Abstract
Background:
C-reactive protein (CRP) is an acute phase reactant and has been proved to be a significant predictor of future cardiovascular events. Recent studies have demonstrated a correlation between periodontitis and elevated CRP levels. However, comparison between the levels of CRP in two main forms of periodontitis is ambiguous. This study aims at determining and comparing the relative levels of serum CRP in aggressive and chronic periodontitis patients.
Materials and Methods:
A total of 240 systemically healthy subjects were divided into three groups of 80 based on having generalized aggressive periodontitis, chronic generalized periodontitis and non-periodontitis (NP; controls). Venous blood samples were collected for quantitative CRP analysis using turbidimetric immunoassay.
Results:
Mean CRP levels were significantly greater in both generalized aggressive periodontitis (7.49±2.31 mg/l) and chronic generalized periodontitis (4.88±1.80 mg/l) groups as compared to NP (0.68±0.23 mg/l) controls. Moreover, CRP levels were significantly higher in aggressive periodontitis as compared to chronic periodontitis patients. Also, CRP levels positively correlated with the amount of periodontal destruction as measured by probing depth and clinical attachment loss for both chronic generalized periodontitis and generalized aggressive periodontitis.
Conclusion:
Findings of the present study indicated that periodontitis should be of particular concern in younger individuals, where elevated levels of CRP may contribute to early or more rapid cardiovascular disease in susceptible patients. Thus, further research should be carried out at a community level to ascertain these findings.
Keywords: C-reactive protein, cardiovascular disease, periodontitis
INTRODUCTION
Periodontitis is a destructive inflammatory disease of supporting tissues of teeth. The host responds to periodontal infections with an array of events involving both innate and adaptive immunities. Although periodontitis is chronic in nature, acute-phase elements are also parts of the innate immunity in periodontitis and confirm that systemic inflammation is present in periodontitis. The acute-phase reactants have pro-inflammatory properties; they activate complement factors, neutralize invasive pathogens and stimulate repair and regeneration of variety of tissues. The acute-phase reactants that have received the most attention are C-reactive protein (CRP), plasminogen activator 1 and fibrinogen. CRP, in particular, has been the focus of attention as a key marker of atherosclerosis and elevated levels constitute a risk predictor for cardiovascular disease (CVD).[1]
CRP is an acute-phase reactant that is produced in response to diverse inflammatory stimuli including heat, trauma, infection and hypoxia. It is synthesized by the liver in response to inflammatory cytokines like interleukin IL-6, IL-1 and tumor necrosis factor (TNF)-α. CRP plays a key role in the innate immune response and is easily measured due to its long plasma half-life (12–18 hours). Thus, CRP levels provide useful information for the diagnosis, monitoring and therapy of the inflammatory process and associated disease. Importantly, CRP is currently regarded as a biomarker of systemic inflammation.[2]
The International Workshop for Classification of Periodontal Diseases and Conditions by American Academy of Periodontology (1999) revised the classification of periodontal diseases. Accordingly, periodontal diseases are classified into three main forms – chronic periodontitis, aggressive periodontitis and periodontitis as the manifestation of systemic disease. Aggressive periodontitis comprises a group of rare (≈1% of population), rapidly progressing form of periodontitis, characterized by severe destruction of periodontal attachment apparatus at an early age. Chronic periodontitis is recognized as the most frequent, slowly progressing form of periodontitis. Its onset may be at any age, with prevalence and severity of the disease increasing with age. It may affect a variable number of teeth and has variable rates of progression.[3]
Recently, it has been found that patients with periodontal infections show elevated CRP levels compared to periodontally healthy individuals.[4–6] Most studies to date have included patients with chronic periodontitis and few investigators have studied CRP levels in subjects with aggressive periodontitis. Since both forms of periodontitis show disparity in the rate of progression, the effect of chronic and aggressive periodontitis on CRP levels seems to be an appealing area of research.
