Abstract
Purpose
The purpose of this study was to evaluate clinical outcomes following one-stage anterior radical debridement, interbody fusion, and sacral rod fixation for the treatment of lumbosacral segment tuberculosis.
Methods
From March 2004 to November 2008, 11 patients diagnosed with spinal tuberculosis received antituberculosis medications for two to three weeks before anterior radical debridement, autologous iliac bone grafting, and internal sacral rod fixation. Surgery was performed when the toxic symptoms of tuberculosis were controlled and erythrocyte sedimentation rates (ESR) decreased to 37.2 ± 9.6 mm/h (25–54 mm/h). Lumbosacral angle, visual analogue scale (VAS) pain, ESR, and neurological performance were assessed before and after surgery.
Results
All surgical procedures were performed successfully without intra or postoperative complication. There were no instances of spinal tuberculosis recurrence. Patients were followed-up for a mean of 19.6 months. The mean lumbosacral angle was significantly increased from the mean preoperative angle (12.9 ± 5.0°) both postoperatively (21.5 ± 6.1°) and at final follow-up (20.1 ± 5.2°) (both P <0.001). The mean VAS scores and ESR were significantly decreased from preoperative levels (7.3 ± 1.2 and 37.2 ± 9.6 mm/h, respectively) both postoperatively (1.5 ± 0.5 at month six and 10.4 ± 4.5 mm/h at month three, respectively) and at final follow-up (0.6 ± 0.5 and 10.5 ± 2.3 mm/h, respectively) (all P <0.001). Bone fusion occurred in all patients at a mean of nine months (range six to 12 months) after surgery. Three patients who had impaired neurological performance before surgery had normal neurological performance after surgery.
Conclusion
Our findings suggest that anterior radical debridement, interbody fusion, and sacral rod fixation can be an effective treatment option for lumbosacral segment tuberculosis.
Introduction
Spinal tuberculosis is the most common form of extrapulmonary tuberculosis, accounting for approximately 50% of all cases of musculoskeletal tuberculosis and 2% of all cases of tuberculosis [1, 2]. Spinal tuberculosis, the incidence of which appears to be increasing [3], may result in a number of potentially serious complications including neurological deficits (e.g., paraplegia) and spinal deformities (e.g., kyphosis) [4]. Hence, timely and effective treatment of spinal tuberculosis is essential.
Antituberculous chemotherapy is essential for the treatment of spinal tuberculosis; however, the complications of spinal tuberculosis, in particular kyphosis, may warrant additional surgical intervention [4]. Various surgical approaches have been described for treating the complications of spinal tuberculosis including debridement with anterior spinal fusion, anterior spinal fusion with posterior spinal fusion, posterior spinal fusion alone, and posterior spinal fusion followed by anterior spinal fusion [4]. The variety of surgical approaches used in part reflects the fact that the symptoms and characteristics of spinal tuberculosis may vary considerably from one individual to the next, particular with regards to the level of deformity, neurological status, and bone quality [5].
The majority (98%) of cases of spinal tuberculosis involve inflammation of the anterior spinal column [6]; however, reports on the management of tuberculosis in the lumbosacral region of the spine are relatively scarce [5, 7, 8]. Further, there is a lack of consensus as to what is the most effective means of managing lumbosacral segment tuberculosis, with conservative treatment, transpedicular drainage, posterior instrumentation and fusion, anterior debridement and fusion, and anterior and posterior fusion having been described to be effective [5, 7, 8]. No report to date has described the use of one-stage anterolateral radical debridement, interbody fusion, and sacral rod fixation for the treatment of lumbosacral segment tuberculosis. Hence, the aim of our clinical study (the results of which are presented in this report) was to evaluate the results / outcomes associated with this approach for the treatment of lumbosacral segment tuberculosis in a series of 11 patients.
