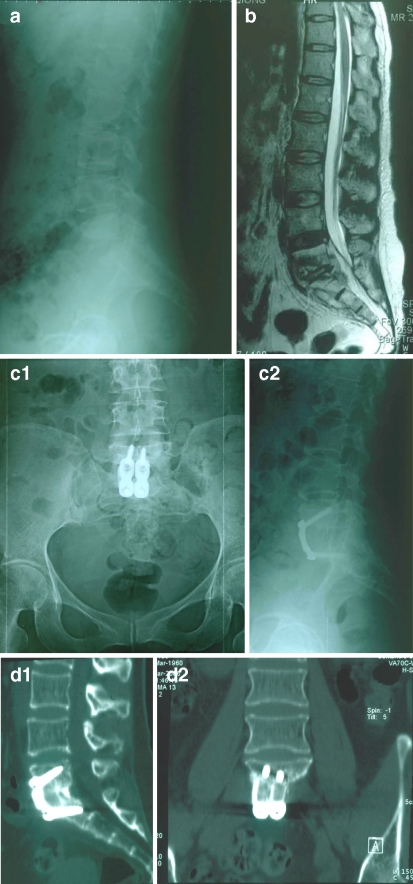
X-ray and CT/MRI were performed for all A group patients, revealing severe damage to the involved vertebral body, intervertebral space narrowing and prevertebral abscess in all cases (Fig. 2a, b); 11 cases were complicated by an anterior sacro-iliac abscess. All 13 patients received a single-stage anterior debridement and autogenous iliac bone-graft fusion combined with plate fixation (Fig. 2c).
Fig. 2.
a Pre-operative lateral radiography of a 33-year-old woman with L5–S1 tuberculosis that caused a neurologic deficit. b Sagittal magnetic resonance imaging showed destruction of the L5–S1 vertebral body and a prevertebral cold abscess extending caudally to S1. c Post-operative antero-posterior (C-1) and lateral (C-2) radiography showing the self-locking titanium anterior lumbo-sacral vertebrae plate fixation anteriorly. d Post-operative sagittal (D-1) and coronal (D-2) computed tomography showing fusion at 12 months post-operatively
Chemotherapy programme
The most common antitubercular chemotherapy programme was a combination of isoniazid, rifampicin, ethambutol and pyrazinamide, with or without streptomycin. Chemotherapy was usually administered for 4 weeks before and 1 year after surgery on an outpatient basis.
Operative approach
AP group The patient was placed in the prone position. The standard pedicle-screw (Medtronic, Inc. Minneapolis, MN USA) technique was used to fix the L5 and S1, and an autogenous bone graft was inserted on the lamina and facet joint. The patient was then placed in the supine position and paramedian incision and retroperitoneal approach were used to reach the diseased vertebrae. After radical debridement, the autogenous iliac bone or mesh with the autogenous iliac bone was tightly inserted into the L5-S1 bone groove (Fig. 1d).
A group The patient was placed in the supine position with the head higher than the feet. A paramedian incision was made through the skin midway between the symphysis pubis and the umbilicus. An open retroperitoneal approach was performed to expose the diseased vertebrae, and after radical debridement, the autogenous iliac bone was tightly inserted into the L5-S1 bone groove. Two self-locking titanium anterior lumbosacral vertebrae plates (PACH; General Corp., Germany) of suitable length were selected and anteriorly fixed at L5-S1 (Fig. 2c).
Observation index
The various indicators were observed and compared, as shown in Tables 2, 3, 4.
Table 2.
Average operative time, blood loss, pre-operative and post-operative lumbo-sacral angles, and lumbo-sacral angles at the last follow-up in the antero-posterior (AP) and anterior (A) groups
| Average operative time (min) | Average blood loss (ml) | Average pre-operative lumbo-sacral angles (°) | Average post-operative lumbo-sacral angles (°) | Lumbo-sacral angles at the last follow-up (°) | |
|---|---|---|---|---|---|
| AP | 497 (380–600) | 980 (820-1500) | 22.3 (21-24.5) | 29.8 (25-31) | 28.3 (23-29) |
| A | 190(128-210)* | 410 (350-600)* | 20.6 (18-23)** | 25.7 (24-30)** | 23.6 (20-28)** |
*p < 0.05, significant difference; **p > 0.05, no significant difference
Table 3.
