Abstract
Purpose
We evaluated the clinical efficacy and feasibility of one-stage posterior internal fixation, debridement and interbody thoracic fusion in the treatment of thoracic tuberculosis.
Methods
Sixty adult patients with monosegmental thoracic tuberculosis were studied retrospectively: 34 men and 26 women with an average age of 37.5 years. Operating time, blood loss, time in bed, complications, neurological function, rate of deformity correction and rate of interbody fusion were investigated.
Results
All cases were followed up for 27.5 months on average. Average mean operating time was 251 min, evaluated blood loss during operation 780 ml, rate of kyphosis correction 79%, corrected kyphosis angle 25° and loss of corrected angle 1.2°. Patients whose neurological function improved accounted for 90.1%. Erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP) decreased to normal levels three months after operation. The rate of bone fusion was 100%, with a 100% cure rate. No severe complications or spinal cord injury occurred.
Conclusions
This approach can successfully remove the focus of tuberculosis with complete interbody thoracic fusion after operation, which restores spinal stability.
Introduction
In recent years, global tuberculosis (TB) incidence has increased due to population migration, increase in the number of patients with HIV infection, emergence of antibiotic-resistant strains and other reasons [1, 2]. Spinal TB leads to increased pressure on the spine and therefore causes neurological injury [2–4]. The chief aim of surgical treatment is focal clearance of TB, relief of spinal nerve compression, reconstruction of spinal stability and correction of the serious spinal deformity [3, 5–7]. The detailed approach of the surgery varies according to patient characteristics [5, 6, 8]. This study reviewed patients with monosegmental spinal TB (MST) following one-stage internal fixation, debridement and interbody thoracic fusion via a posterior approach only [9]. Sixty patients treated in our department from February 2005 to February 2009 were retrospectively analysed.
Patients and methods
Patients
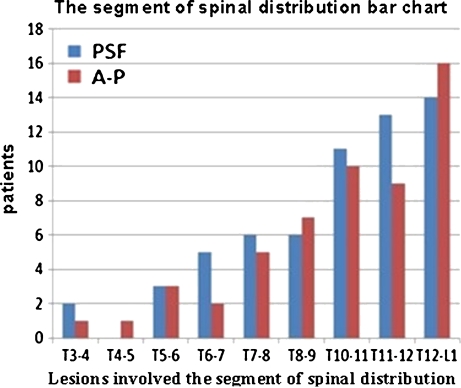
A total of 114 patients with MST were studied. Sixty underwent one-stage internal fixation, debridement and interbody thoracic fusion to treat thoracic TB via a posterior approach only (posterior spinal fusion) (PSF) group. Another 54 cases who underwent one-stage or phased debridement and interbody thoracic fusion via the posterior approach and internal fixation via the anterior approach to treat thoracic TB were the control group (combined anterior/posterior surgery) (A-P) group (Tables 1, 3 and 4; Fig. 1).
Table 1.
General condition of the two groups of patients
| Posterior spinal fusion (PSF) group | Anterior/posterior combined surgery (A-P) group | |
|---|---|---|
| Number | 60 | 54 |
| Sex (male/female) | 34/26 | 30/24 |
| Average age | 37.5 ± 14.7 | 36.9 ± 12.9 |
| Follow-up time (month) | 27.5 ± 3.3 | 26.1 ± 4.0 |
| Obvious kyphosis deformity (sagittal >15°) | 38 | 33 |
| Spinal cord dysfunction (number) | 21 | 24 |
| Average erythrocyte sedimentation rate (ESR) (mm/h) | ||
| Male | 47.7 ± 30.9 | 49.8 ± 32.8 |
| Female | 57.2 ± 30.8 | 57.5 ± 38.1 |
| Average C-reactive protein (CRP) (mg/L) | 29.5 ± 17.2 | 31.9 ± 16.5 |
Table 3.
Preoperative and postoperative American Spinal Injury Association (ASIA) classification comparison of the posterior spinal fusion (PSF) and combined anterior/posterior (A-P) groups
| ASIA classification | PSF group (n) | A-P group (n) | ||||||
|---|---|---|---|---|---|---|---|---|
| Preoperative | Postoperative | Final follow-up | Improvementa | Preoperative | Postoperative. | Final follow-up | Improvementa | |
| A | ||||||||
| B | 2 | 2 | 1 | 1 | 3 | 3 | 1 | 2 |
| C | 7 | 3 | 2 | 6 | 9 | 5 | 4 | 7 |
| D | 15 | 10 | 7 | 13 | 12 | 11 | 7 | 12 |
| E | 36 | 45 | 50 | 29 | 35 | 42 | ||
aASIA grade 1 and above improvement compared with preoperative and final follow-up. Spinal cord function improvement rate: PSF group approximately 90.1%; A-P group approximately 87.5%
Table 4.