Materials and methods
Patients
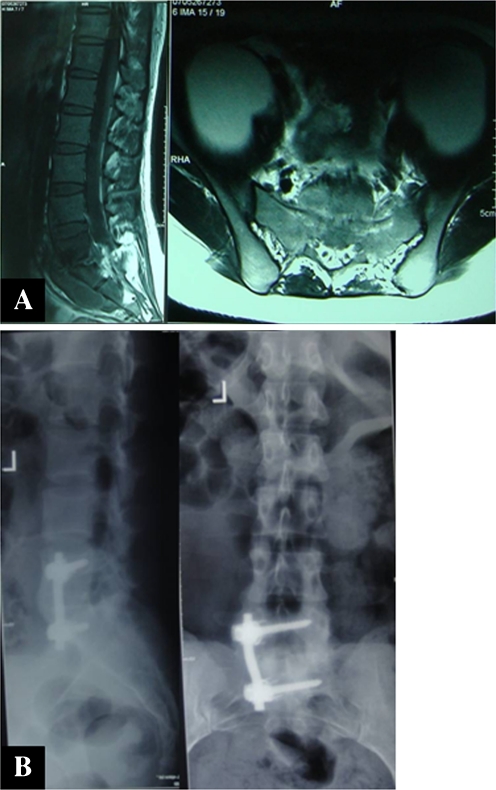
From March 2004 to November 2008, 11 patients diagnosed with spinal tuberculosis in the lumbosacral region underwent surgery at our clinic. All patients were evaluated by plain radiography, computed tomography (CT), and magnetic resonance imaging (MRI), and they were included in the study because the condition of abscess formation and severe vertebral destruction revealed in MRI or CT imaging (with or without neurological deficits) was met (Fig. 1a).
Fig. 1.
Radiographs from a 37-year-old patient who had L5-S1 tuberculosis. a Preoperative magnetic resonance image showing destruction of the anterior and middle columns of the body with an anterior epidural abscess and bilateral psoas abscesses. b The patient received one-stage anterior debridement, iliac crest interbody autografting, and sacral rod fixation. The anteroposterior and lateral radiographs demonstrate bony union nine months after surgery
All patients presented with various degrees of lower back pain; one patient experienced preoperative lower extremity radicular pain, while two patients experienced saddle area anaesthesia. However, only six patients exhibited mild to moderate tuberculous toxic reactions, such as fever, loss of weight, fatigue, and anorexia. Plain radiographs revealed the following abnormal features: osteopenia, reduced disc space, and endplate erosions (all patients); paravertebral abscess and gross bony destruction with deformity (four of 11 patients). Magnetic resonance imaging and CT revealed that all patients had evidence of vertebral and paravertebral body collapse, and prevertebral or epidural abscesses. Involvement of the adjacent vertebral bodies and the intervening disc was apparent in all patients. The levels of the lesions were: L4-S1 (four patients), L5-S1 (two patients), and L4-L5 (five patients).
The diagnosis of tuberculosis was made with reference to clinical and radiological findings and was verified histopathologically after debridement in all patients. Note: all patients underwent routine chest X-rays and sputum examinations for tubercle bacillus, and none of them had open tuberculosis or acute miliary pulmonary tuberculosis.
Preoperative chemotherapy
All patients received standard oral antituberculous chemotherapy after diagnosis comprising isoniazid (300 mg/day), rifampin (450 mg/day), ethambutol (1,200 mg/day), and pyrazinamide (1.5 g/day) for two to three weeks before surgery. Surgery was carried out when the toxic symptoms of tuberculosis were controlled, e.g. the patients regained normal appetite without low fever and anemia, and ESR decreased to 37.2 ± 9.6 mm/h (25–54 mm/h).
