Abstract
Background:
Investigation was designed to evaluate the behavioral changes in children receiving dental treatment while they have been administered combination of Midazolam/Ketamine or Midazolam/Promethazine.
Materials and Methods:
This was a randomized double blind clinical trial with cases being selected from those uncooperative children aged 2 to 6 years from those referred for treatment under general anesthesia. Anxiety score of all cases were recorded before any attempt using Frankel's anxiety scoring system with those in negative category being included. Cases with at least a pair of similar size cavities on similar teeth were selected with each tooth being randomly allocated for one sedative regimen group. To avoid sequence effect, half of the patients received one regimen at the first visit while the other half received the other regimen as the first. Each case served as control for him or herself to reduce influencing factors. Child's reaction was recorded before, during, and at the end of dental procedure. SO2 as well as Pulse rate were recorded as the most critical vital signs. Collected data were then analyzed using analysis of variance (ANOVA) and paired t-test.
Results:
Patients’ mean age was 3.5 years with 43% being male. Only 10% of the Ketamine/Midazolam group showed considerable amount of change in their behavior with a statistical significant difference being presented (P=0.029).
Conclusion:
Under the current circumstances, Ketamine/Midazolam combination provided sufficient sedative effect in lower doses. However, Midazolam/Promethazine combination did not produce similar results.
Keywords: Children, dental fear, ketamine, midazolam, oral sedation, promethazine
INTRODUCTION
Treating anxious children remains to be a big challenge for pediatric dental profession.[1,2] It is proved to be difficult and in certain cases even impossible to treat these fearful young children on a routine set up of dental chair status. Frankel's scaling system classifies child's cooperation level in four points from definitely positive to definitely negative.[3,4] Those scored negative and above are considered as clinically difficult patients who may benefit from a pharmacological preparation and even general anesthesia (GA) prior to any dental intervention.[5,6] In these circumstances, the use of pharmacological methods comes to light in order to enable certain case to be seen effectively. These include the conscious sedation (CS) and GA. Since GA requires high levels of experience along with a minimum hospital set up, CS is suggested as an effective while cheaper and more convenient to both patient and operator.[6] Malamed (2010) indicated that oral sedation is the oldest known yet effective, economic, and easy to use among all routes of CS.[7] High patient's acceptance is the key advantage of the oral route on top of its other advantages. However, this is not necessarily the case in very young fearful individuals.[6] Several side effects including overdose, idiosyncrasy, and allergy could be seen with any drug administration.[7] However, the oral route represents the least reactions amongst the different routes. Late effect is considered as one of the disadvantages of oral sedation along with unpredictable absorption rate and titration limitations. In most instances, the initial sedative signs could not be seen before the first half hour as the pick plasma level of the drug will not reach to obtain its anxiolytic effects.[4] Promethazine is known as antihistaminic drug which provides degrees of sedation. It is well absorbed in Gastrointestinal system and its effect starts within 20 minutes of oral administration with a period of 4-6 hours lasting effect. Its role is also in controlling the nausea, vomiting, and apprehension.[7] In most of the sedative drugs, the highest effect is achieved after half an hour.[4,6–8] A half-life of 60 to 120 minutes with a double value effect of diazepam is seen on the use of Midazolam.[9,10] This is why the pick plasma level is reached late as well as its titration following oral administration of the drug. Titration difficulty is known as one of the most important obstacles facing oral route when central nervous system depression drugs are used. For this reason, any insufficient initial drug dose or its metabolized product should not be compensated by any additive dose of the drug or reverse it quickly when needed. Surprisingly, the lengthy effect of sedative drugs (3-4 hours) could provide both patient and the operator with relaxed status during the treatment and even it could cause a late discharge obligation to avoid problems while still sedated.[2]
Oral sedative drugs usually include anxiolytics, sedatives, barbiturates, narcotics, and antihistamines.[8] The use of inhalation sedation is routine when associated with other routes including oral sedation,[8,11,12] while it has yet to be licensed by the local medical authorities. Midazolam is used as a short- and fast-acting Benzodiazepine prior to GA or several other medical diagnostic approaches.[4,8,12–14] On the other hand, several other studies have looked at the sedative effect of some similar drugs use along Midazolam with a synergic effect to reduce the required dose of Midazolam.[1,4,8] Ketamine and Midazolam are among those already been used successfully in dental treatment of young fearful children.[4,8,12] Varying reports suggest that the administration of oral or rectal ketamine has caused patients some degree of nystagmus, hallucination, and salivation.[13] This study was designed to evaluate the sedative effect of two oral combination drugs namely Ketamine/Midazolam and Promethazine/Midazolam in a group of uncooperative children needing dental treatment.
