Abstract
Objective:
The at-risk mental state (ARMS) is associated with a very high risk of psychosis, but it is difficult to predict which individuals will later develop psychosis on the basis of their presenting symptoms. We investigated psychopathological dimensions in subjects with an ARMS and examined whether particular symptom dimensions predicted subsequent transition to psychosis.
Method:
The sample comprised 122 subjects (aged 16–35 years) meeting Personal Assessment and Crisis Evaluation clinic criteria for the ARMS recruited through Outreach and Support in South London, a clinical service for people with an ARMS. A principal axis factor analysis was performed on symptom scores, obtained at presentation from the Comprehensive Assessment of the At-Risk Mental State, using Varimax rotation. The relationship between dimension scores and transition to psychosis during the following 24 months was then examined employing Cox regression analysis.
Results:
Factor analysis gave rise to a 5-factor solution of negative, anxiety, disorganization/cognitive, self-harm, and manic symptom dimensions, accounting for 37% of the total variance. Scores on the negative and on the disorganization/cognitive dimensions were associated with transition to psychosis during the follow-up period (P = 0.044 and P = 0.005, respectively).
Conclusion:
The symptoms of the ARMS have a dimensional structure similar to that evident in patients with schizophrenia except for the positive symptom dimension. The association between scores on the disorganization/cognitive and negative dimensions and later transition is consistent with independent evidence that formal thought disorder, subjective cognitive impairments, and negative symptoms are linked to the subsequent onset of psychosis.
Keywords: prodrome, psychopathology, schizophrenia
Introduction
A major focus of current research in psychosis is the early recognition and treatment of prodromal symptoms of psychosis. Over the last 2 decades, this has been associated with the development of early intervention services intended to delay or prevent the onset of schizophrenia and other psychotic disorders. Prodromal symptoms are associated with a greatly increased risk of transition to a psychotic disorder; however, only about a third of people with these features go on to develop psychosis.1,2 Individuals with prodromal symptoms can thus be described as having an at-risk mental state (ARMS).3
Despite considerable progress in identifying those at imminent risk of psychosis, the predictive accuracy of current early recognition procedures remains modest,4 with transition rates to psychosis ranging from 9% to 54% within 1 year after inclusion.5–8 This questions the accuracy and adequacy of current early recognition criteria that predominantly include attenuated positive symptoms, brief limited intermittent psychotic symptoms, or a combination of genetic risk and functional deterioration,9 but these criteria differ across the centers.10 More recently, in an attempt to improve predictive validity and early recognition of psychosis, studies have examined neurobiological predictors and have identified potential neurobiological correlates of transition to psychosis, as evidenced in meta-analytic work by Smieskova et al.11
Studies that have primarily focused on predictive value of individual ARMS symptoms have yielded inconsistent results. It thus remains unclear if particular features of the ARMS can predict subsequent transition to psychosis. Attenuated positive psychotic symptoms that are often the most commonly met inclusion criteria for the ARMS12,13 can also be experienced by non–help-seeking subjects in the healthy population.14,15 While it has been reported that they are not predictive of transition to psychosis in the ARMS,16 other studies have found that a number of individual symptoms such as ideas of reference, unusual thought content, and perceptual disturbances are associated with later transition to psychosis.7,8,17–20 Although negative symptoms and depression are not a part of standard inclusion criteria, they have been associated with subsequent transition,6,16–18 as have a number of subjective cognitive impairments,4,6,17,19,21 such as attentional impairment, difficulties with expressing and comprehending speech, reduced speed of information processing, dividing attention, and the blocking or interference with thinking.
There is now growing evidence that the psychopathology of established psychosis may be best described by several symptom dimensions.22 Many factor analytic studies of psychosis symptom profiles have identified multidimensional models such as the popular, 3 syndromic model proposed by Liddle.23 When affective symptoms have been incorporated, more complex dimensional patterns have emerged.24–29 These psychopathological dimensions appear to have distinct genetic and neurocognitive correlates.30,31 The extent to which analogous dimensions exist in the symptoms of those at high risk of psychosis is unclear. Hawkins et al.32 recently conducted a factor analytic study to examine the construct validity of the Scale of Prodromal Symptoms (SOPS) in an ARMS sample. Using a principal component analysis, they identified a 3-factor solution, with negative, general dysphoric, and positive symptom factors, but with restricted specificity for any particular symptom or sign in predicting psychosis. However, principal component analysis is a data reduction method, which is not suitable for detection of latent dimensional constructs, and psychopathological dimensions in the ARMS may be more readily identified by using a factor analysis. The identification of psychopathological dimensions is of particular interest in the ARMS because to date no studies have explored whether a particular constellation of symptoms may predict transition to psychosis, which may have a stronger prognostic value than individual symptom ratings.
The aim of the present study was to examine the dimensional structure of psychopathology in a sample of ARMS subjects using exploratory factor analytical methods on a comprehensive range of symptoms and signs. We predicted that its dimensional structure would resemble that previously described in patients with psychotic disorders.23–29 We then sought to assess the relationship between the identified symptom dimensions and the risk of subsequent transition to psychosis. On the basis of previous studies of psychopathological measures,6,16–19,21 we hypothesized that dimensions with heavy loadings from negative symptoms, depression, and cognitive impairments would be associated with an increased risk of later transition.
Methods
Participants
Individuals aged 16—35 years were recruited through Outreach and Support in South London (OASIS), a clinical service for people with an ARMS in South London.13 OASIS has an ongoing programme of liaison with local health and non-health agencies who may encounter people with prodromal symptoms suggestive of an “ARMS.” The information about early recognition signs and inclusion criteria was disseminated through regular meetings, presentations, and distribution of leaflets. Clients were referred from general practitioner surgeries, schools and colleges, social and faith groups, or adolescent and adult mental health services or have initiated contact themselves. Referred individuals were contacted by phone for an initial screening and then an assessment with OASIS was offered. Clients who met ARMS criteria6 were seen at regular intervals over the next 2 years with close clinical monitoring for signs of frank psychosis. Each participant gave written informed consent after receiving a complete description of the study.