Thus, the present study was undertaken to determine the relative levels of serum CRP and compare them in aggressive and chronic periodontitis patients.
MATERIALS AND METHODS
Patient selection and clinical examination
The Institutional Review Board (IRB), Bagalkot, Karnataka, India, approved the study and an informed consent was obtained from all patients before the start of study. The subjects were examined in the, Department of Periodontics, P. M. N. M. Dental College and Hospital, Bagalkot, Karnataka, India. Following complete medical and dental examination, 240 individuals were selected for the study. Subjects were placed into three groups according to the following definitions:
Non-periodontitis controls
This group comprised 80 patients with the following:
No evidence of attachment loss
Gingival inflammation may be present in variable degrees of severity
Generalized aggressive periodontitis
This group comprised 80 patients with the following:
Probing depth (PD) of ≥5 mm and/or clinical attachment loss (CAL) on eight or more teeth, at least three of which were not first molars and incisors with varying degree of disease severity
With rapid rate of disease progression
Deposits being inconsistent with disease severity
Mostly under 30 years of age
Familial aggregation
Chronic generalized periodontitis patients
This group comprised 80 patients with the following:
PD of ≥5 mm and/or CAL in more than 8 teeth with varying degree of disease severity
Local factors concomitant with the amount of destruction
With moderate rate of progression
Dental examination consisted of oral hygiene index simplified (OHI-S), gingival index (GI), PD and CAL measurements using William's graduated periodontal probe and an orthopantomogram (OPG). All the selected subjects were systemically healthy and none had received periodontal treatment and antibiotic therapy for at least 6 months prior to sampling and recording. Active smokers and subjects with systemic diseases like diabetes, arthritis, CVD, etc. were excluded from the study. Also, pregnant and lactating females were excluded from the study.
Quantitative determination of CRP
Serum levels of CRP were quantified using turbidimetric immunoassay according to the manufacturer's instructions. Kit used was “TURBILYTE-CRP” (Tulip diagnostics, Goa, India) which had a detection limit of 0.5 mg/l and measuring range of 0–22 mg/l.
Method
Turbidimetric immunoassay is based on the principle of agglutination reaction. Only serum should be used for testing. If delay in testing occurs, store samples at 2°C–8°C. Turbid or particulate serum samples are clarified by centrifugation at 2000 rpm for 15 minutes. Use only clear supernatant for testing.
Statistical analysis
Data were presented as mean, standard deviation (SD) and 95% confidence interval (CI) of the mean difference. Comparison of three groups (CGP, GAP, and NP) with respect to CRP values was done by one-way analysis of variance (ANOVA). Comparison of three groups (CGP, GAP, and NP) with respect to CRP values was done using Student's unpaired t-test. Correlation between variables was found by using Pearson's correlation coefficient “r”, and all levels of significance were set at P<0.05.
RESULTS
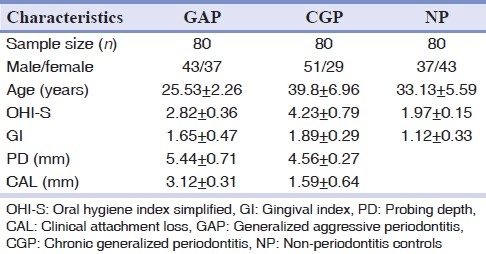
The patients’ characteristics of the three groups are summarized in Table 1. The GAP, CGP and NP groups depicted a mean age of 25.53±2.26, 39.80±6.96 and 33.13±5.59 years, respectively. The CGP group shows poor oral hygiene as well as higher gingival inflammation compared to GAP and NP groups. The mean value of PD (mm) was found to be 5.44±0.71 in GAP group and 4.56±0.27 in CGP group. The mean value of CAL (mm) was found to be 3.1±0.31 in GAP group and 1.59±0.64 in CGP group.
Table 1.
