Abstract
Objective
To investigate adverse pregnancy outcomes in non-obese women with polycystic ovary syndrome (PCOS) compared with obese-PCOS and control groups.
Methods
Women with PCOS who underwent assisted reproductive technology (ART) from August, 2003 to December, 2007, were considered. A total of 336 women with PCOS were included in the study group and 1,003 infertile women who had tubal factor as an indication for ART were collected as controls. They were divided into four groups: a non-obese PCOS group, obese-PCOS group, non-obese tubal factor group, and obese tubal factor group, with obesity defined by a body mass index over 25 kg/m2, and reviewed focusing on the basal characteristics, ART outcomes, and adverse pregnancy outcomes.
Results
There was no difference among the groups' the clinical pregnancy rate or live birth rate. Regarding adverse pregnancy outcomes, the miscarriage rate, multiple pregnancy rate, and prevalence of preterm delivery and pregnancy induced hypertension were not different among the four groups. The incidence of small for gestational age infant was higher in the PCOS groups than the tubal factor groups (p<0.02). On the other hand, the morbidity of gestational diabetes mellitus (GDM) was not high in the non-obese PCOS group but was in the obese groups. And in the obese PCOS group, the newborns were heavier than in the other groups (p<0.02).
Conclusion
Non-obese PCOS presents many differences compared with obese PCOS, not only in the IVF-parameters but also in the morbidity of adverse pregnancy outcomes, especially in GDM and fetal macrosomia.
Keywords: Pregnancy Outcome; Polycystic Ovary Syndrome; Non-obese; Reproductive Techniques, Assisted; Diabetes, Gestational; Fetal Macrosomia; Human
Introduction
Polycystic ovary syndrome (PCOS) is the most common endocrine disorder in reproductive aged women [1], diagnosed by any two of the following three: menstrual irregularity with oligo-anovulation, clinical or biochemical hyperandrogenism, and polycystic ovarian features on ultrasonogram (Rotterdam criteria, 2003). It is characterized clinically by menstrual irregularity, hirsutism, biochemically hyperandrogenism, high serum LH, and insulin resistance, and obesity [2]. Those women suffer from not only menstrual irregularity and infertility but also several obstetric complications and long term metabolic disturbance [3]. Furthermore, some investigators have proposed that the offspring of a PCOS mother might be at an increased risk of several adult disorders in later life [4].
In terms of adverse pregnancy outcomes, gestational diabetes (GDM), fetal macrosomia, small for gestational age (SGA) infant, preterm labor, and preeclampsia are considered to be complications of PCOS pregnancy [5]. However, not only PCOS, but also obesity, which is frequently accompanied by PCOS, is an independent risk factor of these obstetric complications [6].
Many investigators have given attention to obese women with PCOS and the relation of PCOS and obesity. Some researchers reported more severe insulin resistance, worse ovulatory dysfunction, and higher serum testosterone levels in obese PCOS women [7]. In addition, a higher incidence of GDM was described in obese PCOS women than non-obese ones [8]. However, it is debatable whether these complications are as severe in non-obese PCOS women as in obese PCOS women. Therefore, we aimed to investigate the prevalence of adverse pregnancy outcomes in non-obese women with PCOS by comparison with control groups.
Methods
1. Patients
From August 1, 2003 to December 31, 2007, PCOS women who had their infertility treated with controlled ovarian hyperstimulation (COH) with IVF or superovulation were included for the study group. PCOS was defined by the 2003 Rotterdam criteria, and a total of 336 assisted reproductive technology (ART) cycles were also included, retrospectively. As a control group, women who had taken ART during same period due to tubal factor infertility that presented at least unilateral tubal obstruction, were collected. But women who had both PCOS and tubal factor were excluded.
These two groups were divided into 4 groups by body mass index (body mass index [BMI] over 25 kg/m2 or not), i.e., obese PCOS (A), non-obese PCOS (B), obese tubal factor (C), and non-obese tubal factor (D) groups.
