Abstract
Background and Objectives
Identifying symptom clusters of acute myocardial infarction (AMI) and their clinical significance may be useful in guiding treatment seeking behaviors and in planning treatment strategy. The aim of this study was to identify clusters of acute symptoms and their associated factors that manifested in patients with first-time AMI, and to compare clinical outcomes among cluster groups within 1-year of follow-up.
Subjects and Methods
A total of 391 AMI patients were interviewed individually using a structured questionnaire for acute and associated symptoms between March 2008 and June 2009 in Korea.
Results
Among 14 acute symptoms, three distinct clusters were identified by Latent Class Cluster Analysis: typical chest symptom (57.0%), multiple symptom (27.9%), and atypical symptom (15.1%) clusters. The cluster with atypical symptoms was characterized by the least chest pain (3.4%) and moderate frequencies (31-61%) of gastrointestinal symptoms, weakness or fatigue, and shortness of breath; they were more likely to be older, diabetic and to have worse clinical markers at hospital presentation compared with those with other clusters. Cox proportional hazards regression analysis showed that, when age and gender were adjusted for, the atypical symptom cluster significantly predicted a higher risk of 1-year mortality compared to the typical chest pain cluster (hazard ratio 3.288, 95% confidence interval 1.087-9.943, p=0.035).
Conclusion
Clusters of symptoms can be utilized in guiding a rapid identification of symptom patterns and in detecting higher risk patients. Intensive treatment should be considered for older and diabetic patients with atypical presentation.
Keywords: Acute myocardial infarction, Acute coronary syndrome, Symptom, Cluster analysis
Introduction
The symptoms that patients are experiencing during acute coronary events are a key component in health care providers' decision to initiate medical treatment and in further evaluation. In addition, patients' earlier recognition of symptoms will facilitate the need for treatment seeking.1) A study reported that chest pain was the sole symptom in only 35% of cases and chest pain was accompanied by other symptoms in 57% of cases.2) Overall, patients experienced a mean of 4.75 symptoms as part of the acute event of acute myocardial infarction (AMI).3) The absence of chest pain and the vagueness of symptoms might not be recognized as an indication of a cardiac problem, resulting in a delay in seeking medical care. In addition, this atypical presentation predicted lower use of thrombolytic therapy and was associated with hospital complications compared with the typical presentation.4),5)
Symptom clusters can be defined as multiple symptoms that are related to each other and are experienced concurrently.6),7) The clusters share a common etiology and a measurement of frequency, and severity of symptoms within clusters typically correlate with each other.8) They may also be useful in formulating criteria and evaluating patterns of symptoms. It is worthwhile to know how individual symptoms cluster by demographic and clinical characteristics of the subgroups in order to provide key information for early detection and diagnosis.9),10) Identification of symptom clusters can be a clinically relevant way to detect specific demographic groups that are most likely to experience similar symptoms with readily identifiable characteristics.11),12) Previous cluster studies on prehospital symptoms provided a useful grouping of acute coronary syndrome (ACS) patients based on their experienced symptoms.9)-12) The clarification of prospective clinical outcomes for major adverse cardiac events (MACE) should be helpful to health care providers in planning treatment strategies depending on the clusters.
Therefore, this study examined symptom clusters during acute events and clinical outcomes at 1-year follow-up by symptom cluster in patients with first-time AMI. This clinical trial should enable health care providers to educate, more efficiently, individuals in the target populations at risk for cardiovascular disease (CVD), to reduce prehospital delay time in Korea, and to provide a useful treatment strategy for different symptomatic groups.
Subjects and Methods
Study sample
The data for this study were obtained from first-time AMI patients who were hospitalized for revascularization. Subjects were recruited from the pool of patients hospitalized in Chonnam National University Hospital (CNUH) between 2007 and 2009. Inclusion criteria were: 1) patients who had undergone a first attack of ST-elevation myocardial infarction (STEMI) or non-ST-elevation myocardial infarction (NSTEMI), 2) verbally communicable, and 3) those who agreed to participate in the study. After obtaining approval of the institutional review board of the hospital, the principal investigator (PI) contacted eligible patients who were hospitalized in a cardiovascular care unit to ask them to participate in the study.
