Abstract
Over the past 30 years, several interventions have been identified to prevent HIV transmission from HIV-infected persons to uninfected persons in discordant relationships. Yet, transmissions continue to occur. Interventions such as voluntary counselling and testing, condom promotion and risk reduction counselling are very effective in preventing transmission among serodiscordant couples but are underutilized in India despite their widespread availability. New interventions such as pre-risk exposure prophylaxis and universal antiretroviral therapy (irrespective of CD4 count) have been newly identified but face several challenges that impede their widespread implementation in India. Discordant couples in India also face certain unique socio-cultural issues such as marital and fertility pressure. We briefly review the various interventions (existing and novel) available for persons in discordant relationships in India and socio-cultural issues faced by these individuals and make recommendations to maximize their implementation.
Keywords: ART, CD4 counts, HIV- pre-risk exposure prophylaxis, risk reduction counselling, serodiscordant couples
Introduction
The year 2011 marks 30 years since the first report of AIDS appeared in 1981 among men who have sex with men (MSM) in Los Angeles, USA1 and 25 years since the first cases of HIV infection were detected among female sex workers (FSW) in Chennai, India2. Over the past three decades dramatic progress has been made in the battle against HIV in the prevention and treatment arenas both in India and globally. Despite all this progress, new infections continue to occur - in 2009, there were an estimated 2.6 million persons newly infected with HIV globally3. Nearly all new infections (with the exceptions of mother-to-child transmissions and blood product-related transmissions) occur within the context of a discordant relationship - someone infected with HIV is passing on the infection to someone uninfected with HIV through unprotected sex, sharing needles, etc. The purpose of this review article is to discuss the various established and novel tools available to prevent transmission among individuals in discordant relationships and challenges faced in the implementation of these tools.
Serodiscordant relationships
The term “sero discordant couple” or “serodiscordant relationship” conjures up the image of a monogamous heterosexual couple where one partner is HIV-infected and the other partner is HIV-uninfected. This may at least in part be due to the definition that is commonly used in clinical trials focused on serodiscordant couples such as the HIV Prevention Trials Network 052 Protocol4 or the Partners in pre-exposure prophylaxis (PrEP) study5 where almost all discordant couples were in monogamous heterosexual relationships. In clinical trials, investigators can control the environment and their study population - however, this is not usually possible in the real world. Therefore, we discuss here all types of serodiscordant relationships that place an HIV-uninfected person at risk for HIV acquisition from an HIV-infected partner.
Classification of HIV serodiscordant relationships
Among men who are HIV-infected, there are four types of serodiscordant relationships that could occur namely homosexual, heterosexual, bisexual or needle sharing. Hence, men have been classified based on these acts into the four groups (Table I). Both homosexual and heterosexual men have the ability to be either in a monogamous relationship wherein their primary sexual partner is the only individual at risk or they could have multiple sexual partners (e.g., male sex workers) either concurrently or serially that need to be targeted for HIV prevention. HIV-infected men in bisexual relationships always place at least two or more individuals at risk for HIV acquisition. In the case of a HIV-infected injection drug user (IDU), there are several opportunities for transmission both to sexual partners as well as injection partners. There are several reports that suggest high rates of marriage among IDUs with evidence of HIV transmission from the IDU to their spouses both sexually and via needle sharing6–9. In situations where IDUs are in a monogamous relationship and tend to inject drugs by themselves, the only individual at risk is their primary sexual partner. Similarly, HIV-infected IDUs who are not sexually active and have only one injection partner, places only this one individual at risk for HIV acquisition. However, in the majority of cases IDUs have both sexual (one or multiple, male and/or female) and injection partners (one or multiple) to whom they could potentially transmit HIV infection, all of whom need to be targeted by HIV prevention programmes.
Table I.
