Abstract
Purpose
Approximately 5% of patients with spinal tuberculosis will develop a severe kyphotic deformity resulting in increased potential for pain, spinal cord compression, cardiopulmonary dysfunction, costopelvic impingement and cosmetic concerns. This manuscript reviews the evaluation and surgical management of tuberculous kyphosis.
Methods
This is a review article.
Results
Risk factors for the development of severe kyphosis include those who develop spinal tuberculosis as children, multiple vertebral body involvement and thoracic spine involvement. These complications can be prevented by early diagnosis and treatment of spinal tubercular lesions at stages with little to no deformity. When tubercular lesions result in progression of kyphosis to more than 50 degrees, the deformity should be surgically corrected to avoid problems associated with sagittal imbalance. There are several operations described for the treatment of kyphosis secondary to tuberculous spondylitis. The type of the operation depends on the magnitude of correction required.
Conclusions
Anterior, posterior and combined techniques as well as osteotomies and vertebral column resection have been described to correct spinal alignment and restore sagittal balance.
Introduction
Spinal tuberculosis is one of the most common world-wide causes for development of a kyphotic spinal deformity [1–7]. On average, patients with spinal tuberculosis treated nonsurgically show an increase in deformity of about 15 degrees [4], and approximately 5% of patients will develop a severe kyphotic deformity resulting in pain, spinal cord compression, cardiopulmonary dysfunction, costopelvic impingement and cosmetic concerns [2–4]. While the risk of significant progression in the healing stages of the disease is low in adults, in children, spondylitic kyphosis continues to increase with growth even after the tuberculous lesion has healed [3–6].
The worst complication of a progressive kyphotic deformity is a progressive neurological deficit or paraplegia. Neurological complications can be related to the disease itself or the progression of deformity after the disease has healed [8]. Patients who develop paraplegia early in the active stages of tuberculosis require aggressive treatment including chemotherapy and surgery [9]. These patients do better than those who develop paraplegia years after the initial disease has healed. Late paraplegia is prevented by restricting the progression of kyphosis with early stabilisation surgery [8]. Surgical treatment of the lesions involves debridement and reconstruction of the normal sagittal plane alignment of the spine. Surgery is indicated if the lesions are not responding to antibiotics, if there is severe and/or progressive kyphosis, or a developing neurological deficit [1, 2]. There are several techniques described for the treatment of tuberculous spondylitic kyphosis and this review focuses on the indications and outcomes of these techniques.
Risk factors for deformity progression
It is certainly easier and less risky to surgically stabilise a progressive kyphotic deformity in the earlier stages when the magnitude does not require osteotomies or anterior releases to effect deformity correction. It is therefore valuable to identify risk factors which may lead to the development of a severe kyphotic deformity. Rajasekaran identified radiographic signs of instability in paediatric patients with spinal tuberculosis being treated with chemotherapy [5]. These signs included facet dislocation, retropulsion of the diseased fragments, lateral vertebral translation and toppling of the superior vertebra. These signs can help identify patients who are at risk for deformity progression of more than 30 degrees and a final deformity of over 60 degrees.
In a later study by the same group, 61 children under age 15 years with tuberculous spondylitis were followed up to identify risk factors for deformity progression. All demonstrated an increase in deformity during the active disease phase, and 26 continued to progress during the quiescent phase until the growth was complete. In 21 of those 26, there was an increase in angular kyphosis with a final deformity less than 90 degrees. In the other five, the deformity was greater than 100 degrees and associated with facet dislocation and sagittal rotation of the vertebral segments resulting in horizontal vertebrae with vertical growth plates. Risk factors for this “buckling collapse” effect included an age of less than seven years, thoracolumbar involvement, loss of more than two vertebral bodies, and presence of radiographic signs of instability [6]. These patients should be carefully observed with surgical intervention performed before any large increase occurs in the magnitude of the deformity [6, 10].