Pre- and post-operative visual analogue scale (VAS) and ODI scores and average stays for antero-posterior (AP) and anterior (A) groups
| VAS | ODI | Average stay (days) | |
|---|---|---|---|
| AP pre-operative | 6.5 (5–8) | 60.2 (49–70) | |
| AP post-operative | 3.0 (2–4)** | 30.0 (25–41) ** | 21 (14–35) |
| A pre-operative | 6.0 (5–8.5) | 63.0 (45–68) | |
| A post-operative | 2.8 (2–4.5)**, *** | 28.5 (23–42) **, *** | 15 (10–27)* |
*p < 0.05, significant difference, ** p < 0.05 within AP and A groups, respectively, significant difference, ***p > 0.05 between AP and A groups, no significant difference
Table 4.
Neurological American Spinal Injury Association (ASIA) scores before surgery and at the final follow-up in the anteroposterior (AP) and anterior (A) groups
| AP | A | |||
|---|---|---|---|---|
| ASIA score | Preoperative | Final follow-up | Preoperative | Final follow-up |
| A | 0 | 0 | 0 | 0 |
| B | 3 | 0 | 2 | 0 |
| C | 2 | 0 | 2 | 0 |
| D | 1 | 0 | 1 | 0 |
| E | 8 | 14 | 8 | 13 |
| Total | 14 | 14 | 13 | 13 |
Statistical analysis
The paired t test was employed to compare groups by average operative time, blood loss, length of stay, lumbosacral angles before and after surgery and VAS and ODI scores, with p ≤ 0.05 being statistically significant.
Results
Histopathological examination results confirmed tuberculosis in all cases. All patients had significant improvement in constitutional symptoms after surgery. Average operative time, blood loss, pre- and post-operative lumbo-sacral angles, lumbo-sacral angles at the last follow-up, pre- and post-operative VAS and ODI scores, average stay and neurological American Spinal Injury Association (ASIA) scores before surgery and at final follow-up are shown in Tables 2–4.
One case of massive iliac abscess occurred in the AP group after the surgery. After needle aspiration under B-mode ultrasound guidance, catheter flushing and draining, the patient healed well. The other patients in the AP group also had a good recovery. In the A group, there was no tuberculosis recurrence and no occurrence of tubercular peritonitis, erectile dysfunction or retrograde ejaculation. Bony fusion was obtained in both the AP (Fig. 1d) and A (Fig. 2d) groups, with an average fusion time of five and four months, respectively. Average operative time, blood loss and stay for the A group was significantly less than for the AP group (Tables 2 and 3). In both groups, no cases with loosened or broken fixation or with absorbed, detached or subsided grafts were observed. Also, the nerve root and spinal cord were not injured iatrogenically.
Discussion
Early diagnosis and regular and adequate conservative anti-tubercular treatment can actually cure tuberculosis [2]. Bhojraj and Nene [13] reported on 62 cases of lumbar and lumbo-sacral tuberculosis that were treated with conservative therapy, 55 of which were cured in the 2-year follow-up. Surgical treatment was only performed on patients with severe or progressive neurological functional impairment, unstable spine or severe spinal deformity. For patients who do not respond well to conservative treatment, who have relatively massive cold abscesses in the lumbo-sacral vertebrae or who cannot tolerate long-term immobilisation, surgical treatment is still required. Lumbo-sacral tuberculosis surgery is performed with the aim of debriding the focus of infection as completely as possible, restoring nerve function and reconstructing spinal stability. For lumbo-sacral tuberculosis, especially L4-L5 and L5-S1 tuberculosis, posterior debridement and bone-graft fusion is usually adopted by researchers for fear of impairing the presacral nerve and great vessels [13, 14]. Zaveri and Mehta [14] treated 15 cases of lumbar and lumbo-sacral tuberculosis (four L5-S1) with transforaminal lumbar interbody fusion and pedicle screw fixation. Average follow-up was 41 months. All 15 cases were cured.
