Abstract
Dejan Zurovac and colleagues discuss six areas where text messaging could improve the delivery of health services and health outcomes in malaria in Africa.
Summary Points
Across many malaria-endemic areas in rural Africa, the communication gap between managers, health workers, and patients is a significant barrier to efficient malaria control.
The rapid expansion of mobile network coverage and the widespread availability of basic handsets have the potential to substantively bridge the communication gap.
Text messaging, as the least-expensive mobile phone function found on all handsets, could improve the delivery of health services and health outcomes.
Six major areas of malaria control in which deficiencies are apparent and text messaging interventions could be beneficial are: (1) disease and treatment effectiveness surveillance, (2) monitoring of the availability of health commodities, (3) pharmacovigilance and post-marketing surveillance of the safety and quality of antimalarial drugs, (4) health worker adherence to guidelines, (5) patient adherence to medication regimens, and (6) post-treatment review.
Text messages transmitting information from the periphery of the health systems to malaria control managers are in the first three malaria control areas: (1) disease and treatment effectiveness surveillance, (2) monitoring of the availability of health commodities, and (3) pharmacovigilance and post-marketing surveillance of the safety and quality of antimalarial medicines. Future projects in these three areas should demonstrate responses to data signals and comparative advantages with routine information systems.
Text messages in the second three areas transmit information to health workers and patients to support the management of malaria patients by improving (4) health workers' adherence to guidelines, (5) patient adherence to medicines, and (6) post-treatment review. Future priorities in these areas are cost-effectiveness evaluations, qualitative research, and studies measuring impact on the processes of care and health outcomes.
Malaria and Narrowing the Communication Gap in Africa
Across many malaria-endemic areas in rural Africa, health systems are weak, infrastructure is poor, and poverty is widespread. Traditionally, the communication gap between managers of health services, health workers at the periphery, and the patient population they serve has been a barrier to efficient service delivery [1]. This gap, however, has the potential to be bridged through the rapid expansion of mobile network coverage, availability of inexpensive handsets, and decreasing costs of mobile phone services [2],[3]. It has been estimated that over two-thirds of the population in Africa is covered by a mobile network with a penetration rate of 50%, reaching over half a billion mobile phone subscribers across the continent [3],[4]. The very nature of this coverage has resulted in various initiatives to alleviate poverty such as providing market information for rural farmers, assisting contract laborers to find employers [5], or using mobile phones as a virtual bank to pay for goods and services and to ensure immediate transfer of funds to remote areas [6]. The lack of immediate access to funds has been one of the economic barriers to accessing health services in rural areas [7]. Although they are not yet quantified, virtual bank initiatives and mobile money are likely to have a significant impact on access to travel funds to reach distal clinics.
Malaria has plagued Africa for centuries and exacted a heavy public health burden. International interest in its control has varied over the last 100 years. The last 10 years of the Roll Back Malaria Initiative, accompanied by substantial financial assistance from the Global Fund and bilateral agencies, have transformed the availability of preventative measures to poor communities in Africa, resulting in significant reductions in malaria across the continent [8],[9]. However, some of the greatest operational challenges to sustain this progress are in ensuring effective surveillance, continuous stocks of life-saving commodities, and adequate malaria case management [8],[10],[11].
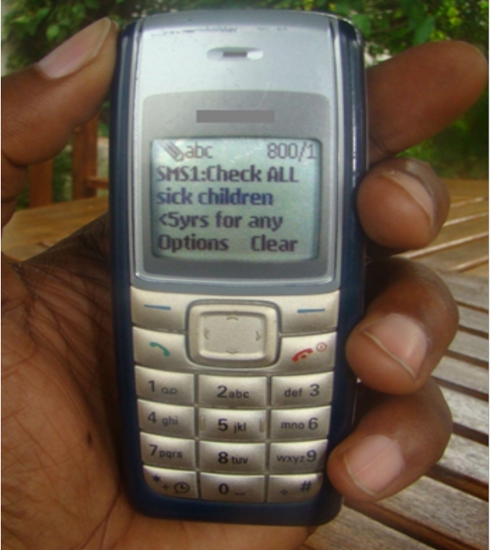
The widespread use of SMS (short message service), the least-expensive mobile phone function, offers a solution that could rapidly overcome weaknesses in communication, potentially leading to improved delivery of health services and better health outcomes. Text messaging is particularly attractive because it is available on most basic handsets without the need for additional applications (Figure 1). SMS functions on a lower bandwidth than does voice, requires minimal skills in its use, offers automated delivery, and is personally convenient because of its asynchronous character [12],[13]. Despite the recognized potential of SMS technology, there are very few studies demonstrating the impact of text messaging in malaria control. For example, we searched Medline database and found only six studies reporting the use of text messaging within the malaria field in Africa (Table 1). The paucity of peer-reviewed studies limits our ability to compare and integrate possible effect sizes of new technologies on health systems or patient outcomes. As with any innovation, evidence from controlled trials is important to promote and effect policy change.
