Abstract
An adequate understanding of the relationship between periodontal tissues and restorative dentistry is paramount to ensure adequate form, function, esthetics and comfort of the dentition. While most clinicians are aware of this important relationship, uncertainty remains regarding specific concepts such as biologic width, its maintenance and applications of crown lengthening in cases of biologic width violation. Relevant publications regarding biologic width, its violation and management were identified up to August 2011 using manual and electronic database search in Medline, Embase, Directory of Open Access Journals and Google Scholar. This review discusses the concept of biologic width around tooth and its relationship to periodontal health and restorative dentistry.
Keywords: Biologic width, crown lengthening, periodontal health
INTRODUCTION
The relationship between periodontal health and the restoration of teeth is intimate and inseparable. Maintenance of gingival health constitutes one of the keys for tooth and dental restoration longevity.[1] An adequate understanding of relationship between periodontal tissues and restorative dentistry is paramount to ensure adequate form, function and esthetics, and comfort of the dentition.[2] Despite an increased emphasis on the perio-restorative interface in restorative dentistry, many clinicians have been unable to utilize the concept of biologic width in a practical manner.[3] Hence, the purpose of this paper is to describe the biologic width anatomy, evaluation and correction of its violation by different methods.
BIOLOGIC WIDTH ANATOMY
In the human body, ectodermal tissue serves to protect against invasion from bacteria and other foreign materials. However, both teeth and dental implants must penetrate this defensive barrier. The natural seal that develops around both, protecting the alveolar bone from infection and disease, is known as the biologic width.[4] The biological width is defined as the dimension of the soft tissue, which is attached to the portion of the tooth coronal to the crest of the alveolar bone. This term was based on the work of Gargiulo et al., who described the dimensions and relationship of the dentogingival junction in humans. Measurements made from the dentogingival components of 287 individual teeth from 30 autopsy specimens established that there is a definite proportional relationship between the alveolar crest, the connective tissue attachment, the epithelial attachment, and the sulcus depth. They reported the following mean dimensions: A sulcus depth of 0.69 mm, an epithelial attachment of 0.97 mm, and a connective tissue attachment of 1.07 mm. [Figure 1] Based on this work, the biologic width is commonly stated to be 2.04 mm, which represents the sum of the epithelial and connective tissue measurements.[5] In 1977, Ingber et al. described “Biologic Width” and credited D.Walter Cohen for first coining the term.[6]
Figure 1.
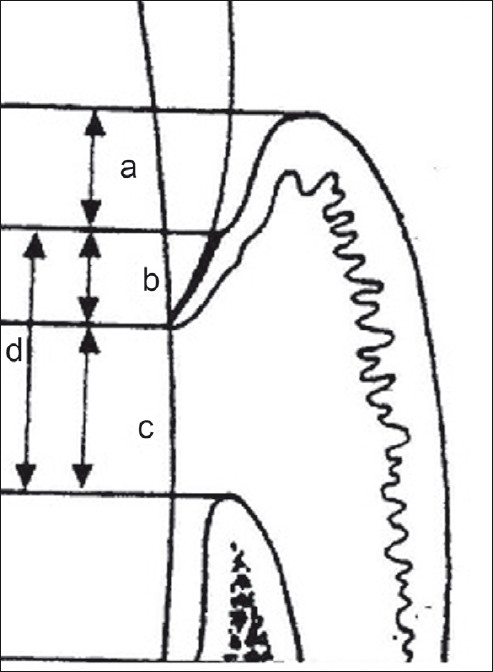
(a) Histological sulcus (0.69 mm), (b) Epithelial attachment (0.97 mm), (c) Connective tissue attachment (1.07 mm), (d) Biologic width (b+c)
The biologic width is essential for preservation of periodontal health and removal of irritation that might damage the periodontium (prosthetic restorations, for example). The millimeter that is needed from the bottom of the junctional epithelium to the tip of the alveolar bone is held responsible for the lack of inflammation and bone resorption, and as such the development of periodontitis. The dimension of biologic width is not constant, it depends on the location of the tooth in the alveolus, varies from tooth to tooth, and also from the aspect of the tooth. It has been shown that 3 mm between the preparation margin and alveolar bone maintains periodontal health for 4 to 6 months.[7] This 3 mm constitutes for 1 mm supracrestal connective tissue attachment, 1 mm junctional epithelium and 1 mm for gingival sulcus on an average. This allows for adequate biologic width even when the restoration margins are placed 0.5 mm within the gingival sulcus.[8]
Nevins and Skurow stated that when subgingival margins are indicated, the restorative dentist must not disrupt the junctional epithelium or connective tissue apparatus during preparation and impressing taking. The authors recommended limiting subgingival margin extension to 0.5-1.0 mm because it is impossible for the clinician to detect where the sulcular epithelium ends and the junctional epithelium begins.[9] In natural dentition, gingival morphology is partly related to the tooth shape and form. Tooth shape is classified in to triangular, ovoid and square; and, the tooth form as long narrow and short wide.[10] Individuals with square shaped teeth have more favorable aesthetic outcomes because of long proximal contacts and less of papillary tissue, where as a triangular tooth shape has a proximal tooth contact located more incisally and needs more tissue height to fill in; and hence, is at a high risk of the ‘black hole disease’.[11]
MARGIN PLACEMENT AND BIOLOGIC WIDTH
A clinician is presented with three options for margin placement: 1. Supragingival, 2. Equigingival, and 3. Subgingival locations.