MATERIALS AND METHODS
This randomized double blind clinical trial was conducted on 30 children aged 2 to 6 years who were selected from those referred to Mofid Children's Hospital Tehran for dental treatment under GA. Patients were randomly divided into two groups with drugs being administered by the anesthesiologist with operator having no clue of the drugs as well as patient. Attempts were made to include those with no systemic disease and no contraindication to these sedative drugs. Cases were also checked to have no past dental experience while having signs of fear and anxiety toward and during dental examination. Cases with at least two similar treatment needs were included in this investigation in order to provide a chance for each patient to act as self control. All required information and instructions were given to parents in writing preoperatively. This included the consent form for the child's involvement in the trial. Ethical approval was also obtained from the Ethic Committee of Shahid Beheshti Medical University prior to the commencement of the investigation. Cases were requested a 6 hour period of fasting preoperatively (nil per oral, NPO). Each patient was scheduled for two appointments. Drugs were administered in first or second visits in a random manner to avoid the sequence effect. All the drugs were administered by the Anesthesiologist in charge, while the dental operator was unaware of the administered drug. This was conducted in such a way to provide a double blind status for patient and operator. Vials of 5 ml Midazolam IV (0.4 mg/ml, Tehran Chemicals, Tehran, Iran) was mixed with 5 mg/kg Ketamine vial (5 mg/ml, Daru Pakhsh, Iran) and a sweetened drinking water of the same volume. The sweetened water was used as the flavored vehicle for the drugs which were then administered to each patient straight before the commencement of the dental treatment using a needleless syringe.[4,15] The second combination consisted of 0.5 mg/kg Midazolam with Promethazine (5 mg/ml, Sina Daru, Iran). A waiting period of 30 minutes was observed before any attempt to start treatments at the waiting area and under constant parent's supervision. This would allow the effect of the administered drugs to reach to their pick. Monitoring was performed and recorded in each 15 minute intervals from the start of the drugs administration to the discharge point using a pulse oximeter and a blood pressure (BP) cough. All treatment steps were performed by a pediatric dentist and the measurements of behavioral changes were recorded by another pediatric dentist. Vital signs were measured and recorded constantly by the anesthesiologist. The anxiety scoring system introduced by Wilson (1985) was used to record child's behavioral status per-, during, and postoperatively.[12,14] BP as well as oxygen saturation (OS) was measured, judged, and recorded by the anesthesiologist as the most critical vital signs of for each patient.