Figure 1. Example of mobile phones common in rural Africa.
Table 1. Studies reporting use of text messaging for malaria control in Africa.
| Country | Area of Malaria Control | No of HFs | Text Messaging Content | Dominant Text Message Flow | Reporting Frequency | Feasibility Shown | Potential Response | Reference |
| Zambia | Disease surveillance (foci detection) | 13 | Name of HF; Name of sender; No RDT tested; No RDT positive | Upstream | Weekly | Yes | Active screening; outbreak response | [20] |
| Madagascar | Disease surveillance (outbreak detection) | 13 | No of patient visits; No of patients meeting case-definition | Upstream | Daily | Yes | Outbreak response | [21] |
| Tanzania | Commodity monitoring | 129 | AL stock for each of 4 packs; stock quinine vials | Upstream | Weekly | Yes | Drug redistribution; Emergency orders | [22] |
| Uganda | Disease surveillance and commodity monitoring | 147 | 26 malaria testing, treatment and ACT and RDT stock parameters | Upstream | Weekly | Yes | Drug redistribution; Emergency orders; Case-management corrections | [23] |
| Tanzania | Post-marketing surveillance | 25 | Patient demographic, date, type of event | Upstream | When occurred | Yes | Investigation of adverse drug reactions | [24] |
| Kenya | Health worker adherence | 52 | 10 different case-management messages per week over 26 weeks | Downstream | Twice daily | Yes | Not applicable | [45] |
ACT, artemisinin-based combination therapy; HF, health facility; RDT, rapid diagnostic test.
In this viewpoint we propose six major areas within malaria control in which solutions are urgently required and simple text messaging could offer the solution to improve routine delivery of health services (Figure 2). We consider text messaging interventions that have the potential for immediate scale-up, benefiting from the widespread availability of basic mobile phones that do not require installation and maintenance of additional applications (Figure 1). The next generations of mobile devices, such as “smartphones,” which are more complex, more expensive, and not yet widely available in rural Africa, are not considered here. We categorized interventions based on the dominant text messaging flow within the health system as those transmitting information from the periphery of the health systems to the control managers and those transmitting information to health workers and patients to support disease management (Figure 2).
Figure 2. Potential applications of text messaging for routine malaria health service delivery.
Blue arrows, dominant SMS communication targeting control managers; red arrows, dominant SMS communication targeting health workers and patients; green boxes, areas of intervention.
Text Messaging Interventions Transmitting Information to Malaria Control Managers
Effective malaria control depends on the range of routinely collected and timely reported health facility data. Three of these that can be broadly categorized as surveillance or monitoring activities are of particular importance following large scale implementations of malaria interventions across Africa [9]. They include (1) disease and treatment effectiveness surveillance, (2) monitoring the availability of commodities such as antimalarial medicines or rapid diagnostic tests, and (3) monitoring of adverse drug events (pharmacovigilance) and of the safety and quality of antimalarial products on the market (post-marketing surveillance). The latter is of particular importance given the threat of artemisinin tolerance recently detected in Southeast Asia and its imminent spread to the African continent; early detection tools are needed as part of treatment effectiveness surveillance [14].
Unfortunately, in many African countries, the routine health, logistics, and surveillance systems through which malaria data are reported in an “upstream” direction to managers are weak components of the health systems [15]–[18]. The validity and utility of information is compromised because the poor quality of source information, low reporting rates, delays in data acquisition, and lack of visibility of predefined unit signals and summary indicators preclude prompt responses to threats and emergencies such as malaria outbreaks, stock-outs of antimalarial drugs, presence of suboptimal drugs [19], or occurrences of severe adverse drug reactions and treatment failures.