Supragingival margin
It has the least impact on the periodontium. This margin location has been applied in non-esthetic areas due to the marked contrast in color and opacity of traditional restorative materials against the tooth. With the advent of more translucent restorative materials, adhesive dentistry, and resin cements, the ability to place supragingival margins in esthetic areas is now a reality.[2]
Advantages[7]
1. Preparation of the tooth and finishing of the margin is easiest 2.Duplication of the margins with impressions that can be removed past the finish line without tearing or deformation is the easiest with supragingival margins. 3. Fit and finish of the restoration and removal of excess material is easiest 4. Verification of the marginal integrity of the restoration is easiest. 5. The supragingival margins are least irritating to the periodontal tissue.
Equigingival margin
The use of equigingival margins traditionally was not desirable because they were thought to favour more plaque accumulation than supragingival or subgingival margins, and therefore result in greater gingival inflammation. There was also the concern that any minor gingival recession would create an unsightly margin display. These concerns are not valid today, not only because the restoration margins can be esthetically blended with the tooth but also because restorations can be finished easily to provide a smooth, polished interface at the gingival margin. From a periodontal viewpoint, both supragingival and equigingival margins are well tolerated.[2]
Subgingival margin
Restorative considerations will frequently dictate the placement of restoration margins beneath the gingival tissue crest because of caries or tooth deficiencies, and/or to mask the tooth/restoration interface. Invasion of biologic periodontal space for additional retention will cause iatrogenic periodontal disease with a premature loss of restoration. Restorative margin placement within the biologic width is detrimental to periodontal health and acts as a plaque retentive factor. When the restoration margin is placed too far below the gingival tissue crest, it will impinge on the gingival attachment apparatus and a constant inflammation is created and made worse by the patient's inability to clean this area. Body attempts to recreate room between the alveolar bone and the margin to allow space for tissue reattachment. This is more likely to occur in areas where the alveolar bone surrounding the tooth is very thin in width. Highly scalloped, thin gingiva is more prone to recession than a flat periodontium with thick fibrous tissue. The more common finding with deep margin placement is that bone level appears to remain unchanged; however, gingival inflammation develops and persists on the tooth restored.[12] Investigators have correlated that sub gingival restorations demonstrated more quantitative and qualitative changes in the micro flora, increased plaque index, gingival index, recession, pocket depth and gingival fluid.[13,14]
EVALUATION OF BIOLOGIC WIDTH VIOLATION
Clinical method
If a patient experiences tissue discomfort when the restoration margin levels are being assessed with a periodontal probe, it is a good indication that the margin extends into the attachment and that a biologic width violation has occurred. The signs of biologic width violation are: Chronic progressive gingival inflammation around the restoration, bleeding on probing, localized gingival hyperplasia with minimal bone loss, gingival recession, pocket formation, clinical attachment loss and alveolar bone loss. Gingival hyperplasia is most frequently found in altered passive eruption and subgingivally placed restoration margins.[7]
Bone sounding
The biologic width can be identified by probing under local anesthesia to the bone level (referred to as “sounding to bone”) and subtracting the sulcus depth from the resulting measurement. If this distance is less than 2 mm at one or more locations, a diagnosis of biologic width violation can be confirmed. This measurement must be performed on teeth with healthy gingival tissues and should be repeated on more than one tooth to ensure accurate assessment, and reduce individual and site variations.
