Abstract
Non-Hodgkin's lymphoma (NHL) commonly presents as non-tender, enlarged lymph nodes, accompanied by diffuse symptoms of fatigue and low-grade intermittent fever and it is derived predominantly from the cells of the B lymphocyte series. NHL cases occur extra-nodally and in 3% of these cases the initial presentation may be in the oral cavity. Though extra-nodal NHL of the oral cavity is a rare finding, patients with oral lesions of NHL commonly present at the dental clinic in the first instance. A careful clinical evaluation supported by histopathological and other laboratory investigations will help in identifying the disease at an early stage, resulting in better prognosis. Any delay in diagnosis has important implications on the morbidity and mortality of the condition. Due to the rarity of intraoral NHL, we present one such a case with a complaint of tumor-like mass on the gingiva of lower molar region. The lesion was clinically thought as pyogenic granuloma and later diagnosed as extra nodal NHL of the oral cavity.
Keywords: Gingival mass, non-Hodgkin's lymphoma, pyogenic granuloma
INTRODUCTION
Malignant lymphoma is the generic term given to tumors of the lymphoid system and these are divided into the following two major categories: Hodgkin's lymphoma and non-Hodgkin's lymphoma (NHL).[1] NHL usually involves lymph nodes but can also involve extra-nodal sites and can occur in the stomach, skin, lung, salivary glands, and rarely in the mouth.[2] Oral lesions of NHL may develop in the soft tissues or centrally within the jaws. Oral lesions appear as non-tender swellings commonly affecting the vestibule, gingival, or posterior hard palate and develop slowly, mimicking a dental abscess of endodontic or periodontal origin.[3]
The present case report of gingival swelling as the first and only manifestation of extra-nodal follicular NHL also emphasizes the importance of accurate clinical and histologic diagnostic procedures to avoid delayed diagnosis or inappropriate treatment strategies when dealing with unspecific lesions in the oral cavity.
CASE REPORT
A 46-year old woman was referred to Department of Periodontics, SJM Dental College and Hospital, Chitradurga, with a painful growth on gums of the posterior teeth of left lower jaw, from a general dentist. The patient had noticed the sudden appearance of a painless mass about 3 weeks prior to referral. On extra-oral examination, she was non-febrile, without any palpable lymph nodes in the facial region, and she did not mention any recent sudden weight loss. The patient gave history of hysterectomy one year back and post operative healing was uneventful. Intraoral examination revealed a gingival growth extending from the mandibular left first premolar region to the retro-molar trigone. The mass was soft to firm and the overlying mucosa was slightly ulcerated and edematous [Figure 1]. There were no palpable lymph nodes of any group in the head and neck region. A panoramic radiograph revealed slight resorption of the alveolar crest between first and second molar [Figure 2]. Clinical diagnoses of “pyogenic granuloma” and “Squamous cell carcinoma” were given.
Figure 1.

Swelling extending from the gingival of left mandibular second premolar region to the retromolar trigone with obliteration of the vestibule
Figure 2.
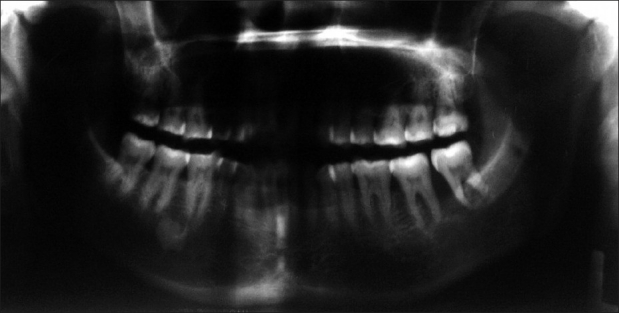
Panoramic radiograph showing only slight resorption of the alveolar bone in left mandibular molar area
The patient underwent an incisional biopsy from the posterior part of the lesion. The presence of numerous lymphocytes separated by thin fibrous septae with ulcerated epithelium and surface exudation was viewed on microscopic examination, and a repeat biopsy was suggested. The diagnosis of a nonspecific inflammatory change was made and repeat biopsy was advised. A second incisional biopsy was undertaken from the centre of the lesion to confirm the diagnosis. Histopathology from second biopsy tissue revealed atypical lymphoid cells arranged in diffuse sheets in a delicate connective tissue stroma with areas hemorrhage [Figure 3]. The tumor cells showed indistinct margins having vesicular, hyperchromatic and pleomorphic nuclei with prominent nucleolus and abundant eosinophilic cytoplasm [Figure 4]. These findings were consistent with NHL. A second opinion from a senior Histopathologist was sought. Based on the histopathological findings of second biopsy and the expert opinion, a final diagnosis of “Non-Hodgkin's lymphoma” was made.
