Abstract
Background
Information is scant assessing outcomes in lung transplantation (LT) in advanced occupational lung diseases (OLD).
Aims
To analyse survival after LT for OLD.
Methods
Using data from the US Organ Procurement and Transplantation Network Registry (OPTN-R), we identified subjects aged ≥18 years transplanted for OLD from 2005 to 2010. OPTN-R selected referents of corresponding age, sex and body mass index (BMI) who underwent LT for other diagnoses were also identified. Post-LT survival time was estimated with Cox proportional hazard models. Baseline age, BMI, forced expiratory volume in 1 s, creatinine, lung allocation score, donor age, donor lung ischaemic time and transplant type (single versus bilateral) were included as covariates. Time-dependent covariates were used to model differences in relative risk over time.
Results
Thirty-seven males underwent LT for silicosis (n = 19) or other OLD (n = 18) during the analytic period (0.5% of all LTs). For non-silicotic OLD, 6-month and 1- and 3-year survival estimates were 66, 55 and 55%, compared with the silicotic group (86, 86 and 76%) and referent group (89, 84 and 67%). During the first year post-transplant, those with OLD (silicosis and others combined) manifested an overall 2-fold increased mortality risk [hazard ratio (HR) 2.3, 95% CI 1.3–4.4; P < 0.05] compared to referents. In stratified analysis, this increased risk of death was restricted to those with non-silicotic OLD (HR 3.1, 95% CI 1.5–6.6; P < 0.01). Poorer survival was limited to the first year post-LT.
Conclusions
Subjects undergoing LT for OLD other than silicosis may be at increased risk of death in the first year post-transplantation.
Keywords: Lung transplantation, occupational lung diseases, pneumoconioses, silicosis, survival
Introduction
For those with end-stage occupational lung diseases (OLD), lung transplantation (LT) may be a therapeutic option. Survival benefits have driven an increased demand for LT [1], but data specific to OLD are limited to case reports [2–5] and two case series [6,7]. We evaluated the LT-associated mortality among persons with OLD compared with referents undergoing LT, accounting for transplant-related and disease-status covariates.
Methods
Using national data from the US Organ Procurement and Transplantation Network Registry (OPTN-R), we identified all cases who underwent LT for silicosis or other OLD (separately coded by the OPTN-R) between March 2005 and October 2010. Referents were restricted to OPTN-R males aged 34–68 years and body mass index (BMI) 18–34 (e.g. the same ranges as the cases). Referents supported by mechanical ventilation or extracorporeal membrane oxygenation were excluded (no cases were supported by these modalities). The study was exempted by our institutional human research committee.
Our primary study outcome was post-LT survival. Survival was calculated from the date of LT until the date of death or last OPTN-R follow-up. Survival time was right-censored for subjects alive at last follow-up.
Silicotic, non-silicotic OLD cases and referents were compared using one-way analysis of variance (continuous) or the chi-square test (categorical). Survival was graphically evaluated using Kaplan–Meier methods. Semiparametric estimates of the relative risk of death were estimated using hazard models.
Because violations of the proportionality of hazards assumption were identified (scaled Schoenfeld residuals), we used risk models including a time-dependent covariate. As a key LT clinical outcome, we set survival at 1 year as the a priori cut-point. Risk of death was adjusted for age, BMI, forced expiratory volume in 1 s (FEV1) % predicted, creatinine, Lung Allocation Score (LAS; a composite score quantifying medical urgency and expected post-LT survival [8]), donor age, transplant type (single versus bilateral) and ischaemic time. We repeated our primary analyses further restricting referents to those transplanted for fibrotic lung disease.
Results
Thirty-seven cases, all male, underwent LT for silicosis (n = 19) or other OLD (n = 18), representing 0.5% of 8129 transplants during the study period (Table 1). Other OLD included: pneumoconioses not further classified (n = 7); coal workers pneumoconiosis (n = 6); asbestosis (n = 2); berylliosis (n = 1); ‘metal pneumoconiosis’ (n = 1) and farmer’s lung (n = 1). There were significant differences in BMI (P < 0.01) among the two case and referent categories (Table 1). There were no statistically significant differences among the groups in age, creatinine, FEV1% predicted, LAS, transplant type (single versus double), ischaemic time, donor age or donor gender.
Table 1.
