Abstract
Purpose
Video-assisted thoracoscopic surgery (VATS) has become an alternative tool for a variety of spinal conditions as this approach minimises much morbidity related to conventional thoracotomy. The purpose of this study was to determine the efficacy of VATS and its long-term results in patients with dorsal spinal tuberculosis.
Materials and methods
This retrospective long-term follow-up study of VATS-assisted surgical treatment of dorsal spine tuberculosis included 30 patients with a mean age of 33.5 years (range 15–60). Patients with dorsal spine tuberculosis who were suitable surgical candidates for VATS underwent a three-portal thoracoscopy for decompression with/without fusion of the spine along with routine chemotherapy for tuberculosis (TB). Patients were assessed for blood loss, duration of surgery, postoperative incision pain, duration of hospital stay, neurological recovery, and progression of deformity. Patients were observed for a minimum of five years.
Results
The mean duration of surgery was 158.8 min (range 90–220 min) with mean blood loss of 296.7 ml (range 200–450 ml). Complications were seen in ten patients. The mean follow-up was 80 months (range 60–90 months) with neurological improvement and return of ambulatory power in all patients at final follow-up. There was an average increase in kyphus angle by 7.5° at final follow-up and 95% of patients achieved an excellent or good subjective outcome.
Conclusion
VATS-assisted surgical decompression can be a safe and effective technique for anterior debridement and fusion in tuberculosis of the dorsal spine to achieve neurological recovery with reduced morbidity, blood loss, and hospital stay compared to thoracotomy.
Introduction
Tuberculosis (TB) is the most common infectious disease worldwide [1], with spine being one of the most common sites of extra pulmonary involvement. Although TB chemotherapy is the mainstay of treatment for spinal TB [2], it may not be applicable to all patients such as those with worsening neurological deficit [3], where surgery would be required in addition. In the absence of major deformity, the primary goal of surgery in these cases is debridement of dead and necrotic tissue to achieve adequate cord decompression and good healing with fusion. Anterior radical debridement and bone grafting [4] has good results [5] and is a valuable surgical option in dorsal spinal TB, but thoracotomy is associated with high morbidity of 10–50% [6, 7] and prolonged hospital stay.
Video assisted thoracoscopic surgery (VATS) is a good surgical alternative to conventional thoracotomy with minimal morbidity [8, 9], though surgically demanding. VATS has been used extensively in spinal deformities such as scoliosis with results comparable to open procedures, but there has been limited use of VATS for decompression in active tuberculosis of dorsal spine [10–12]. The senior author (SK) has reported his early clinical results and good outcome in the past [12]. We now report 30 cases of dorsal spinal tuberculosis with a minimum five-years of follow-up who underwent anterior debridement via the VATS approach to assess the effectiveness of this technique with which we were able to achieve adequate decompression of the cord leading to neurological recovery and good healing of disease in all the cases.
Material and methods
This retrospective study was done at two tertiary care hospitals, Maulana Azad Medical College and Lady Hardinge Medical College New Delhi, following approval from the Institutional Review Boards. Inclusion criteria included single level dorsal spinal tuberculosis (D4–D11) managed with VATS-assisted anterior decompression with/without rib grafting with a minimum follow-up of five years. The indications for surgical decompression [13] were mainly failure of conservative treatment and progressive neurological deficit despite conservative treatment. Only fresh cases and those with soft tissue abscess visible radiologically were included in this study. The primary goal of surgery was adequate decompression of the cord with debridement of caseous material from the spinal canal and from the destroyed vertebral body. Complete vertebrectomy was neither intended nor performed in any of the cases. Cases with more than 50% destruction of vertebral body at the involved segment were scheduled for fusion using autologous rib graft. We excluded cases with thoracic kyphosis over 30° due to concerns regarding adequacy of decompression and kyphosis correction. All patients who were not candidates for endoscopic spine surgery were also excluded from this study [14]. Written informed consent was obtained from each patient and possible need of thoracotomy was also explained to all of them.