Ethical approval for the study was obtained from the Institute of Psychiatry Research Ethics Committee.
Instruments
The presence of the ARMS was determined via a detailed clinical assessment using the Comprehensive Assessment of the At-Risk Mental State (CAARMS).9 An individual can meet ARMS criteria in one or more of 3 ways: (1) a recent decline in functioning, indicated by a 30% drop in the Global Assessment of Functioning (GAF)33 score from premorbid level sustained for a month, coupled with a first degree relative with psychosis; (2) “attenuated” positive psychotic symptoms defined as symptoms that are of a subthreshold intensity, ie, not severe enough (3–5 on “Disorders of Thought Content” subscale, 3–4 on “Perceptual Abnormalities” subscale, and/or 4–5 on “Disorganized Speech” subscales of the CAARMS), lasting at least a week or appearing several times per week; and (3) a brief psychotic episode of less than 1 week's duration that resolves without antipsychotic medication.
Within the CAARMS, 6 of the Huber's basic symptoms1 are incorporated: subjective experience of cognitive change, subjective emotional disturbance, avolition, subjective complaints of impaired motor functioning, subjective complaints of impaired bodily sensations, and subjective complaints of impaired autonomic functioning. Scores for each subscale range from 0 to 6. Only scores on the subscale of positive symptoms are used to evaluate the ARMS criteria.
Social functioning was assessed using the GAF.33 Transition to psychosis was defined as the onset of frank psychotic symptoms, ie symptoms at a severity greater than that corresponding to attenuated psychotic symptoms in the CAARMS, which did not resolve within 1 week. (Severity Scale score of 6 on Disorders of Thought Content subscale, 5 or 6 on Perceptual Abnormalities subscale, and/or 6 on Disorganized Speech subscales of the CAARMS.)12
The CAARMS is a semistructured interview, specifically designed to measure attenuated psychotic symptoms in people with an ARMS and widely used in both clinical and research settings. It includes 7 subscales: “Positive Symptoms” (disorders of thought content, perceptual abnormalities, and disorganized speech), “Negative Symptoms,” “Emotional Disturbance,” “Behavioral Change,” “Motor Changes,” “General Psychopathology” including manic, depressive, and anxiety symptoms, and “Cognitive Change.” “The Cognitive Change” subscale is composed of subjectively reported concentration and attention problems, thought form problems (eg, thought block, racing, or confused thoughts), comprehension difficulties and memory problems, as well as observed inattentiveness during interview or poor performance on simple intellectual functioning such as serial 7s. Subjective and objective observations were rated separately for all subscales.
The CAARMS has previously been reported to have good to excellent reliability (Yung et al. 200534). OASIS has regular interreliability meetings, and every case is discussed in a consensus clinical meeting with senior clinicians to determine whether a subject meets criteria for the ARMS.
Statistical Analysis
Factor Analysis.
Exploratory factor analysis (EFA) on the severity scores (1–5) of 21 CAARMS items definitely present in at least 10% of cases was performed using SPSS (version 16.0). One item, observed changes in motor functioning, was excluded because it was present in only 9.5% of the sample. The decision to choose EFA rather than a confirmatory factor analysis was based on the absence of precise factorial model both in established psychosis and in the ARMS. Furthermore, our aim was to explore latent dimensional constructs and not to test a previously developed method because to date there is no such model. The optimum number of factors was determined using a screen plot in combination with an a priori determined number of factors based on theoretically expected factor structure.35 The decision to retain 5 factors was based on previous studies that have identified 5-factor solutions.28,29,36
Unrotated factors were then subjected to orthogonal rotation using the Varimax method. In addition, we applied Promax rotation, which allows correlation between factors. Based on previous research, only items with robust loadings of greater than 0.4 were used to interpret resulting dimensions.29,36,37 Finally, for each patient, a total score for each dimension was calculated by summing up the scores of items within the dimension. Total scores were then used for subsequent analyses.
Missing Data.
Seven out of the 122 subjects had at least one missing observation (maximum: 3). The total number of missing observations was 20 (1%). To avoid the loss of these subjects in our factor analysis, we used single conditional imputation to replace missing data with estimates using expectation maximization algorithms as implemented in SPSS module “Missing Value Analysis 15.0.” This method imputes missing data with unbiased estimates by using the available information from the available data assuming that the pattern of missingness is related to the observed data only. This assumption of missing at random is less strict than the assumptions of a complete case analysis, which assumes missing completely at random.38 We additionally performed the factor analysis on the complete data set to determine that the obtained factor solution does not differ markedly from the one derived from the imputed data set.
Relationship Between Each Dimension's Total Score With Sociodemographic Variables and Transition to Psychosis.
We performed t test for independent samples, analysis of variance for comparisons of the total scores between 2 or more groups, and Pearson's correlations to assess the relationship between 2 continuous variables, such as GAF scores and total scores of dimensions.
Cox proportional hazards regression was used to examine the relationship between the derived factors (predictor variables) and transition to psychosis (dependent variable) during the 24-month period of clinical observation. To assess which of the 5 dimensions have the greatest effect on transition to psychosis, we standardized the variables so that they have mean of 0 and variance of 1 and rerun the Cox regressions with the standardized variables to obtain standardized regression coefficients. Results are presented as hazard ratios, P values, and 95% CI.
