Abstract
Background
Port wine stains (PWSs) are commonly treated with pulsed dye laser (PDL) as a standard therapy. However, it is not easy to predict the minimal effective dose in the first treatment session.
Objective
The aim of this study was to assess whether dermoscopic findings before and after laser irradiation corresponded with the clinical improvement of PWS in patients undergoing PDL therapy.
Methods
Seven untreated PWSs in 6 patients (a male and 5 females), who presented to our hospital between May 2008 to January 2010, were assessed in this study. The mean age was 36.3 years, ranging from 14 to 57 years. A PDL with a wavelength of 585 nm and a spot size of 7 mm was used. Before and after test irradiation, patients underwent dermoscopy and clinical photography, and we assessed whether the dermoscopic findings corresponded with clinical improvement after 3 months.
Results
There were no obvious differences observed in the clinical photographs between each test level immediately after irradiation. However, dermoscopic photographs showed differences as the irradiated energy increased. These changes corresponded to the clinical improvement after 3 months.
Conclusion
Our study indicates that the minimal effective fluence can be predicted by observing dermoscopic change immediately after irradiation. We think that examining the dermoscopic findings immediately after irradiation allows the laser surgeon to predict the minimal effective fluence and this prevents adverse effects of the skin.
Keywords: Dermoscopy, Port-wine stain, Pulsed dye laser
INTRODUCTION
Port wine stains (PWSs) are commonly treated with pulsed dye laser (PDL), which is widely considered to be the standard therapy. However, it is not easy to predict the minimal effective dose in the first treatment session. Recently, dermoscopy has become a beneficial tool for the early detection of skin cancer, and there is a good relationship between dermoscopic and pathological findings.
The aim of this study was to assess whether dermoscopic findings before and after laser irradiation corresponded with the clinical improvement of PWS in patients undergoing PDL therapy.
MATERIALS AND METHODS
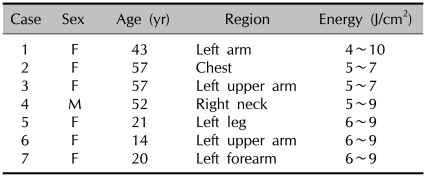
Seven untreated PWSs in 6 patients (a male and 5 females), who presented to our hospital from May 2008 to January 2010, were assessed in this study. The mean age was 36.3 years, ranging from 14 to 57 years (Table 1). Patients who had a history of diseases such as epilepsy or cutaneous photosensitivity were excluded from the study.
Table 1.
Profile of the subjects
F: female, M: male. Six patients with Port wine stain (7 lesions) were enrolled in this study.
Laser parameters and treatment protocol
A PDL with a wavelength of 585 nm and a spot size of 7 mm was used (SPTL-1b. Candela Corporation, Wayland, MA, USA). The pulse duration was set at 0.45 ms. Test irradiation ranged from 4 to 10 J/cm2 and the size of test irradiation was about 15×15 mm. All patients were given steroid ointment for 1 week and were advised to avoid exposure to the sun after test irradiation. The reason why we used hydrocortisone was to treat the mild burns caused by the laser treatment, especially in high fluence1.
Evaluation of results
Before and after test irradiation, patients underwent dermoscopy (Derma9500C-G, contact type, Derma Medical Inc., Yokohama, Japan) and clinical photography, and we assessed whether the dermoscopic findings corresponded to the clinical improvement after three months. If we could see changes on dermoscopic photographs immediately after test irradiation that corresponded to clinical improvement, the correspondence was evaluated as 'good'. If there were some discrepancies, it was evaluated as 'fair'.
RESULTS
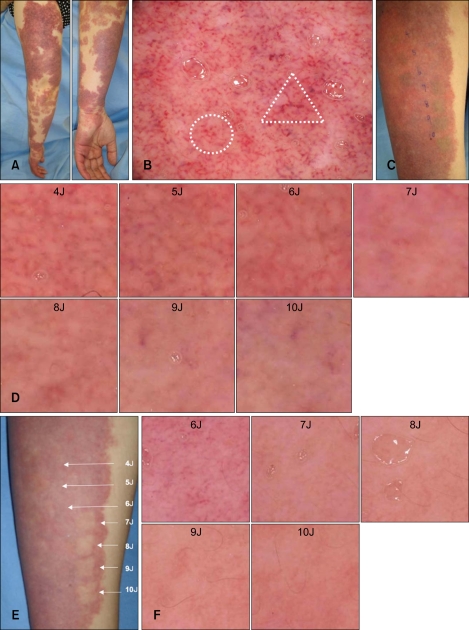
Case 1 is an untreated PWS on the left arm before treatment (Fig. 1A). The dermoscopic photograph before treatment shows dotted and globular vessels (superficial), as well as linear vessels (deep) (Fig. 1B). Immediately after laser irradiation, there are some differences, such as indistinct margins in 4~5 J/cm2 and increased whiteness in 9~10 J/cm2, but it is difficult to know what the most effective fluence is on the naked eye (Fig. 1C).
