Abstract
Background:
With regard to potential retrievability of cement-retained implant restorations, the retentive strength of the luting agents is critical. The aim of this study was to evaluate the retention values of implant-supported metal copings using different luting agents.
Materials and Methods:
Twenty ITI implant analogs and solid abutments of 5.5-mm height were embedded vertically in autopolymerizing acrylic resin blocks. Metal copings with a loop on the occlusal surface were fabricated using base metal alloy (Rexillium III). The copings were luted using eight cements with different retention mechanisms (Panavia F2.0, Fuji Plus, Fleck's, Poly F, Fuji I, Temp Bond, GC-free eugenol, and TempSpan) under static load of 5 kg (n=10). All specimens were incubated at 37°C for 24 hours, conditioned in artificial saliva for 7 days and thermocycled for 5000 cycles (5-55°C). The dislodging force was measured using a universal testing machine at a crosshead speed of 5 mm/min. Statistical analyses were performed using Kruskal-Wallis (α=0.05) and Mann-Whitney tests with Bonferroni correction (α=0.001).
Results:
Fuji Plus and TempSpan had the highest and the least mean retentive strength, respectively (320.97±161.47, 3.39±2.33). There was no significant difference between Fuji Plus, Fleck's, Ploy F, and Panavia F2.0. These cements were superior to provisional cements and Fuji I (P<0.001) which showed statistically same retentive strength.
Conclusion:
Within the conditions of this study, the resin modified glass ionomer, zinc phosphate, zinc polycarboxylate, and Panavia F2.0 had statistically the same retentive quality and are recommended for definitive cementation of single implant-supported restorations. The provisional cements and glass ionomer may allow retrievability of these restorations.
Keywords: Cementation methods, dental cement, dental prosthesis/retention, dental prosthesis, implant-supported
INTRODUCTION
Implant therapy is a well-documented treatment for replacing missing teeth. The implant-supported prostheses are attached to implant abutments either by cementation, or by retaining screws. Because of the advantages of cement-retained implant-supported restorations, such as passive fit, reduced cost, ease of fabrication, superior esthetic, fewer components, and uncomplicated laboratory technique, these restorations have gain popularity compare to screw-retained restorations.[1–3] Even though cement wash outs occur in cement-retained restorations, they do have high clinical success rates.[4]
Retrievability may be a critical aspect of implant-supported restorations because of problems such as loosening or fracture of the abutment screws, mechanical failures, treatment of peri-implant tissues, and evaluation of ailing implants mobility.[5] Although using provisional cements are considered to achieve retrievability of implant-supported prostheses, retrievability of screw-retained prostheses is more secure than cement-retained ones.[6,7]
Retention of implant-supported restorations plays an important role in success of the treatment. Uncemented restorations may cause problems such as inhalation of the restorations, increased bone loss around the implant, prosthesis failure breakage, trauma to antagonistic teeth, food impaction, accumulation of microorganisms resulting in bad odor and soft tissue response. Extra practitioner time and patient embarrassment have also been noted.[8,9] On the other hand, luting agents that are too retentive may damage the osseointegration of the implant during removal of the restoration.[6]
Behavior of permanent and provisional luting agents in cementation of implant-supported prostheses differs from cementation on natural teeth.[10] In particular, water-based cements such as zinc phosphate, zinc polycarboxylate, and glass ionomer, have shown a wide variety of retentive values, which can sometimes be unpredictable.[6,11–15] Some authors suggested the use of permanent and provisional cements for luting single-unit and multi-unit implant-supported restorations, respectively.[16,17] Provisional cements have been recommended for restorations that may require intervention. Whereas more retentive cements, such as resin cement, are more appropriate when future retrievably is not necessary.[18,19]
The use of different cements, protocols, and implant systems may alter the retentive strength of implant-supported restorations. In addition, different aging processes, such as thermal cycling and mechanical loading, as well as different pretreatment techniques can also affect the retentive strength.[20–22]
The aim of this study was to evaluate the retention values of cement retained implant-supported restorations with different luting agents. The null hypothesis was that there is no differenece in retentiveness of cement retained implant-supported restorations with different luting agents.