Results
Sample Characteristics
A total of 122 subjects with complete CAARMS data were included in the study. The mean age of the sample was 23 years, (range 15–35, SD 4.9), and 57% of the subjects were male. Almost half were from ethnic minorities, and most were single (80%) and either in a full-time employment or students (60%). The mean baseline GAF score was 60 (SD 11). Demographic and clinical data for the sample are presented in table 1.
Table 1.
Sociodemographic and Clinical Characteristics of the Outreach and Support in South London Sample
| Age (years) | Mean (SD) | 23.4 (4.9) |
| Gender | Male | 70 (57.4%) |
| Female | 52 (42.6%) | |
| Ethnicity | White British (White, born in UK) | 51 (41.8%) |
| Black British, African, and Caribbean | 35 (28.7%) | |
| White other (White, born outside of the UK) | 21 (17.2%) | |
| Other | 15 (12.3%) | |
| Marital status | Single | 98 (80.3%) |
| Married or living together | 17 (14.0%) | |
| Divorced/separated | 7 (5.7%) | |
| Occupation | Student | 36 (29.5%) |
| Employed | 37 (30.3%) | |
| Unemployed | 49 (40.2%) | |
| GAF score | Mean (SD) | 59.6 (11.1) |
| Transition to psychosis | Yes | 18 (14.8%) |
| No | 104 (85.2%) | |
| At-risk mental state criteria | Attenuated symptoms | 87 (71.3)% |
| Attenuated symptoms and brief limited intermittent psychotic symptoms | 18 (14.8%) | |
| Attenuated symptoms and trait | 17 (13.9%) |
GAF, Global Assessment of Functioning.
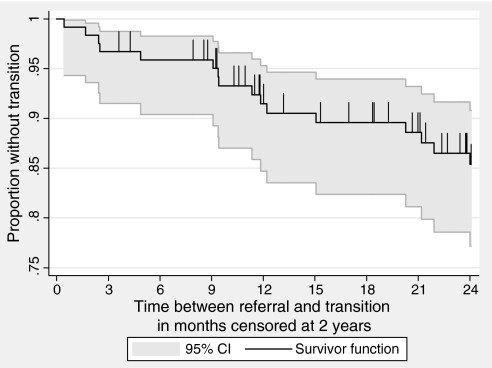
Of the 122 subjects included in the study, 18 (15%) made a transition to psychosis during the follow-up period. The mean duration to transition was 419 days (SD 322.63, minimum 13 to maximum 1101 days, median 352.5). Of the 104 subjects who did not make a transition, 30 (28.8%) have been with OASIS less than 2 years. Figure 1 shows a Kaplan Meyer survival curve indicating transition to psychosis in months from the referral, censored at 2 years.
Fig. 1.
Survival Curve of the Outreach and Support in South London Sample.
Psychopathological Dimensions
Principal factor analysis yielded a 5-factor solution of negative, anxiety, disorganization/cognitive, self-harm, and manic symptom dimensions, explaining 37% of total variance (table 2). Promax and Varimax rotation yielded very similar results, which was also the case with imputed and complete data sets.
Table 2.
Psychopathological Dimensions of the At-Risk Mental State Sample
| Factors |
|||||
| Dimensions (% Variance) | 1 | 2 | 3 | 4 | 5 |
| Negative (13.3) | |||||
| Social isolation | .763 | .009 | .212 | −.038 | .117 |
| Anhedonia | .745 | .000 | .137 | .310 | .026 |
| Impaired role of functioning | .727 | −.040 | .288 | −.051 | .171 |
| Observed blunted affect | .607 | .071 | −.074 | −.064 | −.008 |
| Depression | .564 | .189 | .265 | .353 | −.101 |
| Avolition | .504 | .190 | .301 | .238 | .090 |
| Disorganized behavior | .412 | .084 | .099 | −.022 | .178 |
| Anxiety (7.6) | |||||
| Subjective complaints of impaired autonomic functioning | .144 | .604 | −.009 | .028 | .246 |
| Impaired tolerance to normal stress | .078 | .558 | .067 | .053 | .014 |
| Anxiety | .077 | .538 | −.301 | .171 | .020 |
| Mood swings | .095 | .458 | .192 | .184 | .147 |
| Alogia | .283 | .413 | .191 | .033 | .145 |
| Disorganization/cognitive (6.6) | |||||
| Observed cognitive change | .248 | −.012 | .616 | .042 | .010 |
| Subjective cognitive change | .334 | .249 | .575 | .231 | −.024 |
| Disorganized speech | .055 | .165 | .442 | −.006 | .134 |
| Self-harm (4.8) | |||||
| Suicidality and self-harm | .095 | .213 | −.320 | .620 | −.016 |
| Subjective emotional disturbance | .394 | −.007 | .228 | .446 | .100 |
| Manic (4.2) | |||||
| Mania | −.077 | .042 | .032 | −.029 | .508 |
| Subjective complaints of impaired motor functioning | .192 | .189 | .194 | .275 | .418 |
Note: Principal axis factoring was used. Unrotated factors were subject to orthogonal (Varimax) rotation. High factor loadings are presented in bold.
The first factor comprised 7 items: social isolation, anhedonia, impaired role of functioning, observed blunted affect, depression, avolition, and disorganized behavior. This was categorized as a negative dimension. The second factor comprised subjective complaints of impaired autonomic functioning impaired tolerance to normal stress, anxiety, mood swings, and alogia and was termed anxiety. The third factor, termed the disorganization/cognitive dimension, comprised observed cognitive change, subjective cognitive change, and disorganized speech. Suicidality and self-harm along with subjective emotional disturbance loaded separately onto a fourth factor, termed self-harm, while mania and subjective complaints of impaired motor functioning aligned together along what was categorized as a manic dimension.
