Abstract
The use of guided tissue regeneration (GTR) has become a standard of care in Periodontology. GTR using membrane barriers and/or bone grafting materials has also been used in periapical surgery. However, the application of the GTR principle, particularly in communicating endodontic-periodontal lesions with loss of the buccal cortical plate, is a very challenging task, with very few reported human clinical studies. An interdisciplinary approach, combining endodontic and periodontal (surgical) procedures can save a tooth in the long run that has been defined as hopeless at the preliminary stage of treatment.
Keywords: Endo-perio lesions, guided tissue regeneration, periapical surgery
INTRODUCTION
Although regeneration is the desired outcome of any therapy, it is the most difficult to achieve. In periodontics, regeneration is being achieved using various approaches like guided tissue regeneration (GTR), local application of growth factors/cytokines and host modulating agents etc.
The concept of GTR was introduced by Melcher.[1] Epithelial cells migrate approximately 10 times faster than other periodontal cells types.[2] If the epithelial cells are excluded from the wound long enough for other cell types with regenerative potential to become established, epithelial down growth is prevented and regeneration achieved. This can be done by using various barrier membranes with or without bone grafts. The principle of GTR can also be applied to endodontic defects e.g., root end surgery. Combined endodontic and periodontal lesions present a clinical dilemma to the clinician as the endodontic and periodontal tissues share an embryonic, biologic, and functional interrelationship.
Endodontic infection influences the progression of marginal bone loss in periodontitis.[3] Teeth with periapical radiolucencies have approximately 2 mm less radiographic attachment in comparison to teeth without periapical radiolucencies.[4] There is an approximate three-fold amplification of the rate of marginal radiographic bone loss (0.19 mm/year Vs 0.06 mm/year) for teeth in periodontitis-prone patients with an endodontic infection compared to teeth without an infection.[5]
Persisting endodontic infection may be regarded as a contributing risk factor for aggravating marginal attachment loss.
Thomas Von Arx[6] et al., in 2001, proposed a classification of membrane application in endodontic surgery based on typical periradicular lesions.
Class I a – bone defect confined to periapical region;
Class I b – periapical bone defect with erosion of lingual cortical plate;
Class II a – periapical and concomitant marginal lesions without communication;
Class II b – periapical and concomitant marginal lesions with communication;
Class III a – lateral juxtaradicular lesion; and
Class III b – lateral juxtaradicular lesion with communication to marginal lesion.
Class II lesions represent combined endodontic and periodontal lesions. Class II b lesions (apicomarginal communication) are the most difficult to treat and warrant the use of the GTR principle with the objective of facilitating tissue regeneration by creating an optimum environment (stable and protected wound) and excluding non-desired fast proliferating cells which interfere with desired tissue regeneration.
CASE REPORT
A 40-year-old male patient reported to the department of Periodontology, Bharati Vidyapeeth Dental College and Hospital, Pune, with the chief compliant of pain and mobility in lower front teeth since 10 days [Figure 1]. His dental history included root canal treatment (RCT) and porcelain-fused-to-metal (PFM) crowns in 31, 32, 41, 42 five years ago. H/O-repeat RCT (one month ago), crown lengthening with electrocautery (20 days ago) zirconia crowns (10 days ago). Periodontal findings on examination were bleeding on probing, pockets in 31, 41 (9-10 mm), 32, 42 (6-7 mm), mobility-grade III- 31, grade II 41, 42, 31.
Figure 1.

Pre-operative photograph
Radiographic findings: Root canal treated 31, 32, 41, and 42 [Figure 2].
Figure 2.

Pre-operative radiograph
Widening of periodontal ligament space seen in 32 and 42 regions extending up to apical 1/3rd and periapical radiolucency seen [Figure 3]. Interdental bone loss was seen between 31 and 41 regions.
Figure 3.