The broad availability of mobile phones and with them the use of text messaging among health workers in rural areas could overcome delays, ensure nearly real-time data acquisition, and through computerized platforms make available pre-defined indicators to control managers. Such timely visibility could strengthen governance of scarce resources and should thereby result in prompt responses at different levels of the health system (in many cases, responses at the district level could be sufficient to mitigate the problem). For example, within our first proposed area of intervention—aiming to improve disease and treatment effectiveness surveillance—district supervisors could respond by initiating investigations of and targeted interventions to unusual upsurges of malaria, by reinforcing health workers' testing and treatment practices for detected discrepancies between test-positive and reported malaria cases, or by verifying reports of increased treatment failures and calling for urgent support for studies to confirm or rule out artemisinin resistance. Within our second area of intervention targeting availability of health commodities—district supervisors should be able to respond to threatening stock-outs of medicines or diagnostics by redistributing commodities between facilities or placing emergency orders. Finally, within the third intervention area—pharmacovigilance and post-marketing surveillance—suspected reports of adverse drug reactions and alerts of counterfeit drugs require prompt field verification, sample collection, and initiation of product investigations at the central level with the regular feedback provided to reporting clinicians.
In recognition of the possibilities of timely information transfer by text messaging, it is not surprising that nearly all pilot projects within the malaria field were indeed in the areas of surveillance and commodity monitoring (Table 1). Disease surveillance has been reported by SMS in Zambia [20] and Madagascar [21], and commodity monitoring in Tanzania [22]. In Uganda, the utility of SMS was assessed for both disease and commodities monitoring [23]. In Tanzania, the safety of antimalarial therapy was monitored [24]. The number of SMS reporting parameters ranged from four to 26. All text messages were sent from a health worker's personal mobile phone without additional software applications, and all projects demonstrated the feasibility of reporting real-time data, achieving high rates of reporting, and potential utility for control managers. However, with the exception of the Tanzanian projects, it was unclear how much health workers and the populations they serve benefited from these SMS-enhanced surveillance activities compared to those relying on routine information systems.
We envision that, in the near future, the role of SMS reporting will become most important and effective in areas where malaria public health emergencies are imminent, response mechanisms are clearly defined, and the impact of enhanced real-time reporting is proved superior to routine information systems. We emphasize responses at the health facility level, because failure to do so would both result in missed opportunities to save lives and risk health worker “reporting fatigue” regardless of whether reporting is based on the text messaging or on traditional methods.
Text Messaging Interventions to Support Disease Management
High levels of patient adherence to antimalarial treatments and health worker adherence to malaria treatment guidelines are vital components of successful malaria case management. They help ensure good clinical outcomes for individual patients [25]–[27] and minimize the risk of drug resistance at the population level [28],[29]. Across Africa, clinical practices discordant with national malaria guidelines have been widely reported [30]–[33]. Patient nonadherence to lifesaving antimalarial therapies is also common [34]–[37].
Studies in developed countries [13],[38],[39] and an increasing number of rigorous trials in Africa [40],[41] have investigated the impact of text message reminders on patient adherence to long-term therapies for infectious and noncommunicable diseases, and all have shown encouraging results. To our knowledge, however, no study has yet been undertaken to investigate the use of SMS for widely used short-course therapies with complex dosing regimens in developing countries, such as those prescribed for malaria in Africa. Emphasis has traditionally been on more complex and expensive behavioral change initiatives to improve community- and clinic-based practices, including improved formulations and packaging of antimalarial drugs [42]–[44]. SMS reminders to caretakers and patients while the latter takes prescribed medications could improve compliance. This is one area of disease management where we see a need for carefully designed trials under various operational settings.
A further departure from traditional approaches to improving health worker performance has been recently tested in Kenya [45]. A randomized controlled trial at rural health facilities showed that SMS reminders sent to health workers' personal phones substantially improved their adherence to malaria guidelines, and that improvements were sustained after the end of the intervention. This is another area of intervention for which further work on optimizing intervention replication is necessary.