2. ART protocols
The ovarian stimulation was done with gonadotropins in the usual way as extensively described. Briefly, the basal serum hormonal level was measured at menstrual day 2 or 3, and the absence of growing follicles (over 10 mm in size) or pelvic organic abnormalities was checked by trans-vaginal ultrasonogram (TVS). Gonadotropins were applied with the monitoring of the serum estradiol level and growing follicles by TVS. When two or more follicles reached 18 mm diameter, 5,000 units of hCG (IVF-C®; LG life Science, Seoul, Korea) was administered. IUI was done about 34-36 hours after hCG injection. Luteal support was done with vaginal progesterone tablets (Utrogestan® 100 mg tid/day; Laboratories Besins International, Paris, France) for 14 days.
In COH-IVF cycles, the patients underwent pituitary down-regulation with a low-dose GnRH agonist (Lucrin® 1 mg/day; Abbott Lab., Chicago, IL, USA or Decapeptyl® 0.1 mg/day; Ferring Parmarceuticals, Saint-Prex, Switzland) from the mid-luteal period of the previous cycle or daily GnRH antagonist (Orgalutran® 0.25 mg/day; Schering-Plough, Whitehouse Station, NJ, USA or Cetrotide® 0.25 mg/day; Merk KgaA, Darmstadt, Germany) applied when the dominant follicle reached 12 to 13 mm. When two or more follicles reached 18 mm in diameter, 10,000 units of hCG (Ovidrel®; Industria Farmaceutica Serono SpA, Roma, Italy) was administered. Trans-vaginal ultrasound guided ovum pick-up (OPU) was performed 34-36 hours later and then the maturity and quality of the retrieved oocytes was evaluated. According to the motility and the number of sperm and oocytes, insemination (conventional IVF) or microinjection (ICSI) was carried out 4-6 hours after OPU. After several days of in vitro culture, 4 or fewer selected embryos were transferred (ET) for each cycle. For luteal support, daily intramuscular injection of progesterone (Progesterone®; Watson Pharmaceuticals Inc., Corona, CA, USA) was started on the OPU day to first test serum β-hCG in non-pregnant cycles or in the 7th to 8th gestational weeks in pregnant cycles.
3. Measurement of outcomes
All parameters and pregnancy outcomes were collected from the medical records, retrospectively.
The clinical pregnancy rate and live birth rate were measured and the IVF parameters and implantation rate were collected. Adverse pregnancy outcomes such as multiple pregnancy, miscarriage, preterm delivery, GDM, pregnancy induced hypertension (PIH), fetal macrosomia, and SGA were reported and the incidence of each complication was measured.
The implantation rate was calculated by the number of gestational sacs per transferred embryo and a clinical pregnancy was defined as the presence of a G-sac on the trans-vaginal ultrasound at gestational weeks 5 to 7.
GDM screening with a 50 g oral glucose tolerance test (OGTT) was performed at 24 weeks of gestation. When a glucose value reached to 130-140 mg/dL, a further confirmatory test, i.e., 3 hours 100 g OGTT, was recommended, and GDM was diagnosed according to the protocol of the American Diabetic Association [9]. PIH was described as hypertension with a systolic blood pressure over 140 mm Hg or diastolic blood pressure over 90 mm Hg, with or without proteinuria, developing after 20 weeks of gestation. The birth weight of a newborn over 4,000 g or >90 % of mean weight of gestational age (GA) was defined as fetal macrosomia and <10% of GA was diagnosed as SGA. Preterm birth referred to a birth occurring before 37 complete weeks of gestation.
4. Analysis
Statistical analysis was performed using SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA). Each variable is presented as mean (±SD). ANOVA with the Bonferroni post-hoc test was used wherever appropriate. A p-value of <0.05 was considered statistically significant.
