Abstract
HIV has now become a manageable chronic disease. However, the treatment outcomes may get hampered by suboptimal adherence to ART. Adherence optimization is a concrete reality in the wake of ‘universal access’ and it is imperative to learn lessons from various studies and programmes. This review examines current literature on ART scale up, treatment outcomes of the large scale programmes and the role of adherence therein. Social, behavioural, biological and programme related factors arise in the context of ART adherence optimization. While emphasis is laid on adherence, retention of patients under the care umbrella emerges as a major challenge. An in-depth understanding of patients’ health seeking behaviour and health care delivery system may be useful in improving adherence and retention of patients in care continuum and programme. A theoretical framework to address the barriers and facilitators has been articulated to identify problematic areas in order to intervene with specific strategies. Empirically tested objective adherence measurement tools and approaches to assess adherence in clinical/ programme settings are required. Strengthening of ART programmes would include appropriate policies for manpower and task sharing, integrating traditional health sector, innovations in counselling and community support. Implications for the use of theoretical model to guide research, clinical practice, community involvement and policy as part of a human rights approach to HIV disease is suggested.
Keywords: ART, ARV, follow up, HIV, non-adherence, retention, self reporting
Introduction
Development of drugs and the design of simple and standardized approaches for therapy in the developing world witnessed a public health triumph after the approval of AZT (Azidothymidine or z0 idovudine) in 1987 by Food and Drug Administration of United States1. In the initial period, HIV infected individuals started with treatment through private sector, however, subsequently patients tended to stop treatment owing to the cost of antiretrovirals (ARVs). Irrational prescription practices and leaving patients half-way through the therapy when they ran out of money have been seen in treatment of many other communicable diseases and this was being anticipated for antiretroviral treatment also. In September 2003, lack of access to antiretroviral therapy (ART) was described as ‘a global health emergency’ and an international initiative namely the ‘3-by-5 initiative’, was launched to treat 3 million people living with HIV/AIDS by the year 20052. In 2003, the government of India announced roll-out of free ART and subsequently launched the programme in 2004 at eight tertiary-level government hospitals in six high prevalence states: Andhra Pradesh, Karnataka, Maharashtra, Tamil Nadu, Manipur, Nagaland and National Capital Territory (NCT) of Delhi. Later on, the National AIDS Control Programme (NACP)-III set its target to provide free ART to 300000 adults and 40000 children by 2012 through 250 ART centres to maintain > 95 per cent of drug adherence and minimize loss to follow up (< 5%)3. To facilitate access to ART nearer to beneficiaries’ home, 650 Link ART Centers (LAC) have been established. The LAC also bridges the government integrated counselling and testing centres (ICTCs) and ART centers3.
In this paper, we aim to present problems associated with adherence to ART to strengthen programme and provide recommendations with the intention of providing clarity to the specialist and non-specialist stakeholders.
HIV: A chronic manageable disease
Except among MSM (men having sex with men) population, overall HIV prevalence seems to have stabilized worldwide4,5. The primary goals of ART include maximal and durable reduction in plasma viral load, restoration of immunological functions which ultimately aim at prolongation of life and improvement in quality of life. Thus the numbers of people living with HIV increases steadily as the population grows and their survival time also increases6. In developed world like Europe and North America, average life expectancy has been shown to increase by 13 years between the years 1996-1999 and 2003-2005 because of ART7. Thus, with improved survival prospects HIV has transitioned into chronic disease particularly when ART has become both affordable and accessible in low- and middle-income countries8,9. Nevertheless morbidities, disabilities, mortality and ageing would need to be closely monitored owing to adherence problems, side effects, treatment failures and issues around second line and tertiary regimens.
Chronic disease management is fundamentally different from acute care. It relies on several features such as detection of early disease, a combination of pharmacological and psychosocial interventions. The most important issue is long-term follow up with regular monitoring, promotion of adherence to treatment and involvement of family care giver/s. Primary goals of ART can be achieved only if patients have high adherence to ART at all stages of life. Most of the studies conducted in resource-limited settings, however, have focused solely on adherence to treatment and have provided limited information on effective and practical approaches to improve both adherence as well as retention in care. Non-adherence or suboptimal adherence to ART may ultimately lead to failure of primary regimen10. Therefore, management issues for HIV need to be understood in the context of chronic disease management especially focusing on adherence and retention.
Adherence to antiretroviral therapy
Adherence is defined as a patient's ability to follow a treatment plan, take medications at prescribed times and frequencies, and follow restrictions regarding food and other medications. Adherence includes several operational subunits of definition. For example, adherence to dosage means number of pills taken as prescribed, adherence to schedule means taking pills consistently on time and finally dietary adherence is taking pills as prescribed with/ after/ or before meal11. With the advent of new drugs having long half life, adherence gains more importance as sudden stopping of drugs increases chances of developing resistance to drugs. The national guidelines in India stipulates >95 per cent adherence to first line regimen12.
Adherence assessment
Various tools and methods have been used for assessing adherence in randomized controlled trials and these are also evaluated in comprehensive reviews and meta-analyses. There is no ‘gold standard’ for adherence assessment. Self reporting is the most commonly used measure of adherence in resource- limited settings because it is easy to include in routine clinical practice. However, reliability of answers to the adherence assessment questions might get influenced by patients’ desires to provide socially acceptable answers or mere forgetfulness on the part of the patients13,14. Additionally, adherence also depends on patient provider relationship. These concerns about reliability of adherence by self report get attested by several studies that have shown discrepancy between self reported adherence and biomedical markers15. A report from Mumbai in India has shown viral suppression to be associated with participant self-reported adherence16.
There are some of the objective measures of adherence generally used in research. These measures have been found to be more sensitive than patients’ self-reports for detecting medication adherence. Clinical studies have employed medication event monitoring system17,18 (MEMS), pharmacy refill data19, providers’ estimates20,21 and directly observed therapy (DOT) or directly administered ART (DART) either alone or in combination to measure ART adherence10,22. The current national ART programme in India uses pill count method for assessing adherence. But this method might not give exact compliance calculation as it does not match with number of missed pills (self) reported by patient23 leading to discrepancies between pill count by provider and self report by patient. After being on ART for some time, the patient gets habituated to pill count exercise and manages to bring exact number of pills to the clinic. He/ she may either be throwing pills every day or removing them from the bottles just before visiting the clinic. It is obvious that being a patient enabled issue, any adherence measure related to patient (report/ pill count) has its own disadvantages owing to the psychosocial need of social desirability or merely to avoid reprimand from health care provider.