MATERIALS AND METHODS
Twenty ITI solid abutments with 5.5 mm length and 8° taper (048.541, ITI Dental Implant System, Straumann AG, Basel, Switzerland) and twenty ITI implant analogs (048.124, ITI Dental Implant) were used. The abutments were tightened to implant analogs at 35 Ncm of torque. The implant-abutment complex were embedded vertically in a block of autopolymerizing acrylic resin (Meliodent, Heraeus Kulzer, Hanau, Germany) using a dental surveyor for precise alignment. The copings were made using prefabricated burn-out caps for crowns. A loop of wax was added to the occlusal surface of each coping for retention test. The wax patterns were invested in a phosphate-bonded investment (Ceravest Quick, GC, Tokyo, Japan) and cast in a base metal alloy (Rexillium III, Pentron, Wallingford, CT). After divesting and cleaning with an ultrasonic cleaner and hydrofluoric acid, the inner surface of the castings were inspected under magnification (×4), and surface irregularities were removed with a small round carbide bur. The metal copings were checked for fitness using a silicon disclosing medium (Fit Checker, GC Co, Tokyo, Japan), and further potential interferences of castings were evaluated and adjusted if necessary.
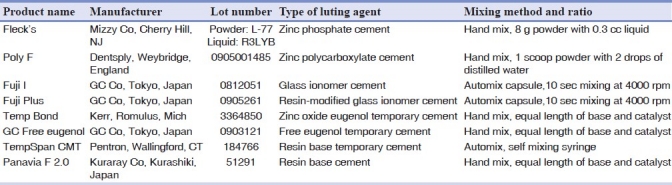
Each casting was randomly numbered and paired with an implant-abutment assembly for further procedures. Eight commercially available luting agents, including provisional (Temp Bond, GC-free eugenol, TempSpan) and definitive (Panavia F2.0, Fuji Plus, Fleck's, Poly F, and Fuji I) cements were evaluated in this study [Table 1]. Each cement was mixed according to the manufacturer's instruction and applied to intaglio surface of the copings (n=10). The copings were gently seated on the abutments and held in place under a 5 kg load for 10 minutes. After initial setting of the cement, the excess cement was removed with an explorer.
Table 1.
Luting agents tested
The specimens were stored in a 37°C incubator for 24 hours, immersed in artificial saliva for 7 days and thermocycled for 5000 cycles (5-55°C) with a 30-s dwell time. After aging process, the dislodging force of the copings was measured using a universal testing machine (4302 Instron Ltd., High Wycombe, UK) at a crosshead speed of 5 mm/min [Figure 1]. The failure modes were recorded after the dislodgment of the copings.
Figure 1.

Luted metal coping during pull out test by universal testing machine
The same copings and abutments were used with each of the eight cements evaluated. To remove the residual cement, the castings were heated to 600°C for 90 minutes and allowed to cool at room temperature. A spoon excavator was used to remove any residual cement from the intaglio surface of castings and the abutments were cleaned with a plastic explorer. The castings and abutments were immersed in ultrasonic cleaner containing cement removal agent (Removalon-I, Premier Dental Products Co, Norristown, PA) for 30 and 15 minutes, respectively. Repeated cementation of castings does not affect tensile strength.[23]
Statistical analysis
Kruskal-Wallis test was used for data analysis (α=0.05). Mann-Whitney test with a Bonferroni adjusted significance level of 0.001 was used for each pairwise comparison to control the overall error rate for all comparisons at an error rate of 0.05. No statistical analysis was performed on failure mode of the studied cements.
