Abstract
Bowel ischemia is a rare and potential life-threatening disorder. The reason for its rarity is the difficulty in its diagnosis. Vague and nonspecific clinical findings and limitations of diagnostic and treatment options make this disease a significant challenge. We hereby report two cases of non-occlusive mesenteric ischemia and the use of cilostazol in the successful management of such cases.
Keywords: Cilostazol, non-occlusive mesenteric ischemia
INTRODUCTION
The spectrum of ischemic bowel disease consists of varied degree of occlusion of celiac trunk, Superior and inferior mesenteric vessels,[1] which include arterial as well as venous occlusion, non-occlusive causes like intestinal vasospasm, atherosclerotic disease and vasculitic disorders. Patients with ischemic bowel disease may present with a history of postprandial pain, typically starting 20-30 minutes after their last meal, some patients present with acute onset of pain which is often disproportionate to physical findings.[2] If not caught early, complications such as sepsis and necrosis can occur as soon as 10-12 hours after the onset of symptoms. Streptokinase and Urokinase, Papaverine, Heparin, Warfarin have all been used in the medical management of occlusive mesenteric ischemia. Patients with non-occlusive ischemia are treated with antiplatelet therapy.[3] With respect to bowel ischemia treatment modalities are few and invasive in some cases. There are no type I data (randomized controlled trials) and there is only few type II data (nonrandomized controlled trials, collaborator case-controlled trials with historical controls), but a surplus of type III data (descriptive studies, blind experience and expert reports).[4,5] The knowledge on this elusive disease is based on such publications. Our experience shows that cilostazol used in the management of non-occlusive bowel ischemia carries an extremely favorable outcome.
CASE REPORTS
Case 1
A 60-year-old female patient, diabetic and hypertensive with primary hypothyroidism of several years duration on regular treatment, presented with moderate to severe pain abdomen of 6-8-week duration.
Pain was more in the upper abdomen radiating diffusely. Pain was precipitated by food intake. The pain was so significant that the patient was scared to consume food and had lost 6 kgs over 2 months. Abdominal examination revealed periumbilical and epigastric tenderness with no organomegaly. Ultrasound abdomen and Echocardiography was normal. Plain X-ray abdomen revealed calcification of abdominal aorta. Upper GI endoscopy showed multiple ulcers of varying sizes at antrum and duodenum extending to distal duodenum. Patient was subjected to enteroscopy which revealed several similar ulcers along small intestine. Patient complained of persistent postprandial pain, not relieved by PPI/Antacids and a diagnosis of abdominal angina was considered. CT angiography of abdomen revealed short segment narrowing of the proximal part of the superior mesenteric artery [Figure 1].
Figure 1.

CT angiography of abdomen revealed short segment narrowing of the proximal part of the superior mesenteric artery.
Case 2
A 42-year-old male patient presented to the emergency room with history of pain abdomen since day 1. Pain was sudden in onset, burning type present over epigastric region and nonradiating. On examination, guarding was present. Patient was a known case of type 2 Diabetes mellitus and ischemic heart disease. Investigations showed, serum amylase 49 U/I . USG-Abdomen, X-Ray erect Abdomen and Echocardiography were normal CT Angiography-Abdomen showed thickening and wall edema of proximal ileal coils, narrowing of the proximal part of the celiac trunk. [Figure 2]
Figure 2.
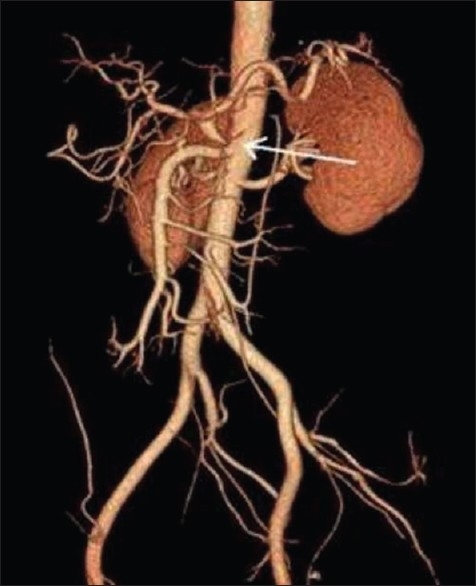
CT angiography-abdomen showed thickening and wall edema of proximal ileal coils, narrowing of the proximal part of the celiac trunk.
