Abstract
The concept of cognitive insight was introduced in 2004 to describe the capacity of patients with psychosis to distance themselves from their psychotic experiences, reflect on them, and respond to corrective feedback. The Beck Cognitive Insight Scale (BCIS) was developed to evaluate these aspects of cognitive flexibility and to complement scales that describe the lack of awareness of mental illness and its characteristics. The BCIS has generated a moderate research literature, which is the subject of the current review. Several independent groups have demonstrated that the BCIS is reliable, demonstrates convergent and construct validity, and distinguishes patients with psychosis from healthy controls and patients without psychosis. While the majority of the studies have focused on the relationship of the BCIS to delusions, several have examined its relationship to negative symptoms, depression, anxiety, and functional outcome. Cognitive insight has predicted positive gains in psychotherapy of psychosis, and improvement in cognitive insight has been correlated with improvement in delusional beliefs. Finally, preliminary findings relate neurocognition, metacognition, and social cognition, as well as reduced hippocampal volume to cognitive insight. A heuristic framework is presented to guide future research.
Keywords: insight, psychosis, delusions, psychosocial treatment
Introduction
As old as psychiatry itself and especially pertinent to psychosis,1 the concept of insight has undergone considerable refinement over the past 100 years. Early accounts defined insight as a single dimension—awareness of having a disorder—to be applied in a binary fashion such that patients possessed insight or lacked it entirely.2,3 Subsequent writers have developed insight into a multidimensional and continuous construct.4 Patients can now be evaluated by the degree to which they demonstrate awareness of illness, its signs and symptoms, and the need for treatment, attribute benefits to treatment, accept the illness label, understand the social consequences of illness, etc.5 The assessment of “clinical insight” in this manner has become invaluable for the formulation and treatment of psychosis.6
An important extension of the insight concept was introduced with the description of “cognitive insight,” defined as a patient's current capacity to evaluate his or her anomalous experiences and atypical interpretations of events.6 Unlike patients with nonpsychotic disorders (eg, depression or panic disorder), patients with psychosis are severely limited in their capacity to reflect upon their thinking problems and to recognize the errors and correct them. Indeed, Beck and Warman6 described 4 aspects of cognitive insight that can be disrupted in psychosis: (a) impairment of ability to be objective about delusional experiences and cognitive distortions, (b) reduced capacity to put these experiences into perspective, (c) unresponsiveness to corrective information from others, and (d) overconfidence in delusional judgments. The authors proposed that these characteristics were identifiable and quantifiable.
The Beck Cognitive Insight Scale (BCIS) was devised to measure patients' capacity for distancing themselves from and re-evaluating anomalous beliefs and misinterpretations.7 The BCIS is a 15-item self-report measure (the full scale appears in the Appendix) composed of 2 subscales: 9 Self-Reflectiveness items that assess objectivity, reflection, and openness to feedback and 6 Self-Certainty items that tap certainty about being right and resistance to correction. A principle components analysis confirmed the validity of a 2-factor solution, with each factor also shown to be internally consistent.7 The authors derived a composite cognitive insight index score (Composite Index) by subtracting the Self-Certainty score from the Self-Reflectiveness score. The Index significantly correlated with the Awareness of Having a Mental Disorder item on the Scale to Assess Unawareness of Mental Disorder (SUMD)8 and differentiated acutely unwell inpatients with psychotic disorders from those with major depressive disorder without psychotic features, demonstrating convergent and criterion validity, respectively. There were a number of limitations in the methodology of the original study of Beck et al.: Neither the reliability nor the validity of the patient diagnoses was determinable, degree of symptomatology was not measured, test-retest reliability was not estimated, and the sample was disproportionately schizoaffective.
In the time that has elapsed since the BCIS was introduced, 21 empirical studies that employ the cognitive insight construct have been published. These articles address the limitations of the original article and extend the scope of findings. The scale has been accurately translated into Chinese,9 Turkish,10 Norwegian,11 French,12 Spanish,13 Korean,14 and Japanese.15 The present article aims to review and synthesize the published literature with an eye to elucidating the psychometric characteristics and applications of the BCIS. The article is divided into 4 sections. The first section addresses the quality of the scale by reviewing the available psychometric data. The second section reports correlations with clinical features of the disorder. The third section reviews applications of cognitive insight to research on treatment, functional outcome, as well as neurocognition and neurobiology. Finally, the fourth section evaluates the state of this developing literature and introduces a heuristic model that charts out fruitful lines of future research.
Psychometrics
Table 1 contains the data for all studies considered in the present review, cross-referenced with the text. For the sake of brevity, the details of each study in terms of sample, design, and results appear in the table.
Table 1.
Studies Including the Beck Cognitive Insight Scale (BCIS)
| Study | Design | Participants | Main Findings |
| Beck et al.7 | Cross-sectional | 150 inpatients: 43 schizoaffective, 32 schizophrenia, 16 MDD with psychotic features, 59 MDD without psychotic features | ▪ Factor analysis: 2 components (SR and SC) |
| ▪ Reliability (alpha): whole sample (SR = .68, SC = .60); schizophrenia/schizoaffective (SR = .67, SC = .61) | |||
| ▪ Clinical insight (r, BCIS, and SUMD): CI and awareness of mental disorder = −.62; SR and delusions = −.67 | |||