Dimensional Scores
The dimensional total scores correlated strongly with their respective factor scores, but not with the other factor scores. Correlations between the total score for each dimension and their respective factor scores ranged between r = 0.79 and r = 0.95 and were less than r = 0.37 with factor scores of the other remaining factors.
Relationship Between Dimensional Scores and Transition to Psychosis
Cox regression analysis revealed that both the negative and the disorganization/cognitive dimensions were significantly associated with the risk of developing psychosis. Subjects who had made a transition to psychosis scored higher on each of these dimensions than those who had not become psychotic. There were no significant differences between these 2 subgroups on the other 3 symptom domains (table 3). Means and SDs for a total sample and separated for those who did and did not make transition are presented in table 4.
Table 3.
Separate Cox Regression Analyses (P values) for Each of the 5 Dimensions (Predictor Variables) and Transition to Psychosis (Dependent Variable) Over a 24-Month Period of Observation
| Hazard Ratio (95% CI) | Robust SE | z | P | Standardized Hazard Ratio (95% CI) | |
| Negative | 1.06 (1.002–1.128) | 0.0323 | 2.202 | 0.044 | 1.68 (1.01–2.80) |
| Anxiety | 0.99 (0.88–1.11) | 0.058 | −0.17 | 0.867 | 0.95 (0.54–1.67) |
| Disorganization/cognitive | 1.21 (1.06–1.38) | 0.082 | 2.79 | 0.005 | 1.70 (1.16–2.39) |
| Self-harm | 1.06 (0.83–1.35) | 0.131 | 0.44 | 0.662 | 1.13 (0.64–2.03) |
| Manic | 1.17 (0.92–1.49) | 0.145 | 1.25 | 0.212 | 1.33 (0.85–2.10) |
Table 4.
Means (SD) of Total Symptom Scores for Patients With and Without a Transition to Psychosis Within the First 2 Years After Referral
| Total Sample | No Transition (N = 106) | Transition (N = 16) | |
| Total Score | Mean (SD) | Mean (SD) | Mean (SD) |
| Negative | 18.09 (8.53) | 17.45 (8.41) | 22.25 (8.36) |
| Anxiety | 5.34 (2.70) | 5.11 (2.62) | 6.88 (2.83) |
| Disorganization/cognitive | 10.51 (4.86) | 10.55 (4.73) | 10.25 (5.80) |
| Self-harm | 3.74 (2.37) | 3.70 (2.32) | 4.06 (2.74) |
| Manic | 1.82 (1.86) | 1.72 (1.71) | 2.44 (2.61) |
There were strong negative correlations between the total score on the negative and anxiety domains and the GAF score. There were also weaker but still significant negative correlations between scores on the disorganization/cognitive and the self-harm domains and the GAF score (table 5).
Table 5.
Correlations Between Dimension Scores and Global Assessment of Functioning (GAF) Score Within the At-Risk Mental State Group at Presentation (n = 122)
| Dimension | Pearson's r | P |
| Negative | −0.57 | <0.0001 |
| Anxiety | −0.34 | <0.0001 |
| Disorganization/cognitive | −0.22 | 0.014 |
| Self-harm | −0.28 | 0.002 |
| Manic | −0.1 | 0.29 |
Relationship Between Dimensional Scores and Sociodemographic Variables
Significant associations emerged between the negative dimension and different occupation types (F(2.117) = 5.3, P = 0.006). Subjects who were students or employed had fewer negative symptoms (students vs unemployed: Cohen's d = −0.54 [95% CI: −0.98 to −0.1], employed vs unemployed: d = 0.64 [95% CI: −1.08 to 0.19]). There were no significant differences in the total score for each dimension between males and females, between black and white subjects, or age.
Discussion
This is the first study to examine psychopathological dimensions in the ARMS using ratings from the CAARMS, one of the most widely used instruments for assessing prodromal symptoms and the first to examine the association between dimensions derived from the CAARMS with later transition to psychosis. Principal axis factoring identified a dimensional structure similar, but not identical, to that previously defined in patients with chronic22,23,36 and recent episode psychosis.29 Furthermore, scores on both the disorganization/cognitive and negative dimensions were significantly associated with subsequent transition to psychosis.
Psychopathological Dimensions in the ARMS
The negative factor that accounted for the most of the variance closely resembles the negative dimension previously described in both chronic and first episode patients with schizophrenia,36,39 and is consistent with findings obtained from a prodromal sample using another psychopathological instrument, the SOPS.32 Apart from negative symptoms such as avolition, blunted affect, and social isolation, in the present study, anhedonia and depression loaded together with these symptoms on the negative dimension. This suggests that in this sample, negative symptoms may be secondary to depression, as suggested by Liddle et al.40 who also reported an association between anhedonia and negative psychotic symptoms. However, because the data in the present study were cross sectional, it is difficult to determine whether negative symptoms were “primary” or a feature of depression. Considerable overlap between depressive and negative symptoms has been reported also in other studies of psychopathology in patients with schizophrenia.41 Dolan et al.42 have suggested that negative symptoms in schizophrenia and depression share a common pathophysiological basis because both have been associated with reduced resting prefrontal activity in neuroimaging studies. However, other studies in schizophrenia have identified an independent depression factor, clearly distinct from negative symptoms.43 These discrepant findings may reflect the use of different rating scales and definitions for depression and negative symptoms across studies and the sampling of different patient populations. Therefore, it is early to draw firm conclusions that the negative symptoms in our sample are of secondary nature, until these findings are further explored and replicated in future studies.