Fig. 1.
(A) A 43-year-old woman with a Port wine stain on the left arm before treatment. (B) Dermoscopic photograph before treatment shows (○) dotted and globular vessels (superficial), as well as (▵) linear vessels (deep). (C) Immediately after laser irradiation, there are some differences, such as indistinct margins in 4~5 J/cm2 and increased whiteness in 9~10 J/cm2, but it is difficult to know which is the most effective fluence by the naked eye. (D) Dermoscopic photographs immediately after irradiation (×10). At an energy level of 7 J/cm2, vessel walls are difficult to detect. (E) Three months after irradiation. at an energy level of 7 J/cm2, treatment was effective. (F) Dermoscpic photographs at 3 months after irradiation. at an energy level of 7 J/cm2, vessel walls have disappeared.
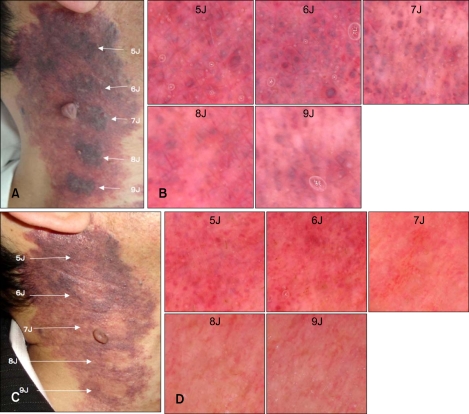
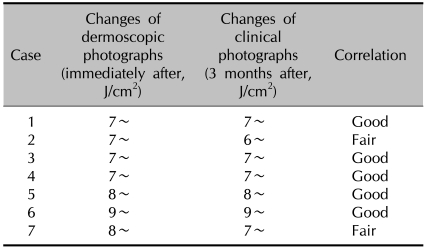
Also, in case 4, except for pulple change, there is no obvious differences in the clinical photographs between each energy level immediately after irradiation (Fig. 2A). However, dermoscopic photographs showed differences as the irradiated energy increased. In case 1 and case 4 (<6 J/cm2), we could detect vessel walls. At over 7 J/cm2, whitish areas appeared and vessel walls were lost (Fig. 1D, 2B). These changes corresponded to clinical improvement after 3 months (Fig. 1E, 2C), and dermoscopic photographs showed the disappearance of vessel walls (Fig. 1F, 2D). There was good correspondence in five patients, whereas it was fair in two (Table 2).
Fig. 2.
(A) A 52-year-old man with a previously untreated Port wine stain on the right neck immediately after irradiation. Except for purple change, no obvious difference was seen between each energy level. (B) Dermoscopic photographs obtained immediately after irradiation (×10). At an energy level of 7 J/cm2, whitish areas appear. (C) Three months after irradiation. At an energy level of 7 J/cm2, we evaluated the treatment as effective. (D) Dermoscpic photographs 3 months after irradiation. At an energy level of 7 J/cm2, vessel walls are difficult to detect.
Table 2.
Treatment results
The correspondence was good for five lesions and fair for two lesions.
DISCUSSION
PWSs are vascular malformations composed of postcapillary venules in the dermis. The distribution of vessel size and depth varies among patients and even within the same lesion2. The depth of the vessels is critical because the response to laser therapy decreases as vessels become deeper, and this has been shown histologically in some studies3,4. The diameter of the vessels is another very important parameter that influences the response to laser therapy. As a rule, vessels with a small diameter show less response to PDL than larger vessels, especially if they are located deeply3,4. All of these vascular differences are reflected in the color of the lesion, i.e., pink lesions have small deep vessels, purple lesions have larger deep vessels, and red lesions have superficial vessels3.