Results
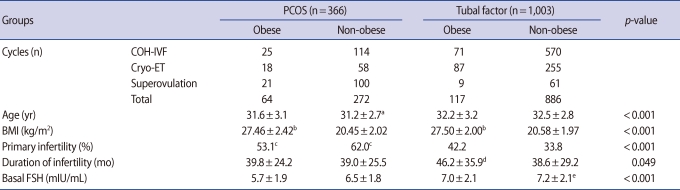
The PCOS women were collected for a total of 336 cycles of ART, including 64 cycles of the obese group (A) and 272 cycles of the non-obese group (B). The control group included 1,003 cycles with 117 for group C and 886 for group D. The mean BMI of each group was about 27.5 kg/m2 (obese groups; groups A and C) and 20.5 kg/m2 (non-obese groups; groups B and D). The non-obese PCOS group (B) was one year younger (mean age was 31.2±2.7 years) than the tubal factor groups (C and D), but there was no difference in age between the two PCOS groups (A and B). The PCOS groups (A and B) had a higher proportion of primary infertility (62.0% vs. 41.2%, p<0.001) than the tubal factor groups. The duration of infertility was near 40 months or less, except for group C (46.2±35.9 months) and the basal serum FSH levels of each group were similar, near 7.0 mIU/mL or less, except group D (7.2±2.1 mIU/mL) (Table 1).
Table 1.
Patient characteristics of each group
Values presented as mean±SD.
PCOS, polycystic ovary syndrome; COH-IVF, controlled ovarian hyperstimulation with in vitro fertilization; ET, embryo transfer; BMI, body mass index.
anon-obese PCOS vs. tubal factor; bobese vs. non-obese; cPCOS vs. tubal factor; dobese vs. non-obese tubal factor; enon-obese tubal factor vs. PCOS.
In the IVF cycles, the number of retrieved oocytes was higher in the non-obese PCOS group than the control groups (groups C and D), but the fertilization rate and number of good embryos were lower than those of the tubal groups (No. of retrieved oocytes was 19.2±9.4 vs. 12.9±8.3, p<0.001, fertilization rate was 59.1±18.0 vs. 67.4±19.7, p<0.001, and number of good embryos was 2.08±1.30 vs. 2.39±1.20, p=0.016). The PCOS groups showed a better implantation rate than the tubal factor groups, especially in the comparison of groups B and D (22.2% vs. 13.1%, p<0.001) (Table 2).
Table 2.
IVF parameters of each group
Values presented as mean±SD.
PCOS, polycystic ovary syndrome; COH-IVF, controlled ovarian hyperstimulation with in vitro fertilization; NS, not significant.
a,b,c,dnon-obese PCOS vs. tubal factor.
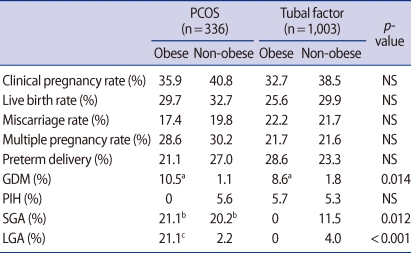
There was no difference among the groups in the clinical pregnancy rate or live birth rate. As for the adverse pregnancy outcomes, the multiple pregnancy rate, miscarriage rate, and prevalence of preterm delivery did not differ among the 4 groups. The morbidity of GDM was definitely higher (10.53% and 8.57% vs. 1.12% and 1.76%, p=0.014) in the obese groups (groups A and C) than the non-obese groups (groups B and D) and the morbidity of mothers with SGA was higher in the PCOS groups (21.1% and 20.2% vs. 11.5%, p=0.012) than the tubal factor groups. In the obese PCOS group, newborns were heavier than in the other groups (While the rate of fetal macrosomia was 21.05% in group A, it was under 5% in the other groups, p<0.001). On the other hand, the incidences of PIH of each group were not different (Table 3).
Table 3.