Post-treatment review of patients treated for malaria is a case-management component that deserves special attention. For malaria treatment reviews, day 3 outcomes are a valuable early warning signal when reported as part of the treatment effectiveness surveillance to detect emerging artemisinin resistance [14]. However, the feasibility of detecting this valuable information is possible only if patients do return to the facility for the post-treatment review. Unfortunately, across most of the outpatient settings in Africa, follow-up is one of the weakest components of the routine clinical process. In developed countries SMS messages have been widely used to remind patients of scheduled appointments [46],[47]. Similarly, more complex mobile phone applications have shown significant improvement in the follow-up of malaria patients in Thailand [48]. The same approaches should be tested in Africa as part of the SMS reminder package to improve patients' adherence to antimalarial treatment schedules.
The impact of text messaging applications in the areas of malaria adherence and post-treatment review is still unclear in Africa. Feasibility projects including rigorous cost-effectiveness evaluations and qualitative research to better understand determinants of the successes or failures of SMS interventions are urgently required. Importantly, even if text message reminders are shown to be simple, inexpensive, and effective in improving adherence they are unlikely to achieve perfect outcomes on their own. Therefore they should be seen as a booster to malaria care and not as a solution replacing basic programmatic inputs such as delivery of in-service training, guidelines and supportive supervision, clinical audits for health workers, or provision of child-friendly medicine formulations with pictorial inserts for patients.
Barriers and Gaps to Adoption of Text Messaging in Routine Malaria Control in Africa
We have highlighted the scarcity of peer-reviewed studies and thus the absence of an evidence platform to gauge the effectiveness of text messaging for malaria control in Africa. SMS-based interventions should be held to the same evidence-based criteria as any other new tool for malaria control, even before considerations of policy adoption and implementation. Furthermore, there are several other adoption barriers that deserve attention. First, despite the focus of our interventions on the use of basic personal mobile phones and the least expensive SMS function, the actual implementation costs must be carefully determined as part of effectiveness studies. Second, high usability of mobile applications for health workers and patients in rural Africa is an important feasibility determinant. Other than the voice function, text messaging is the simplest and the most widely used technology function for which all of the reviewed studies have shown ease of use in reporting periodic data from the health system periphery to control managers. This however remains to be proved for interventions targeting individual patients, to whom a high facility workload or illiteracy may present a barrier. Third, although a substantial number of reporting parameters can be included in SMS interventions [23], these capacities are lower than in more complex software applications that can be installed on the new generations of mobile devices. To allow expansion of SMS-based interventions beyond malaria control, we call for reporting of a minimum number of critical surveillance parameters sufficient to trigger well-established emergency responses. Fourth, the proposed interventions do not depend on installation and maintenance of any software applications on the phone itself. There is, however, a technical requirement for development, hosting, and maintenance of computerized platforms that may not be locally available in all African settings. In addition, the reach of SMS-assisted innovation does depend on mobile network coverage. It is now possible using geographic information systems and cell tower locations to define marginalized health facilities and populations in malaria risk areas where SMS interventions are especially needed but are beyond the national coverage grid. This work must be undertaken in parallel to controlled trials to ensure an effective national policy platform. Finally, from the ownership perspective relevant for policy adoptions, the field of mobile applications in health, which was traditionally led by computer sciences, should evolve into multidisciplinary work including epidemiologists, social scientists, health systems researchers, and national policy makers from health, information technology, and development.
Conclusions
We have suggested six areas of malaria control in which text messaging communication may improve delivery of services and health outcomes (Figure 1). For the three areas in which information is transmitted from the periphery of the health system to malaria control managers—disease and treatment effectiveness surveillance, monitoring the availability of health commodities, and pharmacovigilance and post-marketing surveillance of the safety and quality of antimalarial medicines—future priorities are projects demonstrating responses to detected data signals and comparative advantages with routine information systems. For the three areas in which transmitted information would help support management of malaria patients by improving health worker adherence to guidelines, patient adherence to medicines, and post-treatment review, future priorities are rigorous cost-effectiveness evaluations, qualitative research, and studies measuring impact on the processes of care and health outcomes.
Acknowledgments
The paper is published with the permission of the Director of the Kenya Medical Research Institute.
Footnotes
The authors have declared that no competing interests exist.
DZ is supported by the Wellcome Trust project grant [#084253]. RWS is supported by the Wellcome Trust as Principal Research Fellow [#079080]. AOT is supported by the Worldwide Antimalarial Resistance Network (WWARN) through a Bill & Melinda Gates Foundation grant [#48807.01]. All authors acknowledge support from the Wellcome Trust core grant [#092654/Z/10/A]. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Provenance: Not commissioned; externally peer reviewed.