Surgical procedure
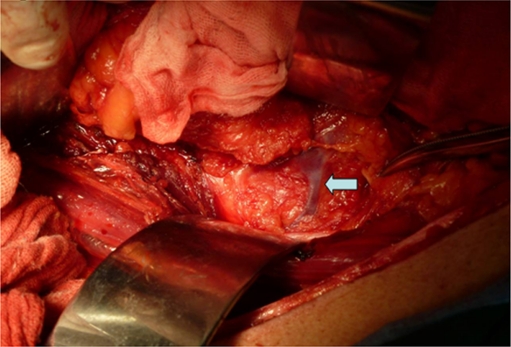
Surgery was performed under general endotracheal anaesthesia. All patients were operated up on in the lateral position taking a standard anterolateral approach to the spine via a retroperitoneal flank incision. Typically, the approach was made from the severely damaged side of the spine. For exposure of the tuberculous foci in L4-S1, mobilisation of the overlying aorta and inferior vena cava was necessary. In such cases, segmental vessels emanating from the aorta and vena cava must be divided to facilitate medial retraction of these vessels thus reducing the risk of thrombosis or tearing of the iliac veins through excessive retraction. Special attention should be given to the iliolumbar or ascending vein, a large venous branch overlying the L5 body and draining into the lateral common iliac vein (Fig. 2); we generally dissected and completely ligated this vessel early in the procedure. The L5 root often runs in close proximity to this branch and hence, should be identified and avoided. After exposure, the abscess was drained and any necrotic material within the body and the disc above and below the affected vertebral bodies was identified and resected with conventional rongeurs and curettes down to bleeding normal bone. If the paravertebral abscess was large, drainage from a stab incision was necessary to identify the margin of the lesion foci. Slots were made in healthy bleeding bone of the vertebral bodies above and/or below the affected vertebral bodies. After radical resection of the involved spine, distraction was performed between adjacent normal vertebrae to correct the kyphosis. The spinal defect was measured at this time. The resultant gap was repaired with suitable length bone grafts harvested from the iliac crest or rib during the procedure. Anterior instrumentation was performed after interbody autografting. The instrumentation consisted of rods and screws (Johnson & Johnson, Medical Equipment Co., Ltd, China) placed in the vertebral body. One screw was inserted through the lateral vertebral body of L4 or L5. The other screw was inserted transversely through the lateral sacral promontory to the opposite side of the sacrum. The rod/screw constructions spanned the S1 and L5 vertebral bodies or one level above the affected vertebrae. After careful haemostasis, a quantity of normal saline was used for space irrigation to eliminate residual tuberculous tissue. Thereafter, three to four grams of streptomycin were placed in the operated area and a local drainage tube were inserted before the incision was closed.
Fig. 2.
Intraoperative photograph showing the iliolumbar vein overlaying the L5 body (arrow). This vessel should be dissected and ligated early in the procedure
Postoperative treatment
The drainage tube was typically removed after 72 hours. Patients were allowed to walk two weeks after surgery while wearing an orthosis (the orthosis was worn for a minimum of six months postoperatively). All patients were treated with a postoperative antituberculous chemotherapy regimen for 12–18 months comprising rifampicin (450 mg per day), isoniazid (300 mg per day), ethambutol (1,200 mg per day), and pyrazinamide (1.5 g per day) for three months, followed by rifampicin, isoniazid, and ethambutol for nine weeks, and finally rifampicin and isoniazid for the remainder of the regimen as mentioned above using the same dose. Liver function and erythrocyte sedimentation rates (ESR) were monitored during follow-up at regular intervals.
Follow-up assessments
Patients were followed-up at monthly intervals to three months after surgery and then every three months to 12 months after surgery. Subsequent follow-up visits were at six-month intervals until the time of the most recent follow-up visit.
The ESR, lumbosacral angle, and pain were assessed before and after surgery. The lumbosacral angle was measured by drawing lines along the posterior border of S1 and the posterior border of the first normal vertebra above the level of the lesion [9]. Pain was evaluated using a visual analogue scale (VAS).
Computer tomography scans were performed at six months or 12 months to confirm bone fusion and/or any recurrence of the disease. Bone fusion was indicated by evidence of fusion on radiographs and computerised tomography scans as well as the absence of localized pain and tenderness over the site of the arthrodesis.
Neurological performance was assessed before and after surgery using the Frankel Grading System.
