Abstract
With the availability of antiretroviral therapy (ART), HIV infection, which was once considered a progressively fatal illness, has now become a chronic treatable condition in children, as in adults. However, the challenges these children are forced to face are far more daunting. The most significant shortcoming in the response to paediatric HIV remains the woefully inadequate prevention of mother-to-child transmission (PMTCT), allowing a large number of children to be born with HIV in the first place, in spite of it being largely preventable. In the west, mother-to-child transmission has been virtually eliminated; however, in resource-limited settings where >95 per cent of all vertical transmissions take place, still an infected infants continue to be born. There are several barriers to efficient management: delayed infant diagnosis, lack of appropriate paediatric formulations, lack of skilled health personnel, etc. Poorly developed immunity allows greater dissemination throughout various organs. There is an increased frequency of malnutrition and infections that may be more persistent, severe and less responsive to treatment. In addition, these growing children are left with inescapable challenges of facing not only lifelong adherence with complex treatment regimens, but also enormous psychosocial, mental and neuro-cognitive issues. These unique challenges must be recognized and understood in order to provide appropriate holistic management enabling them to become productive citizens of tomorrow. To address these multi-factorial issues, there is an urgent need for a concerted, sustainable and multi-pronged national and global response.
Keywords: Challenges, clinical diagnosis, clinical manifestations, early infant diagnosis, immunization in children with HIV, management, nutrition, psychosocial issues, paediatric HIV, trends
Global and national trends
Globally an estimated 2.5 million children are living with HIV/AIDS, 10,000 becoming infected daily and 2,60,000 deaths of children under 15 occur due to AIDS related illnesses1. The estimated 2,60,000 (1,50,000-3,60,000) children who died from AIDS-related illnesses in 2009 were 19 per cent fewer than the estimated 3,20,000 (2,10,000-4,30,000) who died in 2004. This trend reflects the steady expansion of services to prevent transmission of HIV to infants and an increase (albeit slow) in access to treatment for children2. The United Nations General Assembly renewed its commitment to ‘accelerate progress towards the elimination of new child infections by 2015, reducing the number of new HIV infections among children by 90 per cent by the year 2015 and reducing mother-to-child transmission of HIV (MTCT) to 5 per cent1.
In 2009, it was estimated that there were 2.39 million people living with HIV in India. Of these, women constitute 36 per cent while children comprised 4.4 per cent3. The estimated numbers of children living with HIV was 1,05,000. Of these, 77,044 children were registered in 285 ART (antiretroviral therapy) centres, with 21,343 receiving free ART till August 2010. There has been a significant scale up of HIV counselling and testing, PPTCT and ART services for adults, adolescents and children over the last five years. Between 2004 and 2009, the number of pregnant women tested annually in the national prevention of parent-to-child transmission (PPTCT) programme increased from 8,00,000 to 5.4 million, and services have expanded to the rural primary health care level3.
Of the 27 million pregnancies estimated annually in India, only half attend health services to seek skilled care during childbirth. Of those who attend health services, less than half have had HIV counselling and testing3. In the absence of any intervention, a substantial proportion of children born to women living with HIV will acquire the virus from their mother during pregnancy, labour, delivery and through breastfeeding. Without any intervention, the risk of transmission from parent-to-child is estimated to be 20-45 per cent4–8.
Clinical diagnosis of HIV
Children differ from adults in that they have high rates of viral replication, very high HIV-1 viral load, high rates of CD4+ cell destruction, viral mutation, faster rate of disease progression and good immunologic response to ART8.
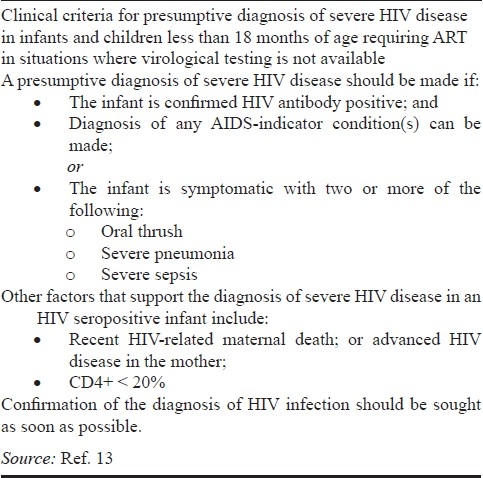
Clinical symptoms vary widely between infants, children and adolescents; most are asymptomatic at birth and do not have any abnormal findings9. In view of the availability of ART since the global roll out, there has been a changing spectrum of opportunistic infections (OIs) from the pre- ART era. The spectrum of infections also varies in those on ART but non- adherent to therapy. WHO clinical criteria for presumptive diagnosis of severe HIV disease in infants and children less than 18 months of age is given in Table I.
