Abstract
Capsaicin is the spice component of red pepper. It can be easily inhaled, inducing a reproducible cough and provokes a secretory response from the human nasal mucosa. To date, there has been no report of occupational rhinitis (OR) caused by capsaicin. We report the case of a 44-year-old female mill worker who developed occupational rhinitis after 4 years of exposure to capsaicin. She developed nasal congestion, rhinorrhea, and itchy nose, which were all aggravated upon exposure at the workplace. The patient had negative responses to all common inhalant allergens, including capsaicin, by skin prick tests. The nasal provocation test with capsaicin showed that the nasal symptom score and eosinophil count increased 10 minutes after the provocation and decreased after 1 to 3 hours; no significant response was noted to house dust mite allergen. The patient's work-related rhinitis improved 1 month after she relocated and started pharmacological treatment. To our knowledge, this is the first case of OR caused by capsaicin exposure in the workplace. We provide evidence suggesting that OR may be mediated by a non-immunological mechanism.
Keywords: Occupational rhinitis, capsaicin
INTRODUCTION
Capsaicin is the spice extract of red peppers and is easily inhaled, causing a dose-dependent and reproducible cough.1 In the laboratory, capsaicin is often used to measure the sensitivity of the cough reflex. It is also one of the most widely used seasonings in Korea. Occupational rhinitis (OR) is two to four times more common than occupational asthma (OA)2 and may be a risk factor for developing OA, although the contribution of workplace exposure to the general burden of rhinitis remains unknown.3 To date, there has been no published report of OR caused by capsaicin. Here, we describe for the first time a case of capsaicin-induced OR confirmed by a nasal provocation test in a mill worker.
CASE REPORT
A 44-year-old female visited our allergy clinic for progressive nasal congestion, rhinorrhea, and itchy nose. She had no history of allergic diseases or chronic medical illness. She had worked at a mill for 7 years, grinding red pepper; during that time, she was exposed to red pepper powder. Her rhinitis symptoms developed 4 years after starting her job; she had no symptoms prior to the job. Her symptoms began at the start of each work day, were more aggravated upon exposure to red pepper powder, and subsided once outside of the workplace. At presentation, blood cell differential count, serum biochemistry, total IgE (48 kU/L), and chest and paranasal sinus radiographs were normal. Nasal endoscopic findings included inferior turbinate hypertrophy with swollen mucosa; there was no evidence of nasal polyps or any other paranasal sinus disease. The patient had negative responses to all common inhalant allergens (Bencard, Bradford, UK), including capsaicin (0.1, 1, 10 mg/mL; Sigma-Aldrich, St. Louis, MO, USA), as determined by skin prick tests. Eosinophils were not present in the patient's sputum or nasal smear samples collected at her initial visit.
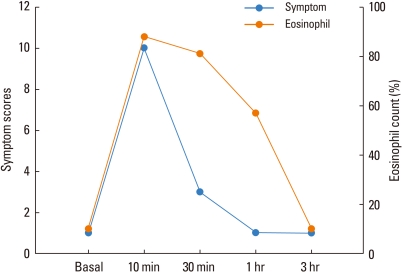
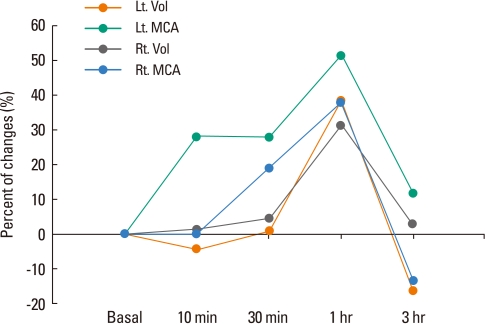
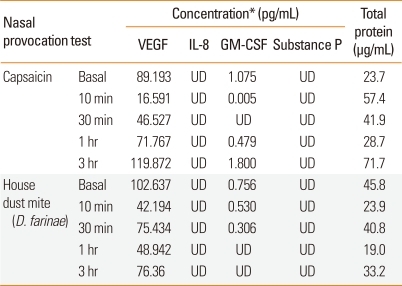
Nasal provocation tests with nasal lavage were performed using capsaicin allergen. Nasal symptom scores and eosinophil counts in the nasal lavage fluid at 10 minutes, 30 minutes, 1 hour, and 3 hours after the provocation test were compared with the baseline values measured before the provocation test. After 10 minutes of exposure to 0.1 µM capsaicin, the patient's nasal symptom score increased and was maintained until 30 minutes, at which point the symptom score decreased; no late response was observed. Eosinophil counts in the nasal lavage fluid increased at 10 minutes, was maintained until 30 minutes, and had decreased at the 1 and 3 hours time points (Fig. 1). The volume and minimum cross-sectional area of the nasal cavity, measured by acoustic rhinometry (ARS 1003; SGS, North Miami Beach, FL, USA), decreased by >25% from 10 minutes until 1 hour after nasal provocation (Fig. 2). As a control, the patient had a negative response to nasal provocation with Dermatophagoides farinae allergen (i.e., house dust mites). There were no significant changes in the levels of four inflammatory mediators, i.e., vascular endothelial growth factor (VEGF), granulocyte-macrophage colony-stimulating factor (GM-CSF), interleukin-8 (IL-8), and substance P (SP), in the nasal lavage fluid during the nasal provocation test (Table).