Preoperative and postoperative erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) comparison between posterior spinal fusion (PSF) and combined anterior/posterior (A-P) groups
| Index | PSF group | A-P group | ||||
|---|---|---|---|---|---|---|
| Preoperative | Postoperative | 3 months after operation | Preoperative | Postoperative | 3 months after operation | |
| ESR (mm/L) | ||||||
| Male | 47.7 ± 30.9 | 61.3 ± 22.1 | 8.6 ± 3.5 | 49.8 ± 32.8 | 72.3 ± 23.3 | 8.1 ± 3.1 |
| Female | 57.2 ± 30.8 | 70.0 ± 23.8 | 9.9 ± 4.7 | 57.5 ± 38.1 | 77.5 ± 20.5 | 10.5 ± 3.8 |
| CRP (mg/) | 29.5 ± 17.2 | 35.3 ± 12.3 | 5.1 ± 2.1 | 31.9 ± 16.5 | 47.1 ± 15.7 | 5.6 ± 1.8 |
Fig. 1.
Lesions involved in the segment of spinal distribution in the posterior spinal fusion (PSF) and anterior/posterior combined surgery (A-P) groups
All patients were primary cases, showed slow disease development , low-back pain, rigidity and other symptoms. Computed tomography (CT) and/or magnetic resonance imaging (MRI) examinations showed different levels of vertebral bone destruction, uneven signals of bone, smaller intervertebral space, paravertebral abscess and lack of sinus-tract formation. The study was approved by Ethics Committee of Medical Research at Xiangya Hospital of Central South University, PRC, and informed consent was obtained orally from all participants.
Pre-operative management
X-ray film, CT, MRI, ESR and CRP tests were done for all patients. Chest-X ray and electrocardiographs (ECG) were used to exclude other concurrent diseases of a cardiopulmonary nature. Regular anti-TB chemotherapy and supportive therapy were given: rifampin 0.3 g, isoniazid 0.45 g and ethambutol 0.75 g daily for seven to 14 days. The operation was performed when ESR and CRP gradually decreased, TB toxicity symptoms obviously improved and nutritional state changed for the better.
Operation
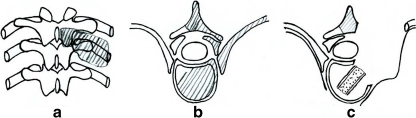
In the PSF group, the following procedures were performed: unilateral facet joint resection; excision of the upper or lower costotransverse joint with a small fragment of ribs; to decompress at 270°; interbody thoracic bone-graft fusion; internal fixation of pedicle screw; fusion between spinous processes and laminae via posterior approach [10] (see Fig. 2).
Fig. 2.
Resection range (shaded portion). C resected zygapophyseal joint, costotransverse joint and small portion of ribs, outward pressure on pleura, bone graft after debridement (shaded portion above discretionary resection portion)
In the A-P group, the following procedures were undertaken: debridement and interbody thoracic fusion were performed first via the anterior approach; internal fixation using a pedicle screw was done later via the posterior approach.
Postoperative management
Antibiotics were given i.v. during the first week after operation; the drainage tube was removed when drainage volume was less than 20 ml/24 hours; stitches were removed two weeks after operation. Patients were asked to wear a brace as soon as possible and for six months [11]. TB treatment with (HRES) lasted for two months after operation, and with isoniazid, rifampicin and ethambutol (HRE) treatment for nine to 15 months. Examination frequency after the operation was once a month to monitor ESR and liver and kidney function. X-ray examination was performed every three months.