In the present study, depression was not only related to the negative dimension alone but also loaded onto the self-harm factor and to a lesser extent on the anxiety dimension. The latter is in line with findings from 2 studies40,44 that reported that anxiety symptoms cosegregated with depressive symptoms on a single factor. Depressive symptoms are relatively common in the ARMS,13 and the nonspecificity of depression in our sample might reflect dysphoria and distress secondary to the recent onset of psychotic experiences. Similarly, we found that alogia loaded with anxiety symptoms, as opposed to negative symptoms. It is possible that different manifestations of alogia, such as reduced speech expression and hesitancies in spontaneous speech, occurred in the context of anxiety in our sample rather than reflecting a primary alogia seen in patients with the “deficit” syndrome of schizophrenia.45
A striking finding was the presence of a disorganization/cognitive dimension in the ARMS, albeit contributing only modestly to the total variance. This comprised subjective and objective cognitive changes and disorganized speech. Cardinal features of disorganization are formal thought disorder and inappropriate affect, but attentional impairment has been reported in several studies as a constituent feature of this dimension.40,46 In the CAARMS, Cognitive Change is a subscale comprising impaired attention, and thought block and racing thoughts, whereas Disorganized Speech includes 2 additional aspects of formal thought disorder, circumstantiality and tangentiality. The disorganization/cognitive dimension in our sample thus resembles the disorganization dimension identified in studies of patients with established psychosis, which typically comprises formal thought disorder and attentional impairment.40
We did not identify the reality distortion dimension that has been consistently reported in studies of patients with established psychosis.29,36,40 This may seem surprising, given that attenuated positive symptoms like abnormal beliefs and perceptions were by far the commonest presenting symptoms in our sample. However, paradoxically, because the attenuated positive symptoms were one of the inclusion criteria, all the subjects we studied scored on these items, and there may have been an insufficient variance within the sample to permit clear segregation of a factor associated with them. This issue might be addressed by applying the present analysis in ARMS subjects who have been followed up after presentation because there is a divergence of symptom severity within ARMS groups over time, with some subjects showing a symptomatic improvement, others remaining stable, and a proportion showing a worsening of symptoms.2 Another approach would be to examine symptom dimensions at an earlier stage of the ARMS when attenuated positive symptoms may be less prevalent.47
Transition to Psychosis
We found that both the disorganization/cognitive and negative dimensions were associated with subsequent transition to psychosis. This is consistent with a report that in adolescents at high risk, a set of attenuated negative and disorganization symptoms, in combination with neurocognitive and social deficits, preceded the onset of schizophrenia.48 Similarly, Gourzis et al.49 categorized Diagnostic and Statistical Manual of Mental Disorders, Third Edition Revised prodromal symptoms into negative, positive prepsychotic, and positive disorganization factors and found that a set of negative symptoms including affective dysfunction and closely resembling the negative dimension in the present study were the most common symptoms in subjects who went on to develop schizophrenia. Our results are also in line with prospective studies of the ARMS that have focused on individual symptoms and have reported that certain negative symptoms particularly, social isolation, are predictive of later psychosis.16,50 On the other hand, other symptoms within our negative dimension, such as avolition, anhedonia, and blunted affect, have not been found to be predictive when they were studied as individual items.2 Retrospective accounts of the prodrome by patients assessed at the first episode psychosis have also pointed to a high prevalence of depressive and negative symptoms prior to the onset of illness, particularly in the early prodromal phase. For example, Hafner et al.51 in a study of 232 first episode subjects found that depressive and negative symptoms were early features of the prodrome, with depression the most frequent and earliest symptom.
Our observation that cognitive features were associated with transition to psychosis is consistent with evidence that both impaired attention and formal thought disorder, components of our disorganization/cognitive dimension, have individually been associated with the later onset of psychosis in the ARMS.2 Additionally, Klotterkotter et al.,17 using basic symptom concept in a 10-year follow-up study, found that a symptom cluster of thought impairment, language, perception, and motor disturbance were highly predictive of subsequent schizophrenia. Furthermore, subjective cognitive impairments were present in all the high-risk subjects that later progressed to psychosis. Finally, research in people with schizotypyal features indicates that the later onset of psychosis is linked to cognitive disorganization and anhedonia52 and to the presence of formal thought disorder manifested as aberrant speech.53
Both Kraepelin54 and Bleuler55 held that a combination of negative and cognitive symptoms were core psychopathological features of schizophrenia. It is possible that these symptoms are the phenomenological expression of an underlying neurodevelopmental perturbation that confers a particularly high risk for the disorder.56
Our findings suggest that more attention should be given to disorganization, cognitive, and negative features. However, the absence of a positive symptom dimension in the present study indicates that an effect of positive symptoms on the risk of transition cannot be excluded.
Association of Dimensions With GAF Scores
There was a striking correlation between negative and anxiety dimensions and poor global functioning, as indexed by the GAF score. This is not surprising, given that the negative dimension comprised items which can have a powerful influence on the GAF score, such as social isolation, impaired role functioning, and avolition. Poor global functioning has previously been independently associated with the subsequent onset of psychosis in the ARMS.57 Cornblatt et al.48 suggested that a sustained attentional impairment in those at high risk disrupts processing of social information, leading to difficulties in interacting with others and the emergence of social difficulties and isolation. There was also a significant but less prominent correlation between the disorganization/cognitive dimension and poor global functioning.
The association between the severity of the negative and disorganization/cognitive dimensions and poor global functioning and evidence that all these may predict subsequent transition to psychosis suggest that they may each be a manifestation of a common underlying process that increases the risk of later illness.
Methodological Issues
The amount of variance explained by the 5-factor solution in our study was relatively low compared with studies of psychopathology in schizophrenia. However, these studies employed principal component analysis, which is a data reduction method with components derived using the variance of the manifest variables rather than the covariance alone. The variance in components is thus likely to be higher than for factors. The amount of variance also depends on the number of items entered into the analysis and hence the clinical instrument used. In general, the severity of symptoms in subjects with an ARMS is less than in patients with schizophrenia,13 and the ARMS is more heterogeneous with respect to subsequent clinical course. This may also have reduced the variance explained. Because none of our subjects were psychotic and most were medication naive, it is unlikely that the symptomatology and dimensional structure were secondary to effects of chronic illness or treatment.