For lumbo-sacral tuberculosis with severe vertebral damage (<1/3 affected vertebrae remaining) or where the iliac vascular bifurcation is too low to be fixed by the plate, the AP approach has been suggested [4, 11, 15]. Its advantage lies in keeping the tubercular focus away from the fixation and fusion region, thus decreasing the incidence of tubercular expansion. This is also the reason we chose the AP option instead of debriding from behind. Even in cases of failure of union or re-occurrence in the tubercular focus region, the posterior fusion is not influenced, and the second-stage revision surgery is comparatively easier [12].
Limitations of the AP approach are also apparent. In our experience, with two positions and two incision being used in the procedure, a long operative time (497 min), large blood loss (980 ml), large wounds, prolonged hospitalisation (21 days) and comparatively higher costs, the AP approach may not be tolerated by patients >65 years who have a poor general state of health.
In the anterior approach, the tubercular focus can be debrided thoroughly under direct vision. The bony fusion is also relatively fast. Mukherjee and Dau [16] reported that among the 38 cases with lumbar tuberculosis (two with lumbo-sacral tuberculosis) who had undergone single-stage anterior debridement and bone-graft fusion, 36 obtained bony union and had complete pain relief at the 4-year follow-up, and five cases with neurological symptoms recovered. A long-term follow-up (average 20 years) of 26 cases of lumbo-sacral tuberculosis found that anterior debridement and bone graft fusion can significantly reduce the incidence and degree of lumbo-sacral kyphosis compared with conservative treatment [3]. Through the anterior approach, debridement, fusion and fixation can be completed at the same time, and only one position and one incision are needed during surgery. As a result, operative time is greatly shortened (190 min), blood loss is reduced (410 ml), and the length of stay is relatively short (15 days).
The pre-condition for L5-S1 tuberculosis anterior debridement and plate fixation is understanding the contribution of the anterior L5-S1 vertebral iliac blood vessels. Through dissection of 37 human cadavers, Tribus and Belanger [17] found that the average distance from the iliac vascular bifurcation to the top of the L5-S1 disc was 18 (range 7–36) mm and the average distance between the left common iliac vein and the right common iliac artery was 33.5 (range 12–50) mm. Most (87.8%) specimens had a space for fixing a plate at L5-S1. Capellades et al. [18] reported that 81.95% of patients had room for a surgical procedure at L5-S1. In 18.05% of the population, however, venous structures overlapped the centre of the L5-S1 disc (the iliac vascular bifurcation was too low), which reduces the operative window. In this case, it is dangerous to perform plate implantation (as in the A group); instead, a small mesh or autogenous bone graft is inserted into the L5-S1 intervertebral space without much difficulty (as in the AP group) because it requires slight traction of the vessels, which provides enough room to insert the bone graft or mesh. The limited ability of the tuberculosis bacillus to adhere to titanium alloy plates is part of the biological basis for anterior plate fixation [19]. Although the lumbo-sacral anterior plate can prevent the graft from dislocating and subsiding into the L5-S1 intervertebral space because of its excellent supportive ability [19, 20], the anterior approach and plate fixation is technically demanding and should only be performed by surgeons whose extensive experience can guarantee a high success rate [3].
Many researchers report that patients with spinal tuberculosis who suffer from functional neurological disturbance obtain satisfactory functional restoration and recovery from tuberculosis through debridement, decompression and stabilisation of the spinal cord [21–24]. Results of our study agree with these statements. Patients with functional nerve impairment—six in the AP group and five in the A group–recovered to grade E in the ASIA scoring system. All patients in both groups obtained bony fusion.
There is no clinical research to date comparing the AP and A approaches for lumbo-sacral tuberculosis; therefore, our study may be of benefit to the field. Our research indicates that individualised treatment should be employed in treating lumbo-sacral tuberculosis. For carefully selected cases of lumbo-sacral tuberculosis, both approaches can successfully cure the disease. There were no significant differences in the time required to obtain bony union, in back-pain relief or in improved lumbar function. Except for patients with <1/3 of the affected vertebrae (L5–S1) remaining and whose iliac vascular bifurcation is too low, anterior debridement, bone-graft fusion and plate fixation have the advantages of a shorter operative time, less blood loss and a shorter length of stay. There were limitations to our research: this was a retrospective rather than a prospective study, and the A group had no cases with an iliac-vessel bifurcation that was too low and with <1/3 of the affected vertebrae (L5–S1) remaining, which might have led to biased clinical outcomes and conclusions.