Individuals at-risk in serodiscordant relationships
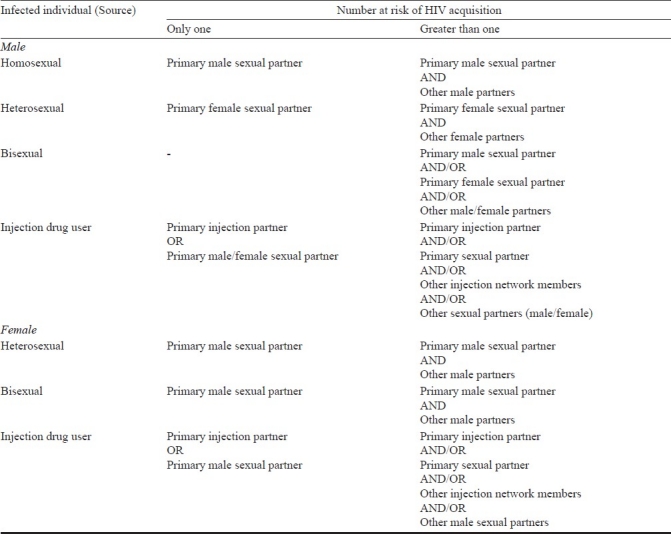
HIV-infected women are only at risk of sexually transmitting HIV only to their male sexual partners via vaginal or anal intercourse. There is no evidence of sexual transmission of HIV from a HIV-infected woman to an uninfected woman. However, HIV-infected female IDUs can transmit HIV infection to other uninfected female members in their network (Table I). While the majority of the IDUs in India are male, there are a significant number of female IDUs especially in the North Eastern states (e.g., Manipur)10. If these women are sexually active, they pose the additional risk of transmission to their uninfected male sexual partners besides their injection network partners (both male and female).
Hijras - the third gender recognized by the Indian government – is the Indian term to identify members of the transgendered community. In the majority of cases, these individuals undergo male to female transformation. Consequently, most hijras self-identify as women and a majority of them indulge in transactional sex with multiple male partners while some have primary male partners11. HIV-infected hijras present the risk of HIV transmission primarily to men - the number of men depends on whether they are in a monogamous or polygamous relationship.
To truly eradicate the HIV epidemic in India, the first step is to acknowledge that the various types of serodiscordant relationships do occur in India more commonly than we would presume. Next, interventions need to be implemented to minimize transmission among all types of discordant relationships especially among the marginalized populations such as MSM, IDUs and hijras.
Interventions for persons in serodiscordant relationships in India
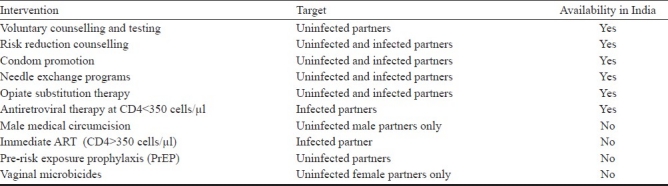
Interventions targeting individuals in serodicordant relationships can be broadly classified as interventions targeting the uninfected partner that minimizes risk of acquisition (e.g., PrEP) or interventions targeted towards the infected partner to minimize risk of transmission (e.g., antiretroviral therapy) or interventions that can be targeted at both partners (e.g., condom promotion) (Table II).
Table II.
Interventions to minimize transmission in serodiscordant couples in India
Interventions targeting the uninfected partner
(i) Voluntary counselling and testing (VCT): VCT though primarily directed at the diagnosis of HIV infection has been shown to greatly influence risk-taking practices among both clients who have tested positive as well as those who test negative12,13. India has over 5000 stand alone VCT centres and greater than 1500 VCTs that have been integrated into ART centres, primary health centres or other such facilities14. Further, there are several laboratories and non-governmental organizations/community-based organizations (CBOs) that provide VCT. Yet, uptake of VCT is overall low especially among high-risk populations. For example, in a large community based survey of 4,597 MSM and hijras in India, rates of ever being tested for HIV ranged from 13-56 per cent11. Also, rates of testing among spouses of HIV-infected individuals (particularly HIV-infected MSM and IDUs) remain low. Interventions need to be developed to improve testing rates among spouses of HIV-infected persons and also to improve rates of testing among individuals who commonly indulge in high-risk behaviour such as unprotected sexual intercourse.
(ii) Male medical circumcision (MMC): Three randomized clinical trials have estimated the efficacy of MMC in the prevention of HIV acquisition to range between 51-60 per cent15–17. Yet, MMC is not an intervention commonly promoted in India. Circumcision has been historically linked with being Muslim in India and; therefore, there may be some hesitation in the adoption of MMC by the Hindu communities in India. Further, the cost-effectiveness of such an intervention in a country where the prevalence of HIV infection is 0.39 per cent is questionable. However, for HIV uninfected men who are in a heterosexual serodiscordant relationship, MMC may be feasible option. Also, MMC could possibly be offered at sexually transmitted disease (STD) clinics as these male clients are more likely to indulge in unprotected discordant sexual relationships.