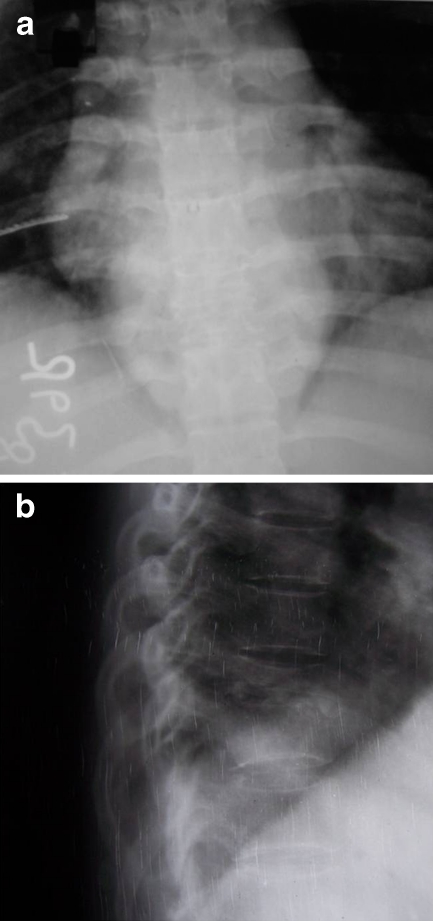
All patients received four-drug antitubercular treatment (RHZE) for a minimum of three weeks as per the Revised National Tuberculosis Control Programme (RNTCP) of India preoperatively. Neurological assessment was done as per Frankel Grading. Standard antero-posterior and lateral X-ray of the dorsal spine (Fig. 1a and 1b) and MRI (Fig. 2) were done in all the cases with routine investigations such as erythrocyte sedimentation rate (ESR). Perioperative measurements included operative time, blood loss, chest tube drainage, post operative pain using visual analogue scale (VAS), length of hospital stay and complications. The clinical outcome data were assessed preoperatively, at three months postoperatively and every six-months follow-up using subjective clinical results [13]. The results were analysed using suitable statistical tests.
Fig. 1.
a X-ray dorsal spine anteroposterior (AP) view showing paravertebral soft tissue shadow. b X-ray dorsal spine lateral view showing reduced disc space and collapsed vertebrae
Fig. 2.
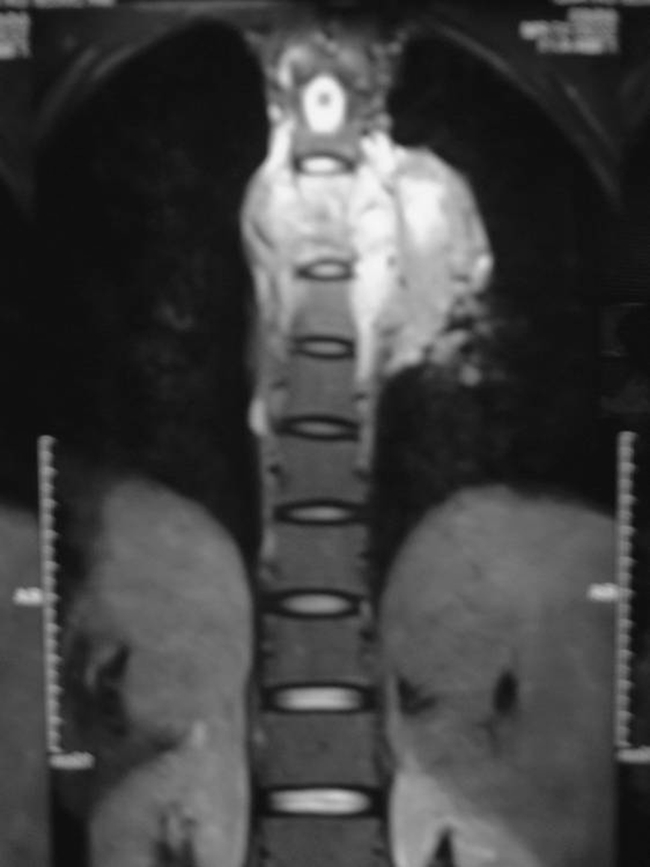
MRI dorsal spine T2W image showing large paravertebral abscess
Operative technique
The surgery was performed under general anaesthesia with a double-lumen endotracheal tube and single lung ventilation. The spine was approached from the left or right side, depending on the radiological findings (i.e., bulk of abscess and destruction of body). An initial 10-mm port for the thoracoscope was made in the sixth or seventh intercostal space near the anterior axillary line. After separating any pleural adhesions, a 25° thoracoscope was inserted for exploratory thoracoscopy. Under thoracoscopic visualisation, the level(s) of diseased vertebrae were identified by inserting Veress needles. Brief insufflation of carbon dioxide at a pressure of 8 cm H2O was used to assist if resorptive atelectasis of the ipsilateral lung was found incomplete. Visualisation of the spine was enhanced by tilting the patient forward so that the collapsed lung fell anteriorly. If required, a fan retractor was inserted thorough the second portal for further retraction of the