[13] Patients were not discharged prior to a final check by the anesthesiologist for their fitness to leave with parents. Ethical approval was obtained for research on human subjects as well as an informed consent signed by the parents/guardians. Parents were also asked to report postoperative complications, if any. Case selection was performed based on their attendance and in a sequential manner as simple sampling. Collected data were statistically analyzed using analysis of variance (ANOVA), Kruskal Wallis, and Mann Whitney tests. Wilcoxon signed rank test was also used to look for intergroup comparisons. Chi Square as well as Pierson/Spearman tests were used to see the correlation coefficient.[14]
RESULTS
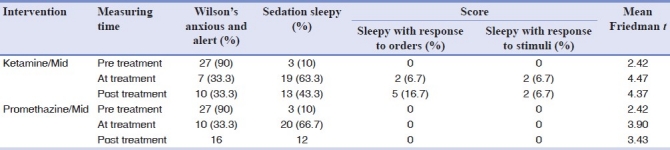
Mean age of the patients was 38.1±3.6 months (43% male and 57% female). All cases were at 92% OS level (within normal limit) but one dropped to 88% from the first group [Table 1]. Mauchly's test of sphericity showed covariance's homogenicity in heart rates recorded (P=0.104, W=0.461). ANOVA test for heart rate showed a significant difference between the two groups (P=0.018, F=2.838). t test showed that heart rate was significantly different in both groups before and after they have received the drugs (P=0.037 for Ketamine, P=0.002 for Promethazine). However, these data were not different when compared at pre- and post-operation points [Table 2]. Wilson's behavioral scoring was carried out before treatment commencement with 53.3% being at a reasonably cooperative level, whereas none were fully cooperative (excellent). Overall, 66.7% had a good score of cooperation while receiving treatment with a 10% fully cooperative up to the end of treatment (Excellent). Friedman test showed that no statistical difference could be detected after 6 times measurements (P=0.053, χ²=10.905) [Table 3]. Wilson's sedation values were compared using Friedman test in three separate occasions with significant differences between groups (P<0.001, χ²=56.297) [Table 4]. Wilcoxon's test showed that the effect of sedation is different when data were statistically compared from the starting point to the time treatment was undergoing (P=0.029).
Table 1.
Comparing the result of the pulse oximeter measurement in each group
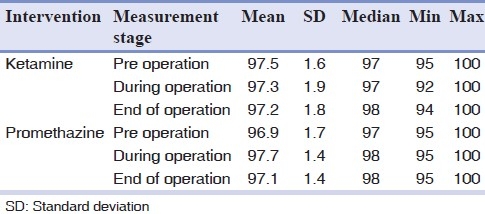
Table 2.
Comparing the result of the pulse rate measurement in each group
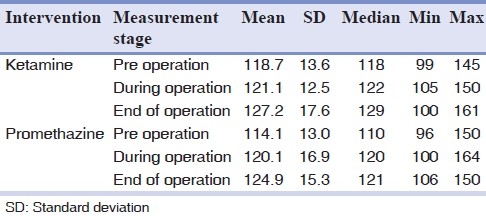
Table 3.
Wilson's behavior scores in two combination groups at three measured times
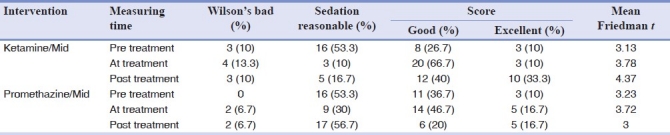
Table 4.
Wilson's sedation scores in two combination groups at three measured times
DISCUSSION
Based on the current literature, there is a growing preference for sedation and GA dental treatment of anxious and very young children.[4,6,8,11] Result of the current randomized clinical trial indicated that both protocols were safe with desirable sedation effect in pediatric dentistry.
The advantage of drug combination used in this study was to maximize sedation level obtained, keeping low doses while such results could not be expected by same drug doses when administered alone.[5] Although promethazine is effective in prevention of apprehension, nausea, and vomiting, its effect to put the child into light sleep has also been documented. However, its combination with Midazolam provided a chance to reduce the dose required for desirable sedation.