Radiographic evaluation
Radiographic interpretation can identify interproximal violations of biologic width. However, on the mesiofacial and distofacial line angles of teeth, radiographs are not diagnostic because of tooth superimposition.[15] Sushama and Gouri have described a new innovative parallel profile radiographic (PPR) technique to measure the dimensions of the dento gingival unit (DGU). The authors infer that the PPR technique could be used to measure both length and thickness of the DGU with accuracy, as it was simple, concise, non-invasive, and a reproducible method.[16]
Categories of biologic width and margin placement guidelines to prevent biologic width violation
Kois proposed three categories of biologic width based on the total dimension of attachment and the sulcus depth following bone sounding measurements, namely: Normal Crest, High Crest and Low Crest.[17,18] [Figure 2]
Figure 2.
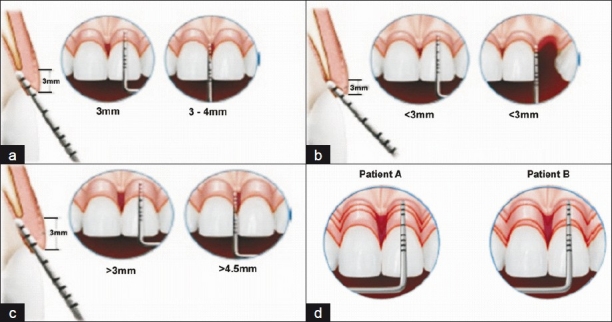
(a) Normal crest showing biologic width on labial and interproximal site, (b) High crest showing biologic width on labial and interproximal site. (c) Low crest showing biologic width on labial and interproximal site, (d) Pateint ALow crest unstable; and, Pateint B-. Low crest stable
Normal crest patient
In the Normal Crest patient, the mid-facial measurement is 3.0 mm and the proximal measurement is a range from 3.0 mm to 4.5 mm. [Figure 2a]. Normal Crest occurs approximately 85% of time. In these cases, the gingival tissue tends to be stable for a long term. The margin of a crown should generally be placed no closer than 2.5 mm from alveolar bone. Therefore, a crown margin which is placed 0.5 mm subgingivally tends to be well-tolerated by the gingiva, and is stable long term in the Normal Crest patient.
High crest patient
High Crest is an unusual finding in nature and occurs approximately 2% of the time. There is one area where High Crest is seen more often: In a proximal surface adjacent to an edentulous site. In the High Crest patient, the mid-facial measurement is less than 3.0 mm and the proximal measurement is also less than 3.0 mm [Figure 2b]. In this situation, it is commonly not possible to place an intracrevicular margin because the margin will be too close to the alveolar bone, resulting in a biologic width impingement and chronic inflammation.
Low crest patient
In the Low Crest patient group, the mid-facial measurement is greater than 3.0 mm and the proximal measurement is greater than 4.5 mm. [Figure 2c] Low Crest occurs approximately 13% of the time. Traditionally, the Low Crest patient has been described as more susceptible to recession secondary to the placement of an intracrevicular crown margin. When retraction cord is placed subsequent to the crown preparation; the attachment apparatus is routinely injured. As the injured attachment heals, it tends to heal back to a Normal Crest position, resulting in gingival recession.
Low crest, stable or unstable
However, the Low Crest attachment is actually more complex because all Low Crest patients do not react the same to an injury to the attachment. Some Low Crest patients are susceptible to gingival recession while others have a quite stable attachment apparatus. The difference is based on the depth of the sulcus, which can have a wide range. For example, If patient A is bone sounded and the mid-facial distance from the gingival crest to the alveolar crest is 5.0 mm, while patient B is bone sounded and the measurement is again 5.0 mm. By definition, both of these patients are Low Crest. However, they are not the same. Patient A has a 3.0- mm sulcus and a 2.0- mm attachment (i.e, epithelium and connective tissue). In contrast, Patient B has a 1.0- mm sulcus and a 4.0- mm attachment (ie, epithelium and connective tissue). [Figure 2d] Patient A has 3.0 mm of unsupported tissue from the base of the sulcus to the gingival crest. This amount of unsupported gingival tissue does not tend to be stable, and this patient is susceptible to gingival recession. However, Patient B has a more substantial attachment apparatus (4.0 mm) and a significantly shallower sulcus (1.0 mm). This patient is much less susceptible to gingival recession. Patient A is classified as an Unstable Low Crest because the patient is more susceptible to gingival recession. Patient B is classified as a Stable Low Crest because this patient reacts more like a Normal Crest patient and is not as susceptible to gingival recession.