Pregnancy outcomes and complications
PCOS, polycystic ovary syndrome; NS, not significant; GDM, gestational diabetes mellitus; PIH, pregnancy induced hypertension; SGA, small for gestational age; LGA, large for gestational age.
aObese vs. non-obese; bPCOS vs. tubal factor; cObese PCOS vs. non-obese PCOS and tubal factor.
Discussion
Several studies have reported on the pregnancy complications of PCOS women, but most were performed in western countries. This study differs from previous reports in several key ways. First, it was performed in Asia, specifically South Korea. Asian women are slightly different from western women in the feature of PCOS, obesity, and their complications. The other distinction of this study is the sub-grouping of PCOS women by BMI to investigate the influence of obesity on adverse pregnancy outcomes, which are considered complications of PCOS.
The WHO defined obesity as BMI over 30 kg/m2 [10]. This was based on coincidence of obesity and several adult diseases such as Type 2 diabetes and cerebro-vascular accidents [11]. However, the prevalence of obesity in Asian populations is lower and the health risks associated with obesity occur at a lower BMI than that of western people [12,13]. Thus the definition of obesity in this study is a BMI over 25 kg/m2 following the new criteria of "WHO - The Asia-Pacific Perspective" [13]. The Republic of Korea's National Nutrition Survey of 2008 [14], announced about 25% of reproductive aged women were classified as obese (BMI>25 kg/m2) by the new criteria of obesity for Asians.
In the PCOS group, the younger age and lower FSH levels may result from earlier visits to the infertility clinic due to menstrual irregularity compared with the other infertile groups.
In the non-obese PCOS groups, more oocytes were retrieved, but the fertility rate and good embryo rate was significantly lower than for the tubal factor groups. As a result, we could agree with Qiao and Feng [15]'s opinion that PCOS is associated with poor quality oocytes. However, this tendency was not significant in the obese PCOS group. Unfortunately, we could not explain why this phenomenon occurred. Despite the poor quality of oocytes, the implantation rate was higher in the PCOS group than the tubal factor group. This could be because of the unfavorable environment to implantation in tubal factor groups such as the presence of inflammatory cytokines from hydrosalpinx.
Regarding adverse pregnancy outcomes, the abortion rate of the PCOS groups was not higher than the other infertile women (tubal factor groups), contrary to the findings of a previous paper, which reported that PCOS women showed more frequent early pregnancy loss (about 40%) than the general population [16]. Some investigators have suggested that this is caused by elevated LH in PCOS [17], while another said that it is due to ovulation inducing agents such as clomiphene citrate, which has an anti-estrogenic effect on the endometrium [18], and another asserted that it is caused by obesity accompanying PCOS [19]. However, all the patients of this study underwent various forms of ART including ovulation induction or superovulation, but the miscarriage rate was not elevated in the PCOS groups and it was the same regardless of BMI.
Normal pregnancy itself induces an insulin resistant state and insulin resistance is thought to be the etiology of PCOS. Therefore, many studies have suggested that women with PCOS are likely to develop GDM and macrosomia, which is a complication of maternal hyperglycemia [6]. However, the prevalence of GDM and LGA was not higher in either PCOS group. GDM frequently developed in the obese subgroups of each group, i.e., group A and C, and the incidence of LGA was higher in only the obese PCOS group. Hence, we assumed that the results of previous published studies presenting the higher incidence of GDM and LGA of PCOS women was mainly caused by obesity, which was likely to occur with PCOS. Thus we suggest that non-obese PCOS is not the risk factor for GDM or LGA.
PCOS can be expected to be a risk factor of PIH, due to its metabolic and vascular status. A meta-analysis of eight studies found that women with PCOS showed a significantly higher incidence of PIH [5], but other larger studies reported that not PCOS itself, but nulliparity that may be caused by anovulatory infertility in PCOS women is a significant risk factor for PIH [20]. In this study, even though the PCOS group consisted of a higher number of primary infertile women, i.e., nulliparity, there was no difference in the incidence of PIH among the groups.
