Abstract
Countries in Africa and the Middle East bear a heavy burden from cardiovascular disease. The prevalence of coronary heart disease is promoted in turn by a high prevalence of cardiovascular risk factors, particularly smoking, hypertension, dyslipidemia, diabetes, and sedentary lifestyles. Patients in Africa and the Middle East present with myocardial infarction at a younger age, on average, compared with patients elsewhere. The projected future burden of mortality from coronary heart disease in Africa and the Middle East is set to outstrip that observed in other geographical regions. Recent detailed nationally representative epidemiological data are lacking for many countries, and high proportions of transient expatriate workers in countries such as Saudi Arabia and the United Arab Emirates complicate the construction of such datasets. However, the development of national registries in some countries is beginning to reveal the nature of coronary heart disease. Improving lifestyles (reducing calorie intake and increasing physical activity) in patients in the region will be essential, although cultural and environmental barriers will render this difficult. Appropriate prescribing of pharmacologic treatments is essential in the prevention and management of cardiovascular disease. In particular, recent controversies relating to the therapeutic profile of beta-blockers may have reduced their use. The current evidence base suggests that beta-blockers are as effective as other therapies in preventing cardiovascular disease and that concerns relating to their use in hypertension and cardiovascular disease have been overstated.
Keywords: coronary heart disease, beta-blockers, cardiovascular risk factors, cardiovascular disease, heart failure
Introduction
Cardiovascular disease is the principal threat to health in countries in Africa and the Middle East, as elsewhere,1 with increases in the projected burden of mortality set to outstrip that observed in other geographical regions.2 These data, discussed in more detail in the following pages, suggest that the management of ischemic heart disease is suboptimal in some Middle Eastern countries, and that more aggressive management of cardiovascular health could bring substantial improvements to long-term clinical outcomes. Access to health care, prompt and accurate diagnosis, and selection of appropriate therapy are all key determinants of outcome in patients with coronary disease.
The purpose of this review is to summarize the current status of the epidemiology and management of coronary heart disease in countries in the region, and to describe initiatives being designed to address the burden of cardiovascular disease in the future. The review will focus on the role of beta-blockers in particular. Treatment with a beta-blocker is strongly recommended in guidelines for the management of patients with coronary heart disease in a number of settings,3 although a recent focus in guidelines on their potential for adverse metabolic effects may have restricted their use to some extent.4,5
Epidemiology of cardiovascular disease in the region
Middle East as a whole
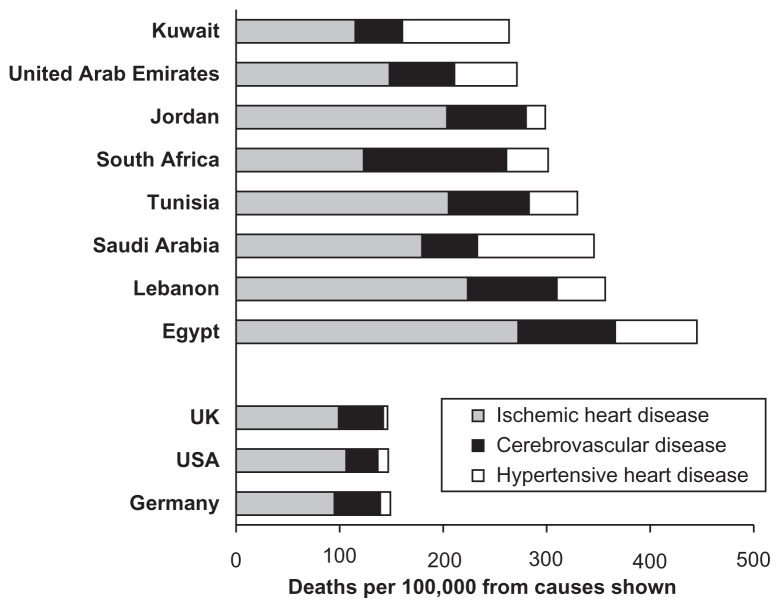
Figure 1 shows age-standardized mortality rates compiled by the World Health Organization (WHO) for some countries in the region.1 There was a marked excess of cardiovascular deaths in most countries from the region compared with data from comparator western countries (UK, Germany and the US), particularly from ischemic heart disease and hypertensive heart disease. Moreover, the INTERHEART study (an international case-control analysis of the risk factors for a first myocardial infarction conducted in more than 15,000 patients presenting with myocardial infarction in 52 countries) showed that the median age at presentation with myocardial infarction was 51 years in the Middle East; this was lower than the median age at presentation in nine other regions, and was 12 years lower than the median age at presentation in Western Europe.6 A projected increase in coronary deaths in the Middle East of 171% between 1990 and 2020 was larger than corresponding values for “established market economies” (46%), India (127%), China (108%), sub-Saharan Africa (144%), and Latin America (144%).2
Figure 1.