Recorded parameters
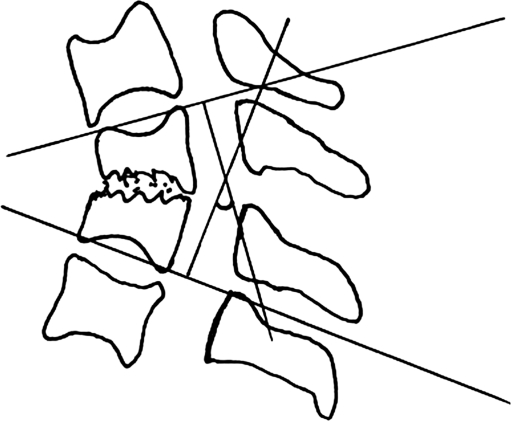
Surgery duration, blood loss during surgery, average time to standing following surgery (day) or postoperative recovery time and clinical complications were recorded. ESR and CRP were checked immediately one month, and three months after the operation. X-ray and CT examinations were performed regularly after the operation, and angular kyphosis was measured. The sagittal index (SI) was used to evaluate the deformity. SI = Gardner segmental deformity posterior convex angle—thoracic/lumbar basis vertebra angle) (Fig. 3).
Fig. 3.
Segmental deformity Angle measurement schemes. Lesions involving the cephalic vertebral endplate above normal and end the vertebral endplate below the normal do two parallel lines, measurement of vertical line Angle
Correct rate = preoperative SI—postoperative SI/preoperative SI x 100%.
Lost corrective angle calculation: lost corrective angle = final follow-up SI—postoperative SI.
Criteria for bone-graft fusion rate: continuity of trabeculae through the bone graft space, fusion segments not active (under 3°) in X- ray of flexion and extension; no trabeculae through the bone graft space, fusion segments not active (>3°) in flexion and extension X-ray.
The standard for spinal TB cure was no relapse six months after operation; ESR within normal range; X-ray showing fusion of pathological vertebrae; recovery of normal activities and work for three to six months. Cure rates in the two groups were also calculated. Postoperative nerve function was assessed using the American Spinal Injury Association (ASIA) classification: Improvement rate = cases of ASIA classification improvement one or more levels/total number of nerve function disorders × 100%. All statistical analyses were done using SPSS 16.0 software.
Results
Results were recorded and analysed with SPSS 16.0 software. Student’s t test for surgery duration (min), blood loss (ml), and average time to standing suggested a significant difference between groups (p < 0.001). There was no significant difference in corrected angle and loss of corrected angle and no significant differences in improvement rates in the ASIA classification, as shown by X-ray (p > 0.05) (Tables 2, 3 and 4).
Table 2.
Surgical results of posterior spinal fusion (PSF) and anterior/posterior combination (A-P) groups
| PSF group | A-P group | |
|---|---|---|
| Surgery duration time(min) | 251 ± 57.9 | 402 ± 59.2 |
| Blood loss(ml) | 780 ± 408.5 | 1129 ± 447.7 |
| Spinal cord function improvement rate(%) | 90.1 | 87.5 |
| Sagittal index (°) | ||
| Preoperative | 32 ± 11.5 | 33 ± 13.0 |
| Postoperative | 6.8 ± 3.7 | 7 ± 4.0 |
| Corrective angle | 25 ± 9.3 | 26 ± 9.6 |
| Correction rate of kyphosis angle (%) | 79 ± 9.9 | 80 ± 8.4 |
| Loss of correction angle (°) | 1.2 ± 1.0 | 1.3 ± 1.2 |
| Average time to stand (days) | 8.3 ± 2.1 | 12 ± 2.2 |
The following is a description of a typical case in our practice.
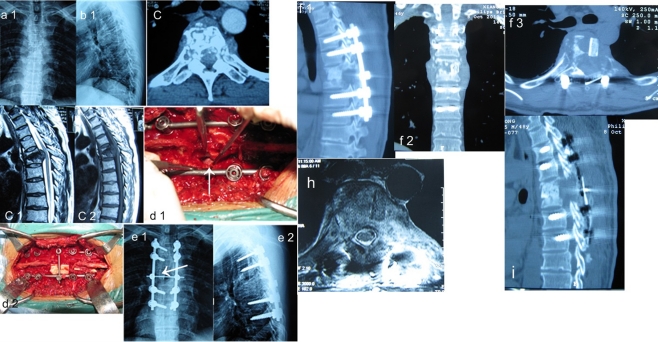
Male, 47 years old. Due to back pain and bilateral lower extremity weakness, hospitalised in March. Neurological function, ASIA grade C. T5–6 intervertebral damage as the centre of single-segment spinal TB, disc completely destroyed and corresponding vertebral body destruction; peripheral abscess. The left sided, focal cleaning, intervertebral bone grafting with Moss Miami screw-rod system (Johnson & Johnson) and allogenic homograft (Shanxi OsteoRad, China). Preoperative SI, 7°; postoperative SI, 0°. Bone graft fusion at 12 months. Correction angle lost 3°, ASIA grade of nerve function recovered to grade E (Fig. 4).