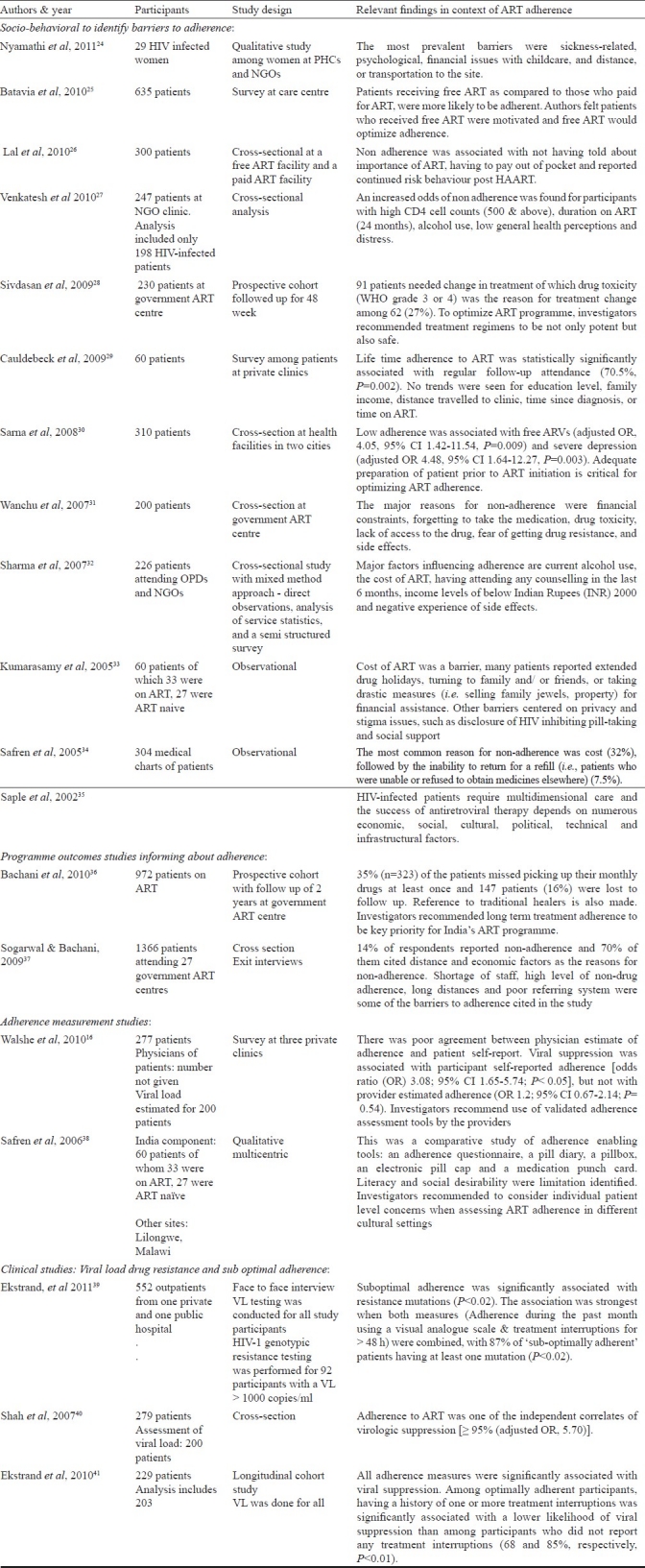
In India, studies have either very briefly discussed or just touched upon the adherence issues (Table I)16,24–41. Systematic studies focusing on ART adherence assessment and issues around adherence within the cultural context are limited.
Table I.
An overview of studies on adherence to ART in India
A single isolated method of adherence assessment seems to be inadequate and impractical. Use of more than one ART adherence measures to capture more accurate information to determine adherence levels have been recommended42. A study comparing adherence to a fixed dose combination (FDC) of Nevirapine, Stavudine and Lamivudine using Nevirapine plasma level monitoring and patient self-report showed that the ‘self-reported’ adherence was significantly higher than adherence measured by the Nevirapine level monitoring43. Measurement of adherence through drug level monitoring is considered sensitive method, yet it has not been used widely because it would be impractical in clinical settings. Other than these methods, a combination approach of pill count and patient report along with CD4 counts and viral load estimation might provide better estimates of patients’ adherence to the treatment44 because viral load serves as a surrogate marker of adherence and clinical outcome. It is clear that an integrated approach of clinical and laboratory monitoring along with patient/ provider enabled adherence measure could be a stronger way to assess adherence. CD4 count along with viral load estimation could be a more practical way of assessing adherence than drug level monitoring in addition to self reports and pill count. Hence, viral load estimation at least annually should be included in the national ART programme in India.
Non adherence, interruptions and retention failure
Adherence is a problem in any chronic disease and average non-adherence rate of 24.8 per cent have been reported45 with the highest rate in patients with HIV, arthritis and gastrointestinal disorders. Consistent adherence among patients with chronic conditions is low and it was reported to drop as early as after the first six months of therapy46. In case of HIV, ART is known to be efficacious but adherence to ART is strikingly behaviour dependent; it depends on sustained retention and cascade effect is foreseen. Worldwide, non-adherence to antiretroviral therapy in adult HIV infected population ranges from 33 to 88 per cent47. Some of the subjective reasons for non-adherence often cited by the patients are distress due to side effects, lack of insight and non belief in treatment, substance abuse, low self esteem and inability to identify the stressors of life. Treatment regimen characteristics, patient characteristics and patient provider relationship have been identified as barriers for ART adherence by the World Health Organization2. Other situations include consistent under- or over-dosing, abrupt over-dosing (neglecting to take medication properly for a period of time, then over-dosing just before a visit to the clinic), drug holidays, random administration (taking drugs whenever the thought occurs), incorrect administration because of not comprehending the physician's prescription and prematurely terminating the medication without consulting the health care provider48,49. Pill taking behaviours like intervals and variation in pill intake might look innocuous but variability in pill intake behaviours of HIV infected patients has been shown to play key role in virologic failure despite reported adherence50. Apart from these, social construction of masculinity; gender and household dynamics may prevent some women from successfully adhering to ART51.
Evidence from ART programme: The treatment outcomes for public ART programme have provided evidence for high adherence, treatment success and survival37,52–54. However, sustainability of optimal adherence in large scale public ART programmes might be a challenge, a cascade effect is observed with the initial enthusiasm diminishing with time, both among patients and health care providers alike. Long-term treatment adherence was recommended to be a key priority for India's ART programme. However, 35 per cent of the patients missed picking up their monthly drugs at least once and 16 per cent were lost to follow up in a period of 2 years of Indian ART programme36. Dahab et al55 have emphasized that as the ART delivery programmes grow beyond pilot phases, focus on maintaining high levels of adherence is essential.
Retention: The public ART programmes in resource-poor settings face major obstacle of retention which eventually leads to non-adherence even among those patients who ‘behaviourally’ believe themselves to be adherent. Retention might emerge as problem as early as right in the beginning when a patient registers for ART (Pre ART) and has to wait till he/ she becomes eligible for ART initiation. Subsequently when the ART is initiated, the drop out could be temporary (temporary migration, vacation, lack of money, sickness, etc.); periodic (attitude of patient, work and other responsibilities, switching to traditional medicine, sickness) and permanent (death, mobility, unable to pool resource for travel to pick drugs/ come for investigations, transitioned to alternative medicine or other sources, religious belief).
Factors affecting adherence to ART
Factors influencing adherence and retention have been thematically identified as pre ARV loss, side effects, socio-cultural factors, switch to alternative medicine system and factors related to vulnerable populations.
Pre-ARV loss: Worldwide, substantial numbers of patients have been reported dropped from the programme even before they start taking the treatment56. Patients registered for ART are most often asymptomatic, they would not have insight to continue reporting for follow ups yet they need retention and behavioural intervention the most. Patients registered as ‘Pre ART’ need to be handled cautiously as they are the reservoirs of HIV ‘on their own’ with limited intervention to relieve them from stress, no guidance to protect others with no mechanism for follow up instituted for them in the programme. Sarna et al30 have cautioned about the challenges in adherence and felt that the provision of free treatment without adequate patient preparation and adherence support might compromise the success of ART scale-up programme.
Side effects: When the patients are initiated on ART, a lot depends on their preparation and education regarding side effects. Their understanding of occurrence and nature of side effects could be limited and may get influenced by contextual factors. Social and psychological factors start playing havoc in patients’ life when they start experiencing side effects. Side effect is often construed by both patients and their family members as ‘becoming sicker’ after being treated with ART. A retrospective analysis of medical records of 345 randomly selected antiretroviral-naive patients showed that 61 per cent of patients changed or discontinued their initial ART regimen; 24 per cent did so because of an adverse event57. Gastrointestinal adverse events of ART were the most frequently cited reason for discontinuation of ART. The experience of side effects with its associated influence on activities of daily living and quality of life is known to have led to treatment fatigue and ART non-adherence in many other studies58. Some of the studies in India have reported relationship between side effects and ART adherence27–31. Sivadasan et al28 found that WHO grade 3 or 4 toxicities were the reasons for change in ART in 27 per cent south Indian patients. A study conducted among 60 patients in India reported common side-effects causing non-adherence as metabolic reasons (66%) and GI symptoms (50%)30. It is important to note that not all side effects are seen immediately after ART initiation. Visible side effects like lipoatrophy or dystrophy leading to central obesity and thinning of limbs due to long term use of s0 tavudine may arouse community suspicion leading to stress and non-adherence among patients who might be otherwise stable on ART. Preparing patients for unavoidable side-effects is critical. Patients are known to approach their family doctors or community doctors in case they start feeling that the medicines are giving ‘trouble’. Educating private practitioners and community doctors would contribute to ART adherence optimization in programme. Systematic in-depth studies are needed to get an emic perspective of understanding of side effects, how patients and their family care givers deal with it and where do they seek advice for further treatment if they feel dissatisfied with the service.
