Abstract
Background
In previous studies, psoriasis has been reported to be associated with metabolic syndrome.
Objective
The purpose of this study was to evaluate risk factors for metabolic syndrome in psoriasis patients and to compare the prevalence of metabolic syndrome in psoriasis and control groups.
Methods
All patients (n=490) and controls (n=682) were investigated for cardiovascular risk factors, including central obesity, hypertension, fasting plasma glucose levels, and blood levels of triglycerides and high-density lipoprotein (HDL).
Results
We found no statistical association between psoriasis and the prevalence of metabolic syndrome when controlling for age and gender. Among individual components of metabolic syndrome, only increased triglyceride levels was significantly prevalent in patients psoriasis. The incidence of other factors such as central obesity, hypertension, fasting plasma glucose and HDL in the psoriasis group were similar to or lower than those in the control group. Although psoriasis patients with metabolic syndrome had severe and large plaque-type psoriasis, the association of metabolic syndrome with the severity or clinical subtype of psoriasis was not significant after adjusting for age and gender.
Conclusion
Our results suggest that there is no close correlation between psoriasis and metabolic syndrome in Korean patients.
Keywords: Cardiovascular risk, Metabolic syndrome, Psoriasis
INTRODUCTION
Recent studies have reported that psoriasis is associated with metabolic disorders, including obesity, dyslipidemia, and diabetes1-3. Moreover, psoriasis has been shown to be an independent risk factor for myocardial infarction, particularly in young patients, and severe psoriasis has been shown to be associated with increased mortality in patients with cardiovascular disease4-6.
Metabolic syndrome, which is called insulin resistance syndrome or syndrome X, is a combination of cardiovascular risk factors, including central obesity, hypertension, glucose intolerance, and dyslipidemia7. This comprehensive concept of metabolic syndrome is of clinical significance because it can be a strong predictor of cardiovascular diseases, diabetes, and stroke8,9.
Although the number of reports about the relationship of psoriasis with metabolic syndrome has been increasing in western countries, such reports are rare in Korea. Therefore, we investigated the association of psoriasis with cardiovascular risk factors and the prevalence of metabolic syndrome in Korean patients with psoriasis.
MATERIALS AND METHODS
Patients and controls
The subjects of this study were 490 patients with psoriasis who visited the Department of Dermatology at the Pusan National University Hospital between 1999 and 2009. Only patients over 18 years of age were included in the study. The severity of psoriasis was assessed using Molin's classification10, which is based on the body surface area affected by psoriasis: mild, <5% of the surface area; moderate, 5~30%; and severe, >30%. Clinical subtypes of psoriasis were classified on the basis of the suggestion of Youn and Jo11. While nummular-type and large plaque-type psoriasis were included in this study, other types such as guttate-type, erythrodermic, and generalized pustular psoriasis, and palmoplantar pustulosis were not. The following criteria should be satisfied for the classification of nummular type: chronic course in older patients, larger cutaneous lesions (typically 1~2 cm), and absence of pre-existing staphylococcal infections.
The exclusion criteria were as follows: patients who had secondary hyperlipidemia (hypothyroidism, nephrotic syndrome, chronic renal insufficiency, obstructive liver disease, and connective tissue disease); patients using medications affecting carbohydrate and lipid metabolism (beta blockers, thiazides, corticosteroids, and lipid-lowering agents); patients with infectious diseases; and patients who were pregnant and breastfeeding. Controls were selected from the Health Promotion Center of the Pusan National University Hospital from May to July 2009. They had no underlying hepatic and renal disorders or infectious diseases.
Data collection
1) Investigation of cardiovascular risk factors
The charts of all patients were reviewed to identify the presence of chronic internal diseases, including diabetes mellitus and hypertension. Triglyceride and high-density lipoprotein (HDL)-cholesterol levels were investigated from the initial blood test. In addition, clinical data, including weight, height, body mass index (BMI), and waist circumference, were collected using telephone surveys. Furthermore, a recent history of diabetes and hypertension and data regarding blood glucose levels and blood pressure measured in the most recent test were collected, again during the telephone surveys. On the basis of this investigation, we assessed the presence of obesity, hypertension, and high fasting plasma glucose levels and blood levels of triglycerides and HDL-cholesterol.