Overview of surgical treatment
Indications for surgical management of tuberculous spondylitic kyphosis include lack of response to antibiotics, severe and/or progressive kyphosis, or a developing neurological deficit [1, 2]. Surgical correction of deformity requires instrumentation of the infected spine which has not been shown to create a nidus for persistent infection when combined with radical debridement and anti-tubercular chemotherapy [11, 12]. In general, debridement is performed anteriorly as the pathology is typically located in the vertebral bodies. In addition, anterior debridement is essential in cases of neurological impairment, multilevel involvement or severe abscess formation [13, 14]. Anterior debridement may be followed by anterior reconstruction with bone graft and either anterior or posterior instrumentation [2, 7, 12, 13, 15–23]. For larger degrees of kyphotic deformity (greater than 80 degrees of kyphosis) and stiffer curves (less than 25% flexibility), several types of osteotomies may be helpful in increasing curve flexibility [24–37].
Anterior debridement and uninstrumented fusion
The success of anterior debridement followed by an uninstrumented fusion has been shown to be inversely correlated with the length of the reconstruction. In an eight year follow-up of 81 patients with spinal tuberculosis treated by anterior debridement and anterior arthrodesis, 59% of the patients demonstrated sagittal plane stability at final follow-up with little additional kyphotic progression. These patients demonstrated minimal bone destruction requiring limited surgical debridement and a short rib autograft for deformity correction. Forty-one percent had fair to poor results, poor results were associated with more extensive vertebral disease requiring aggressive debridement with longer grafts (spanning more than two disc spaces). Poor results were also seen with thoracic vertebral involvement and significant preoperative kyphosis. Graft migration or resorption often occurred in these situations, with longer grafts more likely to fail [7]. These longer reconstructions probably should be supplemented by instrumentation.
Anterior debridement followed by anterior or posterior instrumentation
Several reports have shown good to excellent results with anterior decompression followed by either anterior or posterior instrumentation [12, 15, 17, 19–23, 38, 39]. Yilmaz et al. reported on 38 patients with spinal tuberculosis and moderate to severe kyphotic deformity with anterior decompression, strut grafting using either rib or iliac crest autograft or fibular allograft, and anterior instrumentation with vertebral screws and connecting rods [12]. Twenty-two patients with less than three involved vertebrae had a mean deformity correction of 64%, and 16 patients with multilevel disease had an average correction of 81%. These corrections were maintained at a minimum of two years follow-up. Zhao et al. treated 40 patients with spinal tuberculosis with anterior debridement and iliac crest bone graft with one-stage anterior or posterior instrumentation [23]. At a mean follow-up of 22 months, 92% of patients with a neurological deficit had good to excellent results with a mean 16 degree correction of kyphosis and a 90% fusion rate. Similarly, Benli et al. reviewed 63 patients with spinal tuberculosis who underwent anterior debridement with anterior fusion and anterior instrumentation. At an average follow-up of 51 months, good correction of kyphosis was achieved and 80% of those with neurological dysfunction had full recovery [15]. Bone grafting with structural allograft had been shown to be safe when a radical debridement had been done. It was also effective with a greater than 95% fusion rate [20].
Case series in the literature examining anterior decompression followed by posterior decompression and fusion have also shown excellent results in terms of fusion rate and neurological recovery [17, 21, 22]. Huang et al. reported on 15 patients with spinal tuberculosis treated by anterior decompression, bone grafting, posterior instrumentation, and fusion [17]. At 30 months follow-up, patients demonstrated an improvement in kyphosis of 13 degrees and neurological improvement by one Frankel grade [40]. Similarly, Zhang et al. reported on 23 patients who underwent anterior debridement, strut autografting, and posterior instrumented fusion for multilevel tuberculous spondylitis [22]. Antituberculosis chemotherapy was continued for 18 months. They achieved a 24-degree correction in kyphotic deformity, and 19 patients with a neurologic deficit improved approximately one Frankel grade. Fusion rate was 100%.
Transpedicular approach
Transpedicular decompression is an appealing approach as it allows for access to both the anterior and posterior aspects of the spine through a single incision [41]. Chacko et al. reviewed 11 patients with tuberculous spondylitis treated via a transpedicular approach. None of the patients developed worsening of their neurological status or degree of kyphosis. Over 90% returned to functional activity [16]. Lee et al. reported on seven patients who underwent this approach; all obtained fusion with improvements in kyphosis and Frankel grade. However they suggest that this technique may not be as effective for larger degrees of vertebral column destruction as those cases may require a formal anterior debridement with bone graft reconstruction [18].