Importance of determining the crest category
When preparing anterior teeth for indirect restorations, it is essential that the dentist should know about the Crest category. This allows the operator to determine the optimal position of margin placement, as well as inform the patient of the probable long-term effects of the crown margin on gingival health and esthetics. Based on the sulcus depth the following three rules can be used to place intracrevicular margins: 1) If the sulcus probes 1.5 mm or less, the restorative margin could be placed 0.5 mm below the gingival tissue crest. 2) If the sulcus probes more than 1.5 mm, the restorative margin can be placed in half the depth of the sulcus. 3) If the sulcus is greater than 2 mm, gingivectomy could be performed to lengthen the tooth and create a 1.5 mm sulcus. Then the patient can be treated as per rule 1.[15,19]
METHODS TO CORRECT BIOLOGIC WIDTH VIOLATION
Biologic width violations can be corrected by either surgically removing bone away from proximity to the restoration margin, or orthodontically extruding the tooth and thus moving the margin away from the bone.
Surgical crown lengthening
Crown –lengthening surgery is designed to increase the clinical crown length
Indications[20]
Inadequate clinical crown for retention due to extensive caries, subgingival caries or tooth fracture, root perforation, or root resorption within the cervical 1/3rd of the root in teeth with adequate periodontal attachment.
Short clinical crowns.
Placement of sub gingival restorative margins.
Unequal, excessive or unaesthetic gingival levels for esthetics.
Planning veneers or crowns on teeth with the gingival margin coronal to the cemeto enamel junction (delayed passive eruption).
Teeth with excessive occlusal wear or incisal wear.
Teeth with inadequate interocclusal space for proper restorative procedures due to supraeruption.
Restorations which violate the biologic width.
In conjunction with tooth requiring hemisection or root resection.
Assist with impression accuracy by placing crown margins more supragingivally.
Contraindications[20]
Deep caries or fracture requiring excessive bone removal.
Post surgery creating unaesthetic outcomes.
Tooth with inadequate crown root ratio (ideally 2:1 ratio is preferred)
Non restorable teeth.
Tooth with increased risk of furcation involvement.
Unreasonable compromise of esthetics.
Unreasonable compromise on adjacent alveolar bone support.
External bevel gingivectomy
Gingivectomy is a very successful and predictable surgical procedure for reconstruction of biologic width; however, it can be used only in situations with hyperplasia or pseudopocketing (> 3 mm of biologic width) and presence of adequate amount of keratinized tissue.[21]
Internal bevel gingivectomy
Reduction of excessive pocket depth and exposure of additional coronal tooth structure in the absence of a sufficient zone of attached gingiva with or without the need for correction of osseous abnormalities requires internal-bevel gingivectomy.[2]
Apical repositioned flap surgery
Indication
Crown lengthening of multiple teeth in a quadrant or sextant of the dentition, root caries, fractures.
Contraindication
Apical repositioned flap surgery should not be used during surgical crown lengthening of a single tooth in the esthetic zone.
Apically repositioned flap without osseous resection
This procedure is done when there is no adequate width of attached gingiva, and there is a biologic width of more than 3 mm on multiple teeth.