(iii) Pre-risk exposure prophylaxis (PrEP): PrEP is a novel intervention wherein HIV uninfected individuals take antiretroviral agents [e.g., tenofovir (TDF), emtricitabine (FTC)] to prevent HIV acquisition. Three trials to date that support this strategy are: (i) the iPrEX trial among MSM and transgendered men (n=2499) identified the efficacy of TDF/FTC in the prevention of HIV acquisition to be 44 per cent18; (ii) the TDF2 trial (1200 heterosexual individuals in Africa) reported the efficacy of TDF/FTC to be 63 per cent19; and (iii) the Partners in PrEP (4758 serodiscordant couples in Africa) demonstrated the efficacy of TDF/FTC vs. placebo to be 73 per cent5. Partners in PrEP also had an arm that received TDF monotherapy – the efficacy of this arm vs. placebo was 62 per cent. In the two trials among heterosexual populations, TDF/FTC appeared to be beneficial in preventing transmission among both men and women. One key finding among all these studies was that the efficacy of PrEP increased with increasing levels of adherence. Given the findings of these studies, TDF/FTC appears to be a feasible option in the prevention of HIV acquisition especially among individuals in discordant relationships. But there are several challenges to the implementation of this strategy in the Indian sub-continent. First, TDF/FTC is expensive [ 1000 (US$ 24)] per month and so, without government buy-in, it would not be feasible. Second, in all these studies individuals were tested for HIV infection on a monthly basis to minimize the possibility of development of resistance in the case of seroconverters - this would probably not be possible in the real world. Third, if this was promoted as a strategy in India, any person who thinks he/she might be at the risk of HIV acquisition might procure TDF/FTC from the pharmacies over the counter. This might result in HIV-infected individuals who are unaware of their status taking dual-therapy (TDF/FTC) or monotherapy (TDF) and thereby develop resistance. The cost-effectiveness of this strategy as opposed to the other strategies also remains to be evaluated. Lastly, the acceptability of such a strategy among serodiscorant couples in India is yet to be evaluated.
1000 (US$ 24)] per month and so, without government buy-in, it would not be feasible. Second, in all these studies individuals were tested for HIV infection on a monthly basis to minimize the possibility of development of resistance in the case of seroconverters - this would probably not be possible in the real world. Third, if this was promoted as a strategy in India, any person who thinks he/she might be at the risk of HIV acquisition might procure TDF/FTC from the pharmacies over the counter. This might result in HIV-infected individuals who are unaware of their status taking dual-therapy (TDF/FTC) or monotherapy (TDF) and thereby develop resistance. The cost-effectiveness of this strategy as opposed to the other strategies also remains to be evaluated. Lastly, the acceptability of such a strategy among serodiscorant couples in India is yet to be evaluated.
(iv) Vaginal microbicide: A vaginal microbicide is a substance that a woman can insert intra-vaginally prior to coitus that minimizes her risk of HIV acquisition. To date, only one trial has demonstrated efficacy of such a strategy. The CAPRISA-004 trial was a randomized clinical trial of 889 women in South Africa randomized to either a 1 per cent TDF based gel microbicide vs. placebo gel microbicide20. The overall efficacy was 39 per cent but as with the PrEP trials the efficacy increased with increasing adherence levels. Further evidence is required prior to wide-scale implementation of this strategy. However, once available a vaginal microbicide would be a great tool for Indian women in serodiscordant relationships as negotiation of condom use generally results in intimate partner violence. A vaginal microbicide could serve as a means of a woman protecting herself without the knowledge of her partner. But as with PrEP several challenges exist in the implementation of microbicides in India such as cost, the need for monthly HIV testing and accessibility.