SGA can also be expected to develop often in women with PCOS. The vascular status of PCOS, which possibly causes placental insufficiency and prenatal exposure to sex steroids [21], may bring out fetal growth retardation. However, the published studies presented conflicting results about the relationship between birth weight and PCOS [22]. This disparity may stem from the higher rate of LGA in pregnancy of those with PCOS. In this study, we found a higher incidence of SGA in the PCOS group regardless of obesity.
Preterm birth can be higher in women with PCOS, due to the higher rate of multiple pregnancies from ovulation induction. However, in this study we could not find any differences in the prevalence of preterm birth and multiple pregnancies among the 4 groups.
Regarding the long-term health problems of offspring, some investigators have suggested that the infants of PCOS mothers may be at an increased risk of several adult disorders, such as cardiovascular disease, type 2 diabetes, obesity, and hypertension [4]. Unfortunately, we could not follow up on the infants in this study, so a long-term follow up of the babies of mothers with PCOS should be performed in the future.
PCOS has various properties and presents in heterogeneous subgroups. Several adverse pregnancy outcomes that have been considered to be complications of PCOS are caused by not only PCOS itself, but in combination with other problems such as obesity. Though SGA developed in the PCOS group regardless of obesity, GDM and LGA did not develop as frequently in the non-obese PCOS group as in the obese PCOS group. Therefore, we suggest that the differentiated care of pregnant women with PCOS is needed according to the existence of obesity. For a more definite conclusion about the pregnancy complications of non-obese PCOS women, a large scale long-term follow up study is warranted.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Franks S. Polycystic ovary syndrome. N Engl J Med. 1995;333:853–861. doi: 10.1056/NEJM199509283331307. [DOI] [PubMed] [Google Scholar]
- 2.Rotterdam ESHRE/ASRM-Sponsored PCOS consensus workshop group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS) Hum Reprod. 2004;19:41–47. doi: 10.1093/humrep/deh098. [DOI] [PubMed] [Google Scholar]
- 3.Dunaif A. Insulin action in the polycystic ovary syndrome. Endocrinol Metab Clin North Am. 1999;28:341–359. doi: 10.1016/s0889-8529(05)70073-6. [DOI] [PubMed] [Google Scholar]
- 4.Barker DJ. Maternal and fetal origins of coronary heart disease. J R Coll Physicians Lond. 1994;28:544–551. [PMC free article] [PubMed] [Google Scholar]
- 5.Boomsma CM, Eijkemans MJ, Hughes EG, Visser GH, Fauser BC, Macklon NS. A meta-analysis of pregnancy outcomes in women with polycystic ovary syndrome. Hum Reprod Update. 2006;12:673–683. doi: 10.1093/humupd/dml036. [DOI] [PubMed] [Google Scholar]
- 6.Boomsma CM, Fauser BC, Macklon NS. Pregnancy complications in women with polycystic ovary syndrome. Semin Reprod Med. 2008;26:72–84. doi: 10.1055/s-2007-992927. [DOI] [PubMed] [Google Scholar]
- 7.Laven JS, Imani B, Eijkemans MJ, Fauser BC. New approach to polycystic ovary syndrome and other forms of anovulatory infertility. Obstet Gynecol Surv. 2002;57:755–767. doi: 10.1097/00006254-200211000-00022. [DOI] [PubMed] [Google Scholar]
- 8.Urman B, Sarac E, Dogan L, Gurgan T. Pregnancy in infertile PCOD patients: complications and outcome. J Reprod Med. 1997;42:501–505. [PubMed] [Google Scholar]