Apical repositioned flap with osseous reduction
This technique is used when there is no adequate zone of attached gingiva and the biologic width is less than 3 mm. The alveolar bone is reduced by ostectomy and osteoplasty, to expose the required tooth length in a scalloped fashion, and to follow the desired contour of the overlying gingiva. As a general rule, at least 4 mm of sound tooth structure must be exposed, so that the soft tissue will proliferate coronally to cover 2-3 mm of the root, thereby leaving only 1-2 mm of supragingivally located sound tooth structure.[22,23] Sugumari et al. in a report on surgical crown lengthening with apical repositioned flap with bone resection performed in the fractured maxillary anterior teeth region, showed satisfactory results both in terms of functional (restoring biologic width) and esthetic outcomes.[24]
Orthodontic techniques
Heithersay and Ingber were the first to suggest the use of “forced eruption” to treat “non-restorable” or previously “hopeless” teeth.[25] According to Starr, there are two concepts of forced eruption: Forced eruption with minimal osseous resection, and forced eruption combined with fiberotomy. Frank et al. described forced eruption of multiple teeth.[21] Since then, different clinicians have used various techniques to extrude teeth using removable devices or fixed brackets.[26,27] Forced eruption should be considered in cases where traditional crown lengthening via ostectomy cannot be accomplished, like in the anterior area, as ostectomy would lead to a negative architecture and also remove bone from the adjacent teeth, which can compromise the function of these teeth. Some of the contraindications to forced eruption are inadequate crown-to-root ratio, lack of occlusal clearance for the required amount of eruption and any possible periodontal complications.[28]
Healing after crown lengthening
Restorative procedures must be delayed until new gingival crevice develops after periodontal surgery. In non esthetic areas, the site should be re-evaluated atleast 6 weeks post surgically prior to final restorative procedures. In esthetic areas, a longer healing period is recommended to prevent recession. Wise recommends 21 weeks for soft tissue gingival margin stability. Therefore, restorative treatment should be initiated after 4-6 months. The margin of the provisional restoration should not hinder healing before the biologic width is established by surgical procedures.[29] Shobha et al. in a study on clinical evaluation of crown lengthening procedure had concluded that the biologic width can be re-established to its original vertical dimension along with 2 mm gain of coronal tooth structure at the end of six months.[30]
Complications after crown lengthening
As with any procedure, the patient needs to be informed of any potential complications such as possible poor aesthetics due to ‘black triangles’, root hypersensitivity, root resorption and transient mobility of the teeth.
CONCLUSION
The health of the periodontal tissues is dependent on properly designed restorations. Incorrectly placed restoration margin and unadapted restoration violates the biologic width. If the margin must be placed subgingivally, the factors to be taken into account are: Correct crown contour in the gingival third; correct polishing and rounding of the margin; sufficient zone of the attached gingiva; and, no biologic width violation by the margin. Repeated maintenance visits, patient co-operation and motivation are important for improved success of restorative procedures with pristine periodontal health.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Felippe LA, Monteiro Júnior S, Vieira LC, Araujo E. Reestablishing biologic width with forced eruption. Quintessence. 2003;34:733–8. [PubMed] [Google Scholar]
- 2.Khuller N, Sharma N. Biologic width: Evaluation and correction of its violation. J Oral Health Co mm Dent. 2009;3:20–5. [Google Scholar]
- 3.Robbins JW. Tissue management in restorative dentistry. Funct Esthet Restor Dent. 2007;1:40–3. [Google Scholar]
- 4.Makigusa K. Histologic comparison of biologic width around teeth versus implant: The effect on bone preservation. J Implant Reconstr Dent. 2009;1:20–4. [Google Scholar]
- 5.Gargiulo AW, Wentz FM, Orban B. Dimensions and relations of the dentogingival junction in humans. J Periodontol. 1961;32:261–7. [Google Scholar]
- 6.Ingber JS, Rose LF, Coslet JG. The “biologic width”—a concept in periodontics and restorative dentistry. Alpha Omegan. 1977;70:62–5. [PubMed] [Google Scholar]