Posterior-only approach
In certain cases, a posterior-alone approach without decompression has been advocated as an alternative to anterior debridement. Guven et al. reported on ten cases of tuberculous spondylitis treated with single stage posterior instrumentation and fusion without anterior debridement. Anti-tuberculous chemotherapy was continued for 11 months. At two years follow-up, good correction was observed with a 98% fusion rate and only 3.4-degree average loss of correction at final follow-up. However, this approach alone cannot be used in cases of neurological deficit, anterior abscess formation or multilevel involvement where an anterior debridement is mandatory [13].
Osteotomies and vertebral column resection
In many cases, the kyphotic segment is too rigid to correct without performing osteotomies to increase spinal column flexibility [24, 25, 27–30, 32, 35, 37, 42, 43]. Transpedicular decancellation osteotomy (pedicle subtraction osteotomy) can allow a 20–30 degree correction of kyphotic deformity at a single level [26, 27, 42–44]. However, these procedures have a high complication rate including neurological injury and bleeding [45]. Bezer et al. reported on a five-year follow-up study of 16 patients with tuberculous kyphosis who underwent pedicle subtraction osteotomy. Mean preoperative kyphosis of 30 degrees was corrected to 12 degrees. Forward sagittal balance was reduced from 68 mm to 12 mm. All patients achieved fusion and none had neurological complications [24]. Similarly, others have observed excellent deformity correction (kyphosis reduction to under 50% of the preoperative magnitude) and high fusion rates with pedicle subtraction osteotomy [29, 30].
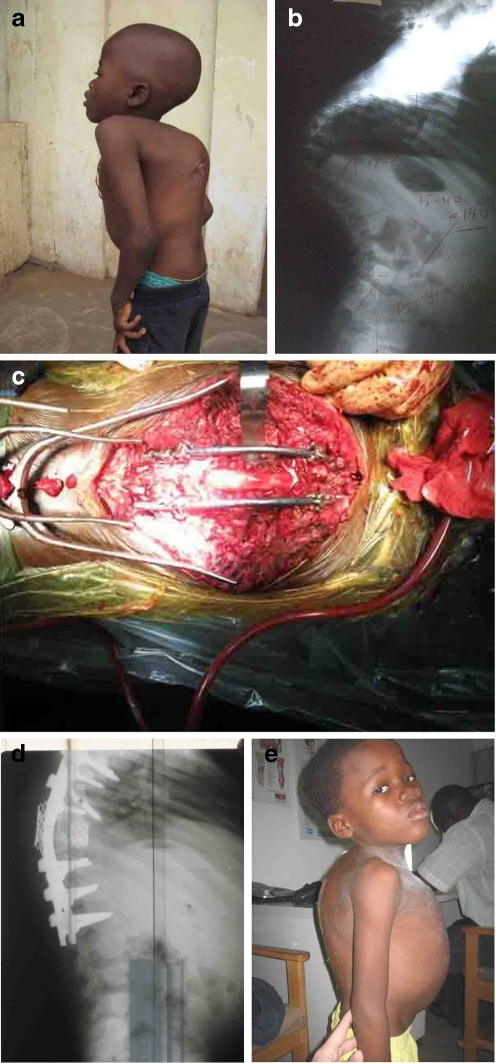
Severe rigid deformities (with flexibility less than 25% and magnitudes exceeding 80 degrees) may require more extensive resection techniques to effect correction of kyphosis and sagittal balance [44, 46–48]. Vertebral column resection is very effective in accomplishing translation of the spinal column in rigid deformities [46] (Fig. 1). Figure 1 shows an eight-year-old boy with spinal tuberculosis treated medically. He developed a progressive severe kyphosis and bilateral leg weakness. Clinically, he demonstrated skin breakdown over the gibbus deformity. Radiographically, there was evidence of sharp (140 degree) angular deformity of the thoracolumbar spine with spinal cord compression. Posterior decompression and vertebral column resection were performed allowing for good deformity correction. This procedure may be done from an anterior-posterior or single posterior approach [26, 31, 33, 34]. It is a technically demanding surgery with high risk for neurological injury, especially when performed in the thoracic spine in patients with preoperative spinal cord compromise [26, 33, 34]. Care must be taken to avoid spinal shortening greater than one-third of the vertebral segment to avoid deformity to the dural sac and spinal cord buckling and ischemia [49].
Fig. 1.