| ▪ Diagnostic (means): psychotic < nonpsychotic (CI and SR); psychotic > nonpsychotic (SC); MDD with psychosis < MDD without psychosis (CI); MDD with psychosis > MDD without psychosis (SC) | |||
| Bora et al.10 | Cross-sectional and longitudinal (n = 30): Turkish-translated BCIS | 138 patients with schizophrenia: 77 inpatients, 61 outpatients | ▪ Clinical insight (r, BCIS, and SUMD total): CI = −.55; SR = −.56; SC = .28 |
| ▪ Symptoms (r, BCIS, and PANSS positive): CI = −.29; SR = −.24; SC = .29 | |||
| ▪ Symptoms (r, BCIS, and PANSS negative): SR = −.25 | |||
| ▪ Diagnostic and CI (means): psychotic symptoms (n = 93) < no psychotic symptoms (n = 45) | |||
| ▪ Posthospitalization: symptoms, SR, and CI improved; neither symptom change nor SUMD correlate with BCIS change | |||
| ▪ Demographic (r): BCIS unrelated to duration of illness, education, age, or hospitalizations | |||
| Buchy et al.27 | Cross-sectional: early intervention service | 70 first-episode patients: 39 schizophrenia, 9 schizoaffective, 1 schizophreniform, 8 psychosis NOS, 1 delusional disorder, 5 bipolar disorder, 3 undetermined | ▪ Symptoms (means): delusional > nondelusional (CI and SR); no difference (SC) |
| Buchy et al.29 | Cross-sectional: early intervention service | 61 first-episode patients: 37 schizophrenia, 9 schizoaffective disorder, 1 schizophreniform disorder, 7 psychosis NOS, 1 delusional disorder, 5 bipolar disorder, 1 undetermined | ▪ Neurocognition (r, BCIS, and verbal learning and memory): CI = .33; SR = .31 |
| ▪ Neuroanatomy: higher CI associated with greater volume of left-hemisphere hippocampus (r = .25); modest proportion of this relationship was attributable to verbal memory performance (partial r = .25, P = .06); greater SC correlated with smaller bilateral hippocampal volumes (r = −.34 for left and r = −.29 for right), independent of verbal memory performance; SR did not significantly correlate with hippocampal volume | |||
| ▪ No significant correlations between SUMD awareness of mental disorder scores and verbal memory or hippocampal volume | |||
| Carlson et al.13 | Cross-sectional + longitudinal (24–48 h, n = 93): Spanish-translated BCIS | 137 inpatients and outpatients with schizophrenia | ▪ Quality of life (Spanish version of Satisfaction with Life Domains Scale): no significant correlations |
| Colis et al.20 | Cross-sectional | 150 inpatients: 12 schizophrenia, 30 schizoaffective disorder, 52 bipolar disorder, 56 MDD | ▪ Reliability (alpha): SR = .73; SC = .70 |
| ▪ Diagnostic (means): MDD > psychotic (CI, d = .51) and bipolar (CI, d = .62); psychotic = bipolar (CI); bipolar last episode mania < bipolar patients last episode mixed or depressive (CI, d = .52) | |||
| ▪ Symptoms (r, BCIS, and anxiety and depression): CI and SR = .27 to .29 | |||
| Engh et al.11 | Cross-sectional: Norwegian-translated BCIS | 235 inpatients and outpatients: 143 schizophrenia spectrum (107 schizophrenia, 26 schizoaffective, 10 schizophreniform), 92 bipolar disorder, 64 healthy controls | ▪ Reliability (alpha): schizophrenia spectrum (SR = .72, SC = .63); bipolar (SR = .73, SC = .61); healthy controls (SR = .73, SC = .63) |
| ▪ Clinical insight (r, BCIS, and PANSS and schizophrenia spectrum): SR = −.21; SC = .38 | |||
| ▪ Diagnostic (means): no significant difference in SR or SC between 3 groups | |||
| ▪ Symptoms (r): SC correlated with mania in schizophrenia-spectrum group | |||
| ▪ Hospitalization (means): inpatients = outpatients (SR and SC, schizophrenia spectrum, n = 78) | |||
| Engh et al.26 | Cross-sectional: Norwegian-translated BCIS | 143 inpatients and outpatients: 107 schizophrenia, 26 schizoaffective, 10 schizophreniform | ▪ Delusions (PANSS ≥ 4; means): delusions < no delusions (CI and SR); delusions > no delusions (SC); both independent of hallucinations |
| ▪ Hallucinations (PANSS ≥ 4; means): nonhallucinators = hallucinators (CI, SR, or SC); delusional hallucinators have lower SR and higher SC than nondelusional hallucinators | |||
| Favrod et al.12 | Cross-sectional: French-translated BCIS | 158 outpatients: 132 schizophrenia, 26 schizoaffective | ▪ Factor analysis (confirmatory): good fit for original 2-factor solution. |
| ▪ Reliability (alpha): SR = .73; SC = .62 | |||
| ▪ Clinical insight (r, BCIS, and PANSS): CI = −.42; SR = −.37; SC = .29. | |||
| ▪ Symptoms (r, BCIS, and PANSS): no significant correlations | |||
| ▪ Functioning (means): nursing home < living independently (CI and SR); nursing home > living independently (SC) | |||
| Granholm et al.34 | Randomized controlled trial: CBSST vs. TAU | 32 middle-aged and older outpatients with chronic schizophrenia or schizoaffective | ▪ CBSST (r, CI change, and PANSS change): positive symptoms = −.40; negative symptoms = −.41; total symptoms r = −.45 |
| ▪ Depression, psychosocial functioning (r): not associated with change in CI | |||
| ▪ Participation in treatment associated with increase in cognitive insight (R2 = .29). | |||
| Granholm et al.32 | Randomized controlled trial of CBSST vs. TAU | 76 middle-aged and older outpatients: 48 schizophrenia, 28 schizoaffective | ▪ Treatment effect (CI): CBSST > TAU (η2 = .12). |
| ▪ Positive symptom reduction (r, BCIS, and PANSS): CI = −.38; SR = −.36 | |||
| ▪ Midtreatment increase in depression (r): CI = .32: SC = −.59 | |||
| Kao and Liu19 | Cross-sectional + longitudinal (4 weeks, N = 30) | 60 schizophrenia or schizoaffective; 60 MDD without psychotic features; 60 healthy controls | ▪ Factor analysis (exploratory): 2 factors (SR and SC), 4 items load (2 for each scale) on other factor than in the other studies |
| ▪ Researchers used their own factor analysis solution for correlational findings, rendering the results not useful for the present review | |||
| Kim et al.14 | Cross-sectional: Korean-translated BCIS | 78 patients (50 outpatients and 28 inpatients): 72 schizophrenia, 4 schizoaffective, 2 other psychotic disorder | ▪ Factor analysis (principal components): confirmed 2-factor structure |
| ▪ Reliability (alpha): SR = .64; SC = .75 | |||
| ▪ Reliability (r, test-retest): CI = .61 | |||
| ▪ Clinical insight (r, BCIS, and Revised Insight Scale for Psychosis): SR = .53; CI = .51 | |||
| ▪ Symptoms, functioning (r): no significant correlations | |||