Socio-cultural factors: Barriers to ART adherence have been identified as treatment (complex dosing schedule), behavioural (alcohol and substance abuse), HIV knowledge related and psychological (depression)59. Major barriers to ART adherence in India are economic factors (Table I). Not having money for travel to ART centre, hunger and waiting time were identified as barriers to ARV adherence similar to African setting60. Lack of money and livelihood issues result in food insecurity. Growing body of literature provides evidence that livelihood is an all encompassing socio-behavioural barrier that can reduce adherence to ART and increase gastrointestinal diseases due to lack of much needed food to go along with ART61,62. In a systematic review of studies in low- and middle-income countries, higher education was associated with adherence63 but some studies reported negative association between education and adherence31,64. Psychological state could be a reason behind such findings. In another study among HIV test seekers, anxiety was shown to be associated with higher education65 and this could explain negative association of higher education with ART adherence. Such patients may tend to self medicate. Mental health was a reported barrier to adherence among Chinese patients66. Anxiety and mental health should be assessed among patients who might not be accessing correct information leading to non-compliance/ non-adherence.
Switch/transition to other systems of medicine: Patients have been known to access health care generally and ART specifically with the alternative/ complementary health practitioners67,68. Studies in Uganda, Zambia, the United States of America, Canada, Australia and India have found that use of complementary and alternative medicines is associated with poor adherence to ART55,69–73. A survey of 1,667 HIV-infected persons in 4 regions of India found that 41 per cent reported using some form of traditional medicine although only 5 per cent believed that traditional medicine was more effective than allopathic ART71. Another study from southern India showed that at some point of time patients switch to community doctors72. The alarming issue in this study was that community doctors had many misconceptions regarding HIV transmission, diagnosis and treatment.. Studies evaluating the impact of traditional medicine practice on ART adherence in India are very limited. One of the studies in India found that among the patients who were referred to speciality centers owing to their poor response to ART, only 10 per cent had adhered to treatment, 50 per cent had stopped taking drugs on advice of traditional healers35.
Issues among vulnerable population: Female sex workers, men who have sex with men and injecting drug users are disproportionately affected by HIV, yet are away from the mainstream. Measuring and identifying factors that influence adherence among disproportionately affected subgroups is necessary to optimize adherence to ART because even smaller changes in adherence among vulnerable/ hard to reach populations can affect the probability of viral suppression. Barriers to adherence to ART among the vulnerable population of MSMs, sex workers and transgender can be manifold at individual, health systems and programmatic levels. Health systems should interface with each other to address the needs of vulnerable population especially in the context of ART adherence73. Studies to understand health seeking and adherence among mobile population, sex workers, MSMs and IVDUs in India are warranted.
ART adherence optimization
Adherence is patient enabled issue comprising many contextual factors such as culture, belief, personality, experience and health seeking behaviour. Sustained adherence requires a consistent supply of medications along with education and support74. In real life situations, adherence decreases after the intervention is terminated. Hence fundamental and applied research on innovations to improve the adherence of the patients for longer duration is needed to be conducted; findings of which can then be translated in programme settings. Less complex regimen and lower pill burden are obvious requirements for optimizing adherence. The regimen should also be determined on the basis of a number of considerations like potency of the drugs, pill burden, side effects, concomitant medicines and ability to keep future treatment options open. Fixed-dose combinations (FdCs) are preferred because they are easy to use, have distribution advantages (procurement and stock management) which result in improved adherence. Well designed systematic studies comparing the safety and efficacy of low cost once daily vs. twice daily ART regimens are needed to generate data on safety and efficacy in Indian setting. Drug developers should aim to devise long acting formulation to enhance adherence and improve both treatment and prevention outcomes.
Shortage of human resource is well documented in case of care and support programmes. A health professional's role needs to be limited to technical medical tasks especially patient care. This means reducing documentation by the physicians and counsellors. Community mobilization could be an adjunct strategy to meet HIV diagnosis, care and treatment needs in resource-limited settings including India75–77. Community support for patients on ART in the public sector represents a continuum that stretches from more formalized community health workers to informal activities, including voluntary support groups for people living with HIV/AIDS (PLHA) and local social capital. Successful treatment response was observed to be significantly higher among patients with an assigned community health worker, and participation in a support group also had a significant positive effect on the selected virological and immunological measures78,79. Government of India responded to the need of providing informal community support apart from structured ART centres and ICTCs by establishing Community Care Centres (CCC) to enable patients to access ART with systematic monitoring, follow up and counselling support for drug adherence80. Adherence to antiretroviral therapy has to be a shared responsibility between the programme and its beneficiaries i.e. making beneficiaries to take responsibility for their own health. Informal support such as social support plays a significant part in maintaining the psychological and physical integrity of the individual over time81. Social support gains even more importance in the context of longer life and ‘ageing with HIV’ that has immunologic features similar to those seen in elderly people without HIV disease82 and ageing would have implication for adherence to ART as along with adherence for other geriatric diseases. Social stability and social capital have both been known to be associated with medication adherence in various settings83,84. The identification of an encouraging confidante to share the burden of disease and the reality of it, and who could encourage acceptance and appropriate lifestyle changes to support better adherence and faith in antiretrovirals85,86. Therefore, while assessing patients’ preparedness for ART and potential coping strategies, it is important to include not only existing but also unforeseeable support avenues which can feasibly be activated in asking for support from other family members, other households, NGOs and the government.
It has been shown that unplanned treatment interruptions may be related to patients’ negative experience with the healthcare systems87,88. Most of the time, adherence counselling focuses on pill compliance and patients’ pill taking behaviour but in real life, patients actually drop out from the programme or become non-adherent in situations where they missed a visit because of a variety of social, cultural, psychological, economic and illness factors. This results in depletion of stock of ART. Guilt, fear of health care providers’ admonishment, laziness or indifference lead to deferring of impending visits resulting in multiple treatment interruptions. Such interruptions pose a greater risk of virological and clinical failure than do the same number of interspersed missed doses at low-to-moderate adherence88,89. Hence adequate efforts should be taken to develop an individual treatment plan that allows introduction of ART into the patient's lifestyle/ daily events. Right amount of assurances need to be given for a situation in which a patient may default. This can be done if there is good rapport between patient and provider. But reports of overburdened health care staff have been documented in various resource limited settings89. The issue of overburdened providers culminates into long waiting periods at the clinic which affects the willingness of the patient to come back again55. Eventually, patients lose faith in the existing system invariably due to operational issues and side effects which they are unable to comprehend. Dissatisfaction and loss of hope leads to switch to traditional/ other systems of medicines. This phenomenon is quite relevant in Indian context where Ayurvedic, Unani, Sidhha and Homeopathy (AYUSH) are recognized and licensed system of health practice90. In addition, traditional healers or community doctors also provide health care services in the country. The alternative medicine practitioners outnumber allopathic providers in India and serve as the primary source for delivering primary care for a majority of India's population91. While free ART roll-out continues to expand, it is also important to determine whether the knowledge, attitudes, and treatment practices of HIV-infected individuals and their health care providers are aligned with current treatment recommendations. Collaboration with health care providers of allopathic and traditional medicine systems is equally important. To address the issues of overburdened service providers in India, endeavours such as provision of ‘pre ARV’ services by the healers/ traditional medicine practitioners92,93 can be tested and replicated in programme setting. It can follow the approach of being used as adjunct rather than substitute for allopathic system. It needs to be recognized that traditional healers form an important segment in India and strengthening the gaps in knowledge among healers on STIs and HIV and addressing the existing misconceptions is warranted. Another thought being debated is that of task shifting. ‘Non-physicians’ could play a role in preventing and managing chronic diseases. A country with the third largest burden of AIDS in the world, India could start thinking about these kinds of task shifting. Communication training of health care providers, opportunities to spend quality time with patients and management of often neglected area of providers’ burn out should be part of ART programme scale up. Real life situations and practical solutions need to be built in communication training of the health care providers.