Eight-year-old boy with spinal tuberculosis treated medically. He developed a progressive severe kyphosis and bilateral leg weakness. a Clinical appearance preoperatively demonstrating skin breakdown over the gibbus deformity. b Lateral radiograph shows sharp (140 degree) angular deformity of the thoracolumbar spine with spinal cord compression. c Appearance after decompression and vertebral column resection. d Lateral radiograph shows anterior cage support with bone graft and posterior instrumented fusion. e Clinical appearance postoperatively
Wang et al. treated nine patients with tuberculous kyphosis with a lateral kyphotic angle of greater than 90 degrees combining transpedicular eggshell osteotomies and multilevel vertebral column resection through a single posterior approach [36, 50]. Mean preoperative kyphosis of 100 degrees was corrected to 16 degrees. All patients achieved fusion [36]. Deng et al. reported on 34 patients with tuberculous kyphosis treated by vertebral resection. Good to excellent outcomes were obtained in 32 patients. Kyphosis improved from 58 degrees preoperatively to 11 degrees postoperatively. Of 19 patients with preoperative neurological deficits, 17 demonstrated improvement by more than 1 ASIA grade. Ten patients had questionable pseudoarthroses [28].
Treatment algorithm
Surgical management of tuberculous spondylitic kyphosis is indicated if there is a lack of response to antibiotics, severe and/or progressive kyphosis, or a developing neurological deficit. Debridement is generally performed anteriorly as the pathology is typically located in the vertebral bodies. Anterior debridement is essential in cases of neurological impairment, multilevel involvement or severe abscess formation. Debridement may be followed by anterior reconstruction with bone graft and either anterior or posterior instrumentation. For larger degrees of kyphotic deformity (greater than 80 degrees of kyphosis) and stiffer curves (less than 25% flexibility), posterior osteotomies may be helpful in increasing curve flexibility. Multilevel Ponte osteotomies can achieve five to ten degrees of correction per level while pedicle subtraction osteotomies or vertebral column resection can create greater than 30–40 degrees of correction. Neuromonitoring is essential for these cases as is the ready availability of blood transfusion.
Conclusion
A severe kyphotic deformity developing from spinal tuberculosis often requires surgical treatment to eradicate infection, restore alignment and reduce pain. Anterior debridement has traditionally been the procedure of choice to debride infected bone and soft tissue and decompress neural elements. Stability can be achieved by either anterior or posterior instrumented fusion with little increased risk of infection. When tubercular lesions result in progression of kyphosis to more than 50 degrees, the deformity should be surgically corrected to restore sagittal balance. The choice of operation depends on the magnitude of correction required with posterior multilevel Ponte osteotomies and fusion or anterior releases followed by anterior or posterior spinal fusion performed in the majority of cases. Pedicle subtraction osteotomies or vertebral column resection are indicated for more severe, rigid deformities which correct to less than 25%. While these are extremely powerful correction techniques, they carry significant risk of neurological injury and blood loss and should therefore be performed by surgeons proficient in these techniques at specialised centers.
References
- 1.Boachie-Adjei O, Squillante RG. Tuberculosis of the spine. Orthop Clin North Am. 1996;27(1):95–103. [PubMed] [Google Scholar]
- 2.Jain AK. Tuberculosis of the spine: a fresh look at an old disease. J Bone Joint Surg Br. 2010;92(7):905–913. doi: 10.1302/0301-620X.92B7.24668. [DOI] [PubMed] [Google Scholar]