ipsilateral lung. A thorough debridement was performed to remove necrotic disc, sequestra, infected granulation tissue and caseous material under direct vision through the thoracoscope. The working portals were enlarged to be used as extended manipulating channels, facilitating the use of conventional spinal instruments [15]. Anterior rib grafts were harvested by subcutaneous dissection of the ribs through the portal incision and used for anterior column support after debridement. Any segmental vessels visible at the operative site were ligated with double titanium clips. The decompression was considered complete only when the dura was exposed in the involved segment and appeared to be devoid of compression. The material removed was sent for histopathology examination. A chest tube was placed prior to wound closure.
Postoperative care
The chest tube was removed when output was less than 100 ml in the last 24 hours with radiological evidence of complete lung inflation. Pain was quantified as a function of postoperative analgesic requirement and on visual analog scale (VAS). The patients marked the grade of pain from 0 mm (absent) to 100 mm (most severe imaginable) on a 100-mm line drawing which was explained to the patients in the preoperative period. All patients received antitubercular treatment (ATT) as per the Revised National Tuberculosis Control Programme (RNTCP) of India postoperatively. In the initial part of the study total duration of ATT was 18 months (prolonged administration of RH), but later it was stopped at six months. The patients were discharged and followed-up in the outpatient department, initially at monthly intervals and later at three-month intervals, until the lesion was completely healed (clinically and radiologically) (Figs. 3, 4). Patients were allowed to sit up in bed with the help of a suitable spinal brace in the postoperative period and, depending on the extent of neurological recovery, ambulation was gradually encouraged. Liver function and ESR were also monitored at regular intervals.
Fig. 3.
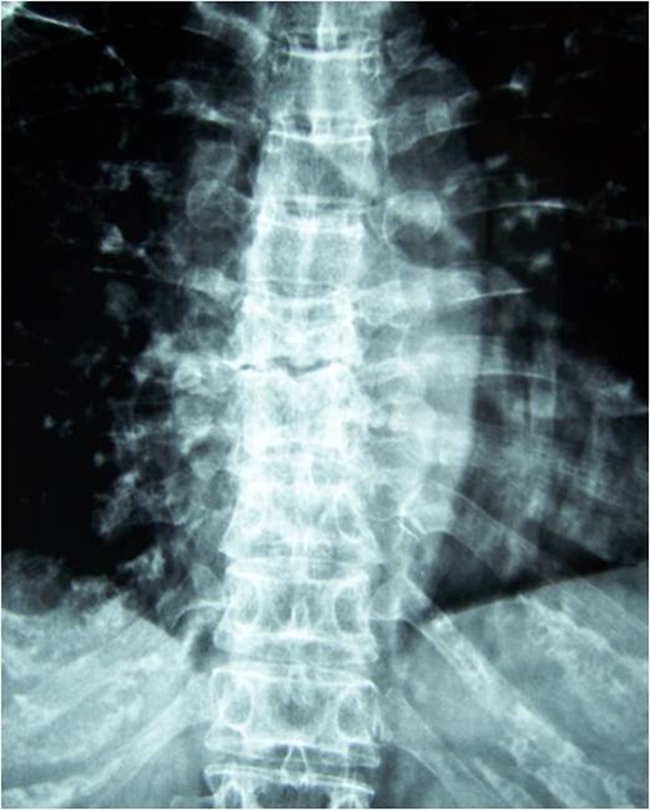
Radiological healing with increased density of vertebral body
Fig. 4.