Addressing the patients’ own perception of side effect is crucial for adherence. Clinically a minor side effect can take a form of major barrier to adherence if it interferes with livelihood or affect family. For example, hallucinations caused by e0 favirenz may interfere with a person who is an automobile driver or who works in shift duties. Programme would obviously take care of change in regimen, however, there could be obvious clinical and resource limitations and this could only be addressed with patient and caregiver education. Motivation is another factor that should be utilized to empower patients to take care of their ‘own’ health despite smaller emergencies of side effects, adjustments at work and endeavour to adhere to ART. Individual-level interventions providing cognitive behavioural support94 and targeting practical medication management skills95 that have shown to improve adherence to ART should be tested to optimize adherence.
Optimizing retention
The definition of adherence has also been expanded to include retention in care which constitutes of regular follow up visits96. Retention emerges as a greater problem than individual non-adherence. Globally, it is estimated that almost 20 per cent of patients are not retained on antiretroviral therapy after 12 months56. Since the inception of large-scale ART access early in this decade, ART programmes in Africa have retained about 60 per cent of their patients at the end of 2 years. Loss to follow up is the major cause of attrition, followed by death74. Preliminary analysis of data obtained from our qualitative study conducted at three ART centres operating under national ART programme in Maharashtra state showed that retention in programme is a major challenge as compared to adherence97. Many studies have identified patient's characteristics, pre-ART health, and health literacy (educational level and knowledge about HIV/AIDS and ART) as predictors of ART outcome and sustainable retention in the programme98–101. Retention actually is a function of direct and indirect treatment costs. Most commonly reported obstacles to adequate health-seeking behaviour of the poor for obtaining prompt and adequate treatment is the indirect cost. Even if direct costs are affordable, or if medical services are free, indirect costs (for transport, special food and special investigations) limit access to treatment, or lead patients to interrupt therapies. To a great extent, visit to an ART centre depends on patients’/ family's capacity and possibility at a specific moment to mobilize resources, both in material and social or symbolic terms. So finally poverty emerges as the structural barrier to retention. A whole gamut of barriers like inhibiting clinic attendance, poor diet and inability to afford absence from work gets acknowledged as hindrance to treatment regimen102. Patients usually adjust by doing occasional work, making minors in the family work, borrowing money, theft and sales of ornaments/ assets. Temporary seasonal migration for generating more money is major cause of follow up failures. The Link ART Centres (LAC) in Indian programme specifically address the issue of access by providing services locally; however, fear of being identified limits the usage of this strategy. Promotion of LAC by education and involvement of local community at the centre is recommended for greater uptake of this facility.
There is a need to understand another component of ART programme which is ‘Pre-ART’. In India, the guidelines emphasize on preparing patients for initiating ART. ‘Pre-ART’ care is one of the neglected areas of ART roll-out programmes worldwide. Ninety per cent of the 1400 newly screened HIV positive persons between 2004 and 2007 were reported as ‘lost to follow up’ in Uganda103. A close attention needs to be paid to the retention of patients registered as ‘Pre ART’ for initiation of ART as soon as they become eligible. Linked to the issue of pre ART patient is the issue of preparing for ART initiation104. Although the national guidelines in India stipulate that adequate time should be spent on baseline evaluation of adherence but bringing the level of preparation for >95 per cent adherence is a labour intensive task. Prior to ART initiation, health care provider needs to have greater understanding of relationship between the phenomenon of readiness and subsequent HIV treatment adherence. Baseline investigation on the past adherence history for other ailments, attitude towards adherence, health seeking behaviour of patient, beliefs, social support and co-morbidities before ART initiation should be performed.
Suggested framework and intervention entry points
Overall areas of intervention to optimize ART adherence vary, however, utilization of health service by the beneficiaries and scale up of the ART programme aiming at optimal adherence and retention can spell out success for ART programme. Theoretically, coherent models for enhancing ART adherence in programme are needed. Taking cue from Anderson's Health Care Utilisation model105 a framework focusing for ART adherence at programmatic level in India is contemplated (Fig.). The principal objective of this framework is to identify problematic areas to intervene with specific health system strategies. The framework considers following elements: predisposing factors (patients’ own personality, behavior, etc.), enabling factors (social capital, patient provider relationship, community education, feeding research evidence into programme, sustained supply, retention, etc.) and need factors (belief, other disease, alternative medicine treatment options, community support). The proposed framework to enhance adherence to ART and sustain retention in the programme comprises three components: (i) Enabling factors: generating evidence through research and programme evaluation, (ii) Need factors: linkages and collaborations, and (iii) Predisposing factors: optimized health care service delivery alluding to patients’ need and behaviour.
Fig.
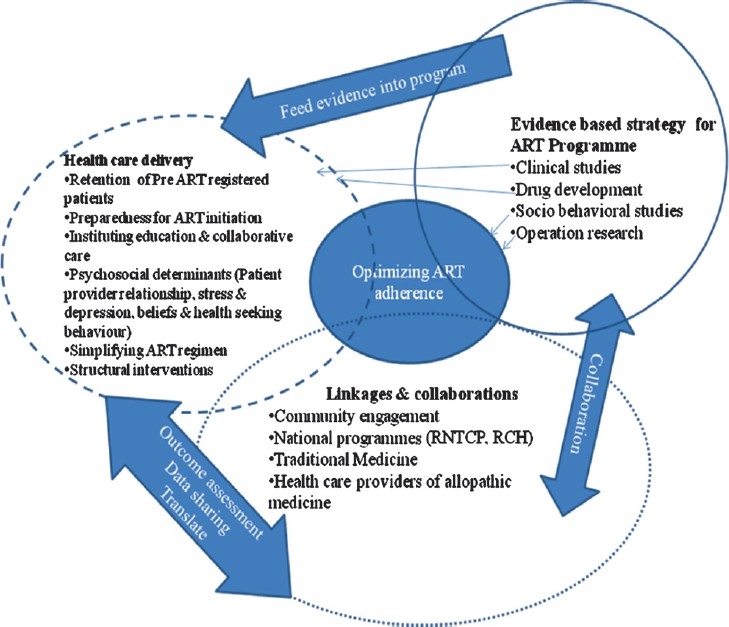
Ecosocial multilevel integrated approach of functioning for optimizing ART adherence.
Each of these components in this framework aims at influencing programme development and patient adherence to antiretroviral therapy or his/ her retention under ART programme umbrella. In addition, we have also conceptualized the linkages between health care system and social and research macro-system. This framework needs testing through which statistical data obtained using the framework would permit the evaluation of the relative weight of different factors in health behavior pertaining to ART, choice between different health resources, non-compliance with treatment, or delayed care seeking and use of research evidence.
At the individual level, enhanced counselling could be a dynamic tool to optimize adherence to ART. It is important not only to focus on pill taking behaviour of patient but it is equally critical to retain patients under the HIV treatment continuum beginning from the pre-ART registration. Various opportunities for counselling intervention are ARV initiation, preparing for initiation, patients stable on ART and finally ageing with ART. There are opportunities to intervene at all these four points of the continuum wherein patient enabling factors, attitude towards medication, programmatic level factors like switching and/ or transitioning to other systems of medicine, retention activities/ counselling at all 4 points would need to be addressed (Table II).
Table II.