Subject characteristics
The mean CRP (mg/l) levels for the GAP, CGP and NP groups, as seen in Table 2 and Figure 1, were 7.49±2.31, 4.88±1.80 and 0.68±0.23, respectively. CRP values of the three patient groups were significantly different from each other, with CRP levels in the GAP group greater than those in the CGP group, which were in turn greater than those in the NP subjects.
Table 2.
Mean CRP (mg/l) levels in three groups (GAP, CGP, NP)
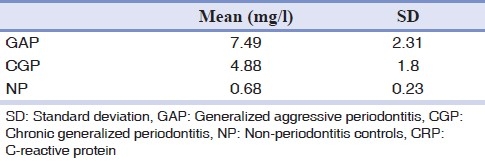
Figure 1.
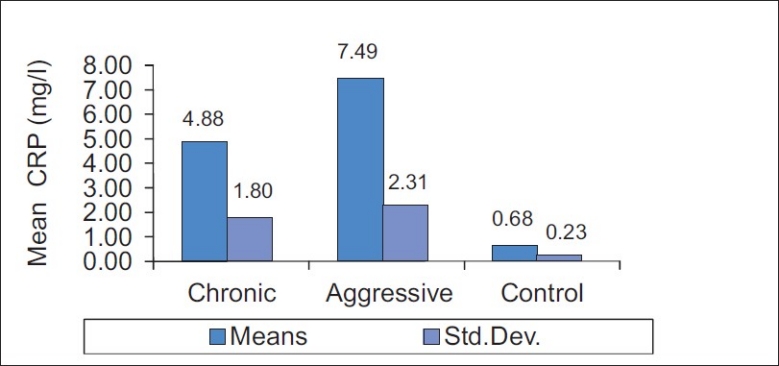
Comparison of three groups (generalized aggressive periodontitis, chronic generalized periodontitis and non-periodontitis controls) with respect to mean C-reactive protein (mg/l) values
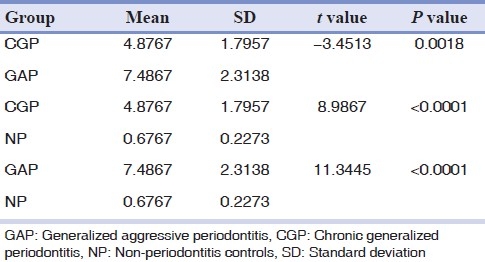
Furthermore, comparison of three groups (CGP, GAP, and NP) with respect to CRP values by one-way ANOVA showed statistical significance (P<0.0001), as seen in Table 3. Also, pairwise comparison of all three groups with respect to CRP values by Student's unpaired t-test [Table 4] illustrated statistical significance.
Table 3.
Comparison of three groups (generalized aggressive periodontitis, chronic generalized periodontitis and non-periodontitis controls) with respect to C-reactive protein values by one-way ANOVA
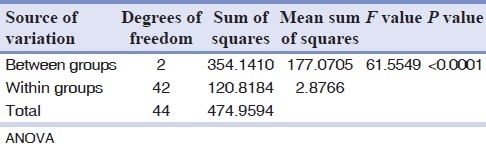
Table 4.