The use of Ketamine/Midazolam combination indicated that deep sedation and drowsiness will be achieved by the use of Ketamine as sedative and Midazolam as anxiolytic.[4,13] Roelofse et al. (2004) indicated that the sedative effect of Midazolam alone (1 mg) was significantly higher than the combination of Midazolam (0.35 mg)/Ketamine.[13] The most advantageous point is that the drug combination lowers the need for higher doses of the drug. Since all children participated scored “Bad” to “Fair” behavior before the start of treatment, dramatic changes was observed in their behavior during and at the end of treatment. An overall difference was noted between the two groups indicating “Good” and “Excellent” behavior score for Midazolam/Ketamine, while this was only scored “Good” for the Midazolam/Promethazine group. However, the difference was not found to be statistically significant between groups (P>0.05). It appears that the use of Promethazine along with Midazolam could help in reducing vomiting and nausea with reduced dose of Midazolam. OS and pulse rate did not show any statistical significant differences in different time intervals in both groups. Small changes noted in these measurements were within the safe range.
As most of the drugs used for sedation are capable of inducing GA in higher doses, care should be taken while administered in chair side. In this regard, sufficient training should be obtained prior to any attempt to sedate children in dental practice.[4,6] Benzodiazepines including Midazolam are considered as a group of safe sedative drugs to have a short acting effect with a highly popular chair side dental application.[4] Ketamine is also known as a dissociative anesthetic agent which has been used as an oral sedative for many years.[4,16–18] Promethazine is an antihistaminic used for mild sedation for daily dental patients.[15] To monitor the safety of the cases, such measurements are being tested with a 15-minute interval on recordings for both pulse oximeter and the BP. However, no significant differences were found between groups after the treatment ended (P>0.05), while this difference was significant between before and during the treatment records (P<0.05). It is important to note that the drug dose usually plays a critical role on the level of sedation achieved, as indicated by Bui et al. (2002). Wilson's Score on the sedative effect of the two combination drugs was also compared resulting in favor of Ketamine, similar to the findings of Bui et al.[15] It is, however, contradicting Damle et al. (2008) and Sheroan et al. (2006) which both indicated that Midazolam had a higher score when compared with Ketamine.[4,11] Roelofse et al. (2004) looked at the different sedative effects of Oral Midazolam with and without Ketamine, concluding Midazolam alone as a better sedative agent than combined with Ketamine.[13] They suggested that 1 mg/kg administered dose of Midazolam alone was more effective than when the reduced dose of 0.35 mg/kg is administered in association with Ketamine. Since the initial signs of the drug effect appeared in a wide range when administered orally, it is not suggested to start treatment in a fixed time following the drug's administration.[4,12,13] It is therefore essential to evaluate the patient's response to the drug in several occasions including before administration, during, and at the end of the treatment (discharge). Follow-up of the cases in the current investigation indicated that a common sleeping period of 1.5 hours was reported postoperatively along with some cases with sporadic sicknesses.
CONCLUSIONS
Despite a small difference between Ketamine and Promethazine groups, the difference was not of significant difference.
Midazolam/Ketamine combination appears to have a deeper sedative effect during and after the treatment.
OS and BP measurements did not show any statistically significant difference among the cases of the two groups when compared.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Roberts GJ, Wignall BK. Efficacy of the laryngeal reflex during oxygen-nitrous sedation (Relative Analgesia) Br J Anaesth. 1982;54:1277–81. doi: 10.1093/bja/54.12.1277. [DOI] [PubMed] [Google Scholar]