| Lepage et al.21 | Cross-sectional: early intervention service | 51 first-episode outpatients: 30 schizophrenia, 7 schizoaffective, 1 schizophreniform, 5 psychosis NOS, 1 delusional disorder, 3 bipolar disorder, 4 unknown | ▪ Clinical insight (r): CI and PANSS = −.39; CI and SUMD awareness of mental illness = −.39 |
| ▪ Neurocognition (r, BCIS, and verbal learning and memory): CI = .32; SC = −.30 | |||
| ▪ Neurocognition (r, PANSS, and SUMD): no significant correlations | |||
| ▪ Full Scale IQ (r): None of the 3 insight measures correlated significantly | |||
| Lysaker et al.36 | Cross-sectional: chronic, postacute phase | 49 male outpatients: 29 schizophrenia, 20 schizoaffective | ▪ Metacognition (rho, BCIS, and Metacognition Assessment Scale): CI and “understanding one's own mind” = .43 |
| Mak and Wu9 | Cross-sectional: Chinese-translated BCIS | 162 outpatients with schizophrenia “or other psychotic disorder” | ▪ Reliability (alpha): SC = .71; SR = .82 |
| ▪ Self-stigma: CI adds 4% to variance explained; higher insight predicts greater self-stigma | |||
| Martin et al.18 | Cross-sectional + longitudinal (45 min, N = 23) | 55 schizophrenia, 38 schizoaffective, 418 nonpsychiatry controls | ▪ Factor analysis (confirmatory): 2-factor structure fits better than 1-factor structure |
| ▪ Reliability (alpha): CI = .76; SR = .74; SC = .75 | |||
| ▪ Reliability (test-retest): CI = .87; SR = .77; SC = .86 | |||
| ▪ Diagnostic (means): patients < control (CI, η2 = .037); patients < control (SR, η2 = .011); patients > control (SC, η2 = .021) | |||
| Pedrelli et al.16 | Cross-sectional | 164 middle-aged and older chronic outpatients: 119 schizophrenia, 45 schizoaffective | ▪ Factor analysis (confirmatory): supported validity of 2-factor structure |
| ▪ Reliability (alpha): CI = .66; SC = .55; SR = .70 | |||
| ▪ Clinical insight (r, BIS): CI and BIS total = .24; CI and BIS relabel = .30; SR and BIS total = .26; SR and BIS relabel = .36 | |||
| ▪ Symptoms (r, PANSS): SC and positive = .24; SC and negative = .19; SC and total = .21; CI and cognitive = −.18 | |||
| Penn et al.31 | Randomized controlled trial: CBT vs. ST | 65 outpatients: 32 schizophrenia, 33 schizoaffective | ▪ Treatment effect on CI: CBT > ST (d = .43, P = .11) |
| Perivoliotis et al.30 | Longitudinal: community CBT clinic | 141 outpatients: 51 schizophrenia, 6 schizoaffective, 11 psychotic NOS, 5 delusional disorder, 2 bipolar, 1 MDD with psychosis, 1 schizotypal, 1 somatoform disorder | ▪ Moderation of symptom reduction (r, BCIS, and PANSS delusions): CI = −.26; SR = −.23 |
| ▪ Gains in cognitive insight during CBT predict symptom reduction (r, BCIS, and PANSS): CI and delusions = −.36; CI and hallucinations = −.40; SR and delusions = −.33; SR and hallucinations = −.28; SC and delusions = .26; SC and hallucinations = .30 | |||
| ▪ Clinically significant symptom reduction: delusions, greater gains in SR and CI; hallucinations, greater reductions in SC and gains in CI | |||
| Tranulis et al.17 | Cross-sectional | 38 first-episode outpatients: 19 schizophrenia, 19 schizoaffective, bipolar with psychosis, delusional disorder, or psychosis NOS | ▪ SR and SC not significantly intercorrelated, supporting 2-factor structure |
| ▪ Clinical insight (r, BCIS, PANSS, and SUMD): SR correlated negatively with both | |||
| ▪ Symptoms (r, BCIS, and PANSS): SR and negative symptoms = −.41; no significant correlations with positive, general, or total symptoms | |||
| Uchida et al.15 | Cross-sectional: Japanese-translated BCIS | 30 inpatients (schizophrenia or schizoaffective), 183 healthy controls (university students) | ▪ Factor analysis (principal components): confirmed original 2-factor structure |
| ▪ Reliability (alpha): SC = .78; SR = .67 | |||
| ▪ Reliability (test-retest, ICC): CI = .82; SC = .79; SR = .86 | |||
| ▪ Clinical insight (r, BCIS, and Japanese Schedule for the Assessment of Insight): CI = .50; SR = .52 | |||
| ▪ Clinical insight (r, BCIS, and PANSS): CI = −.45; SR = −.39 | |||
| ▪ Symptoms (r, BCIS, and BDI-II): CI = .42; no correlations with PANSS symptoms | |||
| ▪ Demographics (r): CI and age = −.47; SR and age = −.37; SC and duration of illness = .46 | |||
| Warman and Martin25 | Cross-sectional | 200 healthy controls (university students without history of psychotic illness) | ▪ Participants with higher delusion proneness showed higher SC and SR |
| Warman et al.24 | Cross-sectional | 49 outpatients with schizophrenia or schizoaffective disorder, 60 healthy controls (university students without history of psychotic illness) | ▪ Diagnostic (means): patients < controls (CI, η2 = .07); patients > controls (SC, η2 = .06); delusional = nondelusional < controls (CI); delusional > nondelusional = control (SC); nondelusional < delusional = control (SR) |
| ▪ Symptoms (r, BCIS, and BDI-II): CI = .20; SR = .19 |
Note: MDD, major depressive disorder; SR, Self-reflectiveness subscale of BCIS; SC, Self-certainty subscale of BCIS; SUMD, Scale to Assess Unawareness of Mental Disorder; CI, Composite Index of BCIS (self-reflectiveness minus self-certainty); PANSS, Positive and Negative Syndrome Scale; CBSST, Cognitive Behavioral Social Skills Training; BIS, Birchwood Insight Scale; CBT, Cognitive Behavior Therapy; TAU, Treatment as Usual; ST, supportive therapy; BDI-II, Beck Depression Inventory II; NOS, Not Otherwise Specified.
Factor Structure
Seven studies have confirmed the 2-factor structure of the BCIS.12,14–19 While the original article established a 2-factor solution for inpatients, the new studies have replicated this finding14 and shown that the same solution fits outpatient,12,16 first-episode,17 and healthy control15,18 samples, both in English16–18 and non-English12,14,15,19 speakers. These studies have, additionally, employed differing analytic strategies: principle components factor analysis,14,15 confirmatory factor analysis,12,16,18 exploratory factor analysis,19 and correlational analysis.17
Reliability and Validity
Internal Consistency.
Eight studies9,11,12,14–16,18,20 have attempted to replicate the internal consistency findings of Beck et al.;7 6 showed internal consistency for the Self-Reflectiveness subscale greater than or equal to .7 (Cronbach's alpha),9,11,12,16,18,20 with all 8 scoring above .6. Five showed internal consistency for the Self-Certainty subscale greater than or equal to .7,9,14,15,18,20 with an additional 2 scoring between .6 and .7.11,12
Test-Retest Reliability.