Pairwise comparison of three groups (generalized aggressive periodontitis, chronic generalized periodontitis and non-periodontitis controls) with respect to C-reactive protein values by Student's unpaired t-test
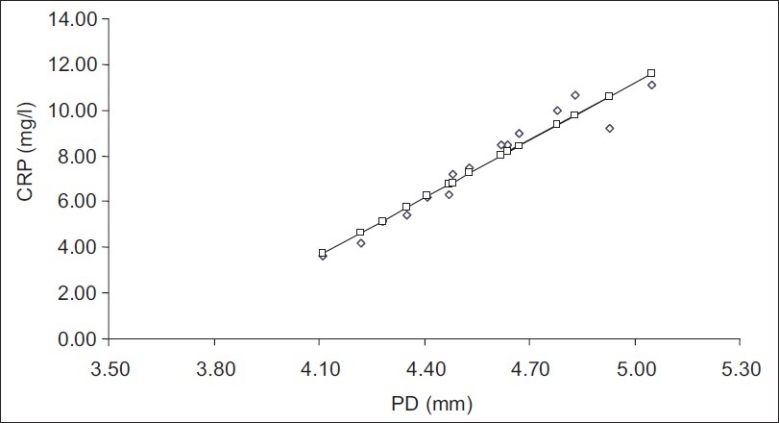
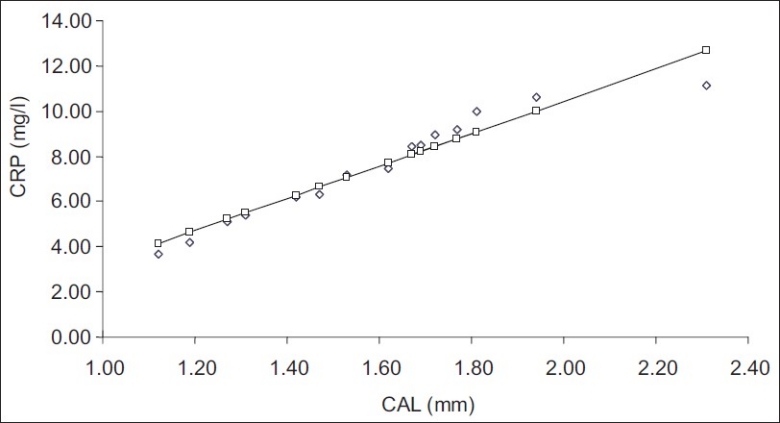
Correlation coefficient between CRP and PD was 0.9853, and between CRP and CAL was 0.8484 in CGP [Table 5]. They were significantly correlated and both the parameters increased with increasing CRP levels, thus indicating a positive correlation [Figures 2 and 3]. Correlation coefficient between CRP and PD was 0.9682, and between CRP and CAL was 0.9672 in GAP [Table 5]. Again, they were significantly correlated and all the parameters increased with increasing CRP levels, thus indicating a positive correlation [Figures 4 and 5].
Table 5.
Correlation coefficient between C-reactive protein, probing depth, and clinical attachment loss levels in chronic generalized periodontitis and generalized aggressive periodontitis
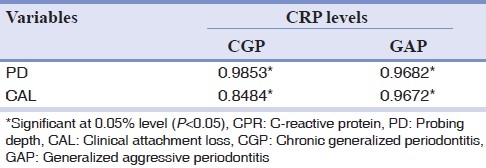
Figure 2.
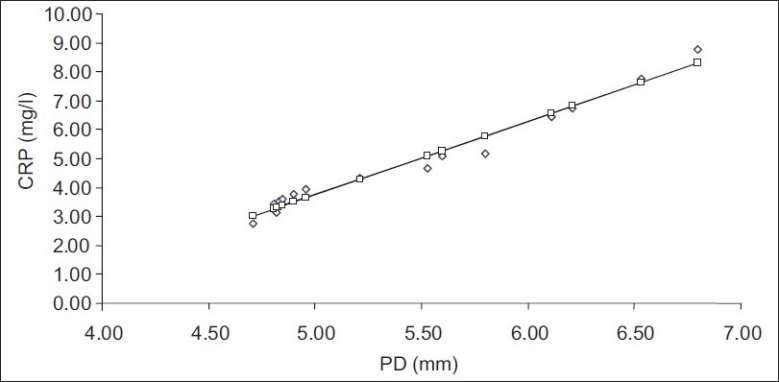
Correlation between C-reactive protein (mg/l) and probing depth (mm) in chronic generalized periodontitis
Figure 3.