Four points of continuum of care for HIV
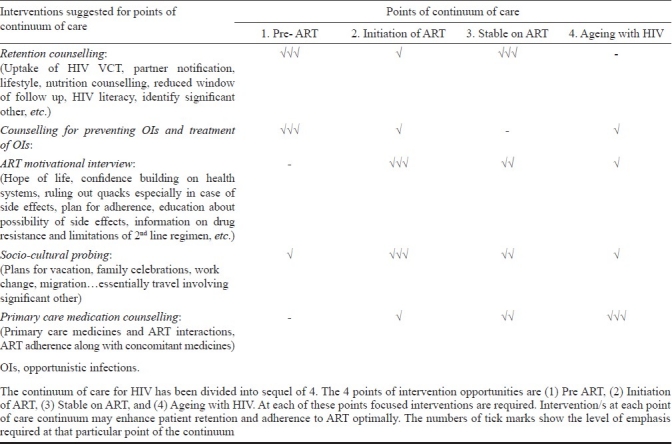
The four points of continuum can be identified as: (i) Pre ART: When a patient is registered for ART but is ART naïve, (ii) Initiation of ART: When a patient is prepared for ART initiation and initiates ART, (iii) Stable on ART: When a patient is on ART at least for 2 years and had no major episode of non adherence, and (iv) Ageing with HIV: Patients on ART over 50 years of age. Salient features of counselling intervention to optimize adherence at these defined 4 points of continuum of care are retention counselling, adherence counselling, counselling related to opportunistic infections, retention and adherence counselling within patients’ own socio-cultural context.
Conclusions
There is a need for ART roll-out programme-based focus of ART optimization especially when HIV/AIDS disease has transitioned into a chronic disease management point. Optimization of adherence to ART is a shared responsibility of the programme, patient, health care providers, families and community. Retention emerges as a challenge for ART adherence optimization.
Research focusing on behaviours, perceived norms and culture specific issues may provide insights into subjective barriers to ART adherence and develop empirically supported behavioural interventions to enhance adherence to ART. Empirically tested objective adherence measurement tools and approaches to assess adherence in clinical/ programme settings are required. Theory based interventions to optimize adherence need to be designed, tested and implemented. Overall, importance of community support and utilization of social capital in achieving durable treatment success are highlighted. Community consultations for implementation of ART programme would enable planners to include culture and situation specific needs for adherence. Strengthening of alternative medicine practitioner and their involvement in ART roll-out programme would be a useful strategy in India.
Acknowledgments
Authors acknowledge the support from the Indian Council of Medical Research, India, and thank Dr R.S. Paranjape, Director, NARI, Pune, for his guidance. Authors also acknowledge the guidance received from Dr S.M. Mehendale, Director, NIE, Chennai, and suggestions on the framework of the manuscript, Smt. Neelam Joglekar for her help in the drafting this paper.
References
- 1.Cimons M. “U.S. Approves Sale of AZT to AIDS Patients”. Los Angeles Times. 1987. Mar 21, [accessed on January 2, 2012]. Available from: http://articles.latimes.com/1987-03-21/news/mn-4526_1_otheraids-patients .
- 2.Geneva: World Health Organization; 2003. [accessed on July 18, 2011]. WHO/UNAIDS. Treating 3 million by 2005: making it happen: the WHO Strategy. Available from: http://data.unaids.org/Publications/External-Documents/who_3 by 5-strategy_en.pdf . [Google Scholar]
- 3.Bachani D, Rewari BB. Antiretroviral therapy: Practice guidelines and National ART Programme. J Indian Med Assoc. 2009;107:310–4. [PubMed] [Google Scholar]
- 4.Department of AIDS Control. ‘NACO Annual report 2009-10’. 2010. Mar, [accessed on August 29, 2011]. Available from: http://www.nacoonline.org/Quick_Links/Directory_of_HIV_Data/
- 5.MMWR Report. HIV Surveillance - United States, 1981-2008. [accessed on August 29, 2011];2011 Jun 3;60:689–93. Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6021a2.htm . [PubMed] [Google Scholar]
- 6.Strong K, Mathers C, Leeder S, Beaglehole R. Preventing chronic diseases: how many lives can we save? Lancet. 2005;366:1578–82. doi: 10.1016/S0140-6736(05)67341-2. [DOI] [PubMed] [Google Scholar]
- 7.Multicohort study. Antiretroviral Therapy Cohort Collaboration. Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies. Lancet. 2008;372:293–9. doi: 10.1016/S0140-6736(08)61113-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.NACO. Draft Guidelines for national roll-out of second line ART. National Guidelines on second line ART for adults and adolescents. NACO Ministry of Health and Family Welfare, Government of India. 2008. Nov, [accessed on January 3, 2012]. Available from: http://www.nacoonline.org/
- 9.Beaglehole R, Jordan JE, Patel V, Chopra M, Ebrahim S, Kidd M, et al. Improving the prevention and management of chronic disease in low-income and middle-income countries: a priority for primary health care. Lancet. 2008;372:940–9. doi: 10.1016/S0140-6736(08)61404-X. [DOI] [PubMed] [Google Scholar]
- 10.Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squire C, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133:21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- 11.Schonnesson LN, Diamond PM, Ross MW, Williams M, Bratt G. Baseline predictor's of three types of antiretroviral therapy (ART) adherence: A two year follow up. AIDS Care. 2006;18:406–14. doi: 10.1080/09540120500456631a. [DOI] [PubMed] [Google Scholar]
- 12.Antiretroviral Therapy Guidelines for HIV-Infected Adults and Adolescents Including Post-exposure Prophylaxis. 2007. May, [accessed on September 30, 2011]. Available from: http://www.nacoonline.org/
- 13.Gao X, Nau DP. Congruence of three self-report measures of medication adherence among HIV patients. Ann Pharmacother. 2000;34:1117–22. doi: 10.1345/aph.19339. [DOI] [PubMed] [Google Scholar]
- 14.Nieuwkerk PT, Oort JF. Self-reported adherence to anti-retroviral therapy for HIV-1 infection and virological treatment response. J Acquir Immun Defic Syndr. 2005;38:445–8. doi: 10.1097/01.qai.0000147522.34369.12. [DOI] [PubMed] [Google Scholar]
- 15.Brown L, Macintyre K, Trujillo L. Interventions to reduce HIV/AIDS stigma: What have we learned. AIDS Education Prevention. 2003;15:49–69. doi: 10.1521/aeap.15.1.49.23844. [DOI] [PubMed] [Google Scholar]
- 16.Walshe L, Saple DG, Mehta SH, Shah B, Bollinger RC, Gupta A. Physician estimate of antiretroviral adherence in India: poor correlation with patient self-report and viral load. AIDS Patient Care STDs. 2010;24:189–95. doi: 10.1089/apc.2009.0208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wagner GJ. Predictors of antiretroviral adherence as measured by self-report, electronic monitoring, and medication diaries. AIDS Patient Care STDs. 2002;16:599–608. doi: 10.1089/108729102761882134. [DOI] [PubMed] [Google Scholar]
- 18.Martin S, Elliott-DeSorbo DK, Calabrese S, Wolters PL, Roby G, Brennan T, et al. A comparison of adherence assessment methods utilized in the United States: perspectives of researchers, HIV-infected children, and their caregivers. AIDS Patient Care STDs. 2009;23:593–60. doi: 10.1089/apc.2009.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bisson GP, Gross R, Bellamy S, Chittams J, Hislop M, Regensberg L, et al. Pharmacy refill adherence compared with CD4 count changes for monitoring HIV-infected adults on antiretroviral therapy. PLoS Med. 2008;5:e109. doi: 10.1371/journal.pmed.0050109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bangsberg DR, Hecht FM, Clague H, Charlebois ED, Ciccarone D, Chesney M, et al. Provider assessment of adherence to HIV antiretroviral therapy. J Acquir Immune Defic Syndr. 2001;26:435–42. doi: 10.1097/00126334-200104150-00005. [DOI] [PubMed] [Google Scholar]
- 21.Murri R, Antinori A, Ammassari A, Nappa S, Orofino G, Abrescia N, et al. AdICoNA Study Group. Physician estimates of adherence and the patient-physician relationship as a setting to improve adherence to antiretroviral therapy. J Acquir Immune Defic Syndr. 2002;31(Suppl 3):S158–62. doi: 10.1097/00126334-200212153-00015. [DOI] [PubMed] [Google Scholar]
- 22.Wise J, Operario D. Use of electronic reminder devices to improve adherence to antiretroviral therapy: a systematic review. AIDS Patient Care STDs. 2008;22:495–504. doi: 10.1089/apc.2007.0180. [DOI] [PubMed] [Google Scholar]
- 23.Mills EJ, Nachega JB, Buchan I, Orbinski J, Attaran A, Singh S, et al. Adherence to antiretroviral therapy in sub-Saharan Africa and North America: A meta-analysis. JAMA. 2006;296:679–90. doi: 10.1001/jama.296.6.679. [DOI] [PubMed] [Google Scholar]
- 24.Nyamathi AM, Sinha S, Ganguly KK, William RR, Heravian A, Ramakrishnan P, et al. Challenges experienced by rural women in India living with AIDS and implications for the delivery of HIV/AIDS care. Health Care Women Int. 2011;32:300–13. doi: 10.1080/07399332.2010.536282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Batavia AS, Balaji K, Houle E, Parisaboina S, Ganesh AK, Mayer KH, et al. Adherence to antiretroviral therapy in patients participating in a graduated cost recovery program at an HIV care center in South India. AIDS Behav. 2010;14:794–8. doi: 10.1007/s10461-009-9663-6. [DOI] [PubMed] [Google Scholar]