Table I.
WHO - Presumptive diagnosis of severe HIV disease in infants < 18 months
Clinical staging of children who have confirmed or highly suspected HIV infection helps to assess the severity of illness, plan treatment options, assess disease progression and determine when to start, stop or switch ARV therapy.
Laboratory diagnosis and follow up
The diagnosis of HIV infection in an infant or child requires an integrated system of clinical, programmatic and laboratory services which are continuously monitored for quality and outcome. It is of critical importance to identify HIV exposure, establish a definitive diagnosis and institute treatment at the earliest in children < 2 years as they can rapidly deteriorate and die8.
The diagnosis of HIV infection in the exposed infants is difficult because routine screening tests like rapid test, ELISA will only detect presence maternal antibodies. Hence, these tests are useful in children > 18 months of age; and for children < 18 months it is necessary to do DNA- PCR testing using dried blood spots (DBS) which detects viral DNA. All diagnostic HIV testing of children must be confidential, accompanied by counselling and informed consent of the parent or guardian. In breast-fed infants, there is a need for repeat DNA-PCR testing at least 6 wk after cessation of breastfeeding to confirm a HIV negative diagnosis. Figs 1 and 2 show early infant diagnosis (EID) algorithm. After 18 months of age a screening test (spot/ ELISA) must be done to confirm the serological status. Infants and children with confirmed HIV infection need a baseline CD4 testing (absolute count & CD4 %) and repeat every 6 months or earlier if clinically indicated. All children on ART should have regular clinical, immunological and virological monitoring (where feasible) for early recognition of treatment failure10.
Fig. 1.
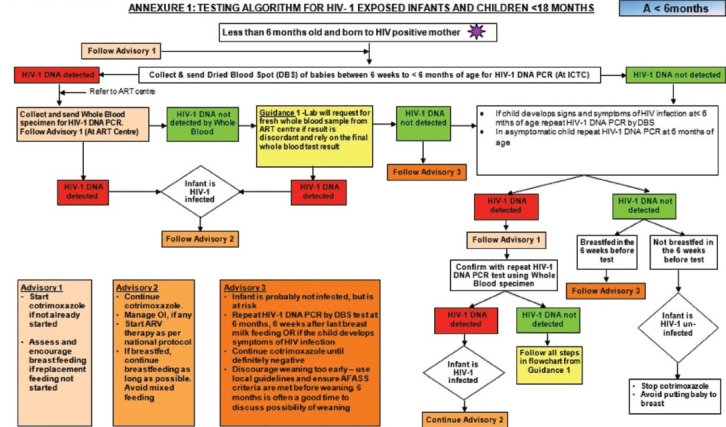
Early infant diagnosis (EID): Testing algorithm for HIV - 1 exposed infants < 6 months. Source: Ref 25.
Fig. 2.
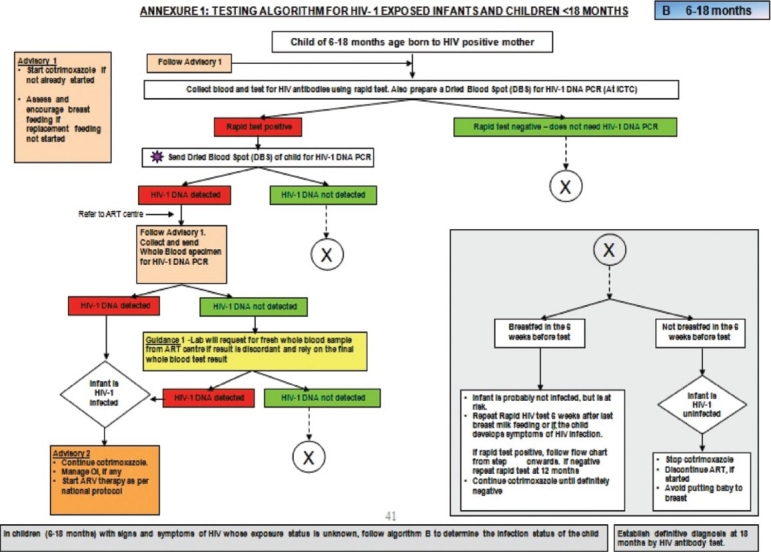
Early infant diagnosis (EID): Testing algorithm for HIV - 1 exposed infants & children 6 - 18 months of age. Source: Ref 25.