2) Definition of metabolic syndrome
The criteria for diagnosing metabolic syndrome were obtained from the National Cholesterol Education Program's Adult Panel III, and visceral obesity was defined by substituting it with BMI or the standard waist circumference in the Asia-Pacific Region. Diagnosis was confirmed when 3 or more of the following criteria were satisfied: central obesity (BMI >30 kg/m2 or waist circumference ≥36 inch for men and ≥32 inch for women), hypertension (≥130/85 mmHg), high fasting plasma glucose (≥110 mg/dl), increased triglycerides (≥ 150 mg/dl), and decreased HDL (<40 mg/dl for men and <50 mg/dl for women).
Comparison of cardiovascular risk factors and metabolic syndrome
1) Psoriasis group vs. control group
After controlling for confounding factors such as age and gender, we analyzed and compared the prevalence of cardiovascular risk factors and metabolic syndrome between the psoriasis and control groups.
2) Psoriasis patients with metabolic syndrome vs. psoriasis patients without metabolic syndrome
We compared the age, gender, clinical subtypes of psoriasis, and severity of psoriasis between these 2 groups.
Statistical analysis
Statistical comparison of the prevalence of metabolic syndrome in the psoriasis and control groups were performed using analysis of covariance (ANCOVA) for continuous variables and a chi-square test for categorical variables. We performed ANCOVA to control for the effects of age and gender in patients with metabolic syndrome. ANCOVA tests whether certain factors have an effect on the outcome variable after removing the variance that is accounted for by the quantitative predictors. We included age and gender as covariates to increase the statistical power of the analyses conducted in this study. All p-values were two-sided, and p<0.05 was considered statistically significant.
RESULTS
Comparison of cardiovascular risk factors and metabolic syndrome: psoriasis group vs. control group
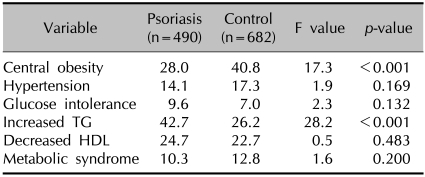
The prevalence of metabolic syndrome between the psoriasis and control groups, after controlling for age and gender, was not significantly different (p=0.200). In addition, intergroup differences in the incidence of hypertension and glucose intolerance and HDL levels were absent (p>0.05). The triglyceride levels in the psoriasis group were higher than those in the control group (p<0.001) (Table 1).
Table 1.
Cardiovascular risk factors and metabolic syndrome in the psoriasis and control groups (adjusting for age and gender, %)
TG: triglyceride, HDL: high density lipoprotein.
Comparison of clinical features between psoriasis patients with metabolic syndrome and those without metabolic syndrome
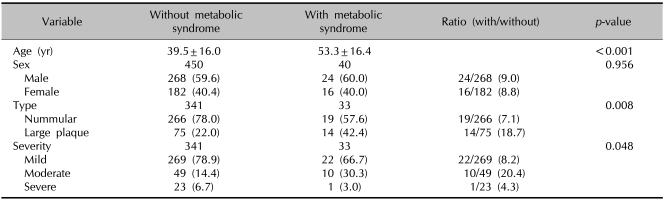
Among the 490 psoriasis patients, 40 had metabolic syndrome and 450 had no metabolic syndrome.
1) Age and gender
Psoriasis patients with metabolic syndrome were older than those without metabolic syndrome (53.3 years vs. 39.5 years; p<0.001). However, there was no significant difference in gender (p=0.956).
2) Clinical subtype (plaque type vs. nummular type) and severity
In patients with nummular-type psoriasis, the ratio between the presence (n=19) and absence (n=266) of metabolic syndrome was 7.1% (n=19/266). However, in patients with large plaque-type psoriasis, the ratio between the presence (n=14) and absence (n=75) of metabolic syndrome was 18.7% (n=14/75) (Table 2).
Table 2.
Comparisons of clinical features according to the presence of metabolic syndrome in psoriasis patients
Values are presented as mean±standard deviation or number (%).