Interventions targeting the infected partner
(i) Standard antiretroviral therapy (ART): Highly active antiretroviral therapy (HAART) has dramatically improved survival of people living with HIV by suppressing viral replication21. Consequently, as a result of viral suppression, HAART also plays a major role in prevention of HIV transmission. The HIV viral load has been shown to be one of the strongest determinants of HIV transmission - the higher the viral load, the higher the risk of transmission22. Therefore, initiating HAART is an effective means of reducing risk of transmission among individuals in discordant relationships. India currently follows the WHO guidelines for initiation of HAART, which suggests initiation of ART at CD4<350 cells/μl. There are ~385,000 persons on first-line ART in India14. The challenge in this strategy is to ensure that the participants on ART maintain optimal adherence levels. There are a few studies that have objectively measured the rate of virological failure among patients on ART in India. Shah and colleagues23 estimated that 37 per cent of patients on ART at a private clinic in Mumbai were not virologically suppressed. No such reports exist in the government sector. However, according to the latest report of the National AIDS Control Organization (NACO), only 77 per cent of the patients initiated on ART were alive and still on ART14. Interventions to improve adherence are essential to maximize secondary prevention benefits of ART in the Indian context.
(ii) Universal ART (CD4>350 cells/μl): Over the past few years, there have been several reports suggesting individual-level benefits of initiating HAART at CD4 counts greater than what is currently recommended24,25. There have also been reports from cohort studies that suggested prevention benefits of initiating patients on ART as it resulted in a decline in the community viral load – the reservoir of HIV infection in the community26. However, the results of the recently halted HIV Prevention Trials Network Protocol 052, a multisite randomized clinical trial among serodiscordant couples, clearly demonstrated the benefit of early initiation of ART in prevention of HIV transmission among serodiscordant couples4. There was only one transmission event among couples randomized to the immediate ART arm compared to 27 transmissions in the delayed arm resulting in a 96 per cent reduction in the risk of HIV transmission. Early initiation of ART also had significant individual level benefits especially a reduced incidence of pulmonary TB. Also of importance was the finding that almost two thirds of the transmissions occurred at CD4 counts >350 cells/μl - the current cut-off for initiation of ART in India27. The one limitation of the study was the short-term follow up of the participants – the median duration of follow up was only 1.7 years. Therefore, long-term outcomes of this strategy are yet to be evaluated. However, the evidence from this trial is sufficient to recommend immediate initiation of ART especially for individuals in discordant relationships. There are a few key challenges to the implementation of such a strategy in the Indian context. First, the most commonly used ART regimen is a fixed-dose combination of stavudine, lamivudine and nevirapine14. Stavudine has several side-effects that result in it almost never being used in the developed world and nevirapine cannot be initiated in patients with higher CD4+ counts. Therefore, zidovudine or tenofovir and efavirenz would need to be used more commonly in first-line regimens if India were to adopt such a strategy, which could result in a dramatic increase in cost. Second, if India were to adopt this strategy it would theoretically imply that all the HIV-infected persons in India (~2.4 million) would qualify for HAART. The infrastructure and staffing to cater to this increased number of eligible persons seem inadequate. While this strategy does appear to be the most effective in prevention of transmission among discordant couples, issues such as cost, infrastructure and costing need to discussed prior to implemention.
Interventions that can be targeted at both partners
(i) Risk reduction counselling (RRC): Risk reduction counselling is often overlooked in the planning of intervention programmes. However, RRC is probably one of the most cost-effective interventions available that is also very easy to implement. RRC has been associated with substantial reduction in both sexual and injection risk taking practices in India28,29. RRC should be promoted as a first-step when dealing with persons in discordant relationships in the Indian context.
(ii) Condom promotion: Male condoms, if properly used, dramatically reduce the risk of HIV acquisition. Condoms also play a key role in the secondary transmission of HIV. If the HIV-infected partner uses a condom correctly, the risk of transmission to his partner is greatly reduced. There is not much evidence to support the role of female condoms in the transmission/acquisition of HIV infection. As with RRC, condoms are a very-cost effective intervention that is widely available. Yet, utilization rates among individuals in discordant relationships is low30. Discordant couples along with RRC should be strongly encouraged to use condoms to minimize sexual transmission of HIV to their uninfected partners.