Data collection
This study was approved by the clinical ethics committee at CNUH before data collection was carried out. The PI interviewed the patients who had undergone a percutaneous coronary intervention using a semi-structured questionnaire. The interview was done in the education room with a research assistant (RA). Electronic medical records (EMR) were also reviewed to collect medical treatment histories and laboratory data. Each patient was asked about his chief complaints and associated symptoms that he experienced during the acute phase of an AMI. If needed, figured descriptors were given for patients to choose and the PI or the RAs checked their symptoms. Patients' pain or discomfort anywhere in the chest was coded as a chest pain. Severity of chest pain or discomfort during the acute phase was asked and recoded on a 1-10 scale. Patients were also asked about risk factors, their chronic disease, and past/family history questions. Data for clinical outcomes including MACE and mortality were also obtained at the 1-year follow-up period. All clinical events were verified through the EMR or telephone follow-up calls by a research nurse. Data for 391 patients were used for analysis.
Statistical analysis
All acute symptoms of patients were coded as a categorical variable; 1 point was given for 'present' and 0 points for 'none'. The coded symptoms in the Statistical Package for the Social Sciences (SPSS, SPSS Inc., Chicago, IL, USA) data set were analyzed by Latent class (LC) cluster analysis using Latent GOLD software, version 3.0.13) Cluster analysis is defined as the classification of similar objects into the form of groups, which refers to the parameters of cluster; that is, to its cluster-specific means, variances, and covariances that have a geometrical interpretation.13) LC cluster analysis is a statistical model-based clustering technique and can include covariates to predict class membership. An individual's posterior class-membership probabilities are computed from the estimated model parameters and his observed scores using the maximum likelihood method. The most popular set of model selection tools in LC cluster analysis are information criteria such as Akaike Information Criterion (AIC) and the Bayesian Information Criterion (BIC).14) In this study, decreases in the values of BIC and AIC were minimal between the three- and four-cluster models. Thus, we decided to adopt a 3-cluster model. The cluster membership of 3 clusters was conversed to an SPSS data set to identify the membership and associated factors. Bivariate analyses using χ2-tests, t-tests, and analysis of variance were conducted to identify the relationship between cluster assignment and patients' characteristics. Cox proportional hazards regression analysis was used to test a cluster membership as an independent predictor of 1-year mortality and MACEs. Age was included and controlled for in the multivariate models of mortality and MACEs due to aging's known prognostic importance.
Results
Baseline clinical characteristics
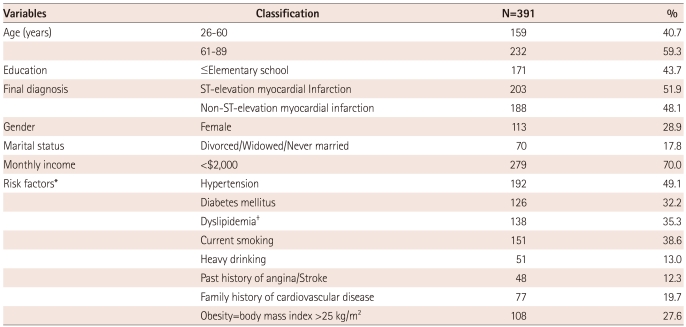
The majority of patients (71.1%) were men and the average age was 63.8±10.3 years (range 26-89). About 52% of the patients were finally diagnosed with STEMI. Of the sample, 49.1% had hypertension and 32.2% had diabetes (average lengths of periods 8.4±7.3 and 11.8±9.7 years). About one third of patients (35.3%) had a dyslipidemia and 38.6% were current smokers. About 12% of the patients had a past history of angina or stroke, and 19.7% had a family history of CVD including hypertension, stroke or ischemic heart disease (Table 1).
Table 1.