Three studies have reported on test-retest reliability of the BCIS.14,15,18 Test-retest was adequate to good in all 3 studies, the correlation being greater than .6 for a 3-month delay in schizophrenia patients,14 greater than .77 for healthy controls over a 45-min delay, and greater than .79 for healthy controls over an undisclosed delay.15
Construct Validity.
Convergent validity has been determined by correlating the BCIS with 5 different measures of clinical insight. Two groups have replicated the finding of Beck et al. that the Composite Index correlated with the SUMD, finding moderate-to-large correlations with the Awareness of a Mental Illness item21 and the total score.10 Five studies11,12,15,17,21 have reported significant mild-to-moderate correlations between the BCIS and Positive and Negative Syndrome Scale (PANSS) Lack of Insight item.22 Similarly, the BCIS has shown significant mild-to-moderate correlations with the Birchwood Insight Scale,16,23 the Schedule for Assessment of Insight (Japanese version), and the Revised Insight Scale for Psychosis.14 One group of researchers has reported divergent validity because they predicted and found that the BCIS did not correlate with a measure of subjective well-being.13
Criterion Validity.
The BCIS has been shown to distinguish between individuals with a psychotic diagnosis and healthy controls. Two studies have reported patients scoring significantly higher than healthy controls on Self-Certainty, though Self-Reflectiveness did not distinguish the 2 groups in either study.11,24 However, in the largest study of this kind, healthy controls had higher Self-Reflectiveness, lower Self-Certainty, and a higher Composite Index than patients with schizophrenia.18 Finally, the BCIS has also been shown to distinguish healthy individuals who are delusion-prone from those who are not: The delusion-prone subjects scored higher on self certainty than their nondelusion-prone counterparts, though, contrary to hypothesis, they showed higher Self-Reflectiveness.25 It seems likely that the failure of the earlier studies to find differences between patients and controls on Self-Reflectiveness can be attributable to insufficient sample size11,24 and differences in translation of items related to unusual experiences.11
Importantly, the BCIS has been shown to distinguish between psychotic and nonpsychotic patient groups because the original finding of Beck et al.7 has been replicated20 and extended by showing that patients experiencing psychosis had lower cognitive insight than patients not experiencing psychosis.10 However, 2 research groups have found little difference on the BCIS between their schizophrenia and bipolar patients.11,20
Cognitive Insight and Psychopathology
Beck and Warman6 have theorized that delusional thinking, in particular, should be related to cognitive insight because low Self-Reflectiveness and high Self-Certainty constitute a reasoning style that would maintain delusional beliefs. Conversely, patients who evidence more Self-Reflectiveness and less Self-Certainty are less intellectually rigid, are more open to alternative explanations for their experiences, and are predicted to be less delusional. Several research groups have employed cross-sectional methodology to investigate the correlation of cognitive insight to delusions, as well as the other characteristic signs and symptoms of schizophrenia.
Positive Symptoms
As a first pass at the hypothesis of Beck and Warman,6 5 studies have reported correlations between the BCIS and the PANSS positive symptoms score. Three did not find any significant correlations,12,15,17 2 studies reported significant positive correlations for Self-Certainty,10,16 and 1 reported significant negative correlations for the Composite Index and Self-Reflectiveness.10
Delusions.
The hypothesis of Beck and Warman6 that patients with active delusions have lower Self-Reflectiveness and higher Self-Certainty than patients without delusions has been supported in both chronic26 and first-episode27 (Self-Certainty was a nonsignificant trend) patients. One group has reported a mixed finding, such that patients with delusions have higher Self-Certainty and, contrary to prediction, higher Self-Reflectiveness.24
Hallucinations.
Because hallucinations are prototypical unusual experiences, patients with poor cognitive insight might be expected to have worse hallucinations because the severity of auditory hallucinations has been linked to patients' beliefs about their “voices.”28 One published study has addressed this hypothesis: While severity of hallucinations, in general, was not associated with the BCIS, delusional hallucinators demonstrated lower Self-Reflectiveness and higher Self-Certainty (at a trend level) than nondelusional hallucinators.26 This finding further supports the link between cognitive insight and delusions.
Negative Symptoms
The reduced expressivity and withdrawal from constructive activity characteristic of negative symptoms would not seem like obvious correlates of cognitive insight. Nonetheless, 3 research groups have reported significant correlations with PANSS negative symptoms, 2 finding an inverse relationship with Self-Reflectiveness,10,17 and 1 finding a direct relationship with Self-Certainty.16 Three studies also failed to find a significant correlation between the BCIS and negative symptoms.11,12,15
Depression and Anxiety
The literature on cognitive insight and depression appears mixed. Four studies have replicated the finding of Beck et al.7 that depression does not correlate with cognitive insight in patients with a psychotic diagnosis.11,12,16,17 However, 2 studies have reported partially contrary findings: In each case, higher Self-Reflectiveness (but not Self-Certainty) was associated with depression in psychotic patients.20,24 Two studies have investigated the association between anxiety and cognitive insight in psychosis, and the results are similar to depression, with one group finding no significant associations29 and the other finding significant positive correlations between anxiety and both the Composite Index and Self-Reflectiveness.20
Applications of Cognitive Insight
Cognitive Insight and Treatment
Given that the literature supports a link between cognitive insight and psychopathology (especially delusions), further questions can be posed regarding possible relationships between cognitive insight and treatment: (a) Is cognitive insight a predictor (moderator) of treatment response? (b) Can cognitive insight be improved in treatment? and (c) Is cognitive insight a mediating variable of treatment outcome? A small literature has begun to address these questions.
Predictor of Favorable Outcome.
To our knowledge, only 1 published study has reported on the prognostic utility of cognitive insight.30 In a naturalistic study, patients with higher cognitive insight at the start of therapy showed a greater reduction in delusion severity at the end of treatment (8 months later) relative to patients who started treatment with poorer cognitive insight.
Improvement in Treatment.
Four published studies have found that cognitive insight improves over the course of psychosocial treatment. These were 2 group intervention studies,31,32 1 individual therapy study30 and 1 multifaceted inpatient treatment study.10 Across all these studies, Self-Reflectiveness appeared to change more by the end of treatment than Self-Certainty.10,32
Mediating Variable.