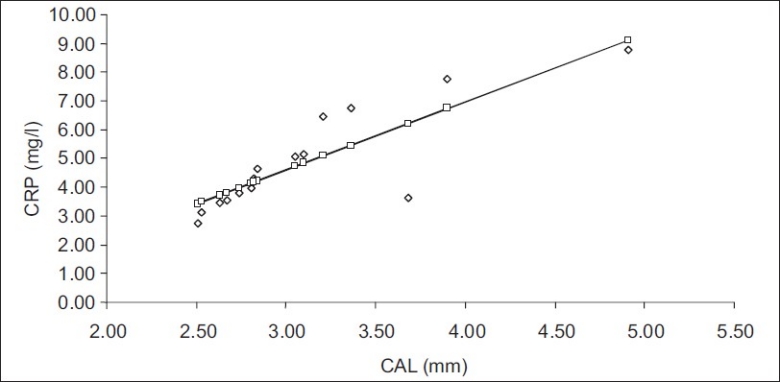
Correlation between C-reactive protein (mg/l) and clinical attachment loss (mm) in chronic generalized periodontitis
Figure 4.
Correlation between C-reactive protein (mg/l) and PD (mm) in generalized aggressive periodontitis
Figure 5.
Correlation between C-reactive protein (mg/l) and clinical attachment loss (mm) in generalized aggressive periodontitis
DISCUSSION
Periodontal disease is a chronic inflammatory destruction of tissues surrounding the teeth, caused by specific anaerobic pathogens contained in dental plaque organized on the tooth surfaces. Two major types of periodontal diseases are recognized: chronic periodontitis, which has a major prevalence in adults with a slow pattern of progression, and aggressive periodontitis, a less common type generally affecting young patients with rapid periodontal destruction that may result in tooth loss with esthetic, functional and psychological problems.
CRP is an acute-phase reactant protein synthesized by the liver in response to the inflammatory cytokines, IL-6, IL-1, and TNF-α. Circulating CRP levels are markers of systemic inflammation and are associated with periodontal disease.[7] Also of significance are the results of prospective longitudinal trials which indicate that this marker appears to be a useful predictor for future cardiovascular events in a variety of population.[8]
The present study evaluated CRP levels in chronic and aggressive periodontitis patients. All the subjects included in the study were systemically healthy and all the other risk factors for periodontitis were excluded. The subject characteristics are mentioned in Table 1. The mean CRP (mg/l) level for chronic periodontitis patients was 4.88±1.8 mg/l and for aggressive periodontitis patients was 7.49±2.3 mg/l, as compared to the control group with 0.68±0.23 mg/l as seen in Table 2. Comparison of three groups (CGP, GAP, and NP) with respect to CRP values by one-way ANOVA showed statistical significance (P<0.0001) as observed in Table 3.
The pairwise comparison of the three groups with respect to CRP values showed statistical significance with P=0.0018 for chronic periodontitis patients and for aggressive periodontitis patients, P<0.0001 for chronic periodontitis group and control group, and P<0.0001 for aggressive periodontitis patients and control group [Table 4]. These results are similar to those of studies which concluded that CRP levels in chronic periodontitis patients are higher than those of NP controls.[5,6,9] Similarly, another study concluded that CRP levels were elevated in aggressive periodontitis as compared to NP controls.[2] Here, we assessed CRP levels in chronic and aggressive periodontitis patients and compared them in both the groups. CRP levels were significantly higher in both the groups as compared to the controls, with the levels in chronic periodontitis group lying in between those of controls and aggressive periodontitis group.
The correlation coefficient between CRP levels and PD as well as CAL in CGP was found to be significant. With increasing mean PD and CAL, we could observe increase in CRP levels [Figures 2 and 3]. These findings are at par with those of a study done by James et al.[10] They reported positive association between periodontitis extent and CRP levels in terms of PD and CAL.