Statistical methods
Preoperative, postoperative, and final follow-up lumbosacral angles, VAS scores, and ESR were compared by repeated measures analysis of variances and Fisher’s least significant difference method. All tests were two-sided and P ≤ 0.05 was considered to indicate statistical significance. All analyses were performed using SPSS Statistical Software for Windows 14.0 (SPSS Inc., Chicago, IL).
Results
Table 1 summarises the patients’ demographic, operative, and disease characteristics. The five men and six women had a mean age of 44.5 ± 8.5 years and a mean duration of symptoms (before surgery) of 5.36 ± 1.69 months. The mean duration of surgery was 123.34 ± 22.48 minutes, while the mean volume of blood lost during surgery was 1163.6 ± 265.6 mL. The mean length of postoperative follow-up was 19.64 ± 5.43 months.
Table 1.
Patient demographics, operative information and disease characteristics
| Patient | Age (years) | Gender | Operation time (min) | Blood loss (mL) | Level | Duration of symptoms (months) | Length of follow-up (months) |
|---|---|---|---|---|---|---|---|
| 1 | 43 | M | 120 | 1500 | L4 to S1 | 4 | 18 |
| 2 | 29 | F | 140 | 1600 | L4 to L5 | 5 | 24 |
| 3 | 38 | F | 150 | 1300 | L4 to S1 | 4 | 30 |
| 4 | 55 | M | 140 | 1100 | L5 to S1 | 7 | 18 |
| 5 | 45 | F | 160 | 1500 | L4 to L5 | 8 | 12 |
| 6 | 37 | M | 130 | 900 | L4 to S1 | 3 | 12 |
| 7 | 49 | F | 100 | 1000 | L4 to S1 | 5 | 24 |
| 8 | 51 | M | 110 | 1000 | L4 to L5 | 6 | 18 |
| 9 | 56 | F | 120 | 1100 | L5 to S1 | 8 | 24 |
| 10 | 49 | F | 90 | 900 | L4 to L5 | 5 | 18 |
| 11 | 37 | M | 100 | 900 | L4 to L5 | 4 | 18 |
| Mean ± SD | 44.45 ± 8.50 | - | 123.34 ± 22.48 | 1163.64 ± 265.60 | - | 5.36 ± 1.69 | 19.64 ± 5.43 |
SD standard deviation, M male, F female
Table 2 summarises the radiological and clinical outcomes. Repeated measures analysis of variances revealed that there was significant difference among pre-operation, post-operation and final follow-up in lumbosacral angle (P <0.001); in the meantime, they had statistical differences at three time points both in VAS score (P <0.001) and ESR (P <0.001). Specifically, the mean lumbosacral angle was significantly increased from the mean preoperative angle to postoperatively (P <0.001). The mean postoperative lumbosacral angle, VAS scores and ESR were all significantly decreased from preoperative levels three or six months postoperatively (all P <0.001) and remained stable until final follow-up.
Table 2.
Summary of radiological and clinical outcomes
| Patient | Lumbosacral angle (°) | VAS score | ESR (mm/h) | Bone fusion (months) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Preop | Postopa | Final | Preop | Postopb | Final | Preop | Postopa | Final | ||
| 1 | 10 | 15 | 14 | 7 | 1 | 0 | 47 | 10 | 12 | 9 |
| 2 | 7 | 16 | 14 | 7 | 2 | 1 | 30 | 11 | 14 | 6 |
| 3 | 5 | 17 | 15 | 5 | 1 | 1 | 34 | 5 | 8 | 9 |
| 4 | 15 | 22 | 20 | 8 | 2 | 0 | 39 | 20 | 7 | 12 |
| 5 | 20 | 29 | 28 | 9 | 1 | 1 | 46 | 13 | 9 | 9 |
| 6 | 13 | 24 | 21 | 7 | 2 | 1 | 54 | 12 | 11 | 9 |
| 7 | 9 | 17 | 17 | 6 | 1 | 1 | 29 | 11 | 13 | 12 |
| 8 | 16 | 28 | 23 | 7 | 1 | 1 | 31 | 5 | 8 | 9 |
| 9 | 20 | 30 | 28 | 8 | 2 | 0 | 25 | 6 | 10 | 9 |
| 10 | 16 | 25 | 24 | 9 | 2 | 1 | 29 | 14 | 11 | 9 |
| 11 | 11 | 13 | 17 | 7 | 1 | 0 | 46 | 7 | 13 | 6 |
| Mean ± SD | 12.9 ± 5.0 | 21.5 ± 6.1* | 20.1 ± 5.2* | 7.3 ± 1.2 | 1.5 ± 0.5* | 0.6 ± 0.5* | 37.2 ± 9.6 | 10.4 ± 4.5* | 10.5 ± 2.3* | 9.0 ± 1.9 |
ESR erythrocyte sedimentation rate, preop preoperative, postop postoperative, SD standard deviation, VAS visual analogue scale
aPostoperative follow-up at three months
bPostoperative follow-up at six months
*Indicates a statistically significant difference between the mean postop or final value and the mean preop value (all P < 0.01)