Fig. 1.
Changes in the nasal symptom score and eosinophil count in the nasal lavage fluid collected from our patient during the nasal provocation test with capsaicin.
Fig. 2.
Changes in the volume (vol) and minimum cross-sectional area (MCA) of the patient's nasal cavity, as measured by acoustic rhinometry, during the nasal provocation test with capsaicin.
Table.
Laboratory data of the nasal lavage fluid collected from our patient during nasal provocation tests with capsaicin and Dermatophagoides farinae allergen
*As measured by enzyme-linked immunosorbent assay; VEGF, vascular endothelial growth factor; IL-8, interleukin-8; GM-CSF, granulocyte-macrophage colony-stimulating factor; UD, undetectable.
The final diagnosis was OR caused by capsaicin. The patient's rhinitis improved after she transferred out of her workplace and started treatment with antihistamines and intranasal corticosteroids.
DISCUSSION
Occupational allergic diseases such as OR are common, and their prevalence among the workforce is on the rise. Cross-sectional studies have determined that the incidence of OR caused by high-molecular-weight agents such as animal-derived allergens, grain dust, and biological enzymes ranges from 2% to 87%, and the incidence of OR caused by low-molecular-weight agents such as diisocyanates, anhydrides, drugs, and chemicals ranges from 3% to 48%.2,3 OR and other allergic diseases have profound effects on workers, resulting in performance deficits, reduced productivity, and psychosocial problems.1 In our study, the patient developed OR symptoms 4 years after starting her pepper mill job. Nasal provocation tests with capsaicin were positive, with increased eosinophils in the nasal lavage fluid, while the control provocation test with house dust mite allergen was negative. Therefore, we concluded that the patient had OR caused by capsaicin exposure from her workplace.
Capsaicin is a neurotoxin capable of stimulating and/or desensitizing sensory neuron C-fibers by activating the transient potential receptor vanilloid 1 (TRPV1).4 In animal models, capsaicin releases neuropeptides and induces neurogenic inflammation, including vasodilation and plasma extravasation.5 However, most clinical studies have shown that capsaicin provokes a secretory response in the absence of vascular permeability,3,6 and there is no direct evidence of the release of neuropeptides such as SP, calcitonin gene-related peptide, or vasoactive intestinal peptide in human nasal mucosa.7
Neuropeptides induce neutrophil adhesion, stimulate the proliferation of human T lymphocytes, and increase inflammatory cytokines.7 Therefore, the leukocyte influx induced by capsaicin may be a nonspecific inflammatory cellular response,8 although it is unclear whether neurogenic inflammation actually occurs in human subjects.9,10 One study concluded that capsaicin caused nasal symptoms and glandular stimulation, without evidence of increased vascular permeability or mast cell activation.11 More recent studies have suggested that C-fibers themselves, not TRPV1, play a role in allergic airway inflammation.12,13 Capsaicin has also been demonstrated to have TRPV1-independent effects, including ion channel activity14 and calcium influx.15 Calcium is a powerful stimulus for cell activation and is critical in regulating cellular activities. In a few studies, capsaicin nasal challenge resulted in neurogenic inflammation in patients with allergic rhinitis.16,17 In the present study, a nasal provocation test with capsaicin induced symptom development and an immediate increase in eosinophils in the nasal lavage fluid, whereas allergy skin tests with capsaicin solution were negative. Furthermore, epithelial cell-derived cytokines such as GM-CSF, VEGF, IL-8, and SP were not detected in the nasal lavage fluid collected during the nasal provocation test with capsaicin or house dust mite allergen. We cannot speculate about the mechanism of eosinophil activation after capsaicin exposure in this patient, but a non-IgE mediated response may be involved.
In conclusion, we report the first published case of OR induced by capsaicin, as confirmed by a nasal provocation test, in a pepper mill worker.
ACKNOWLEDGMENTS
This study was supported by the Korea Science and Engineering Foundation (KOSEF) and a grant from the Korean government (MEST, 2009-007864).
Footnotes
There are no financial or other issues that might lead to conflict of interest.