As in CGP, the correlation coefficient between CRP levels, and PD and CAL in GAP showed statistical significance. As the PD and CAL increased, the CRP levels were found to be increasing [Figures 3 and 4]. Also, PD showed maximum significance amongst all the parameters measured. These results are analogous to those reported by Salzberg et al.[2] They established a positive relationship between elevated CRP levels, and PD and CAL.
Both PD and CAL are helpful in measuring the severity and extent of periodontitis. They depict the periodontal destruction caused by periodontal pathogens and their products. These pathogens not only cause local inflammation and tissue destruction, but are also involved in systemic inflammation and immune responses. Thus, as the severity and extent of periodontal disease increase, the systemic component of inflammation also increases. This may be seen as increased production of CRP due to activation of cascade of inflammatory cytokine production in the presence of bacteria and bacterial products.[6]
Periodontitis is a mixed infection of supporting tissues of the teeth; dental plaque harbors many putative pathogens. Once the disease sets in, the subgingival tissues become inflamed and ulcerated. This provides a pathway for bacteria and bacterial products, such as lipopolysaccharide (LPS), as well as locally produced pro-inflammatory cytokines which enter the systemic circulation. Subsequently, the systemically dispersed bacteria and LPS, as well as cytokines from periodontal lesion, may stimulate hepatocytes to produce elevated CRP levels.[5]
The CRP levels in GAP were much higher compared to those in CGP as well as NP. This indicates that rapid alveolar bone destruction in GAP in the presence of cytokines must be adding to systemic inflammatory burden.
Also, these findings suggest that whenever there is an increase in PD and CAL, the serum CRP levels are raised. These findings are consistent with those of a study which established that CAL and PD were positively associated with CRP.[10] Similar results were found in another study, in which Lim et al concluded that CRP was a significant predictor of sites with PD ≥5 mm and could be a potential risk marker in periodontal destruction.[11] Thus, serum CRP levels can be a possible marker to depict active periodontal destruction and can differentiate progressive disease from a quiescent one.
These findings point to an association between rapidity of periodontal destruction and systemic inflammatory response as measured by serum CRP levels. Thus, periodontitis as a chronic infection may contribute to increase the burden of inflammatory markers like CRP. Lately, many studies have investigated the effect of periodontal treatment on serum CRP levels and reported a reduction in CRP levels following periodontal therapy.[12,13]
Recently, CRP has been proved to be the strongest and most significant predictor of future cardiovascular events.[6,14,15] The results of the present study suggest that elevated CRP levels in periodontitis patients can possibly contribute at least in part to the increased risk for CVD. This may be of particular concern in younger individuals, as represented by GAP patients where elevated levels of CRP due to periodontitis may contribute to early or more rapid CVD in susceptible patients.
CONCLUSION
Thus, there is a complementary need to recognize that apparently healthy individuals may be having extensive periodontal disease, which might be adding to systemic inflammation. Hence, periodontal disease assessment and its treatment should be instituted in current health programs to improve the overall health status of an individual. It should be noted, however, that an additional study in larger samples of patients might further investigate and confirm this idea.