While a proper mediation analysis33 has not, to our knowledge, been conducted with the BCIS, there are 2 suggestive findings. In the first, improvements in the Composite Index significantly correlated with reductions in positive, negative, and total symptoms,34 while the second showed that improvements in Self-Reflectiveness, Self-Certainty, and the Composite Index score were significantly correlated with concomitant reductions in the severity of both delusions and hallucinations.30 While these findings are consistent with cognitive insight being a mediating variable in the treatment of psychotic symptoms, future studies should conduct a true mediation analysis using sufficient measurement points.35
Functional Outcome
One study has addressed whether cognitive insight is related to poor social and vocational functioning: patients living on their own were found to have a significantly higher Composite Index, higher Self-Reflectiveness, and lower Self-Certainty than patients living in nursing homes.12
Cognitive Insight, Neurocognition, and Neurobiology
Recently, investigators have begun to include the BCIS in studies of information processing and neuroimaging. Three studies have been published. In the first, cognitive insight was associated with executive function and understanding one's own mind, suggesting the involvement of neurocognitive and metacognitive processes.36 Similarly, another group of researchers has shown that the neurocognitive domains of verbal learning and memory, as well as attention, were significantly correlated with Composite Index and Self-Certainty; the Composite Index, additionally, was associated with social cognition; and neither the SUMD nor the PANSS correlated with neurocognitive or social cognitive measures.21 A second study by this group largely corroborated these findings, with the exception that Self-Reflectiveness (rather than Self-Certainty) correlated with verbal memory.29 This last study was also the first to report brain imaging results. Specifically, a smaller overall hippocampal volume was associated with higher Self-Certainty, and reduced left-hemisphere hippocampal volume also correlated with a lower Composite Index score. These researchers found no significant correlations between Self-Reflectiveness and total hippocampal volume or between clinical insight (ie, SUMD) and brain volume. Further, the significant associations between cognitive insight and hippocampal volume were independent of verbal memory performance.29
Summary and Future Directions
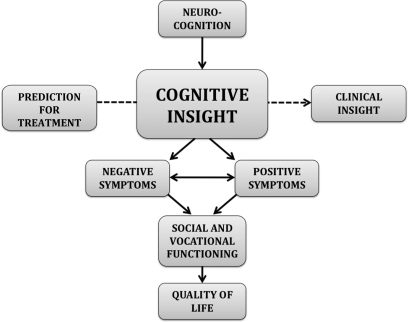
The literature on the BCIS is still at an early stage. Nonetheless, the weight of the evidence supports the conclusion that the BCIS has favorable psychometric properties and is a useful measure for both clinical and research purposes. Figure 1 represents a synthesis of the basic findings into a theoretical model to serve as a template for future research of the BCIS.
Fig. 1.
Theoretical and Empirical Model of Cognitive Insight in Schizophrenia: Template for Present and Future Research.
Scale
Psychometrically, the BCIS has been found to consist of 2 internally consistent factors; the scale is stable across time; it shows convergent validity with measures of clinical insight; and, importantly, it distinguishes patients with psychotic disorders from healthy controls and patients with nonpsychotic disorders. We make the following proposals for future research:
Researchers might consider other means for determining the aggregate cognitive insight score. The original study of Beck et al.7 opted for straight subtraction (Self-Reflectiveness - Self-Certainty); however, the use of a ratio (Self-Reflectiveness/Self- Certainty) might capture more of the richness of the cognitive insight construct, especially because it relates to neurocognitive and neurobiological variables (this would require scoring each item on a 1 [do not agree at all] to 4 [agree completely] scale, rather than 0 to 3).
Additionally, it would be useful for researchers to determine normative scores for the BCIS that define poor cognitive insight.
Investigators ought to compare BCIS differences in bipolar disorder with and without psychotic features. Given that bipolar disorder patients whose last episode was manic had lower cognitive insight than those whose episode was mixed or depressive,20 we propose that patients with mania may also have a lack of cognitive flexibility, in which case both patients with and without psychotic features would demonstrate impaired BCIS scores.
Neurocognition and Neuroanatomy
The neurocognitive findings suggest that deficiency in cognitive insight is related to impairment of basic neurocognitive functions such as verbal memory, attention, and mental flexibility. In figure 1, the arrow from neurocognition to cognitive insight represents the hypothesis that neurocognitive impairment limits cognitive insight. However, this link is based on 3 studies.21,29,36 The neuroanatomical finding is also promising, especially the link between hippocampal volume and Self-Certainty. We anticipate considerable growth in this area of study in the coming years and, accordingly, make the following proposals for future research:
In information processing terms, Self-Reflectiveness should involve working memory and executive functions, both of which have been shown to be components of attention.37 Patients who have difficulty with abstraction and holding mental content in mind should show lower Self-Reflectiveness than patients with better facility in these functions. We expect, further, that frontal circuits will mediate Self-Reflectiveness.
Self-Certainty is a process that is akin to a prejudice in favor of the products of one's own mind. It might be produced by a combination of emotional processes and processes that minimize the deployment of effort; as such, we expect it to correlate with measures of emotion processing,38 general indexes of neurocognition,39 and measures of conservation of effort (eg, attenuated pupillary responses).40 We expect that amygdala circuits will mediate Self-Certainty.
In high-risk research, cognitive impairment is evident prior to the onset of the illness.41 It would be fruitful to determine if cognitive insight is also impaired prodromally. We hypothesize that cognitive insight will be a contributing factor in the transition to psychosis.
Clinical Insight
While the literature shows that cognitive insight consistently correlates with clinical insight, there is evidence that the 2 constructs are “complementary” rather than “overlapping.” For example, cognitive insight taps capacities rather than pathology and therefore may be a better indicator of prognosis. Indeed, it has already shown to be a good marker for prognosis in Cognitive Therapy for psychosis.30 Further evidence of a complementary relationship between clinical insight and cognitive insight comes from the studies showing the BCIS, and not the SUMD, to be associated with neurocognitive and neurobiological factors.21,29,36 These findings suggest that cognitive insight is a basic ability that is more proximal to neurobiological vulnerabilities than clinical insight. The development of adequate clinical insight may therefore depend upon a certain degree of cognitive insight—eg, neurocognitive deficits may limit a patient's ability to consider alternative viewpoints and refrain from thinking that is impermeable to outside information, which may in turn limit the patient's ability to understand that he or she has an illness. We have represented the complementary relationship between clinical and cognitive insight with a dashed arrow in the middle of figure 1. We make the following suggestions for future research:
It would be interesting for clinical trials of biological and psychosocial treatments to employ both the BCIS and a measure of clinical insight, such as the SUMD. Researchers could then perform prognostic and mediational analyses to determine the relative contribution of both forms of insight to treatment response in patients with psychosis. We predict that a change in cognitive insight will predict subsequent change in clinical insight. However, it is also possible that clinical insight will mediate between cognitive insight and functional outcomes.
It is hoped that future researchers might employ longitudinal designs in which neurocognition, neurobiology, clinical insight, and cognitive insight are all included. Such designs might help to elucidate what cognitive insight adds to the understanding of patients with psychosis above and beyond the other factors.