Baseline clinical characteristics
*Answers were duplicated, †Dyslipidemia includes one of the following cases: low density lipoprotein >130 mg/dL, high density lipoprotein <40 mg/dL, Total cholesterol >200 mg/dL, and triglyceride >150 mg/dL
Symptom clusters and associated variables
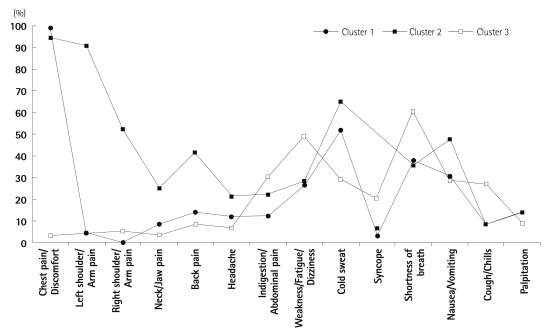
Three distinct clusters of acute symptoms were identified using LC cluster analysis. The size of Cluster 1 was the biggest (n=223, 57.0%), followed by Cluster 2 (n=109, 27.9%) and Cluster 3 (n=59, 15.1%). Symptom distributions by the 3 clustered groups aere shown in Fig. 1. All cluster membership within each symptom cluster was significantly different (p<0.01) except palpitation (p=0.527). The patients in Cluster 1 and Cluster 2 experienced a high frequency of chest pain/discomfort (100% and 94.5%, respectively) and a moderate cold sweating. Among the three groups, Cluster 3 had the least chest pain and moderate frequencies of shortness of breath and weakness or fatigue. We named Cluster 1, 2, and 3 as typical chest pain, multiple symptoms, and atypical symptom clusters, respectively.
Fig. 1.
Symptom distribution by clustered groups.
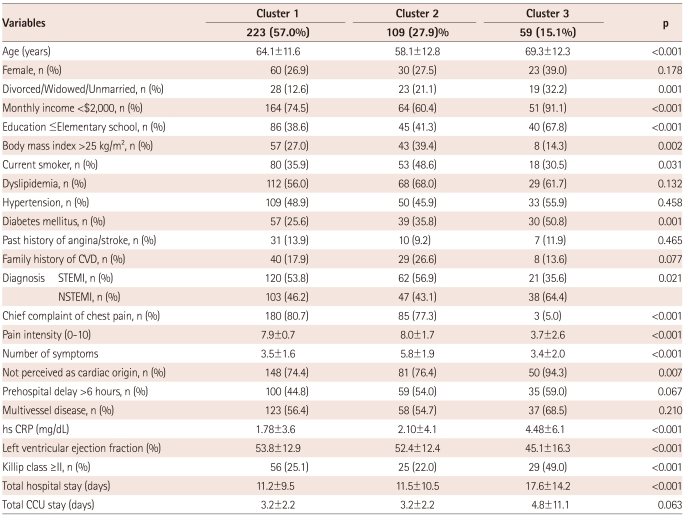
Bivariate analyses showed that patients of Cluster 2 were the youngest (58.1±12.8 years) and those of Cluster 3 were the oldest (69.3±12.3 years) among the three clusters (p<0.001). There were no gender differences in symptom clusters. As for CVD risk factors, the patients of Cluster 2 were more likely to be overweight BMI >25 kg/m2 (p=0.002) and current smokers (p=0.031), and the patients of Cluster 3 were more likely to have diabetes (p<0.001). 94.3% of Cluster 3 reported that they did not perceive their symptoms as cardiac in origin and they had the fewest complaints of acute symptoms and the lowest self-reported intensity score of chest pain among the three groups (p<0.001). The patients of Cluster 3 had the highest value for high sensitivity C-reactive protein (hs-CRP) and the lowest in left ventricular ejection fraction (LVEF), which were checked immediately after hospital admission; they had the longest stay at hospital among the three groups (p<0.001) (Table 2).
Table 2.
Relationships between cluster membership and sample characteristics
CVD: cardiovascular disease, STEMI: ST-elevation myocardial infarction, NSTEMI: non-ST-elevation myocardial infarction, hs-CRP: high sensitivity C-reactive protein, CCU: coronary care unit
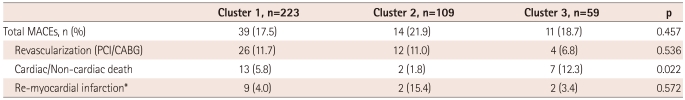
Clinical outcome by symptom clusters during 1-year of follow-up
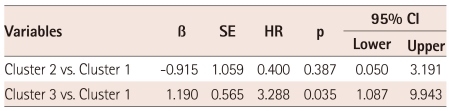
A total of 64 MACEs occurred during the 1-year follow-up period. Bivariate analysis revealed that there was no significant difference among clustered groups in the prevalence of MACEs including an AMI re-attack and total vessel or lesion revascularization. However, the prevalence of cardiac or non-cardiac deaths turned out to be significantly different by clusters (p=0.022) (Table 3). Multivariate Cox proportional hazards regression analysis demonstrated that when age, marital status and monthly income were adjusted for, patients in Cluster 3 predicted a significantly higher risk of 1-year mortality compared to those in Cluster 1, a typical chest pain cluster (hazard ratio 3.288, 95% confidence interval 1.087-9.943, p=0.035) (Table 4).