Conclusion
To date, the assessment and treatment of the ARMS has largely focused on attenuated positive symptoms. Our observations that negative and disorganized/cognitive dimensions are associated with transition to psychosis suggest that, in addition to attenuated positive symptoms, the predictive value of negative symptoms and those relating to disorganization/cognitive construct should also be considered, which may lead to the development of more effective early detection criteria. These symptoms can be assessed in detail using the Bonn Scale for the Assessment of Basic Symptoms and the Schizophrenia Prediction Instrument for Adults,1 although to date these instruments have mainly been used in German-speaking countries. Our findings also raise the possibility that treatment strategies directed at cognitive impairments and negative symptoms may also be useful in the ARMS: to date, pharmacological and psychological interventions have mainly focused on positive psychotic symptoms.58
Funding
The OASIS service was supported by the Guy's and St Thomas’ Charitable Foundation; South London and Maudsley Trust.
Acknowledgments
Recruitment and follow-up of the participants was carried out by the OASIS clinical team, including Matthew Broome, James Woolley, Elvira Bramon, Paul Tabraham, Fern Day, Deana Hall, Oliver Howes, and Toby Winton-Brown. Our special thanks go to the staff and service users of OASIS.
References
- 1.Huber G, Gross G, Schuttler R, Linz M. Longitudinal studies of schizophrenic patients. Schizophr Bull. 1980;6:592–605. doi: 10.1093/schbul/6.4.592. [DOI] [PubMed] [Google Scholar]
- 2.Yung AR, Phillips LJ, Yuen HP, McGorry PD. Risk factors for psychosis in an ultra high-risk group: psychopathology and clinical features. Schizophr Res. 2004;67:131–142. doi: 10.1016/S0920-9964(03)00192-0. [DOI] [PubMed] [Google Scholar]
- 3.McGorry P. Rationale for and the substantial potential benefits linked to early recognition and optimal treatment of psychotic disorders, specifically schizophrenia. Acta Psychiatr Scand. 2001;103:402–403. doi: 10.1034/j.1600-0447.2001.103005401.x. [DOI] [PubMed] [Google Scholar]
- 4.Riecher-Rossler A, Pflueger MO, Aston J, et al. Efficacy of using cognitive status in predicting psychosis: a 7-year follow-up. Biol Psychiatry. 2009;66:1023–1030. doi: 10.1016/j.biopsych.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 5.Miller TJ, McGlashan TH, Rosen JL, et al. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr Bull. 2003;29:703–715. doi: 10.1093/oxfordjournals.schbul.a007040. [DOI] [PubMed] [Google Scholar]
- 6.Yung AR, Phillips LJ, Yuen HP, et al. Psychosis prediction: 12-month follow up of a high risk (“prodromal”) group. Schizophr Res. 2003;60:21–32. doi: 10.1016/s0920-9964(02)00167-6. [DOI] [PubMed] [Google Scholar]
- 7.Haroun N, Dunn L, Haroun A, Cadenhad KS. Risk and protection in prodromal schizophrenia: ethical implications for clinical practice and future research. Schizophr Bull. 2006;32:166–178. doi: 10.1093/schbul/sbj007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ruhrmann S, Schultze-Lutter F, Salokangas RKR, et al. Prediction of psychosis in adolescents and young adults at high risk. Results from the Prospective European Prediction of Psychosis Study. Arch Gen Psychiatry. 2010;67:241–251. doi: 10.1001/archgenpsychiatry.2009.206. [DOI] [PubMed] [Google Scholar]
- 9.Phillips LJ, Yung A, McGorry PD. Identification of young people at “ultra” high risk of psychosis: validation of the personal assessment and crisis evaluation clinic intake criteria. Aust N Z J Psychiatry. 2000;34:S164–S169. doi: 10.1080/000486700239. [DOI] [PubMed] [Google Scholar]
- 10.Klosterkotter J, Schultze_Lutter F, Rurhman S. Kraepelin and psychotic prodromal conditions. Am J Psychiatry. 2008;258:74–84. doi: 10.1007/s00406-008-2010-5. [DOI] [PubMed] [Google Scholar]
- 11.Smieskova R, Fusar-Poli P, Allen P, et al. Neuroimaging predictors of transition to psychosis—A systematic review and meta-analysis. Neurosci Biobehav Rev. 2010;34:1207–1222. doi: 10.1016/j.neubiorev.2010.01.016. [DOI] [PubMed] [Google Scholar]
- 12.Yung AR, Phillips LJ, McGorry PD, et al. Prediction of psychosis. A step towards indicated prevention of schizophrenia. Br J Psychiatry. 1998;172(suppl):14–20. [PubMed] [Google Scholar]
- 13.Broome MR, Woolley JB, Tabraham P, et al. What causes the onset of psychosis? Schizophr Res. 2005;79:23–34. doi: 10.1016/j.schres.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 14.Eaton WW, Badawi M, Melton B. Prodromes and precursors: epidemiologic data for primary prevention of disorders with slow onset. Am J Psychiatry. 1995;152:967–972. doi: 10.1176/ajp.152.7.967. [DOI] [PubMed] [Google Scholar]