- 26.Lal V, Kant S, Dewan R, Rai SK, Biswas A. A two-site hospital-based study on factors associated with nonadherence to highly active antiretroviral therapy. Indian J Public Health. 2010;54:179–83. doi: 10.4103/0019-557X.77256. [DOI] [PubMed] [Google Scholar]
- 27.Venkatesh KK, Srikrishnan AK, Mayer KH, Kumarasamy N, Raminani S, Thamburaj E, et al. Predictors of nonadherence to highly active antiretroviral therapy among HIV-infected South Indians in clinical care: implications for developing adherence interventions in resource-limited settings. AIDS Patient Care STDs. 2010;24:795–803. doi: 10.1089/apc.2010.0153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sivadasan A, Abraham OC, Rupali P, Pulimood SA, Rajan J, Rajkumar S, et al. High rates of regimen change due to drug toxicity among a cohort of South Indian adults with HIV infection initiated on generic, first-line antiretroviral treatment. J Assoc Physicians India. 2009;57:384–8. [PubMed] [Google Scholar]
- 29.Cauldbeck MB, O’Connor C, O’Connor MB, Saunders JA, Rao B, Mallesh VG, et al. Adherence to anti-retroviral therapy among HIV patients in Bangalore, India. AIDS Res Ther. 2009;28:6–7. doi: 10.1186/1742-6405-6-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sarna A, Pujari S, Sengar AK, Garg R, Gupta I, Dam J. Adherence to antiretroviral therapy & its determinants amongst HIV patients in India. Indian J Med Res. 2008;127:28–36. [PubMed] [Google Scholar]
- 31.Wanchu A, Kaur R, Bambery P, Singh S. Adherence to generic reverse transcriptase inhibitor-based antiretroviral medication at a Tertiary Center in North India. AIDS Behav. 2007;11:99–102. doi: 10.1007/s10461-006-9101-y. [DOI] [PubMed] [Google Scholar]
- 32.Sharma M, Singh RR, Laishram P, Kumar B, Nanao H, Sharma C, et al. Access, adherence, quality and impact of ARV provision to current and ex-injecting drug users in Manipur (India): an initial assessment. Int J Drug Policy. 2007;18:319–25. doi: 10.1016/j.drugpo.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 33.Kumarasamy N, Safren SA, Raminani SR, Pickard R, James R, Krishnan AK, et al. Barriers and facilitators to antiretroviral medication adherence among patients with HIV in Chennai, India: a qualitative study. AIDS Patient Care STDs. 2005;19:526–37. doi: 10.1089/apc.2005.19.526. [DOI] [PubMed] [Google Scholar]
- 34.Safren SA, Kumarasamy N, James R, Raminani S, Solomon S, Mayer KH. ART adherence, demographic variables and CD4 outcome among HIV-positive patients on antiretroviral therapy in Chennai, India. AIDS Care. 2005;17:853–62. doi: 10.1080/09540120500038439. [DOI] [PubMed] [Google Scholar]
- 35.Saple DG, Vaidya SB, Vadrevu R, Pandey VP, Ramnani JP. Difficulties encountered with the use of antiretroviral drugs in India. J HIV Ther. 2002;7:56–8. [PubMed] [Google Scholar]
- 36.Bachani D, Garg R, Rewari BB, Hegg L, Rajasekaran S, Deshpande A, et al. Two-year treatment outcomes of patients enrolled in India's national first-line antiretroviral therapy programme. Natl Med J India. 2010;23:7–12. [PubMed] [Google Scholar]
- 37.Sogarwal R, Bachani D. Assessment of ART centres in India: client perspectives. J Indian Med Assoc. 2009;107:276–80. [PubMed] [Google Scholar]
- 38.Safren SA, Kumarasamy N, Hosseinipour M, Harwood MM, Hoffman I, McCauley M, et al. Perceptions about the acceptability of assessments of HIV medication adherence in Lilongwe, Malawi and Chennai, India. AIDS Behav. 2006;10:443–50. doi: 10.1007/s10461-006-9094-6. [DOI] [PubMed] [Google Scholar]
- 39.Ekstrand ML, Shet A, Chandy S, Singh G, Shamsundar R, Madhavan V, et al. Suboptimal adherence associated with virological failure and resistance mutations to first-line highly active antiretroviral therapy (HAART) in Bangalore, India. Int Health. 2011;3:27–34. doi: 10.1016/j.inhe.2010.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shah B, Walshe L, Saple DG, Mehta SH, Ramnani JP, Kharkar RD, et al. Adherence to antiretroviral therapy and virologic suppression among HIV-infected persons receiving care in private clinics in Mumbai, India. Clin Infect Dis. 2007;44:1235–44. doi: 10.1086/513429. [DOI] [PubMed] [Google Scholar]
- 41.Ekstrand ML, Chandy S, Heylen E, Steward W, Singh G. Developing useful highly active antiretroviral therapy adherence measures for India: the Prerana study. J Acquir Immune Defic Syndr. 2010;53:415–6. doi: 10.1097/QAI.0b013e3181ba3e4e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vitolins MZ, Rand CS, Rapp SR, Ribisi PM, Sevick MA. Measuring adherence to behavioral and medical interventions. Control Clin Trials. 2000;21(Suppl 5):188S–94S. doi: 10.1016/s0197-2456(00)00077-5. [DOI] [PubMed] [Google Scholar]
- 43.Kouanfack C, Laurent C, Peytavin G, Ciaffi L, Ngolle M, Mawamba Y, et al. Adherence to antiretroviral therapy assessed by drug level monitoring and self-report in Cameroon. J Acquir Immune Defic Syndr. 2008;48:216–9. doi: 10.1097/QAI.0b013e3181743955. [DOI] [PubMed] [Google Scholar]
- 44.Obioma N, Valerie N, Ehlers J. Adult patients ‘adherence to anti-retroviral treatment: A survey correlating pharmacy refill records and pill counts with immunological and virological indices. Int J Nurs Stud. 2011;48:1323–9. doi: 10.1016/j.ijnurstu.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 45.Di Matteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42:200–9. doi: 10.1097/01.mlr.0000114908.90348.f9. [DOI] [PubMed] [Google Scholar]
- 46.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–97. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 47.Mills EJ, Nachega JB, Bangsberg DR, Singh S, Rachlis B, Wu P, et al. Adherence to HAART: a systematic review of developed and developing nation patient-reported barriers and facilitators. PLoS Med. 2006;3(11):e438. doi: 10.1371/journal.pmed.0030438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chesney M. Adherence to HAART regimens. AIDS Patient Care STDs. 2003;17:169–77. doi: 10.1089/108729103321619773. [DOI] [PubMed] [Google Scholar]
- 49.Kagee A. Adherence to antiretroviral therapy in the context of the national roll-out in South Africa: defining a research agenda for South African Psychology. South Afr J Psychol. 2008;38:413–28. [Google Scholar]
- 50.Ncaca LN, Kranzer K, Orrell C. Treatment interruption and variation in tablet taking behaviour result in viral failure: a case-control study from cape town, South Africa. PLoS One. 2011;6:e23088. doi: 10.1371/journal.pone.0023088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Skovdal M, Campbell C, Nyamukapa C, Gregson S. When masculinity interferes with women's treatment of HIV infection: a qualitative study about adherence to antiretroviral therapy in Zimbabwe. J Int AIDS Soc. 2011 Jun 9;14:29. doi: 10.1186/1758-2652-14-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Weidle N, Wamai P, Solberg C, Liechty S, Sendagala W, et al. Adherence to antiretroviral therapy in a home-based AIDS care programme in rural Uganda. Lancet. 2006;368:1587–94. doi: 10.1016/S0140-6736(06)69118-6. [DOI] [PubMed] [Google Scholar]
- 53.Diabate S, Alary M, Koffi CK. Determinants of adherence to highly active antiretroviral therapy among HIV-1-infected patients in Côte d’Ivoire. AIDS. 2007;21:1799–803. doi: 10.1097/QAD.0b013e3282a5667b. [DOI] [PubMed] [Google Scholar]
- 54.Srikantiah P, Ghidinelli M, Bachani D, Chasombat S, Daoni E, Mustikawati DE, et al. Scale-up of national antiretroviral therapy programs: progress and challenges in the Asia Pacific region. AIDS. 2010;24(Suppl 3):S62–71. doi: 10.1097/01.aids.0000390091.45435.ea. [DOI] [PubMed] [Google Scholar]
- 55.Dahab M, Charalambous S, Hamilton R, Fielding K, Kielmann K, Churchyard GJ, et al. That is why I stopped the ART": Patients’ & providers’ perspectives on barriers to and enablers of HIV treatment adherence in a South African workplace programme. BMC Public Health. 2008;8:63. doi: 10.1186/1471-2458-8-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.WHO/UNAIDS/UNICEF. Towards universal access: Scaling up priority HIV/AIDS Interventions in Health Sector. Progress report. 2010. [accessed on September 30, 2011]. Available from: http://www.who.int/hiv/pub/2010progressreport/report/en/index.html .