Figure 3.
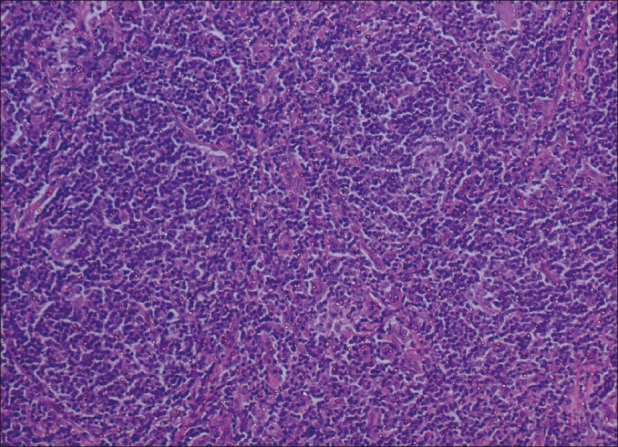
Photomicrograph showing atypical lymphocytes arranged in sheets with minimal connective tissue stroma (H and E, ×100)
Figure 4.
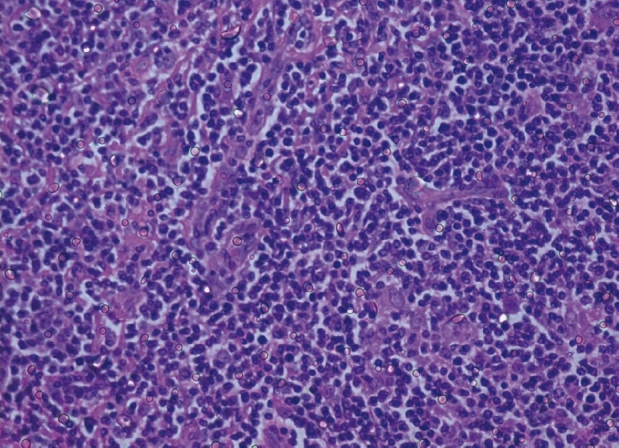
Photomicrograph showing rounded hyperchromatic atypical lymphocytes (H and E, ×250)
The patient's general health was examined by a physician to find out involvement of any other site. Investigations like complete hemogram, radiograph, and computed tomography scan were performed and no other site except the oral cavity (gingival of left posterior teeth) showed involvement. She was then referred to Kidwai Memorial Institute of Oncology, Bangalore, for treatment.
DISCUSSION
NHLs are a group of highly diverse malignancies and have great tendency to affect organs and tissues that do not ordinarily contain lymphoid cells. NHL usually involves lymph nodes and 20 to 30% involve extranodal sites. The head and neck is the second most common region for extra-nodal lymphoma after gastro-intestinal tract. The involvement of NHL in the oral cavity is very uncommon accounting for only 0.1 to 5% of the cases reported.[4,5]
Oral lymphomas are often difficult to diagnose as there are no characteristics clinical features. Patients often present with nonspecific clinical signs and symptoms like local swelling, pain or discomfort, and ulcer. The oral NHL may mimic more common benign, oral and dental pathologic conditions such as pyogenic granuloma, periodontal disease, osteomyelitis, and other malignancies.[6–8]
Many a times, lymphoma presents in the oral cavity as the first identifiable evidence of the disease.[8,9] Sometimes, these may also present as squamous-cell carcinoma and needs to be considered in the differential diagnosis.[5] There is considerable evidence that lymphomas at specific sites show a local inflammatory process in the beginning, followed by increased rate of cell division of lymphocytes and thereby increasing the chance of a malignant clone developing.[2]
The prevalence of NHL is increasing among those who are immunocompromised, receiving organ transplants, and those with autoimmune disorders such as Sjögren's syndrome or rheumatoid arthritis. An increased incidence of NHL has also been recognized in patients suffering from AIDS[8] and oral lesions of NHL have presented as the first manifestation of AIDS.[10]
Until recently, the Rappaport classification has been widely used which was based on the growth pattern of tumor cells (nodular or diffuse), cell type, and degree of cell differentiation.[11] Treatment options depend on histologic classification and clinical staging.