- 15.Tien AY. Distributions of hallucinations in the population. Soc Psychiatry Psychiatr Epidemiol. 1991;26:287–292. doi: 10.1007/BF00789221. [DOI] [PubMed] [Google Scholar]
- 16.Johnstone EC, Ebmeier KP, Miller P, Owens DG, Lawrie SM. Predicting schizophrenia: findings from the Edinburgh High-Risk Study. Br J Psychiatry. 2005;186:18–25. doi: 10.1192/bjp.186.1.18. [DOI] [PubMed] [Google Scholar]
- 17.Klosterkotter J, Hellmich M, Steinmeyer EM, Schultze-Lutter F. Diagnosing schizophrenia in the initial prodromal phase. Arch Gen Psychiatry. 2001;58:158–164. doi: 10.1001/archpsyc.58.2.158. [DOI] [PubMed] [Google Scholar]
- 18.Lencz T, Smith CW, Auther A, Correll CU, Cornblatt B. Nonspecific and attenuated negative symptoms in patients at clinical high-risk for schizophrenia. Schizophr Res. 2004;68:37–48. doi: 10.1016/S0920-9964(03)00214-7. [DOI] [PubMed] [Google Scholar]
- 19.Mason O, Startup M, Halpin S, Schall U, Conrad A, Carr V. Risk factors for transition to first episode psychosis among individuals with ‘at-risk mental states'. Schizophr Res. 2004;71:227–237. doi: 10.1016/j.schres.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 20.Cannon TD, Cadenhad K, Cornblatt B, et al. Prediction of psychosis in youth at high clinical risk. A Multisite Longitudinal Study in North America. Arch Gen Psychiatry. 2008;65:28–37. doi: 10.1001/archgenpsychiatry.2007.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lam MML, Hung SF, Chen EYH. Transition to psychosis: 6-month follow-up of a Chinese high-risk group in Hong Kong. Aust N Z J Psychiatry. 2006;40:414–420. doi: 10.1080/j.1440-1614.2006.01817.x. [DOI] [PubMed] [Google Scholar]
- 22.Van Os J, Fahy TA, Jones P, et al. Psychopathological syndromes in the functional psychoses: associations with course and outcome. Psychol Med. 1996;26:161–176. doi: 10.1017/s0033291700033808. [DOI] [PubMed] [Google Scholar]
- 23.Liddle PF. The symptoms of chronic schizophrenia. A re-examination of the positive-negative dichotomy. Br J Psychiatry. 1987;151:145–151. doi: 10.1192/bjp.151.2.145. [DOI] [PubMed] [Google Scholar]
- 24.Cuesta MJ, Peralta V, Gil P, Artamendi M. Psychopathological dimensions in first-episode psychoses. From the trunk to the branches and leaves. Eur Arch Psychiatry Clin Neurosci. 2003;253:73–79. doi: 10.1007/s00406-003-0410-0. [DOI] [PubMed] [Google Scholar]
- 25.McGorry PD, Bell RC, Dudgeon PL, Jackson HJ. The dimensional structure of first episode psychosis: an exploratory factor analysis. Psychol Med. 1998;28:935–947. doi: 10.1017/s0033291798006771. [DOI] [PubMed] [Google Scholar]
- 26.Kitamura T, Okazaki Y, Fujinawa A, Yoshino M, Kasahara Y. Symptoms of psychoses. A factor-analytic study. Br J Psychol. 1995;166:236–240. doi: 10.1192/bjp.166.2.236. [DOI] [PubMed] [Google Scholar]
- 27.Peralta V, Cuesta MJ, Martinez-Larrea A, Serrano JF. Patterns of symptoms in neuroleptic-naive patients with schizophrenia and related psychotic disorders before and after treatment. Psychol Res. 2001;105:97–105. doi: 10.1016/s0165-1781(01)00319-5. [DOI] [PubMed] [Google Scholar]
- 28.Wickham H, Walsh C, Asherson P, et al. Familiality of symptom dimensions in schizophrenia. Schizophr Res. 2001;47:223–232. doi: 10.1016/s0920-9964(00)00098-0. [DOI] [PubMed] [Google Scholar]
- 29.Demjaha A, Morgan K, Morgan C, et al. Combining dimensional and categorical representation of psychosis: the way forward for DSM-V and ICD-11? Psychol Med. 2009;39:1943–1955. doi: 10.1017/S0033291709990651. [DOI] [PubMed] [Google Scholar]
- 30.Cardno AG, Sham PC, Murray RM, McGuffin P. Twin study of symptom dimensions in psychoses. Br J Psychiatry. 2001;179:39–45. doi: 10.1192/bjp.179.1.39. [DOI] [PubMed] [Google Scholar]
- 31.Norman RM, Malla AK, Morrison-Stewart SL, et al. Neuropsychological correlates of syndromes in schizophrenia. Br J Psychiatry. 1997;170:134–139. doi: 10.1192/bjp.170.2.134. [DOI] [PubMed] [Google Scholar]
- 32.Hawkins KA, McGlashan TH, Quinlan D, et al. Factorial structure of the Scale of Prodromal Symptoms. Schizophr Res. 2004;68:339–347. doi: 10.1016/S0920-9964(03)00053-7. [DOI] [PubMed] [Google Scholar]
- 33.4th ed. Washington, DC: American Psychiatric Association; 1994. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 34.Yung AR, Yuen HP, McGorry PD, et al. Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust N Z J Psychiatry. 2005;39(11-12):964–971. doi: 10.1080/j.1440-1614.2005.01714.x. [DOI] [PubMed] [Google Scholar]
- 35.Tabachnik BG, Fidell LS. Using Multivariate Statistics. 2nd ed. New York, NY: Harper Collins; 1989. [Google Scholar]
- 36.Dikeos DG, Wickham H, McDonald C, et al. Distribution of symptom dimensions across Kraepelinian divisions. Br J Psychiatry. 2006;189:346–353. doi: 10.1192/bjp.bp.105.017251. [DOI] [PubMed] [Google Scholar]