Epiluminescence microscopy is a noninvasive tool for the in vivo evaluation of pigmented lesions5. Digital videomicroscopy achieves a higher magnification and also allows us to record and compare digital images. Resent studies have identified two main patterns of venular malformations: 1) a superficial or blob pattern composed of red globules and dots that correspond to dilated capillary loops in the papillary dermis, and 2) a deep pattern that features red ring structures corresponding to dilated ecstatic vessels located deep in the horizontal vascular plexus2,6,7. Thus, videomicroscopy is widely recognized as a useful tool for assessing the response of PWSs to PDL therapy.
We considered that there would be changes of the vessels after irradiation, which would differ according to the radiation dose, but we can only see a purple change with the naked eye immediately after laser treatment. Therefore, we used dermoscopy to achieve a higher magnification and to allow us to record and compare the digital images. We found that there were some differences even immediately after irradiation. Dermoscopic photographs of the PWSs treated at higher levels showed some whitish areas, with vessels being difficult to detect. The radiation levels causing these changes corresponded to those where treatment was effective after 3 months.
The microvascular response to laser pulse therapy has been reported by Suthamjariya as follows: blood coagulation is seen with an increasing energy level, vasoconstriction, a thread-like appearance of the treated vessels, disappearance of vessels, intravascular cavitation, bubble formation, vessel wall rupture/hemorrhage, and shrinkage of perivascular tissue8. Intravascular cavitation does not always lead to rupture of the vessel and is not the mechanism underlying immediate disappearance of vessels. Instead, the apparent mechanism for immediate loss of vessels is the contraction of intravascular blood and perivascular collagen after thermal denaturation8.
Although immediate disappearance of vessels was not always associated with a good result after three months, our study showed that there was a significant relationship between immediate vessel disappearance and the clinical response.
Our study indicates that the minimal effective fluence can be predicted by observing dermoscopic changes immediately after irradiation. We think that examining the dermoscopic findings immediately after irradiation allows the laser surgeon to predict the minimal effective fluence and prevent adverse effects in the skin.
References
- 1.Lam AY, Wong DS, Lam LK, Ho WS, Chan HH. A retrospective study on the efficacy and complications of Q-switched alexandrite laser in the treatment of acquired bilateral nevus of Ota-like macules. Dermatol Surg. 2001;27:937–941. doi: 10.1046/j.1524-4725.2001.01094.x. [DOI] [PubMed] [Google Scholar]
- 2.Eubanks LE, McBurney EI. Videomicroscopy of port-wine stains: correlation of location and depth of lesion. J Am Acad Dermatol. 2001;44:948–951. doi: 10.1067/mjd.2001.113467. [DOI] [PubMed] [Google Scholar]
- 3.Fiskerstrand EJ, Svaasand LO, Kopstad G, Dalaker M, Norvang LT, Volden G. Laser treatment of port wine stains: therapeutic outcome in relation to morphological parameters. Br J Dermatol. 1996;134:1039–1043. [PubMed] [Google Scholar]
- 4.Onizuka K, Tsuneda K, Shibata Y, Ito M, Sekine I. Efficacy of flashlamp-pumped pulsed dye laser therapy for port wine stains: clinical assessment and histopathological characteristics. Br J Plast Surg. 1995;48:271–279. doi: 10.1016/0007-1226(95)90064-0. [DOI] [PubMed] [Google Scholar]
- 5.Seidenari S, Pellacani G, Pepe P. Digital videomicroscopy improves diagnostic accuracy for melanoma. J Am Acad Dermatol. 1998;39:175–181. doi: 10.1016/s0190-9622(98)70070-2. [DOI] [PubMed] [Google Scholar]
- 6.Motley RJ, Lanigan SW, Katugampola GA. Videomicroscopy predicts outcome in treatment of port-wine stains. Arch Dermatol. 1997;133:921–922. doi: 10.1001/archderm.133.7.921. [DOI] [PubMed] [Google Scholar]
- 7.Procaccini EM, Argenziano G, Staibano S, Ferrara G, Monfrecola G. Epiluminescence microscopy for port-wine stains: pretreatment evaluation. Dermatology. 2001;203:329–332. doi: 10.1159/000051783. [DOI] [PubMed] [Google Scholar]
- 8.Suthamjariya K, Farinelli WA, Koh W, Anderson RR. Mechanisms of microvascular response to laser pulses. J Invest Dermatol. 2004;122:518–525. doi: 10.1046/j.0022-202X.2004.22241.x. [DOI] [PubMed] [Google Scholar]