References
- 1.Ranck J. Health Information and Health Care: The Role of Technology in Unlocking Data and Wellness – A Discussion Paper. Washington, D.C.: United Nations Foundation & Vodafone Foundation Technology Partnership, February 2011; 2011. [Google Scholar]
- 2.Banks K. Mobile phones and the digital divide. 2008. PCWorld Communications Inc. Available: http://www.pcworld.com/article/149075/mobile_phones_and_the_digital_divide.html. Accessed: 11 November 2011.
- 3.International Telecommunication Union. African telecommunication/ICT indicators 2008: at a crossroads. 2008. Available: http://www.itu.int/ITU-D/ict/publications/africa/2008/index.html. Accessed: 11 November 2011.
- 4.International Telecommunication Union. The world in 2010: ICT facts and figures. 2010. Available: http://www.itu.int/ITU-D/ict/material/FactsFigures2010.pdf. Accessed: 11 November 2011.
- 5.Eagle N. Entrepreneurship and education through mobile phones in Kenya. 2005. Massachusetts Institute of Technology. Available: http://web.media.mit.edu/~nathan/africa_nokia.pdf. Accessed: 11 November 2011.
- 6.Hughes N, Lonie S. M-PESA: mobile money for the “un-banked”. Innovations. 2007;2:63–81. [Google Scholar]
- 7.Chuma J, Okungu V, Molyneux C. Barriers to prompt and effective malaria treatment among the poorest population in Kenya. Malaria J. 2010;9:144. doi: 10.1186/1475-2875-9-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Snow RW, Marsh K. Malaria in Africa: progress and prospects in the decade since the Abuja Declaration. Lancet. 2010;376:137–139. doi: 10.1016/S0140-6736(10)60577-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. World Malaria Report 2010. 2010. Geneva. Available: http://www.who.int/malaria/world_malaria_report_2010/en/index.html. Accessed: 11 November 2011.
- 10.World Health Organization. Malaria case management: Operations manual. 2009. Geneva. Available: http://www.who.int/malaria/publications/atoz/9789241598088/en/index.html. Accessed: 11 November 2011.
- 11.World Health Organization. Universal access to malaria diagnostic testing: An operation manual. 2011. Geneva. Available: http://www.who.int/malaria/publications/atoz/9789241502092/en/index.html. Accessed: 11 November 2011.
- 12.Terry M. Text messaging in healthcare: the elephant knocking at the door. Telemed J E Health. 2008;14:520–524. doi: 10.1089/tmj.2008.8495. [DOI] [PubMed] [Google Scholar]
- 13.Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiol Rev. 2010;32:56–69. doi: 10.1093/epirev/mxq004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization. Global Plan for Artemisinin Resistance Containment. 2011. Geneva. Available: http://www.who.int/malaria/publications/atoz/9789241500838/en/index.html. Accessed: 13 November 2011.
- 15.Nsubuga P, Eseko N, Wuhibm T, Ndayimirije N, Chungong S, et al. Structure and performance of infectious disease surveillance and response, United Republic of Tanzania, 1998. Bull World Health Organ. 2002;80:196–203. [PMC free article] [PubMed] [Google Scholar]
- 16.Talisuna AO, Staedke SG, D'Alessandro U. Pharmacovigilance of antimalarial treatment in Africa: is it possible? Malaria J. 2006;5:50. doi: 10.1186/1475-2875-5-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rowe AK, Kachur SP, Yoon SS, Lynch M, Slutsker L, et al. Caution is required when using health facility-based data to evaluate the health impact of malaria control efforts in Africa. Malaria J. 2009;8:209. doi: 10.1186/1475-2875-8-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maokola W, Willey BA, Shirima K, Chemba M, Armstrong Schellenberg JRM, et al. Enhancing the routine health information system in rural southern Tanzania: successes, challenges and lessons learned. Trop Med Int Health. 2011;16:721–730. doi: 10.1111/j.1365-3156.2011.02751.x. [DOI] [PubMed] [Google Scholar]
- 19.Greenwood. African apps boost business growth. 2011. Available: http://www.bbc.co.uk/news/business-13475609. Accessed 7 November 2011.