Acknowledgement
This work was supported by grants from the National Natural Science Foundation of China (No.30300357, 39830100) and National High Technology Development Foundation of China (863) (No.2003AA205021, 2006AA02Z4E3, 2006AA02A122).
Contributor Information
Qingyi He, Email: hqy1225@yahoo.com.cn.
Jianzhong Xu, Email: xjzslw@163.com.
References
- 1.Wellons JC, Zomorodi AR, Villaviciencio AT, Woods CW, Lawson WT, Eastwood JD. Sacral tuberculosis: a case report and review of the literature. Surg Neurol. 2004;61:136–139. doi: 10.1016/S0090-3019(03)00265-9. [DOI] [PubMed] [Google Scholar]
- 2.Moon MS, Moon YW, Moon JL, Kim SS, Sun DH. Conservative treatment of tuberculosis of the lumbar and lumbosacral spine. Clin Orthop Relat Res. 2002;398:40–49. doi: 10.1097/00003086-200205000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Pun WK, Chow SP, Luk KD, Cheng CL, Hsu LC, Leong JC. Tuberculosis of the lumbosacral junction. Long-term follow-up of 26 cases. J Bone Jt Surg Br. 1990;72:675–678. doi: 10.1302/0301-620X.72B4.2143192. [DOI] [PubMed] [Google Scholar]
- 4.Sundararaj GD, Behera S, Ravi V, Venkatesh K, Cherian VM, Lee V. Role of posterior stabilisation in the management of tuberculosis of the dorsal and lumbar spine. J Bone Jt Surg Br. 2003;85:100–106. doi: 10.1302/0301-620X.85B1.13300. [DOI] [PubMed] [Google Scholar]
- 5.Jeanneret B, Magerl F. Treatment of osteomyelitis of the spine using percutaneous suction/irrigation and percutaneous external spinal fixation. J Spinal Disord. 1994;7:185–205. doi: 10.1097/00002517-199407030-00001. [DOI] [PubMed] [Google Scholar]
- 6.Ozturk C, Aydinli U, Vural R, Sehirlioglu A, Mutlu M. Simultaneous versus sequential one-stage combined anterior and posterior spinal surgery for spinal infections (outcomes and complications) Int Orthop. 2007;31(3):363–366. doi: 10.1007/s00264-006-0166-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oguz E, Sehirlioglu A, Altinmakas M, Ozturk C, Komurcu M, Solakoglu C, Vaccaro AR. A new classification and guide for surgical treatment of spinal tuberculosis. Int Orthop. 2008;32(1):127–133. doi: 10.1007/s00264-006-0278-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Samuel S. Comment on Oguz et al.: a new classification and guide for surgical treatment of spinal tuberculosis. Int Orthop. 2010;34(4):613. doi: 10.1007/s00264-009-0939-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang QS, Zheng C, Hu Y, Yin X, Xu H, Zhang G, Wang Q. One-stage surgical management for children with spinal tuberculosis by anterior decompression and posterior instrumentation. Int Orthop. 2009;33(5):1385–1390. doi: 10.1007/s00264-009-0758-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jain S. Comment on Huang et al.: one-stage surgical management for children with spinal tuberculosis by anterior decompression and posterior instrumentation. Int Orthop. 2010;34(5):769–770. doi: 10.1007/s00264-010-0975-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim DJ, Yun YH, Moon SH, Riew KD. Posterior instrumentation using compressive laminar hooks and anterior interbody arthrodesis for the treatment of tuberculosis of the lower lumbar spine. Spine (Phila Pa 1976) 2004;29:E275–E279. doi: 10.1097/01.BRS.0000129027.68574.06. [DOI] [PubMed] [Google Scholar]