RESULTS
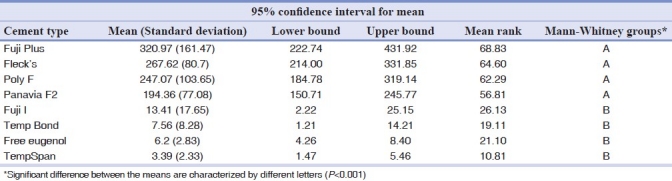
Table 2 represents the mean retentive values and standard deviations in Newton (N), as well as the mean rank of the studied luting agents. Kruskal-Wallis test revealed a significant difference between the retentive values of the studied luting agents (P<0.001). Fuji Plus and TempSpan had the highest and the least mean retention, respectively. Mann-Whitney test showed no significant difference between Fuji Plus, Fleck's, Ploy F, and Panavia F2.0 and these cements were superior to the provisional and Fuji I cements (P<0.001)which showed statistically the same retentive strength.
Table 2.
Mean (standard deviation) dislodging forces of the studied cements (N) and Mann-Whitney groups
Cement failure occurred in the cement-abutment interfaces in all of the Fuji Plus, Panavia F2.0, and Fleck's samples. Zinc polycarboxylate and zinc oxide with and without eugenol cements remained on both the copings and abutment surfaces whereas TempSpan completely remained on the abutment surfaces.
DISCUSSION
In this study, the null hypothesis that the retentiveness of the metal copings would not affect with the studied cements was rejected. The resin modified glass ionomer cement (Fuji Plus) had the highest retention, but there were no significant differences between definitive cements. Some studies indicate that the retentive strength of resinous cement is superior to that of, zinc phosphate and zinc polycarboxylate cements.[6,14,24]
The higher retentive strength of the resin cements was attributed to the adhesive system[25] which was not used in the current study. Furthermore, resin modified glass ionomer cement adheres to metal by chelating metallic ions, but the retentive strength may be weakened by early water contact.[14] In this study, the copings were incubated for 24 hours at 37°C before the aging process and there was no early water contact.
In a study on titanium copings over short ITI solid abutments, the mean retentive values of zinc phosphate cement was comparable to Panavia 21, but the retentive strength was higher than in the present study.[22] A combination of Panavia 21 and titanium alloy was reported to have higher bond strength compared to other alloys.[26,27] In another study on the retention of base metal copings with dental implants, zinc phosphate and resin modified glass ionomer cements showed same retention strength.[5] With regard to the CeraOne system, zinc phosphate cement had highest retention value, and resinous cement presented statistically similar retentive strength.[15,28]
In a similar investigation on retention values of metal copings on ITI solid abutments, Panavia 21 had significantly higher retention than resin modified glass ionomer and polycarboxylate cements. Interestingly, zinc phosphate and zinc oxide eugenol cements had similar retentive strength.[14] The different results with the present study maybe due to using different cements and thermal cycles. Long-term thermal cycling has been shown to reduce the retentive strength of luting agents.[6,14,29] Squier et al.[29] reported a higher retentive value for Panavia than zinc phosphate and resin modified glass ionomer, which differs from the current study. This discrepancy may be related to sandblasting and surface conditioning in this study.[29]
Surprisingly, glass ionomer cement had the lowest retention among the definitive luting agents, which was comparable to the temporary cements. This finding is consistent with a previous study that demonstrated glass ionomer cement showed significantly lower retention than zinc phosphate and resinous cements, and similar retention to zinc oxide cement without eugenol.[15] In the present study, no pretreatment was performed on either the copings or the abutments, and glass ionomer cement does not adhere to an inert surface.[28] Furthermore, the solubility of glass ionomer cement is more than that of other cements, and it is very susceptible to early water contact and desiccation,[30] which can dramatically reduce the mechanical properties of the cement.[31]
The retentive strength of restorations is influenced by taper, surface area, height and surface roughness of the abutment,[32] restoration characteristics, type of cement,[3,29,32,33] marginal accuracy[34] and the treatment method. Thus a direct comparison with other studies may be difficult because of differences in the implant systems, specimens, and methodology.