Death rates from cardiovascular disease in selected countries in Africa and the Middle East. Drawn from data presented by the World Health Organization.1
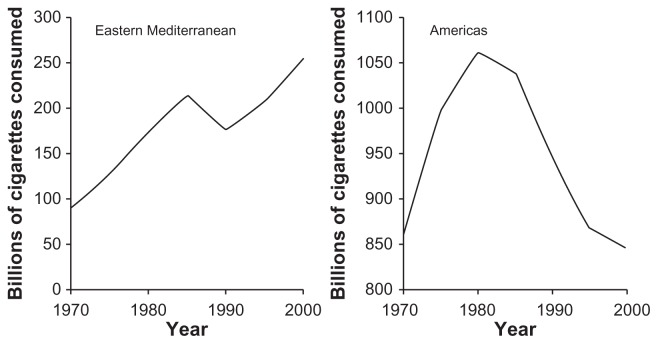
Current data regarding the prevalence of coronary heart disease, and its principal risk factors, are summarized below for a number of countries in the region. Tobacco consumption (including shisha, smoked in a hookah, or water-pipe),7 however, has emerged as a particularly important risk factor in the region and is considered here. Smoking rates have increased in most countries in North Africa and the Middle East, compared with decreasing rates in most western countries, from the latter part of the 1990s onwards (Figure 2).8 Consumption of khat (qat) is also a risk factor for coronary heart disease, particularly in Yemen and the Horn of Africa.9
Figure 2.
Trends in total cigarette consumption in the World Health Organization Eastern Mediterranean and Americas regions. Drawn from data presented by Guindon et al.8
Available data for individual countries in the region
Egypt
The Egyptian National Hypertension Project has provided the two principal sources of information on the epidemiology of coronary heart disease in the region,10–12 in addition to data from the WHO (see Figure 1). This nationally representative survey of 6733 subjects (about half of whom were women) found an adjusted overall prevalence of coronary heart disease of 8.3%. The prevalence of coronary heart disease was somewhat higher in women (8.9%) relative to men (8.0%), but was more clearly associated with an urban versus rural location (8.8% versus 7.2%), and age >50 years versus <50 years (11.1% versus 5.1%). A high prevalence of hypertension in Egypt (26%) was an important driver of adverse cardiovascular outcomes (Table 1).10–12
Table 1.