All wounds healed without chronic infection or sinus formation. There were no complications related to instrumentation. Bone fusion was evident at a mean of nine months (range, six to 12 months) after surgery (Fig. 1b). There was no recurrence of disease in any of the patients at final follow-up and no patients died. Two of 11 patients, who had fluctuating ESRs, received postoperative antituberculosis chemotherapy for the full 18 months.
Three patients had evidence of neurological impairment before surgery as indicated by Frankel grade D (all other patients had normal neurological status, i.e., Frankel grade E). After surgery, there was no evidence of neurological impairment in any patients.
Discussion
We have described 11 rare cases of lumbosacral segment tuberculosis treated by one-stage anterolateral radical debridement, interbody fusion, and sacral rod fixation. Importantly, there were no intra or postoperative complications associated with the treatment approach and all patients exhibited marked postoperative improvement in pain and spinal deformity correction. Our findings suggest that one-stage anterolateral radical debridement, interbody fusion, and sacral rod fixation can be an effective option for treating lumbosacral segment tuberculosis
Although chemotherapy can be effective for the treatment of spinal tuberculosis, residual back pain is relatively common because of kyphosis or hypolordosis of the lumbosacral junction [7]. Indeed, external support may be required during chemotherapy if the associated back pain is severe and/or the duration of treatment is lengthy. Lordosis of the lumbar spine is associated with several biomechanical advantages and is essential for normal functioning [10]. Hence, it is important to preserve normal curvature during treatment of spinal tuberculosis and minimise the chance of kyphosis. As opposed to chemotherapy alone, surgical treatment of spinal tuberculosis can result in rapid mobilisation, spinal stabilisation, and early fusion [11–13]. We suggest that surgery (combined with chemotherapy) should be the preferred treatment approach for lumbosacral segments tuberculosis with abscess formation and severe vertebral destruction (with or without neurologic deficits).
Various surgical approaches have been described for treatment of spinal tuberculosis. One such approach, transpedicular drainage with posterior instrumentation [5, 14], may be effective for treating patients who are diagnosed early in the disease process, but not effective for treating patients with major vertebral collapse and/or neurological deficits. Posterior debridement and instrumentation is another approach that has been used in the treatment of spinal tuberculosis [15]; however, posterior instrumentation without anterior support may not provide optimal spinal stability nor prevent the progression of kyphosis [16]. A further approach is anterior radical debridement accompanied by posterior instrumentation [17]. Although this approach has been reported to be an effective means of treatment [17], the two-stage procedure is associated with increased operating time, prolonged anaesthesia, increased blood loss, and an increased risk of complications compared to one-stage procedures such as that described in our report. We suggest that surgery for spinal tuberculosis should generally be via an anterior approach because the disease invariably destroys the anterior bone and soft tissue structures of the spine. An anterior approach allows for good / direct visualisation of the lesion and facilitates direct and complete decompression of the spinal cord. Laminectomy of anterior vertebral lesions should be avoided because this requires removal of the only healthy segment of the vertebral column and renders the spine unstable.