- 3.Jain AK, Dhammi IK. Tuberculosis of the spine: a review. Clin Orthop Relat Res. 2007;460:39–49. doi: 10.1097/BLO.0b013e318073bd29. [DOI] [PubMed] [Google Scholar]
- 4.Jain AK, Dhammi IK, Jain S, et al. Kyphosis in spinal tuberculosis—Prevention and correction. Indian J Orthop. 2010;44(2):127–136. doi: 10.4103/0019-5413.61893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rajasekaran S. The natural history of post-tubercular kyphosis in children. Radiological signs which predict late increase in deformity. J Bone Joint Surg Br. 2001;83(7):954–962. doi: 10.1302/0301-620X.83B7.12170. [DOI] [PubMed] [Google Scholar]
- 6.Rajasekaran S. Buckling collapse of the spine in childhood spinal tuberculosis. Clin Orthop Relat Res. 2007;460:86–92. doi: 10.1097/BLO.0b013e31806a9172. [DOI] [PubMed] [Google Scholar]
- 7.Rajasekaran S, Soundarapandian S. Progression of kyphosis in tuberculosis of the spine treated by anterior arthrodesis. J Bone Joint Surg Am. 1989;71(9):1314–1323. [PubMed] [Google Scholar]
- 8.Jain AK. Treatment of tuberculosis of the spine with neurologic complications. Clin Orthop Relat Res. 2002;398:75–84. doi: 10.1097/00003086-200205000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Moon MS, Moon YW, Moon JL, et al. Conservative treatment of tuberculosis of the lumbar and lumbosacral spine. Clin Orthop Relat Res. 2002;398:40–49. doi: 10.1097/00003086-200205000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Rajasekaran S. The problem of deformity in spinal tuberculosis. Clin Orthop Relat Res. 2002;398:85–92. doi: 10.1097/00003086-200205000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Oga M, Arizono T, Takasita M, et al. Evaluation of the risk of instrumentation as a foreign body in spinal tuberculosis. Clinical and biologic study. Spine (Phila Pa 1976) 1993;18(13):1890–1894. doi: 10.1097/00007632-199310000-00028. [DOI] [PubMed] [Google Scholar]
- 12.Yilmaz C, Selek HY, Gurkan I, et al. Anterior instrumentation for the treatment of spinal tuberculosis. J Bone Joint Surg Am. 1999;81(9):1261–1267. doi: 10.2106/00004623-199909000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Guven O, Kumano K, Yalcin S, et al. A single stage posterior approach and rigid fixation for preventing kyphosis in the treatment of spinal tuberculosis. Spine (Phila Pa 1976) 1994;19(9):1039–1043. doi: 10.1097/00007632-199405000-00007. [DOI] [PubMed] [Google Scholar]
- 14.author listed No. A 15-year assessment of controlled trials of the management of tuberculosis of the spine in Korea and Hong Kong. Thirteenth Report of the Medical Research Council Working Party on Tuberculosis of the Spine. J Bone Joint Surg Br. 1998;80(3):456–462. doi: 10.1302/0301-620X.80B3.8544. [DOI] [PubMed] [Google Scholar]
- 15.Benli IT, Acaroglu E, Akalin S, et al. Anterior radical debridement and anterior instrumentation in tuberculosis spondylitis. Eur Spine J. 2003;12(2):224–234. doi: 10.1007/s00586-002-0403-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chacko AG, Moorthy RK, Chandy MJ. The transpedicular approach in the management of thoracic spine tuberculosis: a short-term follow up study. Spine (Phila Pa 1976. 2004;29(17):E363–E367. doi: 10.1097/01.brs.0000137063.64650.e1. [DOI] [PubMed] [Google Scholar]
- 17.Huang QS, Zheng C, Hu Y, et al. One-stage surgical management for children with spinal tuberculosis by anterior decompression and posterior instrumentation. Int Orthop. 2009;33(5):1385–1390. doi: 10.1007/s00264-009-0758-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee SH, Sung JK, Park YM. Single-stage transpedicular decompression and posterior instrumentation in treatment of thoracic and thoracolumbar spinal tuberculosis: a retrospective case series. J Spinal Disord Tech. 2006;19(8):595–602. doi: 10.1097/01.bsd.0000211241.06588.7b. [DOI] [PubMed] [Google Scholar]