Hypertension and adverse cardiovascular outcomes in the Egyptian National Hypertension Project10
| Hypertension (n = 1559) | No hypertension (n = 754) | P | |
|---|---|---|---|
| Coronary heart disease (%) | 19.5 | 11.6 | <0.01 |
| Heart failure (%) | 13.3 | 5.8 | <0.0001 |
| Renal failure (%) | 5.3 | 1.9 | 0.0002 |
| Left ventricular hypertrophy (%) | 20 | 5 | <0.001 |
Note: Compiled from data presented by Sharraf et al.10
Lebanon
Age, dysglycemia, hypertension, family history of coronary heart disease, and dyslipidemia predict the development of coronary heart disease in Lebanon as elsewhere.13 Nationally representative data on the epidemiology of coronary heart disease in Lebanon are lacking. However, detailed data on patients presenting with coronary heart disease in Lebanon are available from the Lebanese Interventional Coronary Registry. Coronary angiography remains the principal method for diagnosis of coronary disease and is widely used in Lebanon (only Germany and the US have a higher density of angiography facilities per head of population).14 Cardiovascular risk factors were common in patients presenting for angiography, including hypertension (60%), smoking (50%), diabetes (29%), hypercholesterolemia (29%), and family history of myocardial infarction (26%).15 Prior cardiovascular disease was also common, including angina (61%) and prior myocardial infarction (13%); unstable angina (35%), stable angina (21.2%) and atypical chest pain were the most common symptoms on presentation.15
Interestingly, the ischemic burden remaining following myocardial infarction in patients referred for cardiac imaging (size of the ischemic defect and subsequent risk of mortality) was twice as high in a major referral center in Texas compared with a center in Beirut, Lebanon.16 This difference occurred despite a similar prevalence of cardiovascular risk factors between the centers, suggesting that other factors must have been involved in determining clinical cardiovascular outcomes.
Saudi Arabia
The Gulf Cooperative Council consists of Bahrain, Kuwait, Oman, Qatar, Saudi Arabia, and the United Arab Emirates. The Coronary Artery Disease in Saudi Arabia Study found a high prevalence of hypertension (26%)17 and diabetes (22%),18 together with a prevalence of coronary artery disease of 6%,19 once again higher in the urban setting. Urban location, age, male gender, body mass index, hypertension, smoking, dysglycemia, high serum cholesterol, and triglycerides were significant risk factors for coronary heart disease.
Other Gulf countries
Countries such as Saudi Arabia and the United Arab Emirates have high populations of expatriate workers. Indeed, a recent study has shown that 80% of the United Arab Emirates workforce is of expatriate origin, and that the prevalence of cardiovascular risk factors among ethnic subgroups reflects the prevalence in the country of origin.20 The Gulf-RACE registry has analyzed the epidemiology of coronary heart disease in Bahrain, Kuwait, Oman, Qatar, Yemen, and the United Arab Emirates. A recent analysis of discharge diagnoses found that 39% had ST elevation myocardial infarction (STEMI)/left bundle branch block, 32% had non-STEMI, and 29% had unstable angina.21 Interestingly, the proportion of patients receiving beta-blocker therapy during the first 24 hours of admission was lower in Gulf-RACE relative to GRACE (Global Registry of Acute Coronary Events), either for all patients with an acute coronary syndrome (65% versus 87%, respectively) or ST elevation myocardial infarction (62% versus 87%, respectively). Registry data from Kuwait demonstrated that the proportion of patients with acute myocardial infarction who received beta-blocker therapy was similar to that in the Gulf-RACE population, although the use of beta-blockers appeared to be decreasing (68% in 2004 and 63% in 2007).22
The proportion with either form of myocardial infarction was higher than that in the GRACE,23 while the proportion with unstable angina was lower. The mean age at presentation with myocardial infarction in Gulf-RACE was about 10 years lower than in GRACE (56 versus 66 years). In addition to smoking (see above), diabetes was more prevalent in Gulf residents than in GRACE (41% versus 26%), while lower prevalence values were observed for a diagnosis of hypertension (50% versus 65%) or hyperlipidemia (32% versus 50%). Broadly similar, if slightly lower, rates of previous angina pectoris, myocardial infarction, and percutaneous coronary intervention or coronary artery bypass grafting were observed in the Gulf-RACE versus GRACE population.