Symptoms
The central portion of figure 1 illustrates the links between cognitive insight and the characteristic symptoms of schizophrenia. However, the direction of the arrows between these variables is hypothetical because the necessary longitudinal research has yet to appear.
Positive Symptoms.
The review supports, at most, a weak association between a general index of positive symptoms and the BCIS. There is stronger evidence for the association of delusions and the BCIS26,27 and one study implicating the BCIS in hallucinations.26 The clinical research showing that change in cognitive insight is correlated with change in hallucinations and delusions also buttresses the link between the BCIS and positive symptoms.30 Our recommendations for future research are as follows:
It would be useful for future studies to report summary scores as well as scores for specific psychotic symptoms because there is evidence that specific symptoms may show relationships that are obscured by composite symptom scores in patients with schizophrenia.42
We hypothesize that cognitive insight captures mental processes that participate in the development and maintenance of delusions, but experimental studies are needed to explore this relationship.
The inconsistency regarding Self-Reflectiveness in patients with “active delusions” might be resolved if studies only included patients with moderate-to-severe delusions in this category. The study that found elevated Self-Reflectiveness was the only one to include patients in the “active delusions” group who were rated 3 (mild) on the PANSS delusion item; the criteria for this rating incorporate elements of questioning the delusion, so the rating is consistent with higher Self-Reflectiveness.
Given that beliefs about the origin of hallucinations (eg, implanted chip and spirits) can come from the delusional spectrum, we propose the hypothesis that patients with verbal auditory hallucinations and poor cognitive insight are particularly likely to endorse delusional explanations for voice hearing. Specifically, we predict that lack of Self-Reflectiveness contributes to beliefs about hallucinations—in particular, beliefs that the voices are externally generated, credible sources of information, and powerful enough to be obeyed.28 This hypothesis can be tested by assessing hallucinations with instruments such as the Beliefs About Voices Questionnaire, Revised.43
Negative Symptoms.
The present review supports a tentative link between cognitive insight and negative symptoms. We theorize 2 possible paths underlying this association, as represented in figure 1. First, cognitive insight may impact negative symptoms directly via a rigid reasoning style that fosters disengagement in constructive activity as well as reduced interpersonal expressivity. However, the pathway may be indirect, such that cognitive insight affects positive symptoms, which in turn lead the patients to withdraw from productive pursuits (eg, command hallucination tells the patient to lie down for hours). Our proposals for future research are as follows:
The inconsistent findings between the BCIS and negative symptoms could result from some studies having a disproportionate number of patients with negative symptoms that are secondary to delusions. It would be informative, in this regard, to conduct a study in which Deficit Syndrome44 and Non-Deficit Syndrome patients are compared on the BCIS. Because the Deficit patients have primary negative symptoms that are not secondary to positive symptoms, they are an ideal group to test for a direct relationship between negative symptoms and cognitive insight. If, as we hypothesize, Deficit patients have worse cognitive insight than Non-Deficit patients, this would support the direct link between cognitive insight and negative symptoms. We hypothesize, further, when compared with Non-Deficit patients, Deficit patients will score higher in Self-Certainty because Deficit patients have been shown to be intellectually rigid and to have worse clinical insight.45
All studies have correlated the BCIS with a summary score (the PANSS) for negative symptoms. It would be useful for future investigations to report correlations between the specific negative symptoms and the BCIS because another source of the inconsistency in the literature could be disproportionate inclusion of patients experiencing particular negative symptoms. Based upon clinical experience, we hypothesize that alogia and blunted affect, in particular, will be associated with poor cognitive insight.
Depression and Anxiety.
While the aggregate literature supports a null relationship between depression and the BCIS in patients with psychotic disorders, there are 2 inconsistent findings that show elevated Self-Reflectiveness associated with elevated depression. A similar finding has been reported between anxiety and the BCIS. We make the following proposals:
Two additional findings are potentially relevant to the paradoxical results for cognitive insight and depression: (a) In patients with major depressive disorder, greater cognitive insight was associated with higher depression levels;7 and, (b) in a group intervention study, increased depression was significantly correlated with increased cognitive insight midtreatment but not at the end of treatment.32 Because patients with depression are characterized by a variety of negative biases about the self,46 we propose that the elevated Self-Reflectiveness in such patients is an indication of “bad me” distortions of thinking.47 It would be fruitful for future investigations to explore BCIS responding in patients with depression to test this proposition.
We also propose that the finding of higher Self-Reflectiveness in persons who are delusion prone25 might reflect elevated depression relative to persons who are not delusion-prone because depression is a risk factor for psychosis in high-risk individuals.48 Inclusion of measures of depression in future studies of the BCIS in healthy individuals would allow the test of this proposition.
Future investigations of the BCIS would also benefit from the inclusion of measures of anxiety, especially as anxiety has emerged as an important correlate of psychosis.49 Again, we propose that a “bad me” schema may lead to elevated Self-Reflectiveness in depressed psychotic patients. We, accordingly, expect depression and anxiety to be correlated for these patients, such that anxiety does not pick up any extra variability in Self-Reflectiveness.
Functional Outcome
Patients with higher cognitive insight are more likely to be living independently.12 Further, the relationship between cognitive insight and both metacognition and social cognition suggests that it might also affect social information processing and interpersonal interactions. Does cognitive insight impact acts of daily living directly or is the relationship best characterized as indirect, and secondary, to symptoms? The figure features an indirect path. Additionally, the relationship between quality of life and cognitive insight is relatively unexplored. Figure 1 contains an arrow from functional outcome to quality of life, reflecting the idea that patients who are functioning better will also report higher life satisfaction.
Only 1 study has reported on functional outcome,12 and it would be useful to include cognitive insight in studies of functional outcome to determine if this finding is replicable and extendable. We propose that better social and vocational status should be associated with higher Self-Reflectiveness and lower Self-Certainty.
We suggest that the link between functional outcome and BCIS is indirect. Testing this hypothesis requires a longitudinal study that includes neurocognition, cognitive insight, clinical insight, symptoms, and functional outcome. We predict that cognitive insight will account for unique variability in functional outcome above and beyond the other factors. It would be interesting to see if cognitive insight mediates between neurocognition and functional outcome and whether symptoms (either delusions or negative symptoms) mediate between cognitive insight and functional outcome.
Funding
Foundation for Cognitive Therapy and Research; Heinz Foundation.
Acknowledgments
The authors thank Letitia Travaglini, Nadine Chang, Jessica Olli, Gloria Huh, and Daniel Himelstein for assistance in preparation of the manuscript. The Authors have declared that there are no conflicts of interest in relation to the subject of this study.