Clinical photograph showing healed skin incisions
Results
There were 30 patients (Table 1) available for this retrospective review with mean age of 33.47 years (range 15–60). Back pain and constitutional symptoms such as low grade fever and weight loss were present in all the cases at the time of presentation. The mean duration of backache in the study group was 3.9 months with a range of one to eight months. Because of the low intensity of symptoms in TB, spine patients usually seek attention weeks to months after onset of the original symptoms. This explains in part the advanced degree of paraplegia seen at presentation in developing countries in a large number of cases as evident in our series also with all patients presenting with paraplegia of Frankel grade A or B. Overall, the most common site of involvement was D7-D8 (Table 1). All patients showed elevated ESR at the time of admission with mean value of 53 which improved during the course of treatment and began to approach normal by five to seven months in all the patients. Magnetic resonance imaging (MRI) showed a large paraspinal abscess and dural compression at the involved level in all cases.
Table 1.
Patient information
| Patient number | Age/gender | Duration of backache (months) | Duration of paraplegia (days) | Site | Duration of surgery (min) | Blood loss (ml) | Kyphus angle at admission | Change in kyphus angle at 60 months | Duration of incisional pain (days) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 40/ M | 2 | 18 | D7-D8 | 180 | 390 | 10 | 12 | 3 |
| 2 | 16/ M | 2 | 22 | D6-D7 | 160 | 300 | 13 | 7 | 3 |
| 3 | 24/ M | 4 | 8 | D6-D7 | 140 | 260 | 17 | 9 | 1 |
| 4 | 19/ F | 5 | 13 | D7-D8 | 120 | 320 | 22 | 5 | 2 |
| 5 | 50/ M | 3 | 22 | D4-D5 | 220 | 410 | 16 | 8 | 2 |
| 6 | 48/ F | 4 | 20 | D7-D8 | 160 | 360 | 23 | 6 | 1 |
| 7 | 15/ F | 1 | 11 | D7-D8 | 180 | 400 | 24 | 8 | 4 |
| 8 | 45/ M | 5 | 29 | D9-D10 | 115 | 250 | 15 | 2 | 2 |
| 9 | 22/ F | 3 | 13 | D5-D6 | 180 | 350 | 21 | 11 | 3 |
| 10 | 32/ F | 4 | 14 | D4-D5 | 210 | 450 | 13 | 9 | 1 |
| 11 | 17/ F | 1 | 20 | D8-D9 | 170 | 250 | 14 | 4 | 3 |
| 12 | 15/ F | 1 | 15 | D5-D6 | 150 | 270 | 12 | 7 | 5 |
| 13 | 25/ M | 2 | 15 | D7-D8 | 180 | 230 | 20 | 5 | 2 |
| 14 | 50/ F | 5 | 8 | D8-D9 | 170 | 300 | 8 | 7 | 3 |
| 15 | 30/ F | 4 | 15 | D7-D8 | 200 | 340 | 30 | 3 | 2 |
| 16 | 35/ F | 5 | 29 | D9-D10 | 165 | 280 | 15 | 10 | 1 |
| 17 | 15/ M | 6 | 30 | D5-D6 | 215 | 400 | 28 | 4 | 3 |
| 18 | 45/ F | 4 | 24 | D9-D10 | 190 | 200 | 21 | 5 | 4 |
| 19 | 45/ M | 3 | 60 | D7-D8 | 125 | 210 | 9 | 9 | 2 |
| 20 | 16/ M | 4 | 15 | D6-D7 | 130 | 270 | 19 | 15 | 2 |
| 21 | 15/ M | 5 | 18 | D7-D8 | 165 | 250 | 27 | 16 | 1 |
| 22 | 40/ F | 5 | 25 | D5-D6 | 180 | 450 | 28 | 3 | 8 |
| 23 | 42/ F | 6 | 25 | D6-D7 | 170 | 230 | 24 | 8 | 2 |
| 24 | 29/ M | 5 | 15 | D8-D9 | 100 | 250 | 19 | 14 | 2 |
| 25 | 60/ F | 8 | 55 | D9-D10 | 105 | 200 | 10 | 5 | 2 |
| 26 | 55/ F | 4 | 28 | D9-D10 | 140 | 280 | 28 | 4 | 1 |
| 27 | 45/ F | 3 | 25 | D4-D5 | 165 | 300 | 25 | 7 | 2 |