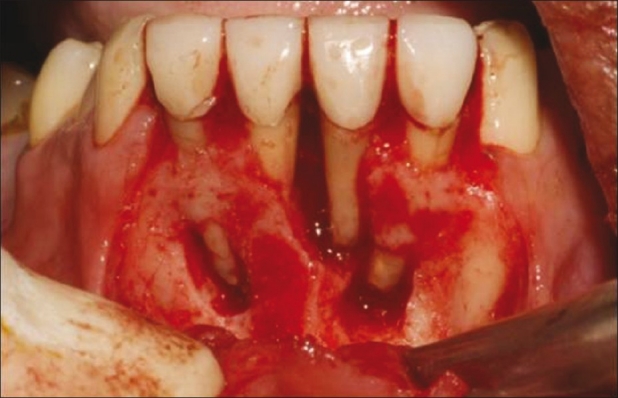
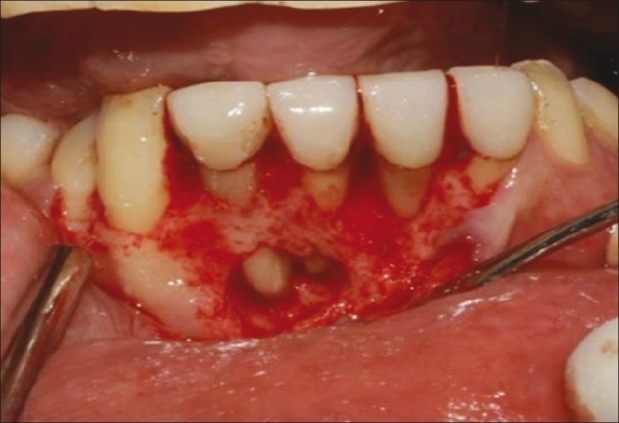
After flap reflection and debridement a class II b defect was evident with 31. Class II a defect was present with 32 and 42 regions. Apicoectomies done with 31, 32, and 42 regions
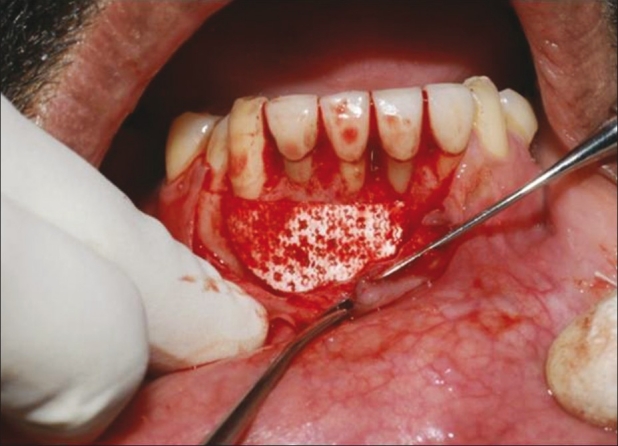
The case was of communicating endodontic – periodontal lesions associated with lower anterior teeth. The patient had no relevant medical history. He was explained about the poor prognosis of the teeth. Under local anesthesia, a mucoperiosteal flap was raised. Thorough curettage was done. The defect dimensions were approximately 2 cm × 1 cm in 31, 32, and 41 regions and 5 mm × 5 mm in the 42 region. The lingual cortical plate was intact [Figures 4and 5]. As the defect was of considerable dimensions and the lesion a class II b with 31 and 41 regions and a class II a with 32 and 42 regions, it was decided to carry out GTR using xenograft (Bio- oss) and a resorbable membrane (Perioguide). Apicoectomies of 31, 32, and 42 were carried out. Flap was replaced and sutures were given [Figure 6]. A course of antibiotics and analgesics were prescribed to the patient. Sutures were removed after 10 days. Patient was followed-up every month. The mobility of the teeth had subsided (from grade III to grade I with 31). There was significant reduction in pocket depth after three months. Wound healing was satisfactory. However, after four months, a small sinus tract was seen in the 42 region. Again the course of antibiotics was repeated and it subsided. But when the patient came back with the same complaint six months post surgery, a surgical re-entry was planned [Figures 7 and 8]. After reflecting the flap, a class II a lesion was evident associated with 41 and 42 regions. Again thorough debridement with apicoectomy of 41 was carried out. GTR was done as earlier [Figure 9]. The most striking finding at the surgical re-entry was the bone fill seen in between 31 and 41 regions, where a bony defect had existed extending apicocoronally with total loss of the buccal cortical plate. The patient is regularly being followed-up. The wound healing is satisfactory. Slight recession is noticed with 32 and 42 regions after the second surgical intervention [Figure 10].