(iii) Syringe needle exchange programs (SNEP): SNEP have been associated with reduced HIV incidence31,32. Adequate access to clean injecting equipment results in minimal sharing consequently resulting in a reduction in the risk of HIV transmission/acquisition. There are several drug users who use drugs only in closed networks. If one of the individuals in this network is HIV-infected, he/she would therotically be engaging in a discordant relationship with all the HIV-uninfected members in the group. SNEP are relatively cheap and easy to implement. Yet, access to clean needles/syringes appear to be a major concern for IDUs in India with most IDUs reporting that they procure their needles from pharmacies33. If needles/syringes were made available to IDUs free-of-charge via SNEP, it would greatly impact the transmission/acquisition of HIV among serodiscordant IDU networks. Also, there have been reports in the North Eastern States of India of sharing of injection needles between husband and wife - again, a risk for HIV transmission that could be avoided with access to clean injection equipment34,35.
(iv) Opiate substitution therapy (OST): Opiate substitution therapy, as with SNEP, reduces the risk of HIV transmission/acquisition by stopping/reducing the frequency of injection31. Like SNEP, OST will only benefit IDUs in discordant injection networks. However, OST is relatively more complicated and expensive to implement compared to SNEP and not widely available in India36. Yet, it is a very effective intervention and should definitely be implemented especially in areas with high-levels of physiological dependence such as the NE States.
Selecting the intervention for a serodiscordant couple
The selection of an intervention(s) depends primarily on the nature of the serodiscordant relationship (e.g., homosexual, heterosexual, etc.), the availability of interventions and the willingness of the persons in the discordant relationship to avail himself/herself of an intervention. There is currently no single intervention that will work for all individuals. Hence, the key is to provide the couple with options and work with them to identify the intervention(s) that is most applicable to their relationship and lifestyle. Figs 1 and 2 provide a rough guide of the variety of interventions available to individuals in a discordant relationship depending on gender and type of discordant relationship. Despite the existence of ample scientific evidence for most of the interventions (with the exception of female microbicides), not all of these interventions are accessible by all persons in India.
Fig. 1.
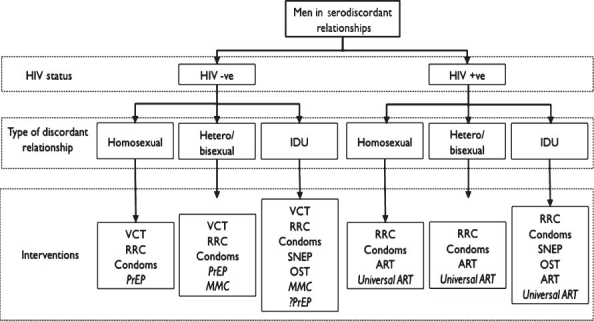
Interventions for men in serodiscordant relationships. VCT, voluntary counseling and testing; RRC, risk reduction counselling; PrEP, pre-risk exposure prophylaxis; MMC, male medical circumcision; SNEP, syringe needle exchange programmes; OST, opiate substitution therapy; ART, antiretroviral therapy. Italicized interventions indicate interventions not currently available in India.
Fig. 2.
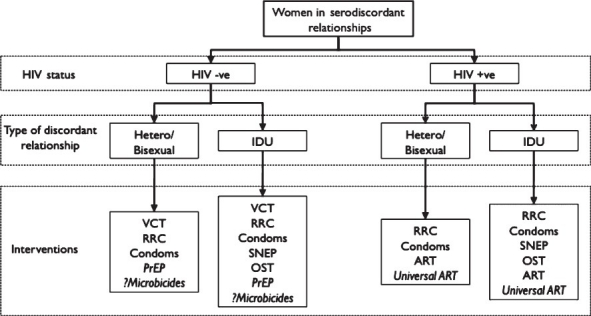
Interventions for women in serodiscordant relationships. VCT, voluntary counselling and testing; RRC, risk reduction counselling; PrEP, pre-risk exposure prophylaxis; SNEP, syringe needle exchange programmes; OST, opiate substitution therapy; ART, antiretroviral therapy. Italicized interventions indicate interventions not currently available in India.
Given these limitations in the access to these interventions, voluntary counselling and testing, risk reduction counselling and condom promotion, if applicable, should definitely be promoted as a first-step in the control of transmission of HIV among persons in discordant relationships. These three interventions are widely available in India and steps should be taken to improve their utilization. Syringe and needle exchange programmes and opiate substitution programmes currently exist in India but are far too few. Steps should be taken to improve access to these services especially in regions with high numbers of IDUs as these interventions are crucial to the control of the spread of HIV among persons in discordant HIV injection networks. HIV-infected persons who qualify for ART should be initiated on ART as soon as possible and measures should be taken to ensure optimal adherence to ART to minimize transmission to their partners.