Appendix: BCIS
Response choices are “do not agree at all,” “agree slightly,” “agree a lot,” and “agree completely”
At times, I have misunderstood other people's attitudes towards me.
My interpretations of my experiences are definitely right.
Other people can understand the cause of my unusual experiences better than I can.
I have jumped to conclusions too fast.
Some of my experiences that have seemed very real may have been due to my imagination.
Some of the ideas I was certain were true turned out to be false.
If something feels right, it means that it is right.
Even though I feel strongly that I am right, I could be wrong.
I know better than anyone else what my problems are.
When people disagree with me, they are generally wrong.
I cannot trust other people's opinion about my experiences.
If somebody points out that my beliefs are wrong, I am willing to consider it.
I can trust my own judgment at all times.
There is often more than one possible explanation for why people act the way they do.
My unusual experiences may be due to my being extremely upset or stressed.
References
- 1.Haslam J. Illustrations of Madness. New York, NY: Routelidge; 1811. [Google Scholar]
- 2.Jaspers K. General Psychopathology. Manchester, UK: Manchester University Press; 1913/1953. [Google Scholar]
- 3.Lewis A. The psychopathology of insight. Br J Med Psychol. 1934;14:332–348. [Google Scholar]
- 4.Mintz AR, Dobson KS, Romney DM. Insight in schizophrenia: a meta-analysis. Schizophr Res. 2003;61:75–88. doi: 10.1016/s0920-9964(02)00316-x. [DOI] [PubMed] [Google Scholar]
- 5.Amador XF, Kronengold H. Understanding and assessing insight. In: Amador XF, David AS, editors. Insight and Psychosis: Awareness of Illness in Schizophrenia and Related Disorders. 2nd ed. Oxford, UK: Oxford University Press; 2004. pp. 3–30. [Google Scholar]
- 6.Beck AT, Warman DM. Cognitive insight: theory and assessment. In: Amador XF, David AS, editors. Insight and Psychosis: Awareness of Illness in Schizophrenia and Related Disorders. 2nd ed. New York, NY: Oxford University Press; 2004. pp. 79–87. [Google Scholar]
- 7.Beck AT, Baruch E, Balter JM, Steer RA, Warman DM. A new instrument for measuring insight: the Beck Cognitive Insight Scale. Schizophr Res. 2004;68:319–329. doi: 10.1016/S0920-9964(03)00189-0. [DOI] [PubMed] [Google Scholar]
- 8.Amador XF, Strauss DH, Yale SA, Flaum MM, Endicott J, Gorman JM. Assessment of insight in psychosis. Am J Psychiatry. 1993;150:873–879. doi: 10.1176/ajp.150.6.873. [DOI] [PubMed] [Google Scholar]
- 9.Mak WWS, Wu CFM. Cognitive insight and causal attribution in the development of self-stigma among individuals with schizophrenia. Psychiatr Serv. 2006;57:1800–1802. doi: 10.1176/ps.2006.57.12.1800. [DOI] [PubMed] [Google Scholar]
- 10.Bora E, Erkan A, Kayahan B, Veznedaroglu B. Cognitive insight and acute psychosis in schizophrenia. Psychiatry Clin Neurosci. 2007;61:634–639. doi: 10.1111/j.1440-1819.2007.01731.x. [DOI] [PubMed] [Google Scholar]
- 11.Engh JA, Friis S, Birkenaes AB, et al. Measuring cognitive insight in schizophrenia and bipolar disorder: a comparative study. BMC Psychiatry. 2007;7:71–77. doi: 10.1186/1471-244X-7-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Favrod J, Zimmermann G, Raffard S, Pomini V, Khazaal Y. The Beck Cognitive Insight Scale in outpatients with psychiatric disorders: further evidence from a French-speaking sample. Can J Psychiatry. 2008;53:783–787. doi: 10.1177/070674370805301111. [DOI] [PubMed] [Google Scholar]
- 13.Carlson J, Ochoa S, Haro JM, et al. Adaptation and validation of the quality-of-life scale: satisfaction with Life Domains Scale by Baker and Intaglita. Compr Psychiatry. 2009;50:76–80. doi: 10.1016/j.comppsych.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 14.Kim HJ, Jhin HK, Chung EK, Chang D, Lee J. Cross-cultural validation of the Beck Cognitive Insight Scale in Korean. Psychiatry Invest. 2007;4:109–115. [Google Scholar]
- 15.Uchida T, Matsumoto K, Kikuchi A, et al. Psychometric properties of the Japanese version of the Beck Cognitive Insight Scale: relation of cognitive insight to clinical insight. Psychiatry Clin Neurosci. 2009;63:291–297. doi: 10.1111/j.1440-1819.2009.01946.x. [DOI] [PubMed] [Google Scholar]
- 16.Pedrelli P, McQuaid JR, Granholm E, et al. Measuring cognitive insight in middle-aged and older patients with psychotic disorders. Schizophr Res. 2004;71:297–305. doi: 10.1016/j.schres.2004.02.019. [DOI] [PubMed] [Google Scholar]
- 17.Tranulis C, Lepage M, Malla A. Insight in first episode psychosis: who is measuring what? Early Interv Psychiatry. 2008;2:34–41. doi: 10.1111/j.1751-7893.2007.00054.x. [DOI] [PubMed] [Google Scholar]
- 18.Martin JM, Warman DM, Lysaker PH. Cognitive insight in non-psychiatric individuals and individuals with psychosis: an examination using the Beck Cognitive Insight Scale. Schizophr Res. doi: 10.1016/j.schres.2010.03.028. In press. [DOI] [PubMed] [Google Scholar]
- 19.Kao Y-C, Liu Y-P. The Beck Cognitive Insight Scale (BCIS): translation and validation of the Taiwanese version. BMC Psychiatry. 2010;10:27. doi: 10.1186/1471-244X-10-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Colis MJ, Steer RA, Beck AT. Cognitive insight in inpatients with psychotic, bipolar, and major depressive disorders. J Psychopathol Behav Assess. 2006;28:242–249. [Google Scholar]
- 21.Lepage M, Buchy L, Bodnar M, Bertrand M-C, Joober R, Malla A. Cognitive insight and verbal memory in first episode psychosis. Eur Psychiatry. 2008;23:368–374. doi: 10.1016/j.eurpsy.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 22.Kay SR, Fiszbein S, Opler LA. The Positive And Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 23.Birchwood M, Smith J, Drury V, Healy J, Macmillan F, Slade M. A self-report insight scale for psychosis: reliability, validity and sensitivity to change. Acta Psychiatr Scand. 1994;89:62–67. doi: 10.1111/j.1600-0447.1994.tb01487.x. [DOI] [PubMed] [Google Scholar]