- 37.Comrey AL, Lee HB. A First Course in Factor Analysis. 2nd ed. Hillsdale, NJ: Lawrence Associates; 1992. [Google Scholar]
- 38.Dempster AP, Laird NM, Rubin DB. Maximum likelihood of incomplete data via the EM algorithm. J R Stat Soc. 1977;39:1–38. [Google Scholar]
- 39.Van Os J, Marcelis M, Sham P, Jones P, Gilvarry K, Murray R. Psychopathological syndromes and familial morbid risk of psychosis. Br J Psychiatry. 1997;170:241–246. doi: 10.1192/bjp.170.3.241. [DOI] [PubMed] [Google Scholar]
- 40.Liddle PF, Ngan ET, Duffield G, Kho K, Warren AJ. Signs and symptoms of psychotic illness (SSPI): a rating scale. Br J Psychiatry. 2002;180:45–50. doi: 10.1192/bjp.180.1.45. [DOI] [PubMed] [Google Scholar]
- 41.Kulhara P, Avasthi A, Chadda R, Chandiramani K. Negative and depressive symptoms in schizophrenia. Br J Psychiatry. 1989;154:207–211. doi: 10.1192/bjp.154.2.207. [DOI] [PubMed] [Google Scholar]
- 42.Dolan RJ, Bench CJ, Liddle PF, et al. Dorsolateral prefrontal cortex dysfunction in the major psychoses; symptom or disease specificity? J Neurol Neurosurg Psychiatry. 1993;56:1290–1294. doi: 10.1136/jnnp.56.12.1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Addington D, Addington J, Maticka-Tyndale E, Joyce J. Reliability and validity of a depression rating scale for schizophrenics. Schizophr Res. 1992;6:201–208. doi: 10.1016/0920-9964(92)90003-n. [DOI] [PubMed] [Google Scholar]
- 44.Emsley RA, Oosthuizen PP, Joubert AF, Roberts MC, Stein DJ. Depressive and anxiety symptoms in patients with schizophrenia and schizophreniform disorder. J Clin Psychiatry. 1999;60:747–751. doi: 10.4088/jcp.v60n1105. [DOI] [PubMed] [Google Scholar]
- 45.Carpenter WT, Jr, Heinrichs DW, Wagman AM. Deficit and nondeficit forms of schizophrenia: the concept. Am J Psychiatry. 1988;145:578–583. doi: 10.1176/ajp.145.5.578. [DOI] [PubMed] [Google Scholar]
- 46.Earnst KS, Kring AM. Construct validity of negative symptoms: an empirical and conceptual review. Clin Psychol Rev. 1997;17:167–189. doi: 10.1016/s0272-7358(96)00052-9. [DOI] [PubMed] [Google Scholar]
- 47.Ruhrmann S, Schultze-Lutter F, Klosterkotter J. Early detection and intervention in the initial prodromal phase of schizophrenia. Pharmacopsychiatry. 2003;36(suppl 3):S162–S167. doi: 10.1055/s-2003-45125. [DOI] [PubMed] [Google Scholar]
- 48.Cornblatt BA. The New York high risk project to the Hillside recognition and prevention (RAP) program. Am J Med Genet. 2002;114:956–966. doi: 10.1002/ajmg.b.10520. [DOI] [PubMed] [Google Scholar]
- 49.Gourzis P, Katrivanou A, Beratis S. Symptomatology of the initial prodromal phase in schizophrenia. Schizophr Bull. 2002;28:415–429. doi: 10.1093/oxfordjournals.schbul.a006950. [DOI] [PubMed] [Google Scholar]
- 50.McGorry PD, McKenzie D, Jackson HJ, Waddell F, Curry C. Can we improve the diagnostic efficiency and predictive power of prodromal symptoms for schizophrenia? Schizophr Res. 2000;42:91–100. doi: 10.1016/s0920-9964(99)00125-5. [DOI] [PubMed] [Google Scholar]
- 51.Hafner H, Maurer K, Trendler G, Heiden Wad, Schmidt M, Konnecke R. Schizophrenia and depression. Challenging the paradigm of two separate diseases—A controlled study of schizophrenia, depression and healthy controls. Schizophr Res. 2005;77:11–24. doi: 10.1016/j.schres.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 52.Venables PH, Bailes K. The structure of schizotypy, its relation to subdiagnoses of schizophrenia and to sex and age. Br J Clin Psychol. 1994;33:277–294. doi: 10.1111/j.2044-8260.1994.tb01124.x. [DOI] [PubMed] [Google Scholar]
- 53.Weinstein S, McKay R, Ngan ET. Positive schizotypy is not associated with speech abnormality. Early Interv Psychiatry. 2008;2:98–102. doi: 10.1111/j.1751-7893.2008.00064.x. [DOI] [PubMed] [Google Scholar]
- 54.Kraepelin E. Dementia Praecox and Paraphrenia. Edinborough, UK: Livingstone; 1919. [Google Scholar]
- 55.Bleuler E. Textbook of Psychiatry. 1924. [Brill AA, Trans]. New York, NY: McMillan; 1924. [Google Scholar]
- 56.Murray RM, Lewis SW. Is schizophrenia a neurodevelopmental disorder? BMJ. 1987;295:681–682. doi: 10.1136/bmj.295.6600.681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yung AR, Stanford C, Cosgrave E, et al. Testing the ultra high risk (prodromal) criteria for the prediction of psychosis in a clinical sample of young people. Schizophr Res. 2006;84:57–66. doi: 10.1016/j.schres.2006.03.014. [DOI] [PubMed] [Google Scholar]
- 58.McGorry PD, Yung AR, Phillips LJ, et al. Randomized controlled trial of interventions designed to reduce the risk of progression to first-episode psychosis in a clinical sample with subthreshold symptoms. Arch Gen Psychiatry. 2002;59:921–928. doi: 10.1001/archpsyc.59.10.921. [DOI] [PubMed] [Google Scholar]