In terms of the novel prevention tools, immediate initiation of ART appears to be the most promising in the control of HIV transmission among serodiscordant couples in the Indian setting given the low HIV prevalence in the country. While results of the trials of MMC and TDF/FTC have also shown promising results, the acceptability and cost-effectiveness of these strategies among all serodiscordant relationships in India remains unclear. Adherence to the interventions appears to be the key element whether it be condoms, PrEP or ART - hence, interventions to improve adherence need to be evaluated and implemented.
Social and cultural issues
There are several social and cultural issues, which play a role among persons in discordant relationships. In India, parents expect their children to get married and often arrange the marriages of their children. In most cases, men/women who are HIV positive do not reveal their status to their parents due to stigma attached to HIV disease. These marriages result in the formation of discordant couples37. While the infected individual might attempt to protect their spouse from HIV infection by practicing safe sex, there is soon pressure on the newly wed couple from the parents and society for children.
The management of these socio-cultural issues is crucial to the control of transmission of HIV among discordant couples. Today, there are a few centres that arrange marriages among HIV-positive persons. But for individuals who are already in discordant relationships and under pressure to produce offspring, counselling should be offered to provide them with option such as adoption or assisted reproductive techniques. The role of ART in the infected partner and/or PrEP/PEP in the uninfected partner to produce a HIV-free conception in cases where the male partner is infected appears to be promising4,5,18 but remains to be evaluated.
Conclusion
There are several novel tools currently available for discordant couples but only a limited number of these are available in India. Despite the availability of interventions such as VCT, condoms and risk reduction counselling, the utilization of these services is still low. Steps should first be taken to ensure that the utilization of these cheap, easy to implement interventions reach the target population. Immediate initiation of ART appears to be the most promising intervention for preventing HIV transmission among serodiscordant couples but several challenges remain prior to its implementation. There are also several socio-cultural issues that need to be considered while dealing with serodiscordant couples in India.
References
- 1.Pneumocystis pneumonia--Los Angeles. MMWR Morb Mortal Wkly Rep. 1981;30:250–2. [PubMed] [Google Scholar]
- 2.Simoes EA, Babu PG, John TJ, Nirmala S, Solomon S, Lakshminarayana CS, et al. Evidence for HTLV-III infection in prostitutes in Tamil Nadu (India) Indian J Med Res. 1987;85:335–8. [PubMed] [Google Scholar]
- 3.UNAIDS. Global Report: UNAIDS Report on the Global AIDS Epidemic. 2010. [accessed on September 21, 2011]. Available from: http://www.unaids.org/globalreport/documents/20101123_GlobalReport_full_en.pdf .
- 4.Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baeten J, Celum C. 6th IAS Conference on HIV Pathogenesis, Treatment and Prevention. Rome, Italy: 2010. Feb 16-19, Antiretroviral Pre-Exposure Prophylaxis for HIV-1 prevention among heterosexual African men and women: the Partners PrEP Study (Abstract #: MOAX0106) [Google Scholar]
- 6.Kumar MS, Virk HK, Chaudhuri A, Mittal A, Lewis G. A rapid situation and response assessment of the female regular sex partners of male drug users in South Asia: factors associated with condom use during the last sexual intercourse. Int J Drug Policy. 2008;19:148–58. doi: 10.1016/j.drugpo.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 7.Solomon SS, Srikrishnan AK, Celentano DD, Johnson SC, Vasudevan CK, Murugavel KG, et al. The intersection between sex and drugs: a cross-sectional study among the spouses of injection drug users in Chennai, India. BMC Public Health. 2011;11:39. doi: 10.1186/1471-2458-11-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Panda S, Chatterjee A, Bhattacharya SK, Manna B, Singh PN, Sarkar S, et al. Transmission of HIV from injecting drug users to their wives in India. Int J STD AIDS. 2000;11:468–73. doi: 10.1258/0956462001916137. [DOI] [PubMed] [Google Scholar]