- 57.O’Brien ME, Clark RA, Besch CL, Myers L, Kissinger P. Patterns and correlates of discontinuation of the initial HAART regimen in an urban outpatient cohort. J Acquir Immune Defic Syndr. 2003;34:407–14. doi: 10.1097/00126334-200312010-00008. [DOI] [PubMed] [Google Scholar]
- 58.Johnson M O, Gamarel KE, Dawson-Rose C. Changing HIV treatment expectancies: A pilot study. AIDS Care. 2006;18:550–3. doi: 10.1080/09540120500241439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rhodes SD, Hergenrather KC, Wilkin AM, Wololdredge R. Adherence and HIV. In: Ockene JK, Shumaker SA, Riekert K, editors. The handbook of health behavior change. 3rd ed. New York: Springer; 2008. pp. 659–75. [Google Scholar]
- 60.Hardon AP, Akurut D, Comoro C, Ekezie C, Irunde HF, Gerrits T, et al. Hunger, waiting time and transport costs: time to confront challenges to ART adherence in Africa. AIDS Care. 2007;19:658–65. doi: 10.1080/09540120701244943. [DOI] [PubMed] [Google Scholar]
- 61.Drimie S, Mullins D, Gillespie S, editors. Mainstreaming HIV and AIDS into livelihood and food security programs: The experience of CARE Malawi. 2006. [accessed on January 3, 2012]. pp. 283–303. Available from: http://citeseerx.ist.psu.edu/viewdoc/summary?doi=10.1.1.139.5417 .
- 62.Masanjala W. The poverty-HIV/AIDS nexus in Africa: a livelihood approach. Soc Sci Med. 2007;64:1032–41. doi: 10.1016/j.socscimed.2006.10.009. [DOI] [PubMed] [Google Scholar]
- 63.Rachlis BS, Mills EJ, Cole DC. Livelihood security and adherence to antiretroviral therapy in low and middle income settings: A systematic review. PLoS One. 2011;6:e18948. doi: 10.1371/journal.pone.0018948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Uzochukwu BSC, Onwujekwe OE, Onoka AC, Okoli C, Uguru NP, Chukwuo O. Determinants of non-adherence to subsidized anti-retroviral treatment in southeast Nigeria. Health Policy Plan. 2009;24:189–96. doi: 10.1093/heapol/czp006. [DOI] [PubMed] [Google Scholar]
- 65.Sahay S, Phadke M, Brahme R, Paralikar V, Joshi V, Sane S, et al. Correlates of anxiety and depression among HIV test-seekers at a Voluntary Counseling and Testing facility in Pune, India. Qual Life Res. 2007;16:41–52. doi: 10.1007/s11136-006-9112-1. [DOI] [PubMed] [Google Scholar]
- 66.Lora S, Desilva MB, Hamer D, Keyi X, Yue Y, Wen F, et al. Barriers to adherence to antiretroviral medications among patients living with HIV in southern China: a qualitative study. AIDS Care. 2008;20:1242–50. doi: 10.1080/09540120801918651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Amon JJ. Dangerous medicines: Unproven AIDS cures and counterfeit antiretroviral drugs. Globalization Health. 2008;4:5. doi: 10.1186/1744-8603-4-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Akileswaran C, Macalino GE, Bhakta N, Mayer K, Kumarasamy N, Solomon S. International Conference on AIDS. Bangkok, Thailand: 2004. Jul 11-16, Sources of information about traditional therapies to treat HIV Seropositive patients in Chennai, India. Abstract ThPeB7246. [Google Scholar]
- 69.Ahmad K. Antiretroviral therapy abandoned for herbal remedies. Lancet Infect Dis. 2007;7:313. doi: 10.1016/s1473-3099(07)70100-7. [DOI] [PubMed] [Google Scholar]
- 70.Owen-Smith A, Diclemente R, Wingood G. Complementary and alternative medicine use decreases adherence to HAART in HIV-positive women. AIDS Care. 2007;19:589–93. doi: 10.1080/09540120701203279. [DOI] [PubMed] [Google Scholar]
- 71.Ramchandani SR, Mehta SH, Saple DG, Vaidya SB, Pandey VP, Vadrevu R, et al. Knowledge, attitudes, and practices of antiretroviral therapy among HIV-infected adults attending private and public clinics in India. AIDS Patient Care STDs. 2007;21:129–42. doi: 10.1089/apc.2006.0045. [DOI] [PubMed] [Google Scholar]
- 72.Belz Chomat AM, Wilson IB, Wanke CA, Selvakumar A, John KR, Isaac R. Knowledge, beliefs, and health care practices relating to treatment of HIV in Vellore, India. AIDS Patient Care STDs. 2009;23:477–84. doi: 10.1089/apc.2008.0222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chakrapani V, Shanmugam M, Michael S, Dubrow R. Barriers to free antiretroviral treatment access for female sex workers in Chennai, India. Indian Network for People living with HIV and AIDS (INP+), India. AIDS Patient Care STDs. 2009;23:973–80. doi: 10.1089/apc.2009.0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rosen S, Fox MP, Gill CJ. Patient retention in antiretroviral therapy programs in Sub-Saharan Africa: A systematic review. PLoS Med. 2007;4(10):e298. doi: 10.1371/journal.pmed.0040298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Standing H, Mushtaque A, Chowdhury R. Producing effective knowledge agents in a pluralistic environment: what future for community health workers? Soc Sci Med. 2008;66:2096–107. doi: 10.1016/j.socscimed.2008.01.046. [DOI] [PubMed] [Google Scholar]
- 76.Sahay S, Ghate M, Mehendale SM. Managing HIV therapy literacy in resource limited settings. HIV Ther. 2009;3:339–44. [Google Scholar]
- 77.Sahay S, Mehendale SM. Engaging community to support HIV prevention research. Eastern J Med. 2011;16:168–77. [PMC free article] [PubMed] [Google Scholar]
- 78.Wouters E, Van Damme W, van Rensburg D, Meulemans H. Impact of baseline health and community support on antiretroviral treatment outcomes in HIV patients in South Africa. AIDS. 2008;22:2545–8. doi: 10.1097/QAD.0b013e32831c5562. [DOI] [PubMed] [Google Scholar]
- 79.Wouter E, Van Damme W, Van Loon F, Van Rensburg D, Meulemans H. Public-sector ART in the Free State Province, South Africa: community support as an important determinant of outcome. Soc Sci Med. 2009;69:1177–85. doi: 10.1016/j.socscimed.2009.07.034. [DOI] [PubMed] [Google Scholar]
- 80.NACP III Goals and objectives. [accessed on June 8, 2010]. Available from: http://www.nacoonline.org/National_AIDS_Control_Program/
- 81.Caplan G. Support systems and community mental health: Lectures on concept development. New York: Behavioral Publications; 1974. [Google Scholar]
- 82.Appay V, Rowland-Jones SL. Premature ageing of the immune system: the cause of AIDS? Trends Immunol. 2002;23:580–5. doi: 10.1016/s1471-4906(02)02338-4. [DOI] [PubMed] [Google Scholar]