Fig. 4.
a1, a2 Preoperative lateral X-ray; b2 preoperative computed tomography (CT); c1, c2 preoperative magnetic resonance image (MRI)clearly shows T5–6bone destruction, peripheral abscess formation, oppressed spinal cord, stable fixation location and bone graft has integrated. d1, d2 Intraoperative images: d1 arrow shows implanted bone mass of between vertebral bodies; d2 bone graft on the vertebral plate and reconstruction. e1, e2 Postoperative lateral X-ray: arrow shows bone graft between vertebral bodies. e1, e2 Postoperative CT; h postoperative MRI shows stable bone mass and internal fixation. i Two years later, CT review shows interbody bone graft has merged
Discussion
In recent years the trends in surgical treatment of thoracic TB have been smaller incisions, static internal fixation and only one patient position during the operation [3, 12]. Here we describe simple internal fixation, debridement and interbody thoracic fusion via one-stage posterior approach only, with debridement, interbody bone graft and internal fixation performed in one operation, with decompression at 270° under direct vision, without causing injury to the spinal cord—all of which demonstrates its major clinical value.
The fact that the thoracic spinal canal volume is small makes this region more susceptible to spinal cord injury [12–15]. Infringement of the anterior and middle column in most cases of spinal TB made it difficult to operate from the back. The approach described here creates enough operating space through resection of the side of the facet joint, the diapophysis, costosternal joints and small rib portions, allowing operation on the vertebral body at a 270° angle under direct visualisation of the outside of the dura mater for complete removal of the focal TB without injuring the spinal cord. Spinal stability of all patients was unaffected by this approach, and all patients attained bony fusion. ESR and CRP values recovered within three months of surgery. Long-term follow-up (average 27.5 months) showed that loss of correction angle was only 1.2°, which is almost negligible, and the rate of internal fixation failure was zero. We conclude that even with the decreased stability caused by resection of the zygapophyseal and costotransverse joints, the final outcome of our approach was satisfying.
It has been suggested that removing the TB focus using the posterior approach could cause intraspinal infection and central nervous system complications of TB infection, such as TB meningitis [8, 16]. Results obtained from this study showed that no patients had TB meningitis, consistent with the other efforts reports [10]. Surgery duration, blood loss, and postoperative recovery time were significantly shorter, and complications were less frequent in the PSF group than in the A-P group. Additionally, complete focal cleaning expanded the scope of operation and allowed removal of all necrotic tissue. We believe this also helps recovery. However, TB cure still relies on formal chemotherapy [17].
Selecting the PSF approach requires the following criteria: A single-section thoracic TB, small paravertebral abscess and a TB lesion that can be removed. One of the following situations were present in our patients: (1) vertebral body collapse and unstable vertebra caused by bone destruction; (2) spinal cord compressed by the abscess, caseous necrosis material, progressively exacerbated clinical neurological symptoms; (3) obvious kyphosis (SI >15°) or ongoing deformities becoming more serious; (4) larger porosis and dead bone, especially around the intervertebral. The posterior approach is especially applicable for upper thoracic lesions and when the anterior approach is risky.
In conclusion, our study showed that simple internal fixation, debridement and interbody thoracic fusion via a one-stage posterior approach for treatment of thoracic TB allowed complete removal of the focus of the TB and permitted intervertebral bone graft implant, with good orthopaedic effect on kyphosis deformity and reconstruction of the spinal stability, with promising clinical effect.
Conflicts of interest None declared.
Footnotes
Author contributions
All authors contributed to the design and performance of the experiment and wrote the manuscript and approved the final version.