Table 3.
Major adverse cardiac events (MACEs) at 1-year follow-up by symptom clusters
*Incidences were duplicated with the ones of revascularization. Three cases of non-cardiac death were included. PCI: percutaneous coronary intervention, CABG: coronary artery bypass graft
Table 4.
Cox proportional hazards regression modeling of 1-year mortality by symptom clusters: adjusted for age, marital status and monthly income
HR: hazard ratio or Exp (B); Cluster 1 is a reference group. Prevalence of mortality included cardiac and non-cardiac deaths, SE: standard error
Discussion
Three clusters of acute symptoms in this study were consistent with previous studies of 1) 1270 AMI women that was made up of older/silent asymptomatic, diverse/mildly symptomatic, and younger/multiple distressing symptom groups,10) and of 2) 247 ACS elderly people that had classic, weary (severe fatigue and shortness of breath), and diffuse symptoms.11) However, four or five groupings were also reported and this grouping differed by a target population, number of examined symptoms, or statistical methods.9),15)
About 97% (56/57) of patients in Cluster 3, the atypical symptom cluster, did not experience any pain or discomfort anywhere but the chest. In addition, they reported the least pain intensity among the three clusters, and instead were more likely to have gastrointestinal symptoms, weakness and syncope compared to the other two clusters. Absence of chest pain led patients to delay the decision to seek medical help. It was also challenging for clinicians in triage to decide on a cardiac diagnosis.4),5)
This delayed decision to seek care in this study was supported by the fact that the majority of the patients in Cluster 3 did not attribute their symptoms to a cardiac origin until they went to the hospital. Failure to recognize the symptoms correctly as cardiac problems was consistently recognized as a significant predicting factor for prehospital delay by lots of nursing researchers.16)-18) In this study, 16.1% of the sample had no chest pain, while previous studies showed that about 9-20% of an international sample9),19) and 9% of a Korean sample experienced no chest pain.20)
Atypical symptoms at the hospital presentation were found in many clinical studies as a significant factor predicting lower use of thrombolytic therapy and adverse hospital outcomes.4),5) The present study also supports the view that the rate of all-causes of death (7/59, 12.3%) in Cluster 3 is significantly higher than that of the other clusters (<6%). This finding might be explained by older age compared to the other clusters. The patients who belonged to Cluster 3 were significantly older than those of the other two clusters. Only 5% of them referred to chest pain as a chief complaint at hospital presentation. This was consistent with a previous study that older AMI patients were less likely to report classic pain and used fewer words to describe their discomfort compared with younger patients.4) This result was also supported by a recent study on older adults (>65 years) based on symptoms they had experienced for a week prior to an acute event showing that fatigue emerged in all three clusters with an overall prevalence of 76.1%, while chest pain was experienced by only 56% of patients.11) The characteristics represented in Cluster 3 were similar to the diffuse symptom cluster that was identified among 331 patients with ACS by Riegel and her colleagues.15) They reported that the diffuse symptom group with a low frequency of symptoms tended to be older than other groups. This finding supports the need for an increased index of supervision for patients with an atypical symptom presentation.
The 10.3% (21/203) of patients with ST-elevation myocardial infarction (STEMI) belonged to Cluster 3, the atypical symptom group, in this study. We should have greater concern for these STEMI patients with atypical presentation to increase their awareness of the benefit of rapid reperfusion therapy. Further research would then be needed to examine the associations between symptom clusters and characteristics especially for STEMI patients, to provide a useful guideline for early recognition of the symptoms during an acute coronary event.