| 28 | 39/ F | 5 | 15 | D5-D6 | 150 | 250 | 16 | 6 | 2 |
| 29 | 15/ M | 3 | 10 | D4-D5 | 140 | 250 | 25 | 10 | 10 |
| 30 | 60/ F | 4 | 6 | D6-D7 | 90 | 200 | 17 | 7 | 1 |
M male, F female
A left-sided approach was used in 19 patients and a right-sided approach in 11. Autologus rib grafting at the involved segment was done in 11 patients. The mean duration of surgery was 158.8 min with mean blood loss of 296.7 ml. The average increase in duration of surgery and blood loss was 34.7 min and 31.7 ml in patients requiring rib grafting. The mean duration of chest tube drainage was 4.25 days (range two to nine days) while postoperative hospital stay was 8.8 days. The mean duration of postoperative incisional pain in was 2.7 days with 83% of patients reporting pain for one to three days. Diagnosis of tuberculosis was confirmed by histopathological examination in 23 cases but all the patients improved clinically as well as radiologically on subsequent follow-up.
The mean follow-up was 80 months (range 60–90 months). Based on the Frankel grading, all the patients improved neurologically (Table 2). No patient had neurological deterioration and all of them regained ambulatory power with no cases of recurrence of tuberculosis. The mean kyphotic angle before treatment was 18.9° (range 8–30°). Final X-ray examination showed an average increase in kyphus angle by 7.5°, with deformity remaining stationary in most of the patients (Table 1). There was no significant change in kyphotic angle between six months postoperatively and final follow-up (p = 0.68). There was also no statistically significant difference in final increase in kyphotic angle between patients managed with or without rib grafting (p = 0.31). The VAS score improved from a pretreatment score of 7.3 to a post-treatment score of 2.1 (p < 0.001, paired-sample t-test). There was a statistically significant difference (p < 0.001 with Student’s t test) in VAS for back pain at three months compared to the preoperative period and at five-year follow-up compared to three months (p < 0.001). For subjective outcomes, excellent results were obtained in 24 patients, good in four, and fair in two, with 95% of patients having a good or excellent result.
Table 2.
Change in neurological status
| Paraplegia grade (Frankel) | Cases on admission | At 3 months | At 12 months | At 60 months |
|---|---|---|---|---|
| Grade A | 24 | 0 | 0 | 0 |
| Grade B | 6 | 1 | 1 | 0 |
| Grade C | 0 | 23 | 13 | 1 |
| Grade D | 0 | 4 | 12 | 2 |
| Grade E | 0 | 2 | 4 | 27 |
There were ten complications including two cases of superficial wound infection which healed by secondary intention on oral antibiotics. There were six pulmonary complications such as pulmonary atelectasis, pleural effusion, and pneumonia in one each. All of these cases were treated expectantly with good recovery. Postoperative air leak was seen in one patient and there was a parenchymal lung injury caused by an adhesion at the very site of first port insertion in another one.