References
- 1.Houshian S, Poulsen S, Riegels-Nielsen P. Bone and joint tuberculosis in Denmark: increase due to immigration. Acta Orthop Scand. 2000;71:312–315. doi: 10.1080/000164700317411942. [DOI] [PubMed] [Google Scholar]
- 2.Almeida A. Tuberculosis of the spine and spinal cord. Eur J Radiol. 2005;55:193–201. doi: 10.1016/j.ejrad.2005.04.018. [DOI] [PubMed] [Google Scholar]
- 3.Issack PS, Boachie-Adjei O (2011) Surgical correction of kyphotic deformity in spinal tuberculosis. Int Orthop. doi:10.1007/s00264-011-1292-9 [DOI] [PMC free article] [PubMed]
- 4.Vidyasagar C, Murthy HK. Spinal tuberculosis with neurological deficits. Natl Med J India. 1996;9:25–27. [PubMed] [Google Scholar]
- 5.Xue HB, Ma YZ, Chen X, Li HW, Cai XJ, Guo LX, Peng W. Surgical treatment of spinal tuberculosis in aged. Zhonghua Wai Ke Za Zhi. 2007;45:1233–1236. [PubMed] [Google Scholar]
- 6.Jutte PC, Van Loenhout-Rooyackers JH (2006) Routine surgery in addition to chemotherapy for treating spinal tuberculosis. Cochrane Database Syst Rev:CD004532. DOI 10.1002/14651858.CD004532.pub2 [DOI] [PubMed]
- 7.Dharmalingam M. Tuberculosis of the spine-the Sabah experience. Epidemiology, treatment and results. Tuberculosis (Edinb) 2004;84:24–28. doi: 10.1016/j.tube.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 8.Ramdurg SR, Gupta DK, Suri A, Sharma BS, Mahapatra AK. Spinal intramedullary tuberculosis: a series of 15 cases. Clin Neurol Neurosurg. 2009;111:115–118. doi: 10.1016/j.clineuro.2008.09.029. [DOI] [PubMed] [Google Scholar]
- 9.Jain AK. Tuberculosis of the spine: a fresh look at an old disease. J Bone Joint Surg Br. 2010;92:905–913. doi: 10.1302/0301-620X.92B7.24668. [DOI] [PubMed] [Google Scholar]
- 10.Zhang HQ, Wang YX, Guo CF, Liu JY, Wu JH, Chen J, Guo D, Tang MX. One-stage posterior approach and combined interbody and posterior fusion for thoracolumbar spinal tuberculosis with kyphosis in children. Orthopedics. 2010;33:808. doi: 10.3928/01477447-20100924-10. [DOI] [PubMed] [Google Scholar]
- 11.Zhang HQ, Wang YX, Guo CF, Zhao D, Deng A, Wu JH, Liu JY. One-stage posterior focus debridement, fusion, and instrumentation in the surgical treatment of cervicothoracic spinal tuberculosis with kyphosis in children: a preliminary report. Childs Nerv Syst. 2011;27:735–742. doi: 10.1007/s00381-010-1319-3. [DOI] [PubMed] [Google Scholar]
- 12.Sihoe AD, Shiraishi Y, Yew WW. The current role of thoracic surgery in tuberculosis management. Respirology. 2009;14:954–968. doi: 10.1111/j.1440-1843.2009.01609.x. [DOI] [PubMed] [Google Scholar]
- 13.Blasberg JD, Donington JS. Infections and radiation injuries involving the chest wall. Thorac Surg Clin. 2010;20:487–494. doi: 10.1016/j.thorsurg.2010.06.003. [DOI] [PubMed] [Google Scholar]
- 14.Lee SF, Lawrence D, Booth H, Morris-Jones S, Macrae B, Zumla A. Thoracic empyema: current opinions in medical and surgical management. Curr Opin Pulm Med. 2010;16:194–200. doi: 10.1097/MCP.0b013e32833883f5. [DOI] [PubMed] [Google Scholar]
- 15.Pezzella AT, Fang W. Surgical aspects of thoracic tuberculosis: a contemporary review–part 1. Curr Probl Surg. 2008;45:675–758. doi: 10.1067/j.cpsurg.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 16.Muthukumar N, Venkatesh G, Senthilbabu S, Rajbaskar R (2006) Surgery for intramedullary tuberculoma of the spinal cord: report of 2 cases. Surg Neurol 66:69–74; discussion 74. DOI 10.1016/j.surneu.2005.10.024 [DOI] [PubMed]
- 17.LoBue PA, Enarson DA, Thoen TC. Tuberculosis in humans and its epidemiology, diagnosis and treatment in the United States. Int J Tuberc Lung Dis. 2010;14:1226–1232. [PubMed] [Google Scholar]