- 83.Ware NC, Idoko J, Kaaya S, Biararo IA, Wyatt MA, Agbaji O, et al. Explaining adherence successes in sub-Saharan Africa: an ethnographic study. PLoS Med. 2009;6(1):e1000011. doi: 10.1371/journal.pmed.1000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Watt MH, Maman S, Earp JA, Eng E, Setel PW, Golin CE, et al. “It's all the time in my mind”: Facilitators of adherence to antiretroviral therapy in a Tanzanian setting. Soc Sci Med. 2009;68:1793–800. doi: 10.1016/j.socscimed.2009.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Nama SL, Katherine F, Ava A, Diana D, Tendani GP, Wenzel G. The relationship of acceptance or denial of HIV-status to antiretroviral adherence among adult HIV patients in urban Botswana. Soc Sci Med. 2008;67:301–10. doi: 10.1016/j.socscimed.2008.03.042. [DOI] [PubMed] [Google Scholar]
- 86.Marcellin F, Boyer S, Protopopescu C, Dia A, Ongolo-Zogo P, Koulla-Shiro S, et al. Determinants of unplanned antiretroviral treatment interruptions among people living with HIV in Yaounde, Cameroon (EVAL survey, ANRS 12- 116) Trop Med Int Health. 2008;13:1470–8. doi: 10.1111/j.1365-3156.2008.02170.x. [DOI] [PubMed] [Google Scholar]
- 87.Oyugi JH, Byakika-Tusiime J, Charlebois ED, Kityo C, Mugerwa R, Mugyenyi P, et al. Multiple validated measures of adherence indicate high levels of adherence to generic HIV antiretroviral therapy in a resource-limited setting. J Acquir Immune Defic Syndr. 2004;36:1100–2. doi: 10.1097/00126334-200408150-00014. [DOI] [PubMed] [Google Scholar]
- 88.Parienti JJ, Das-Douglas M, Massari V, Guzman D, Deeks SG, Verdon R, et al. Not all missed doses are the same: sustained NNRTI treatment interruptions predict HIV rebound at low-to-moderate adherencelevels. PLoS One. 2008;3(7):e2783. doi: 10.1371/journal.pone.0002783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Barnighausen T, Bloom DE, Humair S. Human resources for treating HIV/AIDS: needs, capacities, and gaps. AIDS Patient Care STDs. 2007;21:799–812. doi: 10.1089/apc.2007.0193. [DOI] [PubMed] [Google Scholar]
- 90.New Delhi: Ministry of Health and Family Welfare, India; 2011. [accessed on September 6, 2011]. Department of Ayurveda, Yoga, Unani, Siddha and Homoeopathy. Available from: http://indianmedicine.nic.in/ [Google Scholar]
- 91.Fritts M, Crawford CC, Quibell D, Gupta A, Jonas W, Coulter I, et al. Traditional Indian medicine and homeopathy for HIV/AIDS: a review of literature. AIDS Res Therapy. 2008;5:25. doi: 10.1186/1742-6405-5-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Burnett A, Baggaley R, Ndovi-MacMillan M, Sulwe J, Hang’omba B, Ben Nett J. Caring for people with HIV in Zambia: are traditional healers and formal health workers willing to work together? AIDS Care. 1999;11:481–91. doi: 10.1080/09540129947875. [DOI] [PubMed] [Google Scholar]
- 93.Kaboru BB, Ndubani P, Falkenberg T, Pharris A, Muchimba M, Solo K, et al. A dialogue-building pilot intervention involving traditional and biomedical health providers focusing on STIs and HIV/AIDS care in Zambia. J EBCAN. 2008;13:110–26. [Google Scholar]
- 94.Weber RCL, Christen S, Tschopp S, Znoj H, Schneider C, Schmitt J, et al. Effect of individual cognitive behaviour intervention on adherence to antiretroviral therapy: prospective randomized trial. Antivir Ther. 2004;9:85–95. [PubMed] [Google Scholar]
- 95.Rueda S P-WL, Bayoumi A, Tynan AM, Antoniou T, Rourke S, Glazier R. Patient support and education for promoting adherence to highly active antiretroviral therapy for HIV/AIDS. Cochrane Database Syst Rev. 2006;3 doi: 10.1002/14651858.CD001442.pub2. Art. No. CD001442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Patel A, Hirschhorn L, Fullem A, Ojikutu B, Oser R. Adult aherence to treatment and retention in care. Arlington, VA: USAID | AIDSTAR-ONE PROJECT, Task Order 1; [Google Scholar]
- 97.Joglekar N, Paranjape R, Jain R, Rahane G, Potdar R, Reddy KS, et al. Barriers to ART adherence and follow-ups among patients attending ART centers in Maharashtra, India: A qualitative study. Indian J Med Res. 2011 doi: 10.4103/0971-5916.92642. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Weiss L, French T, Finkelstein R, Waters M, Mukherjee R, Agins B. HIV-related knowledge and adherence to HAART. AIDS Care. 2003;15:673–9. doi: 10.1080/09540120310001595159. [DOI] [PubMed] [Google Scholar]
- 99.Kalichman SC, Benotsch E, Suarez T, Catz S, Miller J, Rompa D. Health literacy and health-related knowledge among persons living with HIV/ AIDS. Am J Prevent Med. 2008;18:325–31. doi: 10.1016/s0749-3797(00)00121-5. [DOI] [PubMed] [Google Scholar]
- 100.van Leth FP, Phanuphak K, Ruxrungtham E, Baraldi S, Miller B, Gazzard P, et al. Comparison of first-line antiretroviral therapy with regimens including nevirapine, efavirenz, or both drugs, plus stavudine and lamivudine: a randomised open-label trial, the 2NN Study. Lancet. 2004;363:1253–63. doi: 10.1016/S0140-6736(04)15997-7. [DOI] [PubMed] [Google Scholar]
- 101.Atkinson MJ, Petrozzino JJ. An evidence-based review of treatment related determinants of patients’ non adherence to HIV medications. AIDS Patient Care STDs. 2009;23:903–14. doi: 10.1089/apc.2009.0024. [DOI] [PubMed] [Google Scholar]
- 102.Simoni JM, Frick PA, Lockhart D, Liebovitz D. Mediators of social support and antiretroviral adherence among an indigent population in New York City. AIDS Patient Care STDs. 2002;16:431–9. doi: 10.1089/108729102760330272. [DOI] [PubMed] [Google Scholar]
- 103.Lubegaa M, Nsabagasanib X, Nazarius M, Tumwesigyee NM, Wabwire-Mangene F, Ekströmd AM, et al. Policy and practice, lost in transition: Reasons for high drop-out from pre-antiretroviral care in a resource-poor setting of eastern Uganda. Health Policy. 2010;95:153–8. doi: 10.1016/j.healthpol.2009.11.021. [DOI] [PubMed] [Google Scholar]
- 104.Enriquez M, Nancy R, Lackey RN, Mary C, O’Connor MD, David S, et al. Successful adherence after multiple HIV treatment failures. J Adv Nurs. 2004;45:438–46. doi: 10.1046/j.1365-2648.2003.02928.x. [DOI] [PubMed] [Google Scholar]
- 105.Andersen R, Neuman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Memorial Fund. Q Health Soc. 1975;51:95–124. [PubMed] [Google Scholar]