Baseline characteristics
| Characteristic | All OLD | Silicosis | Non-silicosis OLD | Referents |
| Data presented as n (%) or mean ± SD | ||||
| N | 37 | 19 | 18 | 3490 |
| Age, years | 54.3 ± 6.9 | 53.4 ± 6.7 | 55.2 ± 7.3 | 57.2 ± 8.1 |
| BMI* | 24.6 ± 4.4 | 25.5 ± 4.5 | 23.6 ± 4.1 | 26.3 ± 3.8 |
| Creatinine (mg/dl) | 0.93 ± 0.21 | 1.00 ± 0.22 | 0.87 ± 0.20 | 0.96 ± 0.32 |
| FEV1 % of predicted | 31.9 ± 16.2 | 32.9 ± 15.4 | 30.8 ± 17.5 | 39.9 ± 21.3 |
| LAS | 45.4 ± 10.1 | 45.8 ± 12.0 | 45.0 ± 8.0 | 43.2 ± 14.0 |
| Donor age | 32.4 ± 13.0 | 30.4 ± 13.3 | 34.6 ± 12.8 | 33.1 ± 14.0 |
| Donor gender, male | 29 (78) | 14 (74) | 15 (83) | 2645 (76) |
| Bilateral lung transplant | 25 (68) | 15 (79) | 10 (56) | 2063 (60) |
| Ischaemic time, hours | 5.5 ± 1.6 | 5.5 ± 2.1 | 5.5 ± 0.9 | 5.1 ± 1.7 |
OLD, occupational lung disease.
*P < 0.01 by analysis of variance among the three groups: silicosis, non-silicosis OLD and referents.
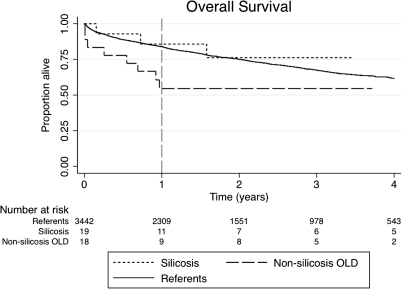
For non-silicotic OLD, 6-month and 1- and 3-year survival estimates were 66, 55 and 55%, compared with silicotic group (86, 86 and 76%) and referent group (89, 84 and 67%), respectively (Figure 1). Causes of death in the non-silicotic OLD group included: infectious (n = 3), cardiac arrest (n = 1), multi-organ failure (n = 1) and not specified (n = 3). Accounting for covariates, the OLD group manifested a 2-fold higher risk of death compared with referents in the first post-transplant year [hazard ratio (HR) 2.3, 95% CI 1.2–4.2; P < 0.05] (Table 2). After 1 year, however, there was no significant difference in risk of death. In a stratified analysis, the higher first post-transplant year mortality risk was limited to subjects with non-silicotic OLD (HR 3.1, 95% CI 1.5–6.6; P < 0.01). Risk estimates were similar when the referent group was restricted to include only those subjects transplanted for lung fibrosis (n = 1839) (Table 2).
Figure 1.
Survival following lung transplantation.
Table 2.
(a) Relative risk of death (hazard ratio) after lung transplant compared to non-OLD controlsa and (b) relative risk of death compared to other fibrotic lung disease controls
| All OLD | Silicosis | Non-silicosis OLD | |
| (a) | |||
| Time since transplant | |||
| 0–1 year | 2.3 (1.3–4.4)* | 1.0 (0.3–4.1) | 3.1 (1.5–6.6)** |
| >1 year | 0.2 (0.03–1.6) | 0.4 (0.1–3.0) | 0.5 (0.1–3.6) |
| (b) | |||
| 0–1 year | 2.3 (1.2–4.5)* | 1.1 (0.3–4.5) | 3.3 (1.5–7.1)** |
| >1 year | 0.5 (0.1–2.0) | 0.5 (0.1–3.3) | 0.5 (0.1–3.7) |
LAS, lung allocation score; OLD, occupational lung disease.
Adjusted for recipient age, FEV1, BMI, LAS, donor age, transplant type (single versus bilateral) and ischaemic time. A hazard ratio of >1.0 represents greater risk for death for subjects who underwent LT for OLD compared with non-OLDs.
*P < 0.05; **P < 0.01.
Discussion
Subjects undergoing LT for OLD manifested a 2-fold increased mortality risk in the first post-transplantation year. This risk was limited to the stratum of non-silicotics and attenuated after the first year post-LT. Importantly, our observations differ from an earlier single-centre report of poorer post-LT survival in silicotics compared with idiopathic pulmonary fibrosis, an analysis that did not adjust for covariates accounted for in our analysis [7].
By using US national data, employing a reasonable strategy to select registry-based referents consistent with prior lung transplant analyses, and controlling for multiple cofactors [9,10], we were able to unmask a previously unidentified pattern of poorer survival following LT for OLD. Our findings provide epidemiological context to prior case reports (including one of the first reported human lung transplants with extended post-surgical survival) and two single-centre analyses of LT performed for OLD [2–7].