- 19.Louw JA. Spinal tuberculosis with neurological deficit. Treatment with anterior vascularised rib grafts, posterior osteotomies and fusion. J Bone Joint Surg Br. 1990;72(4):686–693. doi: 10.1302/0301-620X.72B4.2380228. [DOI] [PubMed] [Google Scholar]
- 20.Ozdemir HM, Us AK, Ogun T. The role of anterior spinal instrumentation and allograft fibula for the treatment of pott disease. Spine (Phila Pa 1976) 2003;28(5):474–479. doi: 10.1097/01.BRS.0000048666.17934.17. [DOI] [PubMed] [Google Scholar]
- 21.Talu U, Gogus A, Ozturk C, et al. The role of posterior instrumentation and fusion after anterior radical debridement and fusion in the surgical treatment of spinal tuberculosis: experience of 127 cases. J Spinal Disord Technol. 2006;19(8):554–559. doi: 10.1097/01.bsd.0000211202.93125.c7. [DOI] [PubMed] [Google Scholar]
- 22.Zhang HQ, Guo CF, Xiao XG, et al. One-stage surgical management for multilevel tuberculous spondylitis of the upper thoracic region by anterior decompression, strut autografting, posterior instrumentation, and fusion. J Spinal Disord Technol. 2007;20(4):263–267. doi: 10.1097/01.bsd.0000211281.68400.1b. [DOI] [PubMed] [Google Scholar]
- 23.Zhao J, Lian XF, Hou TS, et al. Anterior debridement and bone grafting of spinal tuberculosis with one-stage instrumentation anteriorly or posteriorly. Int Orthop. 2007;31(6):859–863. doi: 10.1007/s00264-006-0253-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bezer M, Kucukdurmaz F, Guven O. Transpedicular decancellation osteotomy in the treatment of posttuberculous kyphosis. J Spinal Disord Technol. 2007;20(3):209–215. doi: 10.1097/01.bsd.0000211271.89485.f1. [DOI] [PubMed] [Google Scholar]
- 25.Boachie-Adjei O. Role and technique of eggshell osteotomies and vertebral column resections in the treatment of fixed sagittal imbalance. Instr Course Lect. 2006;55:583–589. [PubMed] [Google Scholar]
- 26.Bradford DS, Tribus CB. Vertebral column resection for the treatment of rigid coronal decompensation. Spine (Phila Pa 1976) 1997;22(14):1590–1599. doi: 10.1097/00007632-199707150-00013. [DOI] [PubMed] [Google Scholar]
- 27.Bridwell KH. Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine (Phila Pa 1976) 2006;31(19 Suppl):S171–S178. doi: 10.1097/01.brs.0000231963.72810.38. [DOI] [PubMed] [Google Scholar]
- 28.Deng Y, Lv G, An HS. En bloc spondylectomy for the treatment of spinal tuberculosis with fixed and sharply angulated kyphotic deformity. Spine (Phila Pa 1976) 2009;34(20):2140–2146. doi: 10.1097/BRS.0b013e3181b34ce7. [DOI] [PubMed] [Google Scholar]
- 29.Gokce A, Ozturkmen Y, Mutlu S, et al. Spinal osteotomy: correcting sagittal balance in tuberculous spondylitis. J Spinal Disord Technol. 2008;21(7):484–488. doi: 10.1097/BSD.0b013e3181586023. [DOI] [PubMed] [Google Scholar]
- 30.Kalra KP, Dhar SB, Shetty G, et al. Pedicle subtraction osteotomy for rigid post-tuberculous kyphosis. J Bone Joint Surg Br. 2006;88(7):925–927. doi: 10.1302/0301-620X.88B7.17366. [DOI] [PubMed] [Google Scholar]
- 31.Pappou IP, Papadopoulos EC, Swanson AN, et al. Pott disease in the thoracolumbar spine with marked kyphosis and progressive paraplegia necessitating posterior vertebral column resection and anterior reconstruction with a cage. Spine (Phila Pa 1976) 2006;31(4):E123–E127. doi: 10.1097/01.brs.0000199900.56446.ee. [DOI] [PubMed] [Google Scholar]
- 32.Smith-Petersen MN, Larson CB, Aufranc OE. Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. Clin Orthop Relat Res. 1969;66:6–9. [PubMed] [Google Scholar]
- 33.Suk SI, Chung ER, Kim JH, et al. Posterior vertebral column resection for severe rigid scoliosis. Spine (Phila Pa 1976) 2005;30(14):1682–1687. doi: 10.1097/01.brs.0000170590.21071.c1. [DOI] [PubMed] [Google Scholar]