Figure 4.
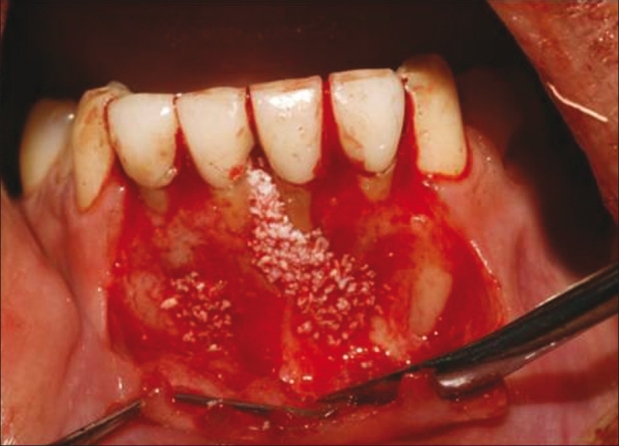
Bone graft (Bio-oss) placed in defect
Figure 5.
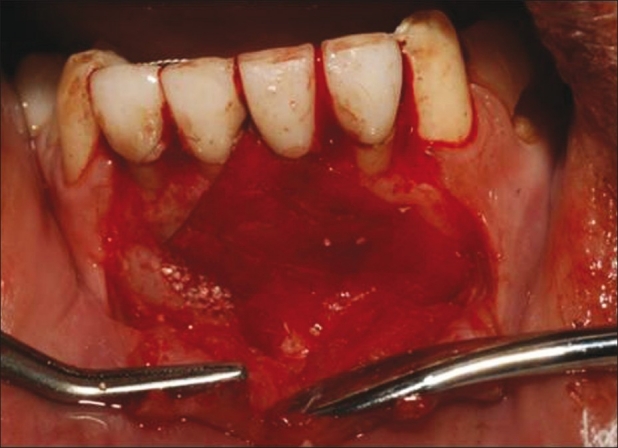
Bioresorbable membrane (perioguide) placed
Figure 6.

Sutures given
Figure 7.
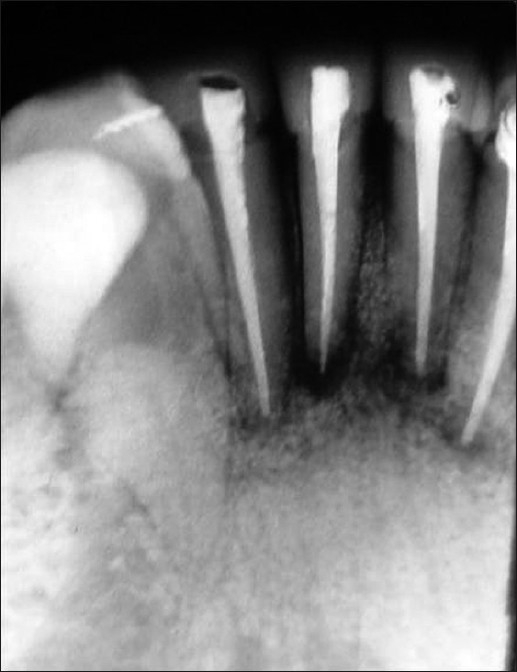
Six months post-operative radiograph showing bone fill between 31 and 41 regions
Figure 8.
Surgical re-entry at six months-dense hard tissue evident between 31 and 41 and apical to 31 and 32 regions. Bony defect (class II a) apical to 41 and 42 regions
Figure 9.
GTR carried out in 41 and 42 regions
Figure 10.