About 51% of the patients in Cluster 3 had a history of diabetes and this was significantly higher compared to the other two clusters. This finding was supported by previous studies demonstrating that AMI patients with atypical symptoms were more likely to be older, female, and diabetic.1),5),21) Therefore, older adults at high risk for CVD, especially those who have diabetes, should pay more attention to their risks of developing AMI and should engage in health-seeking behaviors when unusual symptoms occur.
Clinical outcomes were also significantly worse in patients with Cluster 3. The values of hs-CRP, LVEF, and Killip class were significantly increased and total length of hospital stay was significantly longer in those in the atypical symptom cluster. When age and socio-economic status were adjusted for, although the prevalence of MACEs was not different, the atypical symptom cluster predicted a 3.3 times higher risk of 1-year mortality compared with the typical chest pain cluster. This is consistent with a previous cluster study showing that the patients in the diffuse symptom group had significantly higher mortality at 2 years than those with the other three cluster groups in ACS patients (17% vs. 2-5%).15) These findings support the view that intensive medical treatments are needed for AMI patients with atypical presentations, especially for those who are old and diabetic. However, Riegel's study used a secondary data set, which was obtained from 5 multi-centers during a 2-year follow-up period for known CVD patients including history of AMI and care of a cardiologist.15) This limits direct comparisons with our study, which was conducted in first-time AMI patients through a direct interview at one hospital. Further longitudinal research is needed to replicate and verify the differences in clinical outcome among symptom cluster groups.
Classic symptoms characterized by chest pain and associated symptoms were presented dominantly by Clusters 1 and 2, and the patients of Cluster 2 who were the youngest complained of the largest number of acute symptoms. This finding was consistent with previous observational and cluster studies showing that classic chest symptom was a predictive factor of ACS in younger patients <70 years.1),9),21) They were more likely to be obese, current smokers, and to have dyslipidemia compared to other cluster groups. This supports the conclusion that it is essential to manage individuals with those risk factors to prevent CVD in younger adults.
Limitations of this study
This study has limitations. The study sample was collected conveniently from one hospital located in a city. Therefore, the study population cannot be considered as representative of all AMI patients in Korea. Other limitations include the retrospective nature of the study and the fact that patient information involved personal recollections.
Conclusions
We have identified three distinct clusters among 14 acute symptoms; typical chest pain, multiple symptom, and atypical symptom clusters. The patients with the atypical symptom cluster, which contained older and more diabetic patients, had worse clinical markers at hospital presentation and significantly higher mortality rates within the 1-year of follow-up compared to those in the other two clusters. This study poses a challenge to healthcare providers: how to utilize the symptom cluster to identify common symptom patterns and to develop educational strategies that may facilitate rapid identification of AMI. Also, we recommend that clinicians treat more intensively older AMI patients who have vague or atypical symptoms at hospital presentation.
Acknowledgments
This study was sponsored by research fund from Chosun University, 2011.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Milner KA, Funk M, Richards S, Vaccarino V, Krumholz HM. Symptom predictors of acute coronary syndromes in younger and older patients. Nurs Res. 2001;50:233–241. doi: 10.1097/00006199-200107000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Leslie WS, Urie A, Hooper J, Morrison CE. Delay in calling for help during myocardial infarction: reasons for the delay and subsequent pattern of accessing care. Heart. 2000;84:137–141. doi: 10.1136/heart.84.2.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Horne R, James D, Petrie K, Weinman J, Vincent R. Patients' interpretation of symptoms as a cause of delay in reaching hospital during acute myocardial infarction. Heart. 2000;83:388–393. doi: 10.1136/heart.83.4.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Canto JG, Shlipak MG, Rogers WJ, et al. Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. JAMA. 2000;283:3223–3229. doi: 10.1001/jama.283.24.3223. [DOI] [PubMed] [Google Scholar]