- 34.Suk SI, Kim JH, Kim WJ, et al. Posterior vertebral column resection for severe spinal deformities. Spine (Phila Pa 1976) 2002;27(21):2374–2382. doi: 10.1097/00007632-200211010-00012. [DOI] [PubMed] [Google Scholar]
- 35.Thomasen E. Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop Relat Res. 1985;194:142–152. [PubMed] [Google Scholar]
- 36.Wang Y, Zhang Y, Zhang X, et al. Posterior-only multilevel modified vertebral column resection for extremely severe Pott's kyphotic deformity. Eur Spine J. 2009;18(10):1436–1441. doi: 10.1007/s00586-009-1067-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yau AC, Hsu LC, O'Brien JP, et al. Tuberculous kyphosis: correction with spinal osteotomy, halo-pelvic distraction, and anterior and posterior fusion. J Bone Joint Surg Am. 1974;56(7):1419–1434. [PubMed] [Google Scholar]
- 38.Dai LY, Jiang LS, Wang W, et al. Single-stage anterior autogenous bone grafting and instrumentation in the surgical management of spinal tuberculosis. Spine (Phila Pa 1976) 2005;30(20):2342–2349. doi: 10.1097/01.brs.0000182109.36973.93. [DOI] [PubMed] [Google Scholar]
- 39.Jain AK, Dhammi IK, Prashad B, et al. Simultaneous anterior decompression and posterior instrumentation of the tuberculous spine using an anterolateral extrapleural approach. J Bone Joint Surg Br. 2008;90(11):1477–1481. doi: 10.1302/0301-620X.90B11.20972. [DOI] [PubMed] [Google Scholar]
- 40.Frankel HL. Ascending cord lesion in the early stages following spinal injury. Paraplegia. 1969;7(2):111–118. doi: 10.1038/sc.1969.21. [DOI] [PubMed] [Google Scholar]
- 41.Klimo P, Jr, Dailey AT, Fessler RG. Posterior surgical approaches and outcomes in metastatic spine-disease. Neurosurg Clin N Am. 2004;15(4):425–435. doi: 10.1016/j.nec.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 42.Bridwell KH, Lewis SJ, Lenke LG, et al. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. J Bone Joint Surg Am. 2003;85-A(3):454–463. doi: 10.2106/00004623-200303000-00009. [DOI] [PubMed] [Google Scholar]
- 43.Bridwell KH, Lewis SJ, Rinella A, et al. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. Surgical technique. J Bone Joint Surg Am. 2004;86-A(Suppl 1):44–50. doi: 10.2106/00004623-200403001-00007. [DOI] [PubMed] [Google Scholar]
- 44.Gill JB, Levin A, Burd T, et al. Corrective osteotomies in spine surgery. J Bone Joint Surg Am. 2008;90(11):2509–2520. doi: 10.2106/JBJS.H.00081. [DOI] [PubMed] [Google Scholar]
- 45.Smith JS, Sansur CA, Donaldson WF, 3rd, et al (2011) Short-term morbidity and mortality associated with correction of thoracolumbar fixed sagittal plane deformity: A report from the Scoliosis Research Society Morbidity and Mortality Committee. Spine (Phila Pa 1976) 36(12):958–964 [DOI] [PubMed]
- 46.Smith JS, Wang VY, Ames CP. Vertebral column resection for rigid spinal deformity. Neurosurgery. 2008;63(3 Suppl):177–182. doi: 10.1227/01.NEU.0000320429.32113.85. [DOI] [PubMed] [Google Scholar]
- 47.Joseph SA, Jr, Moreno AP, Brandoff J, et al. Sagittal plane deformity in the adult patient. J Am Acad Orthop Surg. 2009;17(6):378–388. doi: 10.5435/00124635-200906000-00006. [DOI] [PubMed] [Google Scholar]
- 48.Kim HJ, Cunningham ME, Boachie-Adjei O. Revision spine surgery to manage pediatric deformity. J Am Acad Orthop Surg. 2010;18(12):739–748. doi: 10.5435/00124635-201012000-00004. [DOI] [PubMed] [Google Scholar]
- 49.Kawahara N, Tomita K, Kobayashi T, et al. Influence of acute shortening on the spinal cord: an experimental study. Spine (Phila Pa 1976) 2005;30(6):613–620. doi: 10.1097/01.brs.0000155407.87439.a2. [DOI] [PubMed] [Google Scholar]
- 50.Wang Y, Zhang Y, Zhang X, et al. A single posterior approach for multilevel modified vertebral column resection in adults with severe rigid congenital kyphoscoliosis: a retrospective study of 13 cases. Eur Spine J. 2008;17(3):361–372. doi: 10.1007/s00586-007-0566-9. [DOI] [PMC free article] [PubMed] [Google Scholar]