In the surgical treatment of spinal tuberculosis, anterior debridement of the disease focus may create segmental instability. Hence, grafting plays a crucial role in preventing progression of the kyphosis in the unstable segment by providing structural anterior support. However, the graft may be subjected to extreme mechanical stresses, which may cause the graft to fail. The forces transmitted across the graft and the weakening of the graft during the creeping substitution period may cause fracture, slippage, and/or resorption of the graft, or subsidence of the graft into adjacent cancellous vertebral bodies [18, 19]. Therefore, anterior instrumentation is suggested for correcting the kyphotic deformity, stabilising the vertebral column, and preventing graft related complications [11, 20].
Our study has a number of limitations that should be mentioned. First, our study included a small number of patients and comprised a relatively short length of follow-up. Certainly, studies with a larger number of patients and a longer length of follow-up are warranted. However, we do note that lumbosacral segment tuberculosis is not a common form of spinal tuberculosis; hence, finding a larger number of subjects for a single study would be challenging unless multiple institutions were involved. A further limitation is the fact that the technique described is quite clearly not applicable for cases in which the affected S1 vertebral body is severely damaged. Indeed, this technique is only applicable in cases in which the sacral screw can be stably fixed to the S1 vertebral body, i.e., when the S1 vertebral body is not invaded or destroyed by less than one third.
In conclusion, we have summarised our experience treating lumbosacral segment tuberculosis with one-stage anterior decompression, bone grafting, and anterior instrumentation. Two important benefits of this surgical approach include adequate removal of the infected material and early postoperative ambulation (because of the firm internal fixation and correction of the spinal deformity). Furthermore, we found that one-stage anterior decompression, bone grafting, and anterior instrumentation was associated with dramatically reduced postoperative pain, deformity correction, and neurological recovery in patients with lumbosacral segment tuberculosis. One-stage anterolateral radical debridement, interbody fusion, and sacral rod fixation can be an effective option for treating lumbosacral segment tuberculosis
Acknowledgment
None.
Conflict of interest The authors declare no conflict of interest.
References
- 1.Pertuiset E, Beaudreuil J, Liote F, Horusitzky A, Kemiche F, Richette P, Clerc-Wyel D, Cerf-Payrastre I, Dorfmann H, Glowinski J, Crouzet J, Bardin T, Meyer O, Dryll A, Ziza JM, Kahn MF, Kuntz D. Spinal tuberculosis in adults. A study of 103 cases in a developed country, 1980–1994. Medicine (Baltimore) 1999;78:309–320. doi: 10.1097/00005792-199909000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Yao DC, Sartoris DJ. Musculoskeletal tuberculosis. Radiol Clin North Am. 1995;33:679–689. [PubMed] [Google Scholar]
- 3.Jain AK, Dhammi IK. Tuberculosis of the spine: a review. Clin Orthop Relat Res. 2007;460:39–49. doi: 10.1097/BLO.0b013e318073bd29. [DOI] [PubMed] [Google Scholar]
- 4.Jain AK. Tuberculosis of the spine: a fresh look at an old disease. J Bone Joint Surg Br. 2010;92:905–913. doi: 10.1302/0301-620X.92B7.24668. [DOI] [PubMed] [Google Scholar]
- 5.Bezer M, Kucukdurmaz F, Aydin N, Kocaoglu B, Guven O. Tuberculous spondylitis of the lumbosacral region: long-term follow-up of patients treated by chemotherapy, transpedicular drainage, posterior instrumentation, and fusion. J Spinal Disord Tech. 2005;18:425–429. doi: 10.1097/01.bsd.0000171627.11171.6f. [DOI] [PubMed] [Google Scholar]