- 24.Warman DM, Lysaker PH, Martin JM. Cognitive insight and psychotic disorder: the impact of active delusions. Schizophr Res. 2007;90:325–333. doi: 10.1016/j.schres.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 25.Warman DM, Martin JM. Cognitive insight and delusion proneness: an investigation using the Beck Cognitive Insight Scale. Schizophr Res. 2006;84:297–304. doi: 10.1016/j.schres.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 26.Engh JA, Friis S, Birkenaes AB, et al. Delusions are associated with poor cognitive insight in schizophrenia. Schizophr Bull. 2010;36:830–835. doi: 10.1093/schbul/sbn193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Buchy L, Malla A, Joober R, Lepage M. Delusions are associated with low self-reflectiveness in first-episode psychosis. Schizophr Res. 2009;112:187–191. doi: 10.1016/j.schres.2009.03.019. [DOI] [PubMed] [Google Scholar]
- 28.Beck AT, Rector NR, Stolar NM, Grant PM. Schizophrenia: Cognitive Theory, Research and Therapy. New York, NY: Guilford Press; 2009. [Google Scholar]
- 29.Buchy L, Czechowska Y, Chochol C, et al. Toward a model of cognitive insight in first-episode psychosis: verbal memory and hippocampal structure. Schizophr Bull. doi: 10.1093/schbul/sbp015. 2010;36:1040–1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Perivoliotis D, Grant PM, Peters ER, Ison R, Kuipers E, Beck AT. Cognitive insight predicts favorable outcome in cognitive behavioral therapy for psychosis. Psychosis. 2010;2:23–33. [Google Scholar]
- 31.Penn DL, Meyer PS, Evans E, Wirth RJ, Cai K, Burchinal M. A randomized controlled trial of group cognitive-behavioral therapy vs. enhanced supportive therapy for auditory hallucinations. Schizophr Res. 2009;109:52–59. doi: 10.1016/j.schres.2008.12.009. [DOI] [PubMed] [Google Scholar]
- 32.Granholm E, McQuaid J, McClure F, et al. A randomized, controlled trial of cognitive behavioral social skills training for middle-aged and older outpatients with chronic schizophrenia. Am J Psychiatry. 2005;162:520–529. doi: 10.1176/appi.ajp.162.3.520. [DOI] [PubMed] [Google Scholar]
- 33.Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- 34.Granholm E, Auslander LA, Gottlieb JD, McQuaid JR, McClure FS. Therapeutic factors contributing to change in cognitive-behavioral group therapy for older persons with schizophrenia. J Contemp Psychother. 2006;36:31–41. [Google Scholar]
- 35.Gelfand LA, Mensinger JL, Tenhave T. Mediation analysis: a retrospective snapshot of practice and more recent directions. J Gen Psychol. 2009;136:153–178. doi: 10.3200/GENP.136.2.153-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lysaker PH, Warman DM, Dimaggio G, et al. Metacognition in schizophrenia: associations with multiple assessments of executive function. J Nerv Ment Dis. 2008;196:384–389. doi: 10.1097/NMD.0b013e3181710916. [DOI] [PubMed] [Google Scholar]
- 37.Knudsen EI. Fundamental components of attention. Annu Rev Neurosci. 2007;30:57–78. doi: 10.1146/annurev.neuro.30.051606.094256. [DOI] [PubMed] [Google Scholar]
- 38.Kohler CG, Turner TH, Bilker WB, et al. Facial emotion recognition in schizophrenia: intensity effects and error pattern. Am J Psychiatry. 2003;160:1768–1774. doi: 10.1176/appi.ajp.160.10.1768. [DOI] [PubMed] [Google Scholar]
- 39.Marder SR, Fenton W. Measurement and treatment research to improve cognition in schizophrenia: NIMH MATRICS initiative to support the development of agents for improving cognition in schizophrenia. Schizophr Res. 2004;72:5–9. doi: 10.1016/j.schres.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 40.Granholm E, Verney SP, Perivoliotis D, Miura T. Effortful cognitive resource allocation and negative symptom severity in chronic schizophrenia. Schizophr Bull. 2007;33:831–842. doi: 10.1093/schbul/sbl040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Simon AE, Cattapan-Ludewig K, Zimilacher S, et al. Cognitive functioning in the schizophrenia prodrome. Schizophr Bull. 2007;33:761–771. doi: 10.1093/schbul/sbm018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Leifker FR, Bowie CR, Harvey PD. Determinants of everyday outcomes in schizophrenia: the influences of cognitive impairment, functional capacity, and symptoms. Schizophr Res. 2009;115:82–87. doi: 10.1016/j.schres.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 43.Chadwick P, Lees S, Birchwood M. The revised Beliefs About Voices Questionnaire. Br J Psychiatry. 2000;177:229–232. doi: 10.1192/bjp.177.3.229. [DOI] [PubMed] [Google Scholar]
- 44.Carpenter WT, Jr., Heinrichs DW, Wagman AMI. Deficit and nondeficit forms of schizophrenia: the concept. Am J Psychiatry. 1988;145:578–583. doi: 10.1176/ajp.145.5.578. [DOI] [PubMed] [Google Scholar]
- 45.Kirkpatrick B, Buchanan RW, Ross DE, Carpenter WT., Jr A separate disease within the syndrome of schizophrenia. Arch Gen Psychiatry. 2001;58:165–171. doi: 10.1001/archpsyc.58.2.165. [DOI] [PubMed] [Google Scholar]
- 46.Beck AT, Alford BA. Depression: Causes and Treatment. 2nd ed. Philadelphia, PA: University of Pennsylvania Press; 2009. [Google Scholar]
- 47.Trower P, Chadwick PDJ. Pathways to defense of the self: a theory of two types of paranoia. Clin Psychol Sci Pract. 1995;2:263–278. [Google Scholar]
- 48.Yung AR, Phillips LJ, Yuen HP, McGorry PD. Risk factors for psychosis in an ultra high-risk group: psychopathology and clinical features. Schizophr Res. 2004;67:131–142. doi: 10.1016/S0920-9964(03)00192-0. [DOI] [PubMed] [Google Scholar]
- 49.Huppert JD, Smith TE. Anxiety and schizophrenia: the interaction of subtypes of anxiety and psychotic symptoms. CNS Spectr. 2005;10:721–731. doi: 10.1017/s1092852900019714. [DOI] [PubMed] [Google Scholar]