Tunisia, Algeria and Morocco
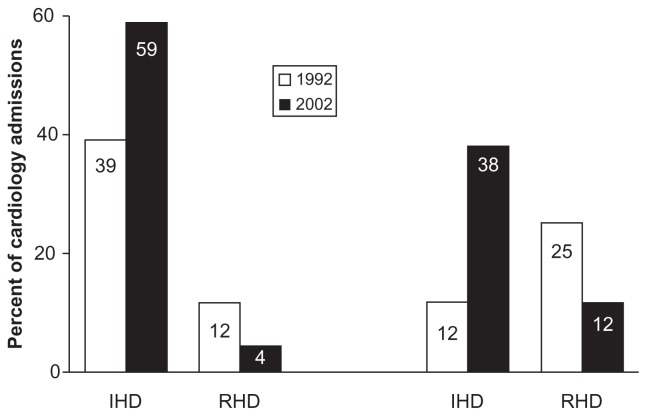
Like other countries in the region, Tunisia is undergoing an epidemiological transition,24 whereby overall life expectancy is increasing, but the risk of ischemic heart disease has also increased (Figure 3).25,26 This shift is accompanied by increasing urbanization; the proportion of Tunisian urban residents increased from 41% in 1966, to 60% in 1990, and to 66% in 2008.27
Figure 3.
Demographic shift in North Africa: increased burden of ischemic heart disease (IHD) and decreasing burden of rheumatic heart disease (RHD) in hospitals in Tunisia.26
Recent data on cardiovascular risk factors in these countries are unavailable, although in 1997, substantial proportions of urban Tunisians were found to have hypertension (16%, defined as blood pressure >160/95 mmHg), diabetes (10%), or obesity (28%, defined as body mass index ≥30 kg/m2).28 A survey in Morocco in 2000 found prevalence values of 34% for hypertension, 7% for diabetes, and 29% for hypercholesterolemia. 29 The TAHINA (Epidemiological Transition And Health Impact In North Africa) project is currently investigating the burden of noncommunicable disease in Tunisia and Algeria, and recent data demonstrate a high prevalence of hypertension (30% and 24%, respectively) and obesity (27% and 21%, respectively).30 Thus, the demographic shift in North Africa is manifesting not only in increasing rates of cardiovascular mortality (particularly from ischemic heart disease), but also provides a reservoir of cardiovascular risk factors that will drive a sharp increase in the future burden of cardiovascular disease.
Other African countries
The high prevalence of human immunodeficiency virus in South Africa, with associated weight loss and early mortality, has distorted the epidemiological transition from communicable to noncommunicable diseases as a major source of morbidity and mortality.31 Heart failure currently appears to be the predominant presentation of cardiovascular disease in South Africa.32 However, a high prevalence of obesity (43%), hypertension (33%), and clustering of risk factors in a survey in the township of Soweto suggests that major problems with coronary heart disease will arise in South Africa in future.33
A recent systematic review has highlighted the need for well designed prospective cohort studies to quantify the burden of cardiovascular disease in sub-Saharan Africa (defined as all of Africa south of the Sahara).34 Although 41 studies (from 11 countries in the region) were identified for evaluation, they were heterogeneous in their design, study populations, durations, and specified outcomes. These studies confirmed the presence of a health transition in sub-Saharan Africa, with cardiovascular risk factors such as hypertension, hypercholesterolemia, and smoking emerging as the most important ones for an emerging burden of cardiovascular disease. Abdominal obesity was found to explain the increased cardiovascular risk associated with urbanization of populations in Benin, consistent with these observations.35 The emergence of obesity as an increasingly important risk factor for hypertension in Sudanese children provides a worrying indication of future trends in developing nations in Africa.36
Implications for management of coronary heart disease in the region
Coronary prevention
There is a need for more recent data on the epidemiology of coronary heart disease in the region, given the projected sharp increases in the prevalence of coronary heart disease in the Middle Eastern countries described earlier. For example, the Egyptian National Hypertension Survey was carried out between 1991 and 1993. Collecting such data is challenging where infrastructure is lacking and populations are often transitory, although the national surveys and registries described above represent real progress.