Discussion
Spinal tuberculosis still remains a major health problem in the developing world, contributing to deformity and neurological deficit. The surgical technique of choice, whenever required, for spinal tuberculosis has been a topic of discussion throughout the history of spinal surgery. In tuberculosis, since the compression is anterior, it is logical to decompress the spinal cord via the anterior approach. VATS can also be a useful alternative to conventional thoracotomy in TB of dorsal spine [11, 12] to avoid potentially delayed rehabilitation caused by postoperative pain and complications [16] of thoracotomy.
Unlike anterior release in scoliosis, thoracoscopic decompression in spinal tuberculosis is surgically more demanding because of grossly altered anatomy and inflammatory tissue making isolation of segmental vessels on the inflamed vertebrae difficult. This difficulty can be circumvented by identifying the rib head and then tracing back the intercostal nerve to the neural canal. It is also helped by proceeding from the unaffected area to the affected zone. But there is a steep learning curve before all the surgical goals of the open method such as instrumentation and deformity correction can be attained through minimal access surgery (VATS) in the tuberculous spine. Acknowledging this fact is important in patient selection, especially in the early stage of the learning curve, which is why we started thoracoscopy with decompression and debridement in TB spine. The broad indication for surgical decompression in our series of TB dorsal spine was the same, namely, the failure of adequate conservative treatment. However, indications for the use of thoracoscopic surgery were strict and specific. Only fresh cases with visible radiographic soft tissue shadow were operated upon using this technique. It made identification of the site, debridement of necrotic tissue, and decompression easier and safe.
One of the major goals of surgery was to achieve adequate neurological decompression through VATS. The decompression was adequate as indicated by the neurological recovery in most of the cases in accordance with available literature showing neurological recovery varying from 82 to 95% recovery of ambulatory status [17, 18]. Adequate debridement and decompression also makes room for healthy cancellous bone apposition resulting in high fusion rates [19, 20]. We did not include patients with multilevel disease or those with severe kyphosis. This might explain the favourable results we obtained including minimal progression of deformity on long-term follow-up. Working around the spinal cord in dorsal spine with a severe kyphotic deformity and inflammation is challenging even as an open procedure, but once the surgeon gains adequate surgical control and expertise severe deformities can also be addressed by VATS.
Strut grafts may not provide adequate anterior column support if they span more than two levels [3] and they must be protected with spinal braces until radiological evidence of fusion is seen. The same protocol was followed in all of our cases as all patients in this series had single level disease and they were also protected with suitable braces in the postoperative period for a sufficient period of time, though allowed to mobilise themselves. We observed no major spinal deformities on long-term follow-up in our series, and in our opinion these good results, even during the learning period, were due to careful patient selection and to our past experience in doing similar operations by open techniques.
One of the major reported advantages of VATS [21, 22] is the reduction in intraoperative blood loss and postoperative stay, and this was also observed in our series. The average duration of surgery and blood loss in our series is less than that reported by other authors [11, 23], which may be attributed to limitation to debridement and grafting only without the use of instrumentation in our patients. Postoperative stay was less than reported by thoracotomy patients in other studies [22], which is a major consideration in developing countries with a high patient load in tertiary care hospitals. Another advantage of any minimal access surgery is the cosmetically appealing small surgical scar along with less postoperative pain, early mobilisation and decreased chest infection risk compared to thoracotomy [22], since the rib cage is not widely retracted during surgery, leading to an early return of good chest movements in the postoperative period.
All the complications of conventional thoracotomy are still possible with the VATS procedure with a reported rate of 24.4–31.3% [12, 24, 25]. In our series, pulmonary complications were seen in 20% of cases. All lung complications such as atelectasis and pneumonia improved with perioperative pulmonary therapy. These pulmonary complications are usually due to lung parenchyma injury during mobilisation of lung adhesions from the chest wall.
This study has several limitations, including its retrospective, uncontrolled design despite the evaluation of prospectively collected data for the assessment of clinical outcomes in a relatively small sample of patients. Another potential disadvantage of this approach may be the involved higher cost of endoscopic instrumentation, which is an important consideration in developing countries. But these higher costs could, however, be offset by savings in the long term from avoiding unnecessary long duration of hospital admissions for such patients.