Although the oral involvement of NHL is rare, they are the second most common oral malignant disease after oral squamous cell carcinoma, constituting 2.2% of all malignancies of the head-neck, and 3.5% of intraoral malignancies.[12,13]
A differential diagnosis was made which included the following conditions: Pyogenic granuloma, peripheral giant cell granuloma, squamous-cell carcinoma, and periodontal disease. Due to lack of local factors and good oral hygiene, pyogenic granuloma and periodontal disease were excluded from the diagnosis. Histopathologic findings ruled out peripheral giant cell granuloma and squamous-cell carcinoma.
In the present case, the general dentist had difficulty diagnosing the lesion and hence had referred to us. The radiographic findings were non-contributory. However, there was no evidence of the disease other than the gingiva. Diagnosis was made from histopathologic appearance of surgical biopsies. Histopathology of NHL usually shows sheets of chronic inflammatory cells, especially lymphocytes, mimicking an inflammatory reaction. Careful examination by an expert histopathologist is necessary to find out the pleomorphic and atypical lymphoid cells. Primary NHL of the gingiva can mimic other benign or reactive lesions and hence it is necessary to perform a biopsy and microscopic examination in cases where signs and symptoms persist in spite of treatment.
An early biopsy will provide an appropriate diagnosis and may help in avoiding the disease progression, thus improving the prognosis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Evans LS, Hancock BW. Non-hodgkin lymphoma. Lancet. 2003;362:139–46. doi: 10.1016/S0140-6736(03)13868-8. [DOI] [PubMed] [Google Scholar]
- 2.Wolvius EB, van der Valk P, van der Wal JE, van Diest PJ, Huijgens PC, van der Waal I, et al. Primary extranodal non-Hodgkin lymphoma of the oral cavity.An analysis of 34 cases. Eur J Cancer B Oral Oncol. 1994;30B(2):121–5. doi: 10.1016/0964-1955(94)90063-9. [DOI] [PubMed] [Google Scholar]
- 3.Neville BW, Damm DD, Allen CM, Bouquot JE. 2nd Ed. Pennsylvania: WB Saunders; 1995. Oral and Maxillofacial Pathology; pp. 432–4. [Google Scholar]
- 4.Takahashi H, Tsuda N, Tezuka F, Okabe H. Primary non-hodgkin's lymphoma of the oral region. J Oral Pathol Med. 1989;18:84–91. doi: 10.1111/j.1600-0714.1989.tb00742.x. [DOI] [PubMed] [Google Scholar]
- 5.Chan AC, Chan JC. Lyon: IARC Press; 2005. Haematolymphoid tumours.In World Health Organization Classification of Tumours, Pathology and Genetics of Head and Neck Tumors; pp. 199–205. [Google Scholar]
- 6.Richards A, Castelloe MA, Everson JW, Scully C, Irvine GH, Rooney N. Oral mucosal non-Hodgkin.s lymphoma: A dangerous mimic. Oral Oncol. 2000;36:556–8. doi: 10.1016/s1368-8375(00)00047-6. [DOI] [PubMed] [Google Scholar]
- 7.Wilson TG, Wright JM. Non-Hodgkin's lymphoma of the gingiva: review of the literature: Report of a case. J Periodontol. 1986;57:155–8. doi: 10.1902/jop.1986.57.3.155. [DOI] [PubMed] [Google Scholar]
- 8.Beral V, Peterman T, Berkelman R, Jaffe H. AIDS-associated non-Hodgkin lymphoma. Lancet. 1991;337:805–9. doi: 10.1016/0140-6736(91)92513-2. [DOI] [PubMed] [Google Scholar]
- 9.Werder P, Altermatt HJ, Zbären P, Mueller-Garamvölgyi E, Bornstein MM. Palatal swelling as the first and only manifestation of extranodal follicular non-Hodgkin lymphoma: A case presentation. Quintessence Int. 2010;41:93–7. [PubMed] [Google Scholar]
- 10.Wolvius E-B, Schulten EA, van der Waal I. Non Hodgkin's lymphoma of the oral cavity as the first manifestation of AIDS. Br Dent J. 1997;182:107–8. doi: 10.1038/sj.bdj.4809316. [DOI] [PubMed] [Google Scholar]
- 11.Cotran RS, Kumar V, Collins T. 6th Ed. London: WB Saunders Company; 1999. In Robins Pathologic Basis of Disease. [Google Scholar]
- 12.DePeña CA, Van Tassel P, Lee YY. Lymphoma of the head and neck. Radiol Clin North Am. 1990;28:723–43. [PubMed] [Google Scholar]
- 13.Epstein JB, Epstein JD, Le ND, Gorsky M. Characteristics of oral and paraoral malignant lymphoma: a population-based review of 361 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:519–25. doi: 10.1067/moe.2001.116062. [DOI] [PubMed] [Google Scholar]