- 9.Panda S, Kumar MS, Lokabiraman S, Jayashree K, Satagopan MC, Solomon S, et al. Risk factors for HIV infection in injection drug users and evidence for onward transmission of HIV to their sexual partners in Chennai, India. J Acquir Immune Defic Syndr. 2005;39:9–15. doi: 10.1097/01.qai.0000160713.94203.9b. [DOI] [PubMed] [Google Scholar]
- 10.Sarkar S, Mookerjee P, Roy A, Naik TN, Singh JK, Sharma AR, et al. Descriptive epidemiology of intravenous heroin users--a new risk group for transmission of HIV in India. J Infect. 1991;23:201–7. doi: 10.1016/0163-4453(91)92364-b. [DOI] [PubMed] [Google Scholar]
- 11.Brahmam GN, Kodavalla V, Rajkumar H, Rachakulla HK, Kallam S, Myakala SP, et al. Sexual practices, HIV and sexually transmitted infections among self-identified men who have sex with men in four high HIV prevalence states of India. AIDS. 2008;22(Suppl 5):S45–57. doi: 10.1097/01.aids.0000343763.54831.15. [DOI] [PubMed] [Google Scholar]
- 12.Denison JA, O’Reilly KR, Schmid GP, Kennedy CE, Sweat MD. HIV Voluntary Counseling and Testing and behavioral risk reduction in developing countries: A meta-analysis, 1990-2005. AIDS Behav. 2007;12:363–73. doi: 10.1007/s10461-007-9349-x. [DOI] [PubMed] [Google Scholar]
- 13.Painter TM. Voluntary counseling and testing for couples: a high-leverage intervention for HIV/AIDS prevention in sub-Saharan Africa. Soc Sci Med. 2001;53:1397–411. doi: 10.1016/s0277-9536(00)00427-5. [DOI] [PubMed] [Google Scholar]
- 14.National AIDS Control Organization (NACO) I. Annual Report 2010-11. 2011. [accessed on September 21, 2011]. Available from: http://nacoonline.org/upload/REPORTS/NACO%20Annual%20Report%202010-11.pdf .
- 15.Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS Med. 2005;2:e298. doi: 10.1371/journal.pmed.0020298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bailey RC, Moses S, Parker CB, Agot K, Maclean I, Krieger JN, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet. 2007;369:643–56. doi: 10.1016/S0140-6736(07)60312-2. [DOI] [PubMed] [Google Scholar]
- 17.Gray RH, Kigozi G, Serwadda D, Makumbi F, Watya S, Nalugoda F, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet. 2007;369:657–66. doi: 10.1016/S0140-6736(07)60313-4. [DOI] [PubMed] [Google Scholar]
- 18.Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363:2587–99. doi: 10.1056/NEJMoa1011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thigpen MC, Kebaabetswe P, Smith DK, Segolodi TM, Soud FA, Chillag K, et al. 6th IAS Conference on HIV Pathogenesis, Treatment and Prevention. Rome, Italy: 2011. Jul 17-20, Daily oral antiretroviral use for the prevention of HIV infection in heterosexually active young adults in Botswana: results from the TDF2 study (Abstract #: WELBC01) [Google Scholar]
- 20.Abdool Karim Q, Abdool Karim SS, Frohlich JA, Grobler AC, Baxter C, Mansoor LE, et al. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science. 2010;329:1168–74. doi: 10.1126/science.1193748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mocroft A, Vella S, Benfield TL, Chiesi A, Miller V, Gargalianos P, et al. Changing patterns of mortality across Europe in patients infected with HIV-1.EuroSIDA Study Group. Lancet. 1998;352:1725–30. doi: 10.1016/s0140-6736(98)03201-2. [DOI] [PubMed] [Google Scholar]
- 22.Gray RH, Wawer MJ, Brookmeyer R, Sewankambo NK, Serwadda D, Wabwire-Mangen F, et al. Probability of HIV-1 transmission per coital act in monogamous, heterosexual, HIV-1-discordant couples in Rakai, Uganda. Lancet. 2001;357:1149–53. doi: 10.1016/S0140-6736(00)04331-2. [DOI] [PubMed] [Google Scholar]