- 20.Davis RG, Kamanga A, Castillo-Salgado C, Chime N, Mharakurwa S, et al. Early detection of malaria foci for targeted interventions in endemic southern Zambia. Malaria J. 2011;10:260. doi: 10.1186/1475-2875-10-260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Randrianasolo L, Raoelina Y, Ratsitorahina M, Ravolomanana L, Andriamandimby S, et al. Sentinel surveillance system for early outbreak detection in Madagascar. BMC Public Health. 2010;10:31. doi: 10.1186/1471-2458-10-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barrington J, Wereko–Brobby O, Ward P, Mwafongo W, Kungulwe S. SMS for Life: a pilot project to improve anti-malarial drug supply management in rural Tanzania using standard technology. Malar J. 2010;9:298. doi: 10.1186/1475-2875-9-298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Asiimwe C, Gelvin D, Lee E, Amor YB, Quinto E, et al. Use of an innovative, affordable, and open-source short message service–based tool to monitor malaria in remote areas of Uganda. Am J Trop Med Hyg. 2011;85:26–33. doi: 10.4269/ajtmh.2011.10-0528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kabanywanyi AM, Mulure N, Migoha C, Malila A, Lengeler C, et al. Experience of safety monitoring in the context of a prospective observational study of artemether-lumefantrine in rural Tanzania: lessons learned for pharmacovigilance reporting. Malaria J. 2010;9:205. doi: 10.1186/1475-2875-9-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fogg C, Bajunirwe F, Piola P, Biraro S, Checchi F, et al. Adherence to a six-dose regimen of artemether-lumefantrine for treatment of uncomplicated Plasmodium falciparum malaria in Uganda. Am J Trop Med Hyg. 2004;71:525–530. [PubMed] [Google Scholar]
- 26.Piola P, Fogg C, Bajunirwe F, Biraro S, Grandesso F, et al. Supervised versus unsupervised intake of six-dose artemether-lumefantrine for treatment of acute, uncomplicated Plasmodium falciparum malaria in Mbarara, Uganda: a randomized trial. Lancet. 2005;365:1467–1473. doi: 10.1016/S0140-6736(05)66416-1. [DOI] [PubMed] [Google Scholar]
- 27.Conteh L, Stevens W, Wiseman V. The role of communication between clients and health care providers: implications for adherence to malaria treatment in rural Gambia. Trop Med Int Health. 2007;12:382–391. doi: 10.1111/j.1365-3156.2006.01806.x. [DOI] [PubMed] [Google Scholar]
- 28.Nosten F, Brasseur P. Combination therapy for malaria: the way forward? Drugs. 2002;62:1315–1329. doi: 10.2165/00003495-200262090-00003. [DOI] [PubMed] [Google Scholar]
- 29.Barnes KI, Watkins WM, White NJ. Antimalarial dosing regimens and drug resistance. Trends Parasitol. 2008;24:127–134. doi: 10.1016/j.pt.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 30.Zurovac D, Rowe AK. Quality of treatment for febrile illness among children at outpatient facilities in sub-Saharan Africa. Ann Trop Med Parasitol. 2006;100:283–296. doi: 10.1179/136485906X105633. [DOI] [PubMed] [Google Scholar]
- 31.Eriksen J, Tomson G, Mujinja P, Warsame MY, Jahn A, et al. Assessing health worker performance in malaria case management of underfives at health facilities in a rural Tanzanian district. Trop Med Int Health. 2007;12:52–61. doi: 10.1111/j.1365-3156.2006.01753.x. [DOI] [PubMed] [Google Scholar]
- 32.Hamer DH, Ndhlovu M, Zurovac D, Fox M, Yeboah-Antwi K, et al. Improved diagnostic testing and malaria treatment practices in Zambia. JAMA. 2007;297:2227–2231. doi: 10.1001/jama.297.20.2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nyandigisi A, Memusi D, Mbithi A, Ang'wa N, Shieshia M, et al. Malaria case-management following change of policy to universal parasitological diagnosis and targeted artemisinin-based combination therapy in Kenya. PLoS One. 2011;6:e24781. doi: 10.1371/journal.pone.0024781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Beer N, Ali AS, Rotllant G, Abass AK, Omari RS, et al. Adherence to artesunate-amodiaquine combination therapy for uncomplicated malaria in children in Zanzibar, Tanzania. Trop Med Int Health. 2009;14:1–9. doi: 10.1111/j.1365-3156.2009.02289.x. [DOI] [PubMed] [Google Scholar]