The location of the cement failure may be an important factor in cement selection. Adhesion of the cement to abutment may be difficult to remove and damage the abutment surface. In this study, the resinous and resin modified glass ionomer cements completely adhered to the intaglio surface of the copings. It could be related to the lack of an adhesive system in this study. The casting retention luted using zinc phosphate cement was provided by micromechanical interlocking. The surface of implant abutment is relatively smooth, which caused remaining zinc phosphate cement in the inner surface of the copings. The primary failure mode for the polycarboxylate cement was adhesive, but there was also some cohesive failure. It may be explained by zinc polycarboxylate bonding to the titanium surface.[14] The temporary cements, with the exception of TempSpan, adhered to both inner surface of the copings and the abutment surfaces. TempSpan completely adhered to the abutment surfaces and was easily removed.
Our results suggest that the tested definitive cements are not desirable if retrievability of single-unit metal restorations is sought. The dislodgement force for an implant with 4-mm diameter and 6 mm height directly out of the socket along its long axis was about 290 N.[35]
In this study the snap-on mechanism of the burn-out cap was removed by a reamer from the inner surface of the castings, which resulted in a passive fit. Thus, the role of luting agents to crown retention was better assessed.
The force that is used to retrieve the implant-supported restoration is high impact and of short duration. On the other hand, in this study a monotonic static test was used. The failures of the restorations result in several comparative small dynamic loadings and the axial dislodging of cemented implant crowns is a rather seldom clinical event. Cement behavior under fatigue loading may be different compared with static load application. The results of this in vitro study should be interpreted with caution and confirmed with clinical studies.
CONCLUSIONS
Within the limitations of this study, the following conclusions can be drawn:
The most retentive luting agent was resin-modified glass ionomer, but there was no significant difference between this cement and Panavia 2.0, zinc phospate, and zinc polycarboxylate cements. These definitive cements are recommended for luting single-unit implant-supported metal restorations.
The temporary and glass ionomer cements were the least retentive cements and might not be suitable for luting single-unit implant-supported restorations.
ACKNOWLEDGMENT
This study was supported by Isfahan University of Medical Sciences Research Grant # 288107. The authors do not have any financial interest in the companies whose materials are included in this article.
Footnotes
Source of Support: This study was supported by Isfahan University of Medical Sciences Research Grant # 288107
Conflict of Interest: None declared.
REFERENCES
- 1.Hebel KS, Gajjar RC. Cement-retained versus screw-retained implant restorations: Achieving optimal occlusion and esthetics in implant dentistry. J Prosthet Dent. 1997;77:28–35. doi: 10.1016/s0022-3913(97)70203-8. [DOI] [PubMed] [Google Scholar]
- 2.Chee WW, Torbati A, Albouy JP. Retrievable cemented implant restorations. J Prosthodont. 1998;7:120–5. doi: 10.1111/j.1532-849x.1998.tb00191.x. [DOI] [PubMed] [Google Scholar]
- 3.Michalakis KX, Hirayama H, Garefis PD. Cement-retained versus screw-retained implant restorations: A critical review. Int J Oral Maxillofac Implants. 2003;18:719–28. [PubMed] [Google Scholar]