Anterior decompression in spinal tuberculosis is the gold standard procedure with time-tested results, but VATS can be considered as a valuable adjunct to the available options for spine surgery due to the advantages of decreased blood loss and reduced postoperative morbidity with good cosmetic acceptance. Reduced duration of stay in hospital is a definitive advantage as it helps to improve the efficiency of already overworked public hospitals with a relative shortage of beds. Selecting patients judiciously and acknowledging ones own surgical skill level can give both patient and surgeon a satisfying result.
Acknowledgments
Conflict of interest statement The authors declare that they have no conflict of interest.
References
- 1.World Health Organization (2008) Global tuberculosis control: surveillance, planning, financing. Publication no. WHO/HTM/TB/ 2008.393. World Health Organization, Geneva, Switzerland
- 2.Tuli SM. Results of treatment of spinal tuberculosis by “middle-path” regime. J Bone Joint Surg. 1975;57B:13–23. [PubMed] [Google Scholar]
- 3.Rajasekaran S, Soundarapandian S. Progression of kyphosis in tuberculosis of spine treated by anterior arthrodesis. J Bone Joint Surg Am. 1989;71:1314–1323. [PubMed] [Google Scholar]
- 4.Hodgson AR, Stock FE, Fang HS, Ong GB. Anterior spinal fusion. The operative approach and pathological findings in 412 patients with Pott’s disease of the spine. Br J Surg. 1960;48:172–178. doi: 10.1002/bjs.18004820819. [DOI] [PubMed] [Google Scholar]
- 5.Upadhyay SS, Sell P, Saji MJ, Sell B, Hsu LC. Surgical management of spinal tuberculosis in adults. Hong Kong operation compared with debridement surgery for short and long term outcome of deformity. Clin Orthop Relat Res. 1994;302:173–182. [PubMed] [Google Scholar]
- 6.Amini A, Beisse R, Schmidt MH. Thoracoscopic spine surgery for decompression and stabilization of the anterolateral thoracolumbar spine. Neurosurg Focus. 2005;19:E4. [PubMed] [Google Scholar]
- 7.Ikard RW. Methods and complications of anterior exposure of the thoracic and lumbar spine. Arch Surg. 2006;141:1025–1034. doi: 10.1001/archsurg.141.10.1025. [DOI] [PubMed] [Google Scholar]
- 8.Newton PO, Marks M, Faro F, Betz R, Clements D, Haher T, Lenke L, Lowe T, Merola A, Wenger D. Use of video assisted thoracoscopic surgery to reduce perioperative morbidity in scoliosis surgery. Spine. 2003;28:S249–S254. doi: 10.1097/01.BRS.0000092475.04293.F5. [DOI] [PubMed] [Google Scholar]
- 9.Crawford AH. Anterior surgery in the thoracic and lumbar spine: endoscopic techniques in children. Instr Course Lect. 2005;54:567–576. [PubMed] [Google Scholar]
- 10.Dusmet M, Halkic N, Corpataux JM. Video assisted thoracic surgery diagnosis of thoracic spinal tuberculosis. Chest. 1999;116:1471–1472. doi: 10.1378/chest.116.5.1471. [DOI] [PubMed] [Google Scholar]
- 11.Huang TJ, Hsu RW, Chen SH, Liu HP. Video-assisted thoracoscopic surgery in managing tuberculous spondylitis. Clin Orthop Relat Res. 2000;379:143–153. doi: 10.1097/00003086-200010000-00017. [DOI] [PubMed] [Google Scholar]
- 12.Kapoor SK, Agarwal PN, Jain BK, Jr, Kumar R. Videoassisted thoracoscopic decompression of tubercular spondylitis: clinical evaluation. Spine (Phila Pa 1976) 2005;30:E605–E610. doi: 10.1097/01.brs.0000182328.03082.e2. [DOI] [PubMed] [Google Scholar]