Treatment
After the availability of free global ART roll out, HIV infection which was once considered a progressive fatal illness, has now become a chronic treatable illness. The barriers to efficient management of paediatric HIV/AIDS are delayed infant HIV diagnosis, lack of appropriate paediatric ARV formulations and lack of skilled health personnel. All infants with a positive virological test should be started on ART and it is well established that initiation of ART at an early age can reduce morbidity and mortality11. Once an infant or child has been started on ART, regular monitoring for adherence, response to therapy, potential drug toxicities or treatment failure should be done vigilantly12. Baseline clinical and laboratory assessment should be done in every child before initiating ART (Table II)12.
Table II.
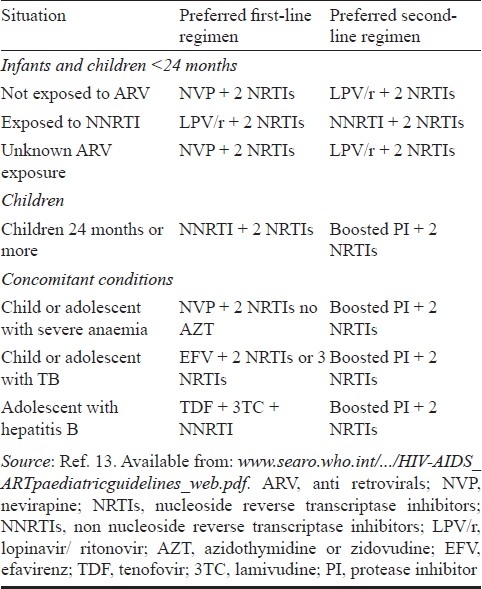
Summary of preferred first line ARV regimens for infants and children
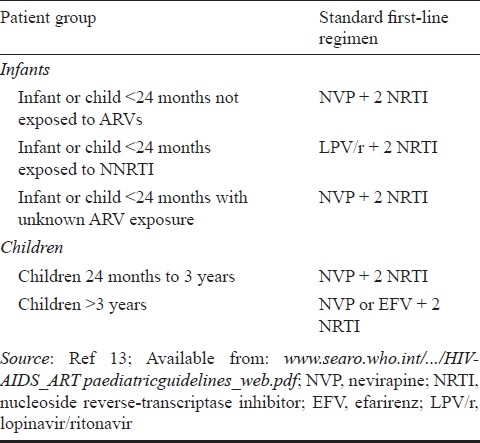
The use of three ARV medications is the standard treatment for HIV infection in order to achieve the best possible viral suppression, increase CD4 count and improve clinical staging12. The preferred option when choosing a first-line regimen for infants and children is two nucleoside reverse transcriptase inhibitors (NRTIs) plus one non-nucleoside reverse transcriptase inhibitor (NNRTI) (Table II)13.
These regimens are efficacious, less expensive, and available from the national ART roll out programme and a cold chain is not required. In addition, the potent class of protease inhibitors (PIs) are to be saved for the second line regimen.
It is appropriate to initiate ART for all HIV infected children < 2 yr of age irrespective of the CD4 count and clinical staging because of high mortality (upto 50%) and poor predictability of immunologic status by CD4 count13. In children less than two years of age who are not exposed to ARV during antenatal, natal and postnatal period, it is appropriate to start with NNRTI (nevirapine, NVP) based regimen. Efavirenz (EFV) is not considered in children <3 yr of age because of inadequate information on dosage. If the Hb is <8 g/dl, stavudine (d4T) is preferred over zidovudine (AZT) to avoid haemopoietic toxicity.