- 9.Metzger BE, Coustan DR. Summary and recommendations of the Fourth International Workshop-Conference on Gestational Diabetes Mellitus. The Organizing Committee. Diabetes Care. 1998;21(Suppl 2):B161–B167. [PubMed] [Google Scholar]
- 10.World Health Organization. Report of a WHO consultation. Geneva (CH): WHO; 1998. Obesity: preventing and managing the global epidemic. [Google Scholar]
- 11.Hubert HB, Feinleib M, McNamara PM, Castelli WP. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation. 1983;67:968–977. doi: 10.1161/01.cir.67.5.968. [DOI] [PubMed] [Google Scholar]
- 12.Deurenberg-Yap M, Yian TB, Kai CS, Deurenberg P, van Staveren WA. Manifestation of cardiovascular risk factors at low levels of body mass index and waist-to-hip ratio in Singaporean Chinese. Asia Pac J Clin Nutr. 1999;8:177–183. doi: 10.1046/j.1440-6047.1999.00091.x. [DOI] [PubMed] [Google Scholar]
- 13.The World Health Organization Western Pacific Region; The international Association for the Study of Obesity, and The international Force. The Asia-Pacific perspective: redefining obesity and its treatment. Sydney: Health Communications Australia Pty Limited; 2000. [Google Scholar]
- 14.Korea Centers for Disease Control and Prevention. Seoul: Korea Centers for Disease Control and Prevention; 2010. [cited 2011 May 10]. The Republic of Korea's national nutritional survey of 2008 [Internet] Available from: http://knhanes.cdc.go.kr. [Google Scholar]
- 15.Qiao J, Feng HL. Extra- and intra-ovarian factors in polycystic ovary syndrome: impact on oocyte maturation and embryo developmental competence. Hum Reprod Update. 2011;17:17–33. doi: 10.1093/humupd/dmq032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jakubowicz DJ, Iuorno MJ, Jakubowicz S, Roberts KA, Nestler JE. Effects of metformin on early pregnancy loss in the polycystic ovary syndrome. J Clin Endocrinol Metab. 2002;87:524–529. doi: 10.1210/jcem.87.2.8207. [DOI] [PubMed] [Google Scholar]
- 17.Homburg R, Armar NA, Eshel A, Adams J, Jacobs HS. Influence of serum luteinising hormone concentrations on ovulation, conception, and early pregnancy loss in polycystic ovary syndrome. BMJ. 1988;297:1024–1026. doi: 10.1136/bmj.297.6655.1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dickey RP, Taylor SN, Curole DN, Rye PH, Pyrzak R. Incidence of spontaneous abortion in clomiphene pregnancies. Hum Reprod. 1996;11:2623–2628. doi: 10.1093/oxfordjournals.humrep.a019182. [DOI] [PubMed] [Google Scholar]
- 19.Wang JX, Davies MJ, Norman RJ. Polycystic ovarian syndrome and the risk of spontaneous abortion following assisted reproductive technology treatment. Hum Reprod. 2001;16:2606–2609. doi: 10.1093/humrep/16.12.2606. [DOI] [PubMed] [Google Scholar]
- 20.Mikola M, Hiilesmaa V, Halttunen M, Suhonen L, Tiitinen A. Obstetric outcome in women with polycystic ovarian syndrome. Hum Reprod. 2001;16:226–229. doi: 10.1093/humrep/16.2.226. [DOI] [PubMed] [Google Scholar]
- 21.Manikkam M, Crespi EJ, Doop DD, Herkimer C, Lee JS, Yu S, et al. Fetal programming: prenatal testosterone excess leads to fetal growth retardation and postnatal catch-up growth in sheep. Endocrinology. 2004;145:790–798. doi: 10.1210/en.2003-0478. [DOI] [PubMed] [Google Scholar]
- 22.Sir-Petermann T, Hitchsfeld C, Maliqueo M, Codner E, Echiburú B, Gazitúa R, et al. Birth weight in offspring of mothers with polycystic ovarian syndrome. Hum Reprod. 2005;20:2122–2126. doi: 10.1093/humrep/dei009. [DOI] [PubMed] [Google Scholar]