- 13.Griffiths DL, Seddon HJ, Roaf R (1956) Pott’s paraplegia. Oxford University Press, London
- 14.Regan JJ (1997) Endoscopic spine surgery. In: Frymoyer J et al. (eds) The adult spine: principle and practice. Raven, Philadelphia, pp 1665–1684
- 15.Huang TJ, Hsu RW, Liu HP, Liao YS, Shih HN. Technique of video assisted thoracoscopic surgery for the spine: new approach. World J Surg. 1997;21:358–362. doi: 10.1007/PL00012253. [DOI] [PubMed] [Google Scholar]
- 16.Faciszewski T, Winter RB, Lonstein JE, Denis F, Johnson L. The surgical and medical perioperative complications of anterior spinal fusion surgery in the thoracic and lumbar spine in adults. A review of 1223 procedures. Spine (Phila Pa 1976) 1995;20:1592–1599. doi: 10.1097/00007632-199507150-00007. [DOI] [PubMed] [Google Scholar]
- 17.Louw JA. Spinal tuberculosis with neurological defect: treatment with anterior vascularised rib grafts, posterior osteotomies and fusion. J Bone Joint Surg Br. 1990;72:686–693. doi: 10.1302/0301-620X.72B4.2380228. [DOI] [PubMed] [Google Scholar]
- 18.Jain AK, Aggarwal A, Dhammi IK, Aggarwal PK, Singh S. Extrapleural anterolateral decompression in tuberculosis of the dorsal spine. J Bone Joint Surg Br. 2004;86:1027–1031. doi: 10.1302/0301-620X.86B7.14546. [DOI] [PubMed] [Google Scholar]
- 19.Medical Research Council A 10year assessment of a controlled trial comparing debridement and anterior spinal fusion in the management of tuberculosis of the spine in patients on standard chemotherapy in Hong Kong: Eighth report of the Medical Research Council working party on the tuberculosis of the spine. J Bone Joint Surg Br. 1982;64:393–398. doi: 10.1302/0301-620X.64B4.7047536. [DOI] [PubMed] [Google Scholar]
- 20.Laheri VJ, Badhe NP, Dewnany GT. Single stage decompression, anterior interbody fusion and posterior instrumentation for tuberculosis kyphosis of the dorsolumbar spine. Spinal Cord. 2001;39:429–436. doi: 10.1038/sj.sc.3101185. [DOI] [PubMed] [Google Scholar]
- 21.Landerneau RJ, Hazelrigg SR, Mack MJ, et al. Postoperative pain related morbidity: Video assisted thoracic surgery versus thoracotomy. Ann Thorac Surg. 1993;56:1285–1289. doi: 10.1016/0003-4975(93)90667-7. [DOI] [PubMed] [Google Scholar]
- 22.Mangione P, Vadier F, Senegas J. Thoracoscopy versus thoracotomy in spinal surgery: comparison of two paired series. Rev Chir Orthop Repratrice Appar Mot. 1999;85:574–580. [PubMed] [Google Scholar]
- 23.Lu G, Wang B, Li J, Liu W, Cheng I (2011) Anterior debridement and reconstruction via thoracoscopy assisted mini-open approach for the treatment of thoracic spinal tuberculosis: minimum 5-year follow-up. Eur Spine J. Oct 14 [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 24.Huang TJ, Hsu RW, Sum CW, Liu HP. Complications in thoracoscopic spinal surgery: a study of 90 consecutive patients. Surg Endosc. 1999;13:346–350. doi: 10.1007/s004649900987. [DOI] [PubMed] [Google Scholar]
- 25.Watanabe K, Yabuki S, Konno S, Kikuchi S. Complications of endoscopic spinal surgery: a retrospective study of thoracoscopy and retroperitoneoscopy. J Orthop Sci. 2007;12:42–48. doi: 10.1007/s00776-006-1086-x. [DOI] [PubMed] [Google Scholar]