- 6.Jain AK, Aggarwal A, Mehrotra G. Correlation of canal encroachment with neurological deficit in tuberculosis of the spine. Int Orthop. 1999;23:85–86. doi: 10.1007/s002640050313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pun WK, Chow SP, Luk KD, Cheng CL, Hsu LC, Leong JC. Tuberculosis of the lumbosacral junction. Long-term follow-up of 26 cases. J Bone Joint Surg Br. 1990;72:675–678. doi: 10.1302/0301-620X.72B4.2143192. [DOI] [PubMed] [Google Scholar]
- 8.Bhojraj S, Nene A. Lumbar and lumbosacral tuberculous spondylodiscitis in adults. Redefining the indications for surgery. J Bone Joint Surg Br. 2002;84:530–534. doi: 10.1302/0301-620X.84B4.12363. [DOI] [PubMed] [Google Scholar]
- 9.Rajasekaran S. The natural history of post-tubercular kyphosis in children. Radiological signs which predict late increase in deformity. J Bone Joint Surg Br. 2001;83:954–962. doi: 10.1302/0301-620X.83B7.12170. [DOI] [PubMed] [Google Scholar]
- 10.Farfan HF. The biomechanical advantage of lordosis and hip extension for upright activity. Man as compared with other anthropoids. Spine (Phila Pa 1976) 1978;3:336–342. doi: 10.1097/00007632-197812000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Yilmaz C, Selek HY, Gurkan I, Erdemli B, Korkusuz Z. Anterior instrumentation for the treatment of spinal tuberculosis. J Bone Joint Surg Am. 1999;81:1261–1267. doi: 10.2106/00004623-199909000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Christodoulou AG, Givissis P, Karataglis D, Symeonidis PD, Pournaras J. Treatment of tuberculous spondylitis with anterior stabilization and titanium cage. Clin Orthop Relat Res. 2006;444:60–65. doi: 10.1097/01.blo.0000201175.87635.28. [DOI] [PubMed] [Google Scholar]
- 13.Jin D, Qu D, Chen J, Zhang H. One-stage anterior interbody autografting and instrumentation in primary surgical management of thoracolumbar spinal tuberculosis. Eur Spine J. 2004;13:114–121. doi: 10.1007/s00586-003-0661-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee SH, Sung JK, Park YM. Single-stage transpedicular decompression and posterior instrumentation in treatment of thoracic and thoracolumbar spinal tuberculosis: a retrospective case series. J Spinal Disord Tech. 2006;19:595–602. doi: 10.1097/01.bsd.0000211241.06588.7b. [DOI] [PubMed] [Google Scholar]
- 15.Guzey FK, Emel E, Bas NS, Hacisalihoglu S, Seyithanoglu MH, Karacor SE, Ozkan N, Alatas I, Sel B. Thoracic and lumbar tuberculous spondylitis treated by posterior debridement, graft placement, and instrumentation: a retrospective analysis in 19 cases. J Neurosurg Spine. 2005;3:450–458. doi: 10.3171/spi.2005.3.6.0450. [DOI] [PubMed] [Google Scholar]
- 16.Chen WJ, Wu CC, Jung CH, Chen LH, Niu CC, Lai PL. Combined anterior and posterior surgeries in the treatment of spinal tuberculous spondylitis. Clin Orthop Relat Res . 2002;398:50–59. doi: 10.1097/00003086-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Talu U, Gogus A, Ozturk C, Hamzaoglu A, Domanic U. The role of posterior instrumentation and fusion after anterior radical debridement and fusion in the surgical treatment of spinal tuberculosis: experience of 127 cases. J Spinal Disord Tech. 2006;19:554–559. doi: 10.1097/01.bsd.0000211202.93125.c7. [DOI] [PubMed] [Google Scholar]
- 18.Lifeso RM, Weaver P, Harder EH. Tuberculous spondylitis in adults. J Bone Joint Surg Am. 1985;67:1405–1413. [PubMed] [Google Scholar]
- 19.Rajasekaran S, Soundarapandian S. Progression of kyphosis in tuberculosis of the spine treated by anterior arthrodesis. J Bone Joint Surg Am. 1989;71:1314–1323. [PubMed] [Google Scholar]
- 20.Korkusuz F, Islam C, Korkusuz Z. Prevention of postoperative late kyphosis in Pott's disease by anterior decompression and intervertebral grafting. World J Surg. 1997;21:524–528. doi: 10.1007/PL00012280. [DOI] [PubMed] [Google Scholar]