In the assessment of severity, the ratio between the presence and absence of metabolic syndrome was highest in the moderate psoriasis group (20.4%, n=10/49) (Table 2). However, there was no significant difference in the prevalence of metabolic syndrome according to the clinical subtype and severity after controlling for age and gender (p>0.05).
DISCUSSION
Psoriasis is a chronic inflammatory skin disease, and recent reports have increasingly shown the association between psoriasis and cardiovascular disease6. In addition, epidemiological studies in the English language literature have established the direct relationship between psoriasis and metabolic syndrome12,13. However, the relationship between cardiovascular risk factors and metabolic syndrome has not been sufficiently reported in the Korean literature.
Therefore, we conducted a study on metabolic syndrome and cardiovascular risk factors in patients with psoriasis. Our study yielded the following results. First, the prevalence of metabolic syndrome was 10.3% in the psoriasis group (Table 1). Second, our statistical analysis did not show any significant difference in the prevalence of metabolic syndrome between the psoriasis and control groups after controlling for age and gender (p=0.200) (Table 1). Finally, the triglyceride level was higher in the psoriasis group (42.7%) than in the control group (26.2%, p<0.001) (Table 1).
There has been a rapid increase in the number of reports that link psoriasis to cardiovascular disease; however, there have also been some controversies on the relationship between psoriasis and cardiovascular risk, particularly in patients with metabolic syndrome. In addition, only a few studies have investigated the direct relationship between metabolic syndrome and psoriasis1,4,6,14-16. Although Gisondi et al.12 reported that the prevalence of metabolic syndrome was higher in psoriasis patients (30.1%) than in patients with general dermatological conditions (20.6%), the prevalence of hypertriglyceridemia and abdominal obesity-individual components of the metabolic syndrome was significantly greater in patients with psoriasis than in controls. In addition, Sommer et al.13 observed a high prevalence of metabolic syndrome among patients (4.3%) with psoriasis than in controls (1.1%). However, the prevalence of metabolic syndrome in both patients (4.3%) and controls (1.1%) was very low, and the risk of metabolic syndrome was high only in patients with severe psoriasis.
This observation suggests that the occurrence of cardiovascular complications may be restricted to the severe form of psoriasis; however, this finding has not yet been confirmed. Recently, Wakkee et al.17 conducted a large population-based Dutch cohort study and provided additional evidence suggesting that psoriasis or severe psoriasis may not be a relevant risk factor for myocardial infarction. In addition, genetic and racial differences may influence the prevalence of metabolic syndrome. According to Chen et al.18, central obesity, hypertension, and glucose intolerance were more prevalent in Asian patients with psoriasis than in controls. However, the incidence of metabolic syndrome among psoriasis patients (14.1%) was lower than among controls (16.3%).
The National Health Nutrition Examination Survey in Korea analyzed the prevalence of metabolic syndrome in 1998 and 2001, and reported that 22.5% and 24.1% of Korean adults, respectively, had metabolic syndrome19. The prevalence of metabolic syndrome was lower in our psoriasis group (10.3%) than in the groups of the above-mentioned survey and the groups mentioned in a recent study by Lym et al.20 (20~29 years [3.8%]; 30~39 years [13.9%]; 40~49 years [14.8%]; 50~59 years [24.2%]; 60~69 years [27.1%]).
Our results showed that metabolic syndrome was not associated with psoriasis, but our study had several limitations. First, there is a possibility that young patients and those with early disease have been over-polled because this study was aimed at new patients visiting the outpatient clinic. Second, this study was a retrospective study and it might not reflect accurate results. In principle, strict numerical measurements had to be obtained to evaluate the risk factors of metabolic syndrome. However, this study used medical records and telephone surveys to investigate risk factors, and this may have introduced a bias. Psoriasis has a prolonged disease course, and a difference in the prevalence of metabolic syndrome may exist between early manifestation and chronic disease stages. Moreover, questions such as whether psoriasis predisposes the patient to metabolic syndrome and whether metabolic disorders can lead to psoriasis have remained unanswered16. In this study, the investigation involved telephone surveys conducted over a follow-up period of up to 10 years and a comprehensive review of medical histories. This may have helped overcome the limitations of a cross-sectional study. Assuming a relationship between psoriasis and metabolic syndrome, our findings may suggest that the onset of psoriasis leads to the development of metabolic syndrome.