- 23.Shah B, Walshe L, Saple DG, Mehta SH, Ramnani JP, Kharkar RD, et al. Adherence to antiretroviral therapy and virologic suppression among HIV-infected persons receiving care in private clinics in Mumbai, India. Clin Infect Dis. 2007;44:1235–44. doi: 10.1086/513429. [DOI] [PubMed] [Google Scholar]
- 24.Sterne JA, May M, Costagliola D, de Wolf F, Phillips AN, Harris R, et al. Timing of initiation of antiretroviral therapy in AIDS-free HIV-1-infected patients: a collaborative analysis of 18 HIV cohort studies. Lancet. 2009;373:1352–63. doi: 10.1016/S0140-6736(09)60612-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kitahata MM, Gange SJ, Abraham AG, Merriman B, Saag MS, Justice AC, et al. Effect of early versus deferred antiretroviral therapy for HIV on survival. N Engl J Med. 2009;360:1815–26. doi: 10.1056/NEJMoa0807252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Montaner JS, Lima VD, Barrios R, Yip B, Wood E, Kerr T, et al. Association of highly active antiretroviral therapy coverage, population viral load, and yearly new HIV diagnoses in British Columbia, Canada: a population-based study. Lancet. 2010;376:532–9. doi: 10.1016/S0140-6736(10)60936-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.NACO ART guidelines for HIV- infected adults and adolescents including PEP, (May 2007) - November 2011 revision. New Delhi: NACO; 2011. National AIDS Control Organization (NACO), India. [Google Scholar]
- 28.Solomon SS, Celentano DD, Srikrishnan AK, Vasudevan CK, Murugavel KG, Iqbal SH, et al. Low incidences of human immunodeficiency virus and hepatitis C virus infection and declining risk behaviors in a cohort of injection drug users in Chennai, India. Am J Epidemiol. 2010;172:1259–67. doi: 10.1093/aje/kwq288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Solomon SS, Solomon S, Masse BR, Srikrishnan AK, Beauchamp G, Thamburaj E, et al. Risk reduction counseling is associated with decreased HIV transmission-associated behaviors in high-risk Indian heterosexuals. J Acquir Immune Defic Syndr. 2006;42:478–83. doi: 10.1097/01.qai.0000221684.83057.2f. [DOI] [PubMed] [Google Scholar]
- 30.Serwadda D, Gray RH, Wawer MJ, Stallings RY, Sewankambo NK, Konde-Lule JK, et al. The social dynamics of HIV transmission as reflected through discordant couples in rural Uganda. AIDS. 1995;9:745–50. doi: 10.1097/00002030-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 31.Drucker E, Lurie P, Wodak A, Alcabes P. Measuring harm reduction: the effects of needle and syringe exchange programs and methadone maintenance on the ecology of HIV. AIDS. 1998;12(Suppl A):S217–30. [PubMed] [Google Scholar]
- 32.Hurley SF, Jolley DJ, Kaldor JM. Effectiveness of needle-exchange programmes for prevention of HIV infection. Lancet. 1997;349:1797–800. doi: 10.1016/S0140-6736(96)11380-5. [DOI] [PubMed] [Google Scholar]
- 33.Solomon SS, Desai M, Srikrishnan AK, Thamburaj E, Vasudevan CK, Kumar MS, et al. The profile of injection drug users in Chennai, India: identification of risk behaviours and implications for interventions. Subst Use Misuse. 2010;45:354–67. doi: 10.3109/10826080903452447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chakrapani V, Newman PA, Shunmugam M, Dubrow R. Social-structural contexts of needle and syringe sharing behaviours of HIV-positive injecting drug users in Manipur, India: a mixed methods investigation. Harm Reduct J. 2011;8:9. doi: 10.1186/1477-7517-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rezza G, Titti F, Tempesta E, di Giannantonio M, Weisert A, Rossi GB, et al. Needle sharing and other behaviours related to HIV spread among intravenous drug users. AIDS. 1989;3:247–8. [PubMed] [Google Scholar]
- 36.Steinbrook R. HIV in India--a complex epidemic. N Engl J Med. 2007;356:1089–93. doi: 10.1056/NEJMp078009. [DOI] [PubMed] [Google Scholar]
- 37.Newmann S, Sarin P, Kumarasamy N, Amalraj E, Rogers M, Madhivanan P, et al. Marriage, monogamy and HIV: a profile of HIV-infected women in south India. Int J STD AIDS. 2000;11:250–3. doi: 10.1258/0956462001915796. [DOI] [PubMed] [Google Scholar]