Healing four months after surgical re-entry
DISCUSSION
Class II b lesions have been found to be the most challenging to treat. In a clinical trial involving periapical surgery, by Hirsch[7] et al. only 27.3% of teeth with total buccal bone loss showed healing, whereas the success rate of teeth with an intact buccal bone plate was 49.5%.
Skoglund and Persson[8] carried out a retrospective evaluation of teeth which showed complete loss of buccal plate during periapical surgery and reported that after three years only 37% were successful, whereas the success rate was 90% for teeth with intact marginal periodontium.
However, in 1996, Douthitt,[9] demonstrated 89% bone fill in class II b lesions treated using the membane, whereas only 67% in control sites. The membrane sites revealed a significantly better connective tissue attachment (4.1 mm Vs 1.8 mm).
In our case, the placement of a barrier membrane supported by an underlying xenograft resulted in a considerable amount of dense and hard tissue both radiographically and upon re-entry. This has been reported in many case reports.[10] The majority of cases have reported good to excellent tissue regeneration.
The achievement in combining endodontic and periodontal surgical procedures would be to salvage a tooth or teeth on a long term basis that had been defined as hopeless at the initiation of treatment, thus proving to be a new ray of hope!
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Melcher AH. On the repair potential of periodontal tissues. J Periodontol. 1976;47:256–60. doi: 10.1902/jop.1976.47.5.256. [DOI] [PubMed] [Google Scholar]
- 2.Engler WO, Ramfjord SP, Hiniker JJ. Healing following simple gingivectomy: A tritiated thymidine radioautographic study-I: Epithelialization. J Periodontol. 1966;37:298–308. doi: 10.1902/jop.1966.37.4.298. [DOI] [PubMed] [Google Scholar]
- 3.Jansson L, Ehnevid H, Lindskog S, Blomlöf LB. Relationship between periapical and periodontal status.A clinical retrospective study. J Clin Periodontol. 1993;20:117–23. doi: 10.1111/j.1600-051x.1993.tb00325.x. [DOI] [PubMed] [Google Scholar]
- 4.Jansson LE, Ehnevid H, Lindskog SF, Blomlöf LB. Radiographic attachment in periodontitis-prone teeth with endodontic infection. J Periodontol. 1993;64:947–53. doi: 10.1902/jop.1993.64.10.947. [DOI] [PubMed] [Google Scholar]
- 5.Jansson L, Ehnevid H, Lindskog S, Blomlöff L. The influence of endodontic infection on progression of marginal bone loss in periodontitis. J Clin Periodontol. 1995;22:729–34. doi: 10.1111/j.1600-051x.1995.tb00254.x. [DOI] [PubMed] [Google Scholar]
- 6.von Arx T, Cochran DL. Rationale for the Application of theGTR Principle Using a Barrier Membrane in Endodontic Surgery: A Proposal of Classification and Literature Review. Int J Periodontics Restorative Dent. 2001;21:127–39. [PubMed] [Google Scholar]
- 7.Hirsch JM, Ahlström U, Henrikson PA, Heyden G, Peterson LE. Periapical surgery. Int J Oral Surg. 1979;8:173–85. doi: 10.1016/s0300-9785(79)80016-2. [DOI] [PubMed] [Google Scholar]
- 8.Skoglund A, Persson G. A follow-up studyof apicoectomized teeth with total loss ofthe buccal bone plate. Oral Surg Oral Med Oral Pathol. 1985;59:78–81. doi: 10.1016/0030-4220(85)90120-3. [DOI] [PubMed] [Google Scholar]
- 9.Douthitt JC. Dallas: Baylor Univ; 1996. Management of MarginalAlveolar Bone Defects During Peri-radicular Surgery Using the GuidorBioresorbable Matrix Barrier [thesis] [Google Scholar]
- 10.Brugnami F, Mellonig JT. Treatment of a large periapical lesion with loss of labial cortical plate using GTR: A case report. Int J Periodontics Restorative Dent. 1999;19:243–9. [PubMed] [Google Scholar]