Remarkably, our results showed higher levels of triglycerides in the psoriasis group than in the control group (Table 2). In a cross-sectional study, which compared psoriasis patients with controls, 16,851 psoriasis patients in Israel showed increased total cholesterol and triglycerides, decreased HDL, and no alteration in low-density lipoprotein (LDL)21. Another cross-sectional study conducted in Iran showed that, compared to controls, psoriasis patients have significantly higher levels of triglycerides, total cholesterol, LDL, and very low-density lipoprotein, but no alteration in HDL22. Therefore, we think that careful attention must be paid to dyslipidemia, particularly the triglyceride levels, in psoriasis patients.
In addition, our study produced 3 meaningful results by comparing the two groups on the basis of the presence or absence of metabolic syndrome. First, psoriasis patients with metabolic syndrome (53.3 years) were significantly older than those without metabolic syndrome (39.5 years) (p<0.001). Second, plaque-type psoriasis was much more common in patients with metabolic syndrome than in those without metabolic syndrome. Finally, patients with metabolic syndrome had more severe psoriasis than those without metabolic syndrome, as estimated on the basis of the body surface area (p=0.048) (Table 2).
This large-scale, long-term study investigated cardiovascular risk factors in Korean patients. Although we did not find any significant differences in the prevalence of metabolic syndrome between psoriasis patients and controls, the results of our study suggest that patient age and severity of psoriasis are predisposing factors for metabolic syndrome. Thus, special care must be taken in the case of elderly patients with plaque-type psoriasis. In addition, triglyceride levels showed significant correlations with psoriasis in this study, and hence plasma lipid profiling should be routinely conducted.
Footnotes
This study was supported by Medical Research Institute Grant (2011-8), Pusan National University Hospital.
References
- 1.Neimann AL, Shin DB, Wang X, Margolis DJ, Troxel AB, Gelfand JM. Prevalence of cardiovascular risk factors in patients with psoriasis. J Am Acad Dermatol. 2006;55:829–835. doi: 10.1016/j.jaad.2006.08.040. [DOI] [PubMed] [Google Scholar]
- 2.Mallbris L, Ritchlin CT, Ståhle M. Metabolic disorders in patients with psoriasis and psoriatic arthritis. Curr Rheumatol Rep. 2006;8:355–363. doi: 10.1007/s11926-006-0065-8. [DOI] [PubMed] [Google Scholar]
- 3.Henseler T, Christophers E. Disease concomitance in psoriasis. J Am Acad Dermatol. 1995;32:982–986. doi: 10.1016/0190-9622(95)91336-x. [DOI] [PubMed] [Google Scholar]
- 4.Wakkee M, Thio HB, Prens EP, Sijbrands EJ, Neumann HA. Unfavorable cardiovascular risk profiles in untreated and treated psoriasis patients. Atherosclerosis. 2007;190:1–9. doi: 10.1016/j.atherosclerosis.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 5.Gelfand JM, Neimann AL, Shin DB, Wang X, Margolis DJ, Troxel AB. Risk of myocardial infarction in patients with psoriasis. JAMA. 2006;296:1735–1741. doi: 10.1001/jama.296.14.1735. [DOI] [PubMed] [Google Scholar]
- 6.Mallbris L, Akre O, Granath F, Yin L, Lindelöf B, Ekbom A, et al. Increased risk for cardiovascular mortality in psoriasis inpatients but not in outpatients. Eur J Epidemiol. 2004;19:225–230. doi: 10.1023/b:ejep.0000020447.59150.f9. [DOI] [PubMed] [Google Scholar]