In children <2 yr of age who are exposed to maternal or/and infant nevirapine, it is recommended to start a boosted protease inhibitor (PI) based regimen (lopinavir/ritonavir, LPV/r) because of concerns about persistence of resistant mutants to NVP. In children between 2-5 yr of age, ART may be initiated if the CD4 is less than 25 per cent or <750 cells/μl (or whichever is lower). Children 3 yr and older can be started on NNRTI based regimen plus two NRTIs. Children older than 3 yr with HIV-TB co-infection should be given efavirenz to avoid interaction between nevirapine and rifampicin. In adolescents older than 12 yr of age with HIV and hepatitis B co-infection, the recommended regimen is tenofovir (TDF) + emtricitabine (FTC)/lamivudine (3TC) + NVP/EFV13. This regimen offers the benefit of providing two potent drugs against hepatitis-B infection. The use of efavirenz should be avoided in adolescent girls due to its teratogenic potential in the first trimester of pregnancy and to children less than three years of age due to lack of dosage information.
The use of triple NRTI regimen can be considered an option for initial therapy in some special circumstances like HIV-TB co-infection in children <3 yr where EFV cannot be used as a substitute to NVP. The bottom line in ART is to ensure >90 per cent adherence to maximize the long term benefits of virological suppression, immunological improvement and clinical recovery.
Co-trimoxazole (CTX) prophylaxis is given to all HIV exposed infants from 6 wk onwards and continued till 5 yr of age irrespective of clinical/immune category because it provides prophylaxis against Pneumocystis carinii pneumonia (PCP) and other common childhood infections13. When HIV infection has been excluded or a child >5 yr of age who is on ART with a sustained CD4 >25 per cent, CTX prophylaxis can be stopped13.
Immune reconstitution inflammatory syndrome (IRIS) is a paradoxical clinical deterioration caused by an exaggerated inflammatory immune response and may occur in the context of treated or untreated infections such as TB, cytomegalovirus (CMV), Herpes, etc., and typically presents during the period following ART initiation in the presence of a rising CD4 count and a decreasing HIV viral load.
Monitoring and follow up of children on ART
After commencing an infant or child on ART it is vital for frequent clinical monitoring at 2 wk after initiation and every 4 wks thereafter. These visits are to evaluate growth and development, immunization status and provide nutrition counselling. There is also an opportunity to educate the parents and care providers on adverse drug reactions, ART adherence and symptoms of common OIs13.
ARV drug toxicities12
The most common toxicities include the following:
Haematological: with AZT (anaemia, neutropenia and, thrombocytopenia).
Mitochondrial dysfunction: with other NRTI drugs: include lactic acidosis, hepatic toxicity, pancreatitis and peripheral neuropathy.
Lipodystrophy and other metabolic abnormalities: more common with stavudine (d4T) and protease inhibitors, and to a lesser degree with other NRTI drugs. Abnormalities include fat maldistribution and body habitus changes, hyperlipidaemia, hyperglycaemia, insulin resistance, diabetes mellitus, osteopenia, osteoporosis and osteonecrosis.
Allergic reactions: including skin rashes and hypersensitivity reactions. These are more common with the NNRTI drugs, but also seen with certain NRTI drugs, such as abacavir (ABC).
Hepatic dysfunction: in children with hepatic dysfunction of any aetiology NVP requires careful consideration because of its potential life threatening hepatotoxicity.
Discontinuation and drug substitution
As a general principles mild toxicities do not require discontinuation of therapy or drug substitution, and symptomatic treatment may be given (e.g. antihistamines for a mild rash). Moderate or severe toxicities may require substitution with a drug in the same ARV class but with a different toxicity profile, or with a drug from a different class. These do not require discontinuation of all ART. Severe life-threatening toxicities require discontinuation of all ARV drugs, and the initiation of appropriate supportive therapy until the patient is stabilized and the toxicity is resolved.
ART regimen failure
Poor adherence, inadequate drug levels or primary drug resistance can all contribute to ARV treatment failure. Genetic differences in drug metabolism may also be important14–16. When treatment failure is confirmed, switching to a new second-line regimen becomes necessary. Prior to switching therapy, it is essential to assess and address adherence issues.