- 5.Brieger D, Eagle KA, Goodman SG, et al. Acute coronary syndromes without chest pain, an underdiagnosed and undertreated high-risk group: insights from the Global Registry of Acute Coronary Events. Chest. 2004;126:461–469. doi: 10.1378/chest.126.2.461. [DOI] [PubMed] [Google Scholar]
- 6.Barsevick AM, Whitmer K, Nail LM, Beck SL, Dudley WN. Symptom cluster research: conceptual, design, measurement, and analysis issues. J Pain Symptom Manage. 2006;31:85–95. doi: 10.1016/j.jpainsymman.2005.05.015. [DOI] [PubMed] [Google Scholar]
- 7.Dodd M, Janson S, Facione N, et al. Advancing the science of symptom management. J Adv Nurs. 2001;33:668–676. doi: 10.1046/j.1365-2648.2001.01697.x. [DOI] [PubMed] [Google Scholar]
- 8.Miaskowski C, Dodd M, Lee K. Symptom clusters: the new frontier in symptom management research. J Natl Cancer Inst Monogr. 2004;32:17–21. doi: 10.1093/jncimonographs/lgh023. [DOI] [PubMed] [Google Scholar]
- 9.Ryan CJ, DeVon HA, Horne R, et al. Symptom clusters in acute myocardial infarction: a secondary data analysis. Nurs Res. 2007;56:72–81. doi: 10.1097/01.NNR.0000263968.01254.d6. [DOI] [PubMed] [Google Scholar]
- 10.McSweeney JC, Cleves MA, Zhao W, Lefler LL, Yang S. Cluster analysis of women's prodromal and acute myocardial infarction symptoms by race and other characteristics. J Cardiovasc Nurs. 2010;25:311–322. doi: 10.1097/JCN.0b013e3181cfba15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lindgren TG, Fukuoka Y, Rankin SH, Cooper BA, Carroll D, Munn YL. Cluster analysis of elderly cardiac patients' prehospital symptomatology. Nurs Res. 2008;57:14–23. doi: 10.1097/01.NNR.0000280654.50642.1a. [DOI] [PubMed] [Google Scholar]
- 12.Fukuoka Y, Lindgren TG, Rankin SH, Cooper BA, Carroll DL. Cluster analysis: a useful technique to identify elderly cardiac patients at risk for poor quality of life. Qual Life Res. 2007;16:1655–1663. doi: 10.1007/s11136-007-9272-7. [DOI] [PubMed] [Google Scholar]
- 13.Vermunt JK, Magidson J. Latent Gold user's guide. Belmont: Statistical Innovations; 2000. [Google Scholar]
- 14.Fraley C, Raftery AE. How many clusters? Which clustering method? Answers via model-based cluster analysis. Comput J. 1998;41:578–588. doi: 10.1093/comjnl/41.8.578. [Google Scholar]
- 15.Riegel B, Hanlon AL, McKinley S, et al. Differences in mortality in acute coronary syndrome symptom clusters. Am Heart J. 2010;159:392–398. doi: 10.1016/j.ahj.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thuresson M, Jarlöv MB, Lindahl B, Svensson L, Zedigh C, Herlitz J. Thoughts, actions, and factors associated with prehospital delay in patients with acute coronary syndrome. Heart Lung. 2007;36:398–409. doi: 10.1016/j.hrtlng.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 17.Moser DK, Kimble LP, Alberts MJ, et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on Cardiovascular Nursing and Stroke Council. Circulation. 2006;114:168–182. doi: 10.1161/CIRCULATIONAHA.106.176040. [DOI] [PubMed] [Google Scholar]
- 18.Hwang SY. Comparison of clinical manifestations and treatment-seeking behaviors in younger and older patients with first-time acute coronary syndrome. J Korean Acad Nurs. 2009;39:888–898. doi: 10.4040/jkan.2009.39.6.888. [DOI] [PubMed] [Google Scholar]
- 19.Berg J, Björck L, Dudas K, Lappas G, Rosengren A. Symptoms of a first acute myocardial infarction in women and men. Gend Med. 2009;6:454–462. doi: 10.1016/j.genm.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 20.Hwang SY, Park EH, Shin ES, Jeong MH. Comparison of factors associated with atypical symptoms in younger and older patients with acute coronary syndromes. J Korean Med Sci. 2009;24:789–794. doi: 10.3346/jkms.2009.24.5.789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Then KL, Rankin JA, Fofonoff DA. Atypical presentation of acute myocardial infarction in 3 age groups. Heart Lung. 2001;30:285–293. doi: 10.1067/mhl.2001.116010. [DOI] [PubMed] [Google Scholar]