- 35.Gerstl S, Dunkley S, Mukhtar A, Baker S, Maikere J. Successful introduction of artesunate combination therapy is not enough to fight malaria: results from an adherence study in Sierra Leone. Trans Roy Soc Trop Med Hyg. 2010;104:328–335. doi: 10.1016/j.trstmh.2009.12.008. [DOI] [PubMed] [Google Scholar]
- 36.Lawford H, Zurovac D, O'Reilly L, Hoibak S, Cowley A, et al. Adherence to prescribed artemisinin-based combination therapy in Garissa and Bunyala districts, Kenya. Malaria J. 2011;10:281. doi: 10.1186/1475-2875-10-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mace KE, Mwandama D, Jafali J, Luka M, Filler SJ, et al. Adherence to treatment with artemether-lumefantrine for uncomplicated malaria in rural Malawi. Clin Infect Dis. 2011;53:772–779. doi: 10.1093/cid/cir498. [DOI] [PubMed] [Google Scholar]
- 38.Krishna S, Boren SA, Balas EA. Healthcare via cell phones: a systematic review. Telemed J E Health. 2009;15:231–240. doi: 10.1089/tmj.2008.0099. [DOI] [PubMed] [Google Scholar]
- 39.Fjeldsoe BS, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short-message service. Am J Prev Med. 2009;36:165–173. doi: 10.1016/j.amepre.2008.09.040. [DOI] [PubMed] [Google Scholar]
- 40.Lester RT, Ritvo P, Mills EJ, Kariri A, Karanja S, et al. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): a randomised trial. Lancet. 2010;376:1838–1845. doi: 10.1016/S0140-6736(10)61997-6. [DOI] [PubMed] [Google Scholar]
- 41.Pop-Eleches C, Thirumurthy H, Habyarimana JP, Zivin JG, Goldstein MP, et al. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: a randomized controlled trial of text message reminders. AIDS. 2011;25:825–834. doi: 10.1097/QAD.0b013e32834380c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Marsh VM, Mutemi WM, Muturi J, et al. Changing home treatment of childhood fevers by training shop keepers in rural Kenya. Trop Med Int Health. 1999;4:383–389. doi: 10.1046/j.1365-3156.1999.00403.x. [DOI] [PubMed] [Google Scholar]
- 43.Kabanywanyi AM, Lengeler C, Kasim P, King'eng'ena S, Schlienger R, et al. Adherence to and acceptability of artemether-lumefantrine as first-line anti-malarial treatment: evidence from a rural community in Tanzania. Malaria J. 2010;9:28. doi: 10.1186/1475-2875-9-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yeboah-Antwi K, Gyapong JO, Asare IK, Barnish G, Evans DB, et al. Impact of prepackaging antimalarial drugs on cost to patients and compliance with treatment. Bull World Health Organ. 2001;79:394–399. [PMC free article] [PubMed] [Google Scholar]
- 45.Zurovac D, Sudoi RK, Akhwale WS, Ndiritu M, Hamer DH, et al. The effect of mobile phone text-message reminders on Kenyan health workers' adherence to malaria treatment guidelines: a cluster randomised trial. Lancet. 2011;378:795–803. doi: 10.1016/S0140-6736(11)60783-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Car J, Gurol-Urganci I, de Jongh T, Vodopivec-Jamsek V, Atun R. Mobile phone messaging reminders for attendance at scheduled healthcare appointments. Cochrane Database of Systematic Reviews. 2008 doi: 10.1002/14651858.CD007458.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hasvold PE Wootton. Use of telephone and SMS reminders to improve attendance at hospital appointments: a systematic review. J Telemed Telecare. 2011;17:358–364. doi: 10.1258/jtt.2011.110707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Meankaew P, Kaewkungwal J, Khamsiriwatchara A, Khunthong P, Singhasivanon P, et al. Application of mobile-technology for disease and treatment monitoring of malaria in the “Better Border Health Care Programme”. Malaria J. 2010;9:237. doi: 10.1186/1475-2875-9-237. [DOI] [PMC free article] [PubMed] [Google Scholar]