Clinical criteria
The appearance of new WHO clinical stage 3 or 4 events in a child on ART may reflect disease progression and treatment failure provided the child is adherent to therapy15,17.
Immunological criteria: It is characterized by a drop in the CD4 count to values at or below the age-dependent values, or a failure of the CD4 count to rise above these threshold values7. It can be defined as a return of CD4 cell count to ‘pre-therapy baseline’ or below, after initial immune recovery, without any other concomitant infection to explain transient CD4 cell decrease or a greater than 50 per cent fall from ‘on therapy CD4 cells peak level’ without any other concomitant infection to explain transient CD4 cell decrease18.
Virological criteria: Virological failure is recognized if the child is adherent to first-line ART regimen for more than 24 wk from initiation, and has a persistent viral load over 5000 copies/ml. In resource-limited settings it may not be feasible to perform viral load testing. Availability of viral load is not a prerequisite for initiation of ART or for determination of treatment failure18.
Choice of second-line regimen: Children who fail the initial regimen of 2 NRTIs + 1 NNRTI, a regimen based on a protease inhibitor boosted with Ritonavir (PI/r) and combined with 2 NRTIs is recommended as the second-line treatment. The child should be referred to a setting where specialized HIV care is provided (Table III)7.
Table III.
Preferred first- and second-line regimens
Other issues
Psychosocial management of pediatric HIV: HIV is a social disease and its management requires all aspects of physical, psychological, spiritual and social support along with community mobilization and participation. Children face social ostracization, drop out from school and face an endless fall through the social security network. Worldwide HIV is leaving children orphaned and vulnerable to every conceivable danger, disease and disaster19,20.
Since most paediatric infections are vertical transmissions, the implications are that the mother and quite possibly the father are also infected. Therefore, counselling is necessary for the family as a unit. Family members should be sensitized about the importance of status disclosure to children and provide age specific information periodically. During adolescent years counselling should focus on life skill management and ART adherence.
Children who are orphaned due to HIV/AIDS fall through the established social security networks. A child orphaned due to causes other than HIV is usually absorbed into the extended family, whereas, HIV may create an impenetrable barrier to such an opportunity. The children who lose extended family support are less likely to access health care, are at a higher risk of labour and sexual exploitation and contracting HIV/AIDS if they have not already got it through their parents. They lack legal protection, lose inheritance rights and access to essential services available to other community members. Professional help from doctors, teachers and lawyers may be less forthcoming to a child who does not have a parent or foster care provider19,20.
Immunization: HIV-infected children are more susceptible to diseases caused by infectious agents and are more likely to develop severe complications when compared to immune-competent children. Thus it becomes imperative to immunize them against all vaccine-preventable diseases. HIV-infected infants and children can safely receive most childhood vaccines although effective response depends on the degree of immune-suppression.
NACO recommends routine immunization to all HIV exposed infants and children18.
In general, it is preferable to avoid live-virus vaccines if an alternative inactivated vaccine is available such as polio, influenza. Also, live attenuated vaccines are generally not recommended with the exception of measles, mumps, rubella vaccine and varicella vaccines which can be given to children who are not severely immuno-compromised. The current WHO recommendation is that for infants born to HIV-infected mothers where early HIV diagnostic testing can be performed, BCG can be deferred until diagnostic testing results are available, in view of the significantly high risk of disseminated BCG disease in sick infants10.
Inactivated vaccines are used for diphtheria, tetanus, and pertussis and thus are unlikely to pose significant risk to patients with HIV infection. Invasive pneumococcal disease remains a source of significant morbidity and mortality among HIV-infected individuals, hence pneumococcal vaccination will help reduce invasive pneumococcal disease; Likewise Haemophilus influenzae and meningococcal vaccines will help reduce invasive diseases.
All other vaccines under the Expanded Programme of Immunisation (EPI), including Haemophilus influenzae type B and pneumococcal vaccine should be offered. Human papilloma virus vaccine is recommended for young girls between 9 to 26 yr, since this virus is associated with an increased risk of anogenital cancers in HIV infection112,21,22.