- 2.Hosey MT. Anxious children: Coping in dental practice. Dental update. 1995;22:210–5. [PubMed] [Google Scholar]
- 3.Frankl L, Hellman I. Symposium on child analysis. The ego's participation in the therapeutic alliance. Int J Psychoanal. 1962;43:333–7. [PubMed] [Google Scholar]
- 4.Damle SG, Gandhi M, Laheri V. Comparison of oral Ketamine and oral Midazolam as sedative agent in pediatric dentistry. J Indian Soc Pedod Prev Dent. 2008;26:97–101. [PubMed] [Google Scholar]
- 5.Wilson S. Pharmacologic patient management for pediatric dental treatment. Pediatric Clin North Am. 2000;22:107–12. doi: 10.1016/s0031-3955(05)70262-5. [DOI] [PubMed] [Google Scholar]
- 6.Lökken P, Bakstad OJ, Fonnelöp E, Skogedal N, Hellsten K, Bjerkelund CE, et al. Conscious sedation by rectal administration of Midazolam or Midazolam plus Ketamin as alternatives to general anesthesia for dental treatment of uncooperative children. Scand J Dent Res. 1994;102:274–80. doi: 10.1111/j.1600-0722.1994.tb01468.x. [DOI] [PubMed] [Google Scholar]
- 7.Malamed SF. Sedation: A guide to patient management. 5th ed. California: C. V. Mosbey Co., Elsevier; 2010. pp. 95–110. Chap 7. [Google Scholar]
- 8.Torres-Pérez J, Tapia-García I, Rosales-Berber MA, Hernandez-Sierra JF, Pozos-Guillen Ade J. Comparison of three conscious sedation regimens for pediatric dental patients. J Clin Pediatr Dent. 2007;31:185–8. doi: 10.17796/jcpd.31.3.e82526q0432375n0. [DOI] [PubMed] [Google Scholar]
- 9.Gerecke M. Chemical structure and properties of Midazolam compared with other benzodiazepines. Br J Clin Pharmacol. 1983;16:11–6. doi: 10.1111/j.1365-2125.1983.tb02266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kupietzky A, Houpt MI. Midazolam: Review of its uses for conscious sedation of children. Pediatric Dent. 1993;15:237–41. [PubMed] [Google Scholar]
- 11.Sheroan MM, Dilley DC, Lucas WJ, Vann WF. A prospective study of 2 sedation regimens in children: Chloral hydrate, meperidine, and hydroxyzine versus Midazolam, meperidine and hydroxyzine. Anesth Prog. 2006;53:83–90. doi: 10.2344/0003-3006(2006)53[83:APSOSR]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilson E, David A, MacKenzie N, Grant IS. Sedation during spinal anaesthesia: Comparison of propofol and Midazolam. Br J Anaesth. 1990;64:48–52. doi: 10.1093/bja/64.1.48. [DOI] [PubMed] [Google Scholar]
- 13.Roelofse JA, Shipton EA, de la Harpe CJ, Blignaut RJ. Intranasal Sufentanil/Midazolam versus Ketamine/Midazolam for analgesia/sedation in the pediatric population prior to undergoing multiple dental extractions under general anesthesia: A prospective, double-blind, randomized comparison. Anesth Prog. 2004;51:114–21. [PMC free article] [PubMed] [Google Scholar]
- 14.Wilson PR, Beimans J, Stafford KJ, Veltman CJ, Spoorenberg J. Xylazine and a xylazine/fentanyl citrate/azaperone combination in farmed deer. I: Dose rate comparison. N Z Vet J. 1996;44:81–7. doi: 10.1080/00480169.1996.35941. [DOI] [PubMed] [Google Scholar]
- 15.Bui T, Redden RJ, Murphy S. A comparison study between Ketamine and Ketamine-Promethazine combination for oral sedation in pediatric dental patients. Anesth Prog. 2002;49:14–8. [PMC free article] [PubMed] [Google Scholar]
- 16.Bal N, Saricaoglu F, Uzun S, Dal D, Celebi N, Celiker V, et al. Perioperative anxiety and postoperative behavioral disturbances in children: Comparison between induction techniques. Eur J Anaesthesiol. 2006;23:470–5. doi: 10.1017/S0265021506000408. [DOI] [PubMed] [Google Scholar]
- 17.Roelofse JA, van Der Bijl P. Adverse reaction to Midazolam and Ketamine premedication in children. Anesth Prog. 1991;38:73. [PMC free article] [PubMed] [Google Scholar]
- 18.Sullivan DC, Webb MD, Wilson CF. A comparison of two oral Ketamine-Diazepam regimens for sedation of anxious pediatric dental patients. Pediatr Dent. 2001;23:233–7. [PubMed] [Google Scholar]