- 7.Jorgic-Srdjak K, Plancak D, Maricevic T, Dragoo MR, Bosnjak A. Periodontal and prosthetic aspect of biological width part I: Violation of biologic width. Acta Stomatol Croat. 2000;34:195–7. [Google Scholar]
- 8.Rosenberg ES, Cho SC, Garber DA. Crown lengthening revisited. Compend Contin Educ Dent. 1999;20:527. [PubMed] [Google Scholar]
- 9.Nevins M, Skurow HM. The intracrevicular restorative margin, the biologic width, and the maintenance of the gingival margin. Int J Periodont Restor Dent. 1984;4:30–49. [PubMed] [Google Scholar]
- 10.Olsen M, Lindhe J. Periodontal characteristics in individuals with varying form of the upper central incisor. J Clin Periodontol. 1991;18:78–82. doi: 10.1111/j.1600-051x.1991.tb01124.x. [DOI] [PubMed] [Google Scholar]
- 11.Dhir S. The Peri-implant esthetics: An unforgettable entity. J Indian Soc Periodontol. 2011;15:98–102. doi: 10.4103/0972-124X.84375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Waerhaug J. Healing of the dento-epithelial junction following subgingival plaque control.II: As observed on extracted teeth. J Periodontol. 1978;49:119–34. doi: 10.1902/jop.1978.49.3.119. [DOI] [PubMed] [Google Scholar]
- 13.Valderhaug J, Birkeland JM. Periodontal conditions in patients 5 years following insertion of fixed prostheses. Pocket depth and loss of attachment. J Oral Rehabil. 1976;3:237–43. doi: 10.1111/j.1365-2842.1976.tb00949.x. [DOI] [PubMed] [Google Scholar]
- 14.Newman, Takei, Klokkevold . Carranza's Clinical Periodontology. 10th ed. Philadelphia: Saunders, Elsevier Publishing; 2006. pp. 1050–69. [Google Scholar]
- 15.Galgali SR, Gontiya G. Evaluation of an innovative radiographic technique- parallel profile radiography- to determine the dimensions of the dentogingival unit. Indian J Dent Res. 2011;22:237–41. doi: 10.4103/0970-9290.84294. [DOI] [PubMed] [Google Scholar]
- 16.Kois J. Altering gingival levels: The restorative connection, Part 1: Biologic variables. J Esthet Dent. 1994;6:3–9. [Google Scholar]
- 17.Kois JC. The restorative-periodontal interface: Biological parameters. Periodontol 2000. 1996;11:29–38. doi: 10.1111/j.1600-0757.1996.tb00180.x. [DOI] [PubMed] [Google Scholar]
- 18.Robinson PJ, Vitek RM. The relationship between gingival infla mmation and the probe resistance. J Periodontal Res. 1975;14:239–43. doi: 10.1111/j.1600-0765.1979.tb00229.x. [DOI] [PubMed] [Google Scholar]
- 19.Freeman K, Bebermeyer R, Moretti A, Koh S. Single-tooth crown lengthening by the restorative dentist: A case report. J Greater Houston Dent Soc. 2000;2:14–6. [Google Scholar]
- 20.Jorgic-Srdjak K, Dragoo MR, Bosnjak A, Plancak D, Filipovic I, Lazic D. Periodontal and prosthetic aspect of biological width part II: Reconstruction of anatomy and function. Acta Stomatol Croat. 2000;34:441–4. [Google Scholar]
- 21.Smukler H, Chaibi M. Periodontal and dental considerations in clinical crown extension: A rationale basis for treatment. Int J Periodont Restor Dent. 1997;17:464–77. [PubMed] [Google Scholar]
- 22.Pontoriero R, Carnevale G. Surgical crown lengthening: A 12- month clinical wound healing study. J Periodontol. 2001;72:841–8. doi: 10.1902/jop.2001.72.7.841. [DOI] [PubMed] [Google Scholar]
- 23.Elavarasu S, Kermani K, Thangakumaran S, Jeyaprakash GS, Maria R. Apically repositioned flap in reconstruction of mutilated teeth. JIADS. 2010;1:63–6. [Google Scholar]
- 24.Heithersay GS. Combined endodontic-orthodontic treatment of transverse root fractures in the region of the alveolar crest. Oral Surg Oral Med Oral Pathol. 1973;36:404–15. doi: 10.1016/0030-4220(73)90220-x. [DOI] [PubMed] [Google Scholar]
- 25.Durham T, Goddard T, Morrison S. Rapid forced eruption: A case report and review of forced eruption techniques. Gen Dent. 2004;48:167–75. [PubMed] [Google Scholar]
- 26.Murchison DF, Schwartz RS. The use of removable appliances for forced eruption of teeth. Quintessence Int. 1986;17:497–501. [PubMed] [Google Scholar]
- 27.Uddin M, Mosheshvili N, Segelnick SL. A new appliance for forced eruption. N Y State Dent J. 2006;72:46–50. [PubMed] [Google Scholar]
- 28.Wise MD. Stability of the gingival crest after surgery and before anterior crown placement. J Prosthet Dent. 1985;53:20–3. doi: 10.1016/0022-3913(85)90057-5. [DOI] [PubMed] [Google Scholar]
- 29.Shobha KS, Mahantesha, Seshan H, Mani R, Kranti K. Clinical evaluation of the biologic width following surgical crown lengthening procedure: A prospective study. J Indian Soc Periodontol. 2010;14:160–7. doi: 10.4103/0972-124X.75910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Robbins JW. Tissue management in restorative dentistry. Funct Esthet Restor Dent. 2007;1:40–3. [Google Scholar]