Nutrition: Micro- and macronutrients deficiencies are common in HIV infected children impacting on the progression of the disease leading to growth failure and increased risk of morbidity and mortality. Energy needs increase by 10 per cent even in asymptomatic children, up to 25-30 per cent with chronic or recurring infections and TB, and going up further to a maximum of 50-100 per cent increase during periods of severe malnutrition12. Common causes for inadequate nutrition are chronic illness, poverty, lack of knowledge, inadequate access to food, parental illness, psychosocial problems and adverse effects of drugs.
Although the risk of transmission through breast feeding is about 14 per cent, the decision on policy to breastfeed or not is left to national health authorities taking into consideration socio-economic conditions, quality of health services, local epidemiology, causes of infant and child mortality. NACO recommends exclusive breast feeding for the first six months7,12.
Challenges and way ahead in paediatric HIV/AIDS
To address the multi-factorial issues that revolve around HIV/AIDS in children, there is an urgent need for a concerted, sustainable and multi-pronged national and global response20–22:
-
(i)
Improved ANC coverage.
-
(ii)
Flexibility of PMTCT protocol in different health care settings.
-
(iii)
Quality care to keep mother and child alive and healthy.
-
(iv)
Ensuring breast milk safer by extended ARV prophylaxis during lactation.
-
(v)
Improve follow up of mother - infant pair and early infant diagnosis leading to early initiation of ART in children <2 yr of age.
-
(vi)
Periodic RNA-PCR assay (viral load) in children on ART for early diagnosis of failing regimen and initiation of 2nd line ART.
-
(vii)
Improve availability and accessibility of 2nd line ART.
-
(viii)
Update policies and legal documents pertaining to confidentiality, consent and status disclosure in children and adolescents.
-
(ix)
Need for a comprehensive supplementary nutrition programme to be urgently implemented (micro & macro nutrients).
-
(x)
Inclusion of a paediatrician as integral part of care continuum of children living with HIV/AIDS.
-
(xi)
Identify areas of need based research in pediatric AIDS.
“Offer care beyond illness,
care beyond ART and
care beyond childhood and adolescence”
References
- 1.HIV/AIDS in the context of other global challenges, Global 2015, Special report for the UN high level meeting on AIDS. 2011 [Google Scholar]
- 2.UNAIDS report on the global AIDS epidemic. 2010. [accessed on August 13, 2011]. Available from: www.unaids.org/globalreport/global_report.htm .
- 3.NACO Annual report. [accessed on August 8, 2011]. Available from: http://www.nacoonline.org/Quick_Links/HIV_Data/
- 4.AIDS epidemic update, Global report. UNAIDS. 2010. [accessed on December 2011]. Available from: http://www.unaids.org/documents/20101123_GlobalReport_Chap2_em.pdf .
- 5.Report of the First National Consultative Meeting of Pediatric HIV, facilitated by NACO, IAP & UNICEF. Supported by WHO & Clinton Foundation. 2006 [Google Scholar]
- 6.UNICEF India HIV/AIDS. [accessed on August 13, 2011]. Available from: http://www.unicef.org/india/hiv_aids.html .