Both cases were put on cilostazol 100 mg BID. Over the next 48-72 hours, both patients had shown improvement of symptoms. They were relieved of abdominal angina and were symptom-free by the end of 1st week. The first patient has been on follow-up for over 4 years on cilostazol during which she has not experienced similar pain abdomen. Repeat upper GI endoscopy after 4 weeks showed no evidence of ulcers in the stomach. The second patient has also been under follow-up on medication for 6 months and is also symptom free. Similar is our experience with other cases also.
DISCUSSION
The intestinal mucosa has a high metabolic rate and a high blood flow requirement. Decreased perfusion in the intestine leads to ischemia leading to disruption of mucosal barrier, allowing release of bacteria, toxins, and vasoactive mediators, which in turn leads to myocardial depression and systemic inflammatory response. Bowel ischemia can be of three types, embolic, thrombotic (acute) or non-occlusive causes (chronic).[3]
Cilostazol is a selective inhibitor of type 3 phosphodiesterase, with therapeutic focus on increasing cAMP. An increase in cAMP results in an increase in the active form of Protein Kinase A, which is directly related with an inhibition in platelet aggregation and vasodilatation. Studies done in Japan have shown cilostazol to reduce triglycerides and increase HDL cholesterol.[6]
This triple effect on circulating plasma lipids, platelet aggregation and vasodilatation makes cilostazol effective in the treatment of PVD. The same mechanism of action is responsible in the management of non-occlusive mesenteric ischemia. Our experience with cilostazol in the treatment of NOMI has shown promising results. Invasive interventions though effective have their own limitations. Cilostazol should be a cost-effective and early modality of treatment for a disease where satisfactory therapy is still eluding us. To the best of our knowledge use of Cilostazol in the treatment of bowel ischemia has not been reported in literature.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Moawad J, Gewertz BL. Chronic mesenteric ischemia Clinical presentation and diagnosis. Surg Clin North Am. 1997;77:357–69. doi: 10.1016/s0039-6109(05)70554-5. [DOI] [PubMed] [Google Scholar]
- 2.Burns BJ, Brandt LJ. Intestinal ischemia. Gastroenterol Clin North Am. 2003;32:112743. doi: 10.1016/s0889-8553(03)00093-1. [DOI] [PubMed] [Google Scholar]
- 3.Sreenarasimhaiah J. Diagnosis and management of intestinal ischaemic disorders. BMJ. 2003;326:1372–6. doi: 10.1136/bmj.326.7403.1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hoyt DB. Clinical practice guidelines. Am J Surg. 1997;173:32–4. doi: 10.1016/S0002-9610(96)00378-9. [DOI] [PubMed] [Google Scholar]
- 5.Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, et al. ACC/AHA 2005 Guidelines for the Management of Patients with Peripheral Arterial Disease (Lower Extremity, Renal, Mesenteric, and Abdominal Aortic) J Am Coll Cardiol. 2006;47:1239–312. doi: 10.1016/j.jacc.2005.10.009. [DOI] [PubMed] [Google Scholar]
- 6.Elam MB, Heckman J, Crouse JR, Hunninghake DB, Herd JA, Davidson M, et al. Effect of the Novel Antiplatelet Agent Cilostazol on Plasma Lipoproteins in Patients With Intermittent Claudication. Arterioscler Thromb Vasc Biol. 1998;18:1942–7. doi: 10.1161/01.atv.18.12.1942. [DOI] [PubMed] [Google Scholar]