- 7.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 8.Wilson PW, D'Agostino RB, Parise H, Sullivan L, Meigs JB. Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation. 2005;112:3066–3072. doi: 10.1161/CIRCULATIONAHA.105.539528. [DOI] [PubMed] [Google Scholar]
- 9.Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002;288:2709–2716. doi: 10.1001/jama.288.21.2709. [DOI] [PubMed] [Google Scholar]
- 10.Molin L. Psoriasis. A study of the course and degree of severity, joint involvement, socio-medical conditions, general morbidity and influences of selection factors among previously hospitalized psoriatics. Acta Derm Venereol Suppl (Stockh) 1973;53:1–125. [PubMed] [Google Scholar]
- 11.Youn JI, Jo SJ. Clinical Study on 3, 123 Psoriatic Patients: Observation of the patients registered for the past 20 years (1982-2002)at Seoul National University Hospital Psoriasis Clinic. Korean J Dermatol. 2004;42:1536–1542. [Google Scholar]
- 12.Gisondi P, Tessari G, Conti A, Piaserico S, Schianchi S, Peserico A, et al. Prevalence of metabolic syndrome in patients with psoriasis: a hospital-based case-control study. Br J Dermatol. 2007;157:68–73. doi: 10.1111/j.1365-2133.2007.07986.x. [DOI] [PubMed] [Google Scholar]
- 13.Sommer DM, Jenisch S, Suchan M, Christophers E, Weichenthal M. Increased prevalence of the metabolic syndrome in patients with moderate to severe psoriasis. Arch Dermatol Res. 2006;298:321–328. doi: 10.1007/s00403-006-0703-z. [DOI] [PubMed] [Google Scholar]
- 14.Prodanovich S, Kirsner RS, Kravetz JD, Ma F, Martinez L, Federman DG. Association of psoriasis with coronary artery, cerebrovascular, and peripheral vascular diseases and mortality. Arch Dermatol. 2009;145:700–703. doi: 10.1001/archdermatol.2009.94. [DOI] [PubMed] [Google Scholar]
- 15.Lindegård B. Diseases associated with psoriasis in a general population of 159,200 middle-aged, urban, native Swedes. Dermatologica. 1986;172:298–304. doi: 10.1159/000249365. [DOI] [PubMed] [Google Scholar]
- 16.Azfar RS, Gelfand JM. Psoriasis and metabolic disease: epidemiology and pathophysiology. Curr Opin Rheumatol. 2008;20:416–422. doi: 10.1097/BOR.0b013e3283031c99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wakkee M, Herings RM, Nijsten T. Psoriasis may not be an independent risk factor for acute ischemic heart disease hospitalizations: results of a large population-based Dutch cohort. J Invest Dermatol. 2010;130:962–967. doi: 10.1038/jid.2009.321. [DOI] [PubMed] [Google Scholar]
- 18.Chen YJ, Wu CY, Shen JL, Chu SY, Chen CK, Chang YT, et al. Psoriasis independently associated with hyperleptinemia contributing to metabolic syndrome. Arch Dermatol. 2008;144:1571–1575. doi: 10.1001/archderm.144.12.1571. [DOI] [PubMed] [Google Scholar]
- 19.Lim S, Lee EJ, Koo BK, Cho SI, Park KS, Jang HC, et al. Increasing trends of metabolic syndrome in Korea -based on Korean national health and nutrition examination surveys- J Korean Diabetes Assoc. 2005;29:432–439. [Google Scholar]
- 20.Lym YL, Hwang SW, Shim HJ, Oh EH, Chang YS, Cho BL. Prevalence and risk factors of the metabolic syndrome as defined by NCEP-ATP III. J Korean Acad Fam Med. 2003;24:135–143. [Google Scholar]
- 21.Cohen AD, Sherf M, Vidavsky L, Vardy DA, Shapiro J, Meyerovitch J. Association between psoriasis and the metabolic syndrome. A cross-sectional study. Dermatology. 2008;216:152–155. doi: 10.1159/000111512. [DOI] [PubMed] [Google Scholar]
- 22.Akhyani M, Ehsani AH, Robati RM, Robati AM. The lipid profile in psoriasis: a controlled study. J Eur Acad Dermatol Venereol. 2007;21:1330–1332. doi: 10.1111/j.1468-3083.2007.02260.x. [DOI] [PubMed] [Google Scholar]