ACKNOWLEDGMENTS
The authors thank Dr. Arun T. Miskin (general pathologist) and Prof. S. B. Jawali (statistician) for their help extended during this study. We appreciate the support provided by the staff members at Department of Periodontics, P. M. N. M. Dental College and Hospital.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Paraskevas S, Huizinga JD, Loos BG. A systemic review and meta-analyses on C-reactive protein in relation to periodontitis. J Clin Periodontol. 2008;35:277–90. doi: 10.1111/j.1600-051X.2007.01173.x. [DOI] [PubMed] [Google Scholar]
- 2.Salzberg TN, Overstreet BT, Rogers JD, Califano JV, Best AM, Schenkein HA. C-reactive protein levels in patients with aggressive periodontitis. J Periodontol. 2006;77:933–9. doi: 10.1902/jop.2006.050165. [DOI] [PubMed] [Google Scholar]
- 3.Picolos DK, Lerche-Sehm J, Abron A, Fine JB, Papapanou PN. Infection patterns in chronic and aggressive periodontitis. J Clin Periodontol. 2005;32:1055–106. doi: 10.1111/j.1600-051X.2005.00828.x. [DOI] [PubMed] [Google Scholar]
- 4.Slade GD, Offenbacher S, Beck JD, Heiss G, Pankow JS. Acute-phase inflammatory response to periodontal disease in the US population. J Dent Res. 2000;79:49–57. doi: 10.1177/00220345000790010701. [DOI] [PubMed] [Google Scholar]
- 5.Loos BG, Craandijk J, Hoek FJ, Wertheim-van Dillen PM, van der Velden U. Elevation of systemic markers related to cardiovascular diseases in the peripheral blood of periodontitis patients. J Periodontol. 2000;71:1528–34. doi: 10.1902/jop.2000.71.10.1528. [DOI] [PubMed] [Google Scholar]
- 6.Noack B, Genco RJ, Trevisan M, Grossi S, Zambon JJ, Nardin ED. Periodontal infections contribute to elevated systemic C-reactive protein level. J Periodontol. 2001;72:1221–7. doi: 10.1902/jop.2000.72.9.1221. [DOI] [PubMed] [Google Scholar]
- 7.Waranuch P, Kaumudi JJ, Janet W, Paige W, Chester WD, Mattew WG. Periodontitis and plasma C-reactive protein during pregnancy. J Periodontol. 2006;77:821–5. doi: 10.1902/jop.2006.050193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.D’Aiuto F, Ready D, Tonetti MS. Periodontal disease and C-reactive protein- associated cardiovascular risk. J Periodontal Res. 2004;39:236–41. doi: 10.1111/j.1600-0765.2004.00731.x. [DOI] [PubMed] [Google Scholar]
- 9.Craig RG, Yip JK, So MK, Boylan RJ, Socransky SS, Haffajee AD. Relationship of destructive periodontal disease to acute phase response. J Periodontol. 2003;74:1007–16. doi: 10.1902/jop.2003.74.7.1007. [DOI] [PubMed] [Google Scholar]
- 10.James BD, Offenbacher S. Relationship between clinical measures of periodontal disease and their associations with systemic markers. Ann Periodontol. 2002;7:79–89. doi: 10.1902/annals.2002.7.1.79. [DOI] [PubMed] [Google Scholar]
- 11.Lim LP, Tay FB, Sum CF, Thai AC. Relationship between markers of metabolic control and inflammation on severity of periodontal disease in patients with diabetes mellitus. J Clin Periodontol. 2007;34:118–23. doi: 10.1111/j.1600-051X.2006.01032.x. [DOI] [PubMed] [Google Scholar]
- 12.Bozkurt FY, Ay ZY, Delibas N. The effect of phase I therapy on blood lipid and CRP levels. J Clin Periodontol. 2003;30:149. [Google Scholar]
- 13.D’Aiuto F, Parkar M, Andreou G, Suvan J, Brett PM, Ready D, et al. Periodontitis and systemic inflammation. Control of the local infection is associated with a reduction in serum inflammatory markers. J Dent Res. 2004;83:156–60. doi: 10.1177/154405910408300214. [DOI] [PubMed] [Google Scholar]
- 14.Joshipura KJ, Wand HC, Merchant AB, Rimm EB. Periodontal disease and biomarkers related to cardiovascular disease. J Dent Res. 2004;83:151–5. doi: 10.1177/154405910408300213. [DOI] [PubMed] [Google Scholar]
- 15.Persson GR, Thomas P, Ola O, Stefan R. High-sensitivity serum C-reactive protein levels in subjects with or without myocardial infarction or periodontitis. J Clin Periodontol. 2005;32:219–24. doi: 10.1111/j.1600-051X.2005.00648.x. [DOI] [PubMed] [Google Scholar]