References
- 1.Dicpinigaitis PV. Short- and long-term reproducibility of capsaicin cough challenge testing. Pulm Pharmacol Ther. 2003;16:61–65. doi: 10.1016/S1094-5539(02)00149-9. [DOI] [PubMed] [Google Scholar]
- 2.Siracusa A, Desrosiers M, Marabini A. Epidemiology of occupational rhinitis: prevalence, aetiology and determinants. Clin Exp Allergy. 2000;30:1519–1534. doi: 10.1046/j.1365-2222.2000.00946.x. [DOI] [PubMed] [Google Scholar]
- 3.Moscato G, Vandenplas O, Van Wijk RG, Malo JL, Perfetti L, Quirce S, Walusiak J, Castano R, Pala G, Gautrin D, De Groot H, Folletti I, Yacoub MR, Siracusa A. EAACI position paper on occupational rhinitis. Respir Res. 2009;10:16. doi: 10.1186/1465-9921-10-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wolf G, Anderhuber W, Hauser-Kronberger C, Saria A. Treatment of nonspecific hyper-reflectory rhinopathy (vasomotor rhinitis) with capsaicin. Laryngorhinootologie. 1995;74:289–293. doi: 10.1055/s-2007-997742. [DOI] [PubMed] [Google Scholar]
- 5.Didier A, Kowalski ML, Jay J, Kaliner MA. Neurogenic inflammation, vascular permeability, and mast cells. Capsaicin desensitization fails to influence IgE-anti-DNP induced vascular permeability in rat airways. Am Rev Respir Dis. 1990;141:398–406. doi: 10.1164/ajrccm/141.2.398. [DOI] [PubMed] [Google Scholar]
- 6.Thong BY. Update on the management of antibiotic allergy. Allergy Asthma Immunol Res. 2010;2:77–86. doi: 10.4168/aair.2010.2.2.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stjärne P, Rinder J, Hedén-Blomquist E, Cardell LO, Lundberg J, Zetterström O, Anggård A. Capsaicin desensitization of the nasal mucosa reduces symptoms upon allergen challenge in patients with allergic rhinitis. Acta Otolaryngol. 1998;118:235–239. doi: 10.1080/00016489850154955. [DOI] [PubMed] [Google Scholar]
- 8.Philip G, Sanico AM, Togias A. Inflammatory cellular influx follows capsaicin nasal challenge. Am J Respir Crit Care Med. 1996;153:1222–1229. doi: 10.1164/ajrccm.153.4.8616545. [DOI] [PubMed] [Google Scholar]
- 9.Barnes PJ. Neurogenic inflammation and asthma. J Asthma. 1992;29:165–180. doi: 10.3109/02770909209099025. [DOI] [PubMed] [Google Scholar]
- 10.Kim D, Baraniuk JN. Neural aspects of allergic rhinitis. Curr Opin Otolaryngol Head Neck Surg. 2007;15:268–273. doi: 10.1097/MOO.0b013e328259c372. [DOI] [PubMed] [Google Scholar]
- 11.Bascom R, Kagey-Sobotka A, Proud D. Effect of intranasal capsaicin on symptoms and mediator release. J Pharmacol Exp Ther. 1991;259:1323–1327. [PubMed] [Google Scholar]
- 12.Seitz CS, Bröcker EB, Trautmann A. Diagnostic testing in suspected fluoroquinolone hypersensitivity. Clin Exp Allergy. 2009;39:1738–1745. doi: 10.1111/j.1365-2222.2009.03338.x. [DOI] [PubMed] [Google Scholar]
- 13.Sachs B, Riegel S, Seebeck J, Beier R, Schichler D, Barger A, Merk HF, Erdmann S. Fluoroquinolone-associated anaphylaxis in spontaneous adverse drug reaction reports in Germany: differences in reporting rates between individual fluoroquinolones and occurrence after first-ever use. Drug Saf. 2006;29:1087–1100. doi: 10.2165/00002018-200629110-00008. [DOI] [PubMed] [Google Scholar]
- 14.Fujimoto S, Mori M, Tsushima H, Kunimatsu M. Capsaicin-induced, capsazepine-insensitive relaxation of the guinea-pig ileum. Eur J Pharmacol. 2006;530:144–151. doi: 10.1016/j.ejphar.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 15.Fujimoto S, Mori M. Characterization of capsaicin-induced, capsazepine-insensitive relaxation of ileal smooth muscle of rats. Eur J Pharmacol. 2004;487:175–182. doi: 10.1016/j.ejphar.2004.01.014. [DOI] [PubMed] [Google Scholar]
- 16.Roche N, Lurie A, Authier S, Dusser DJ. Nasal response to capsaicin in patients with allergic rhinitis and in healthy volunteers: effect of colchicine. Am J Respir Crit Care Med. 1995;151:1151–1158. doi: 10.1164/ajrccm.151.4.7697245. [DOI] [PubMed] [Google Scholar]
- 17.Sanico AM, Atsuta S, Proud D, Togias A. Dose-dependent effects of capsaicin nasal challenge: in vivo evidence of human airway neurogenic inflammation. J Allergy Clin Immunol. 1997;100:632–641. doi: 10.1016/s0091-6749(97)70167-2. [DOI] [PubMed] [Google Scholar]