Even in such a large cohort of LT recipients, transplantation for OLD is relatively rare. We cannot exclude, however, that other cases of OLD might have been obscured within the OPTN-R diagnostic coding schema. For example, a separate code allows for hypersensitivity pneumonitis without allowance for a specific cause. Also, the OPTN-R does not capture potentially relevant recipient characteristics and has limited information on cause of post-transplant death. Indeed, cause of death was missing for 38% of non-silicotic OLD cases. These limitations make it challenging to identify causal mechanisms for the observed pattern of risk. Potential explanations may be that non-silicotic OLD cases had concurrent co-morbidities such as secondary pulmonary hypertension or were exposed to empiric immunosuppressive therapy prior to LT, thereby increasing the risk for infectious complications post-transplant. Nevertheless, while the excess early mortality risk appears to be contributed by non-silicosis OLD, assigning a cause for this, as well as the later convergence in mortality risk among the three groups, would be highly speculative. Lastly, the non-silicotic OLD group was heterogeneous. Thus, it is not possible using an epidemiological approach to isolate individual characteristics that might have accounted for the observed grouped differences in mortality risk. It is unlikely, although not impossible, that unmeasured confounding played a role. If it did, it would have had to operate uniformly across this very same heterogeneity. Given the myriad of factors that impact individual post-transplant survival, including post-operative technical and infectious complications, it is unlikely that other approaches to referent selection or stratified sub-analyses would better control for such confounders, if indeed they were present.
In sum, practitioners should be cognizant that persons with end-stage non-silicosis OLD may have an increased mortality risk in the first year after LT. There is, however, insufficient evidence to modify current clinical practice in regard to such LT candidates. For persons with end-stage OLD, LT may be the only therapeutic option.
Key points
Lung transplantation for occupational lung diseases is relatively rare in the USA, representing 0.5% of all transplants performed.
Subjects undergoing lung transplantation for occupational lung diseases appear to be at risk for poorer survival in the first post-transplant year.
This first post-transplant year risk appears to be restricted to those subjects undergoing lung transplantation for non-silicotic occupational lung diseases.
Funding
This work was supported by the National Heart Lung and Blood Institute at the National Institute of Health (K24 HL097245) and Health Resources and Services Administration contract 231-00-0115.
Conflicts of interest
None declared.
Acknowledgments
The content is the responsibility of the authors alone and does not necessarily reflect the views or policies of the US Department of Health and Human Services.
References
- 1.Christie JD, Edwards LB, Kucheryavaya AY, et al. The Registry of the International Society for Heart and Lung Transplantation: twenty-seventh official adult lung and heart-lung transplant report—2010. J Heart Lung Transplant. 2010;29:1104–1108. doi: 10.1016/j.healun.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 2.Derom F, Barbier F, Ringoir S, et al. Ten-month survival after lung homotransplantation in man. J Thorac Cardiovac Surg. 1971;61:835–846. [PubMed] [Google Scholar]
- 3.Lung Transplant Group. Single lung transplantation for end-stage silicosis: report of a case. J Formos Med Assoc. 1992;91:926–932. [PubMed] [Google Scholar]
- 4.Brichon PY, Blin D, Noirclerc M, et al. [Diffuse bronchomalacia after double lung transplantation. Thoughts apropos of a case] Ann Chir. 1992;46:105–109. [PubMed] [Google Scholar]
- 5.Demoulin AS, Hermans G, Gustin M. [An unusual interstitial pneumonitis] Rev Med Liege. 2009;64:373–376. [PubMed] [Google Scholar]
- 6.Mao WJ, Chen JY, Zheng MF, et al. Lung transplantation for end-stage silicosis. J Occup Environ Med. 2011;53:845–849. doi: 10.1097/JOM.0b013e3182260e50. [DOI] [PubMed] [Google Scholar]
- 7.Di Giuseppe M, Gambelli F, Hoyle GW, et al. Systemic inhibition of NF-kappaB activation protects from silicosis. PLoS One. 2009;4 doi: 10.1371/journal.pone.0005689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Egan TM, Murray S, Bustami RT, et al. Development of the new lung allocation system in the United States. Am J Transplant. 2006;6:1212–1227. doi: 10.1111/j.1600-6143.2006.01276.x. [DOI] [PubMed] [Google Scholar]
- 9.Allen JG, Arnaoutakis GJ, Weiss ES, et al. The impact of recipient body mass index on survival after lung transplantation. J Heart Lung Transplant. 2010;29:1026–1033. doi: 10.1016/j.healun.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 10.Gries CJ, Rue TC, Heagerty PJ, et al. Development of a predictive model for long-term survival after lung transplantation and implications for the lung allocation score. J Heart Lung Transplant. 2010;29:731–738. doi: 10.1016/j.healun.2010.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]