- 12.Klöckner C, Valencia R. Sagittal alignment after anterior debridement and fusion with or without additional posterior instrumentation in the treatment of pyogenic and tuberculous spondylodiscitis. Spine (Phila Pa 1976) 2003;28:1036–1042. doi: 10.1097/01.BRS.0000061991.11489.7F. [DOI] [PubMed] [Google Scholar]
- 13.Bhojraj S, Nene A. Lumbar and lumbosacral tuberculous spondylodiscitis in adults. Redefining the indications for surgery. J Bone Joint Surg Br. 2002;84:530–534. doi: 10.1302/0301-620X.84B4.12363. [DOI] [PubMed] [Google Scholar]
- 14.Zaveri GR, Mehta SS. Surgical treatment of lumbar tuberculous spondylodiscitis by transforaminal lumbar interbody fusion (TLIF) and posterior instrumentation. J Spinal Disord Tech. 2009;22:257–262. doi: 10.1097/BSD.0b013e31818859d0. [DOI] [PubMed] [Google Scholar]
- 15.Bezer M, Kucukdurmaz F, Aydin N, Kocaoglu B, Guven O. Tuberculous spondylitis of the lumbosacral region: long-term follow-up of patients treated by chemotherapy, transpedicular drainage, posterior instrumentation, and fusion. J Spinal Disord Tech. 2005;18:425–429. doi: 10.1097/01.bsd.0000171627.11171.6f. [DOI] [PubMed] [Google Scholar]
- 16.Mukherjee SK, Dau AS. Anterior lumbar fusion in Pott's disease. Clin Orthop Relat Res. 2007;460:93–99. doi: 10.1097/BLO.0b013e318067bcd9. [DOI] [PubMed] [Google Scholar]
- 17.Tribus CB, Belanger T. The vascular anatomy anterior to the L5-S1 disk space. Spine. 2001;26:1205–1208. doi: 10.1097/00007632-200106010-00007. [DOI] [PubMed] [Google Scholar]
- 18.Capellades J, Pellisé F, Rovira A, Grivé E, Pedraza S, Villanueva C. Magnetic resonance anatomic study of iliocava junction and left iliac vein positions related to L5-S1 disc. Spine (Phila Pa 1976) 2000;25:1695–1700. doi: 10.1097/00007632-200007010-00013. [DOI] [PubMed] [Google Scholar]
- 19.Ha KY, Chung YG, Ryoo Adherence and biofilm formation of staphylococcus epidermidis and mycobacterium tuberculosis on various spinal implants. Spine. 2005;30:38–43. doi: 10.1097/01.brs.0000154674.16708.af. [DOI] [PubMed] [Google Scholar]
- 20.Rajasekaran S, Soundarapandian S. Progression of kyphosis in tuberculosis of the spine treated by anterior arthrodesis. J Bone Joint Surg Am. 1989;71:1314–1323. [PubMed] [Google Scholar]
- 21.Wenjun WANG, Bichun QUAN, Lile LIU. The application of U shape titanium plate in surgical treatment of lumbar and sacrum spinal tuberculosis. Chin J Spine Spinal Cord. 2005;15:729–731. [Google Scholar]
- 22.Lee SH, Sung JK, Park YM. Single-stage transpedicular decompression and posterior instrumentation in treatment of thoracic and thoracolumbar spinal tuberculosis: a retrospective case series. J Spinal Disord Tech. 2006;19:595–602. doi: 10.1097/01.bsd.0000211241.06588.7b. [DOI] [PubMed] [Google Scholar]
- 23.Güzey FK, Emel E, Bas NS, Hacisalihoglu S, Hacisalihoglu S, Seyithanoglu MH, Karacor SE, Ozkan N, Alatas I, Sel B. Thoracic and lumbar tuberculous spondylitis treated by posterior debridement, graft placement, and instrumentation: a retrospective analysis in 19 cases. J Neurosurg Spine. 2005;3:450–458. doi: 10.3171/spi.2005.3.6.0450. [DOI] [PubMed] [Google Scholar]
- 24.Korovessis P, Petsinis G, Koureas G, Iliopoulos P, Zacharatos S. Anterior surgery with insertion of titanium mesh cage and posterior instrumented fusion performed sequentially on the same day under one anesthesia for septic spondylitis of thoracolumbar spine: is the use of titanium mesh cages safe? Spine. 2006;31:1014–1019. doi: 10.1097/01.brs.0000215049.08622.9d. [DOI] [PubMed] [Google Scholar]