- 4.Kwan N, Yang S, Guillaume D, Aboyoussef H, Ganz SD, Weiner S. Resistance to crown displacement on a hexagonal implant abutment. Implant Dent. 2004;13:112–9. doi: 10.1097/01.id.0000127519.68325.d7. [DOI] [PubMed] [Google Scholar]
- 5.Sheets JL, Wilcox C, Wilwerding T. Cement selection for cement-retained crown technique with dental implants. J Prosthodont. 2008;17:92–6. doi: 10.1111/j.1532-849X.2007.00262.x. [DOI] [PubMed] [Google Scholar]
- 6.Maeyama H, Sawase T, Jimbo R, Kamada K, Suketa N, Fukui J, et al. Retentive strength of metal copings on prefabricated abutments with five different cements. Clin Implant Dent Relat Res. 2005;7:229–34. doi: 10.1111/j.1708-8208.2005.tb00068.x. [DOI] [PubMed] [Google Scholar]
- 7.Gervais MJ, Wilson PR. A rationale for retrievability of fixed, implant-supported prostheses: A complication-based analysis. Int J Prosthodont. 2007;20:13–24. [PubMed] [Google Scholar]
- 8.Misch CE. Principles of cement-retained fixed implant prosthodontics. In: Misch CE, editor. Dental Implant Prosthetics. St.louis: Elsevier Mosby; 2005. pp. 414–51. [Google Scholar]
- 9.Cranin AN. Atlas of Oral Implantology. 2nd ed. St. louis: Mosby; 1999. Root form implant prosthodontics abutments; pp. 320–40. [Google Scholar]
- 10.Breeding LC, Dixon DL, Bogacki MT, Tietge JD. Use of luting agents with an implant system: Part I. J Prosthet Dent. 1992;68:737–41. doi: 10.1016/0022-3913(92)90194-f. [DOI] [PubMed] [Google Scholar]
- 11.Mehl C, Harder S, Wolfart M, Kern M, Wolfart S. Retrievability of implant-retained crowns following cementation. Clin Oral Implants Res. 2008;19:1304–11. doi: 10.1111/j.1600-0501.2008.01587.x. [DOI] [PubMed] [Google Scholar]
- 12.Pan Y-H, Ramp LC, Lin C-K, Liu P-R. Comparison of 7 luting protocols and their effect on the retention and marginal leakage of a cement-retained dental implant restoration. Int J Oral Maxillofac Implants. 2006;21:587–92. [PubMed] [Google Scholar]
- 13.Wolfart M, Wolfart S, Kern M. Retention forces and seating discrepancies of implant-retained castings after cementation. Int J Oral Maxillofac Implants. 2006;21:519–25. [PubMed] [Google Scholar]
- 14.Mansour A, Ercoli C, Graser G, Tallents R, Moss M. Comparative evaluation of casting retention using the ITI solid abutment with six cements. Clin Oral Implants Res. 2002;13:343–8. doi: 10.1034/j.1600-0501.2002.130401.x. [DOI] [PubMed] [Google Scholar]
- 15.Montenegro AC, Machado AN, Depes Gouvêa CV. Tensile strength of cementing agents on the CeraOne system of dental prosthesis on implants. Implant Dent. 2008;17:451–60. doi: 10.1097/ID.0b013e31818c4947. [DOI] [PubMed] [Google Scholar]
- 16.Akça K, Iplikçioğlu H, Cehreli MC. Comparison of uniaxial resistance forces of cements used with implant-supported crowns. Int J Oral Maxillofac Implants. 2002;17:536–42. [PubMed] [Google Scholar]
- 17.Hill EE. Dental cements for definitive luting: A review and practical clinical considerations. Dent Clin North Am. 2007;51:643–658. doi: 10.1016/j.cden.2007.04.002. vi. [DOI] [PubMed] [Google Scholar]
- 18.Ramp MH, Dixon DL, Ramp LC, Breeding LC, Barber LL. Tensile bond strengths of provisional luting agents used with an implant system. J Prosthet Dent. 1999;81:510–4. doi: 10.1016/s0022-3913(99)70203-9. [DOI] [PubMed] [Google Scholar]
- 19.Dudley JE, Richards LC, Abbott JR. Retention of cast crown copings cemented to implant abutments. Aust Dent J. 2008;53:332–9. doi: 10.1111/j.1834-7819.2008.00075.x. [DOI] [PubMed] [Google Scholar]
- 20.GaRey DJ, Tjan AH, James RA, Caputo AA. Effects of thermocycling, load-cycling, and blood contamination on cemented implant abutments. J Prosthet Dent. 1994;71:124–32. doi: 10.1016/0022-3913(94)90019-1. [DOI] [PubMed] [Google Scholar]