- 7.National guidelines for the prevention of parent to child transmission (PPTCT) - Technical guidelines, National AIDS Control Organisation. [accessed on September 24, 2011]. Available from: http://www.nacoonline.org/National_AIDS_Control_Program/Services_for_Prevention/PPTCT/
- 8.Behrman R, Kleigman R, Jenson H. Nelson textbook of pediatrics. 18th ed. Philadelphia: W.B. Saunders Company; 2007. [Google Scholar]
- 9.Abuzaitoun O, Hanson I. Organ-specific manifestations of HIV disease in children. Pediatr Clin North Am. 2000;47:109–25. doi: 10.1016/s0031-3955(05)70197-8. [DOI] [PubMed] [Google Scholar]
- 10.Antiretroviral therapy of HIV infection in infants and children in resource-limited settings, towards universal access: Recommendations for a public health approach. WHO 2006 ART of HIV infection in infants and children in RL settings. 2006 [PubMed] [Google Scholar]
- 11.Violari A, Cotton M, Gibb D. Early antiretroviral therapy and mortality among HIV-infected infants. N Engl J Med. 2008;359:2233–44. doi: 10.1056/NEJMoa0800971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Manual on paediatric hiv0 care and treatment for district hospitals. Geneva: World Health Organisation, Department of Child and Adolescent Health and Development (CAH) and HIV/AIDS; 2011. WHO. [Google Scholar]
- 13.Antiretroviral therapy for HIV infection in children: Towards universal access. Recommendations for a public health approach. Geneva: World Health Organisation; 2010. [accessed on October ‥, 2011]. WHO. Available from: http://www.searo.who.int/linkfiles/hiv-aids_artpaediatricguidelines_web.pdf . [PubMed] [Google Scholar]
- 14.Sharland M, Blanche S, Castelli G, Ramos J, Gibb DM. PENTA Steering Committee. Penta guidelines for the use of antiretroviral therapy, 2004. HIV Med. 2004;5(Suppl 2):61–86. doi: 10.1111/j.1468-1293.2004.00227.x. [DOI] [PubMed] [Google Scholar]
- 15.Verweel G, van Rossum AM, Hartwia NG, Wolfs TF, Scterpbier HJ, de Groot R. Treatment with highly active antiretroviral therapy in human immunodeficiency virus type 1-infected children is associated with a sustained effect on growth. Pediatrics. 2002;109:E25. doi: 10.1542/peds.109.2.e25. [DOI] [PubMed] [Google Scholar]
- 16.Puthanakit T, Oberdorfea P, Akarathum N, Wannarit P, Sirisanthana T, Sirisanthana V. Immune reconstitution syndrome after highly active antiretroviral therapy in human immunodeficiency virus infected Thai children. Pediatr Infect Dis J. 2006;25:53–8. doi: 10.1097/01.inf.0000195618.55453.9a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCoig C, Castrejon MM, Castano E, De Suman O, Baez C, Redondo W, et al. Effect of combination antiretroviral therapy on cerebrospinal fluid HIV RNA, HIV resistance, and clinical manifestations of encephalopathy. J Pediatr. 2002;141:36–44. doi: 10.1067/mpd.2002.125007. [DOI] [PubMed] [Google Scholar]
- 18.National AIDS Control Organization. Guidelines for HIV care & treatment in infants & children: 2006. [accessed on August 11, 2011]. Available from: http://www.nacoonline.org/NACO/
- 19.Rwemisisi J, Wolff B, Coutinho a, Grosskurth H, Whitworth J. “What if they ask how I got it?” Dilemmas of disclosing parental HIV status and testing children for HIV in Uganda. Health policy and planning [Internet] 2008 Jan;23(1):36–42. doi: 10.1093/heapol/czm040. [cited 2011 Aug 15]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18156633 . [DOI] [PubMed] [Google Scholar]
- 20.Mallmann SS-A. Building Resilience in Children Affected by HIV / AIDS, Catholic AIDS Action, Namibia, Maskew Miller Longman. 2003 [Google Scholar]
- 21.Ciaranello AL, Park J-E, Ramirez-Avila L, Freedberg K a, Walensky RP, Leroy V. Early infant HIV-1 diagnosis programs in resource-limited settings: opportunities for improved outcomes and more cost-effective interventions. BMC medicine [Internet] 2011 Jan;9(1):59. doi: 10.1186/1741-7015-9-59. [cited 2011 Jul 12]; Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3129310&tool=pmcentrez&rendertype=abstract . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.CDC- Sexually Transmitted diseases (STDs) – Genital HPV infection: Fact sheet. [accessed on September 14, 2011]. Available from STD Facts - Human papillomavirus (HPV) www.cdc.gov/std/hpv/stdfact-hpv.htm. - Cached .
- 23.Mysore Declaration of Appeal for global commitment and action for Pediatric HIV, Unpublished conference proceedings. In: India International Pediatric AIDS Conference. 2009 [Google Scholar]
- 24.Report of Care Support and Treatment (CST) WORKING GROUP FOR National AIDS Control Program (NACP)-IV, Vision document. 2011 [Google Scholar]
- 25.Draft Guidelines for Care of HIV Exposed Infants and Children less than 18 months January 2010. [accessed on October 2011]. Available from: http://upaidscontrol.up.nic.in/pptct , Draft Guidelines on Care of HIV Exposed Infant and Child less than_ 18 Months 25-1-10, pdf .