- 21.Michalakis K, Pissiotis AL, Kang K, Hirayama H, Garefis PD, Petridis H. The effect of thermal cycling and air abrasion on cement failure loads of 4 provisional luting agents used for the cementation of implant-supported fixed partial dentures. Int J Oral Maxillofac Implants. 2007;22:569–74. [PubMed] [Google Scholar]
- 22.Sadig WM, Al Harbi MW. Effects of surface conditioning on the retentiveness of titanium crowns over short implant abutments. Implant Dent. 2007;16:387–96. doi: 10.1097/ID.0b013e31815c8d7b. [DOI] [PubMed] [Google Scholar]
- 23.Kaar D, Oshida Y, Andres CJ, Barco MT, Platt JA. The effect of fatigue damage on the force required to remove a restoration in a cement-retained implant system. J Prosthodont. 2006;15:289–94. doi: 10.1111/j.1532-849X.2006.00126.x. [DOI] [PubMed] [Google Scholar]
- 24.Piwowarczyk A, Lauer HC, Sorensen JA. In vitro shear bond strength of cementing agents to fixed prosthodontic restorative materials. J Prosthet Dent. 2004;92:265–73. doi: 10.1016/j.prosdent.2004.06.027. [DOI] [PubMed] [Google Scholar]
- 25.Ernst CP, Wenzl N, Stender E, Willershausen B. Retentive strengths of cast gold crowns using glass ionomer, compomer, or resin cement. J Prosthet Dent. 1998;79:472–6. doi: 10.1016/s0022-3913(98)70164-7. [DOI] [PubMed] [Google Scholar]
- 26.Burke FJ, Fleming GJ, Nathanson D, Marquis PM. Are adhesive technologies needed to support ceramics.An assessment of the current evidence? J Adhes Dent. 2002;4:7–22. [PubMed] [Google Scholar]
- 27.Kim Y, Yamashita J, Shotwell JL, Chong KH, Wang HL. The comparison of provisional luting agents and abutment surface roughness on the retention of provisional implant-supported crowns. J Prosthet Dent. 2006;95:450–5. doi: 10.1016/j.prosdent.2006.03.020. [DOI] [PubMed] [Google Scholar]
- 28.Clayton GH, Driscoll CF, Hondrum SO. The effect of luting agents on the retention and marginal adaptation of the CeraOne implant system. Int J Oral Maxillofac Implants. 1997;12:660–5. [PubMed] [Google Scholar]
- 29.Squier RS, Agar JR, Duncan JP, Taylor TD. Retentiveness of dental cements used with metallic implant components. Int J Oral Maxillofac Implants. 2001;16:793–8. [PubMed] [Google Scholar]
- 30.Powers JM, Sakaguchi RL. Cements. In: Powers JM, Sakaguchi RL, editors. Craig's Restorative Dental Materials. 12th ed. St. louis: Mosby; 2006. pp. 480–511. [Google Scholar]
- 31.Shen C. Dental Cements. In: Anusavice K, editor. Phillips’ science of dental materials. 11th ed. St.louis: Elsevier Saunders; 2007. pp. 443–94. [Google Scholar]
- 32.Bernal G, Okamura M, Muñoz CA. The effects of abutment taper, length and cement type on resistance to dislodgement of cement-retained, implant-supported restorations. J Prosthodont. 2003;12:111–5. doi: 10.1016/S1059-941X(03)00006-8. [DOI] [PubMed] [Google Scholar]
- 33.Covey DA, Kent DK, St Germain HA, Jr, Koka S. Effects of abutment size and luting cement type on the uniaxial retention force of implant-supported crowns. J Prosthet Dent. 2000;83:344–8. doi: 10.1016/s0022-3913(00)70138-7. [DOI] [PubMed] [Google Scholar]
- 34.Nejatidanesh F, Lotfi HR, Savabi O. Marginal accuracy of interim restorations fabricated from four interim autopolymerizing resins. J Prosthet Dent. 2006;95:364–7. doi: 10.1016/j.prosdent.2006.02.030. [DOI] [PubMed] [Google Scholar]
- 35.Hallgren C, Sawase T, Ortengren U, Wennerberg A. Histomorphometric and mechanical evaluation of the bone-tissue response to implants prepared with different orientation of surface topography. Clin Implant Dent Relat Res. 2001;3:194–203. doi: 10.1111/j.1708-8208.2001.tb00141.x. [DOI] [PubMed] [Google Scholar]