Nevertheless, it is clear that the prevalence of cardiovascular risk factors in North Africa and the Middle East is high. Thus, intervention to control hypertension and dyslipidemia, and to reduce the risk of developing diabetes is an urgent public health and clinical priority for these countries. Lifestyle intervention (diet and exercise) is effective in reducing a number of cardiovascular risk factors simultaneously.37 Arab populations tend to ingest relatively large amounts of carbohydrates (eg, in the form of dates, figs, or refined sugars) and fats, which is consistent with the high prevalence of obesity.38–40 Sedentary lifestyles are common in all urban populations, although higher levels of sedentary living have been reported for populations of Arab descent relative to other heritages.41,42 Importantly, increased physical activity has been shown to reduce insulin resistance similarly in subjects of Arabian and European descent.43 Education of African/Middle Eastern populations on the benefits of an improved lifestyle will be vital in reducing the future burden of cardiovascular disease. However, achieving improved lifestyles in this population is challenging. For example, 82% of a randomly selected population attending a primary care clinic in Saudi Arabia were physically inactive, and cited a number of barriers to increased physical activity or improved diet.44 Cultural factors are important, and reaching older family members can be especially difficult where younger relatives are expected to run errands, allowing them to remain sedentary at home.
Re-examining the role of beta-blockade
Appropriate prescribing improves outcome for patients with coronary risk factors or with established coronary heart disease. Increased use of evidence-based treatments such as beta-blockers, angiotensin-converting enzyme inhibitors, aspirin, heparin, nitrates, and thrombolytics significantly reduced inhospital mortality rates following admission for acute myocardial infarction in Lebanon in 1996.45
An exhaustive review of the use of pharmacological treatments in patients with coronary heart disease is beyond the scope of this article. However, current guidelines in Europe recommend that beta-blockers have numerous applications in cardiovascular care, not only in the management of hypertension,4 but in patients with established coronary heart disease (Table 2).3,46 Nevertheless, the use of beta-blockers remains controversial in some groups of patients, and there is some evidence that the use of beta-blockers varies within countries in the Middle East. For example, a large survey of the use of various cardiovascular therapies in patients with coronary heart disease in developing countries revealed a lower use of beta-blockers.47 In contrast, data from Lebanon, Saudi Arabia, Israel, and the United Arab Emirates from the REACH (Reduction of Atherothrombosis for Continued Health) registry showed that beta-blockers were prescribed for 61% of high-risk patients with atherothrombotic disease, which was higher compared with angiotensin-converting enzyme inhibitors (58%), diuretics (46%), calcium channel blockers (43%), or angiotensin II receptor blockers (21%).48
Table 2.
Summary of European guideline recommendations on the use of beta-blockers in patients with selected manifestations of established cardiovascular disease
| Indication | Recommended use of beta-blocker therapya | Summary of potential benefit |
|---|---|---|
| Acute MI | All patientsa,b | Limitation of infarct size, ↓ life-threatening cardiac arrhythmias, relief of pain, reduced mortality (including sudden cardiac death) |
| Post-MI | Long-term use in all survivors of MI | 20%–25% improvement in survival through reductions in cardiac mortality, sudden cardiac death and reinfarction |
| NSTEMI-ACS | Use acutely and long-term after the acute phase has passed | Control myocardial ischemia and prevent acute myocardial infarction or reinfarction |
| Stable coronary artery disease | Long-term use for all patients | Control ischemia, prevent infarction, improve survival |
| HF with reduced LV systolic function | Stable, mild-to-severe chronic heart failure (ischemic or non-ischemic) and ↓LV ejection fraction, in NYHA class II–IV; use with ACEI for systolic dysfunction post-MI irrespective of presence/absence of HF symptoms | Long-term reduction in total and cardiovascular mortality, sudden cardiac death and death due to progression of HF |
| HF with preserved LV systolic function | No pharmacologic intervention has been shown to reduce morbidity and mortality in this population; managing cardiac ischemia and hypertension is considered of importance | |
| Supraventricular arrhythmias | Atrial fibrillation, of atrial ectopic activity; use in selected individuals with sinus tachycardia (investigate primary cause) | Slow heart rate, improve control of ventricular rhythm |
| Ventricular arrhythmias | Patients with ventricular arrhythmias related to sympathetic activation (eg, stress-induced arrhythmias, MI, perioperative, heart failure, catecholaminergic polymorphic ventricular tachycardia) | Improve control of ventricular rhythm, including reduced risk of sudden cardiac death |
| Cardiomyopathy | Dilated cardiomyopathy (no specific recommendation for the use of beta-blockers in hypertrophic cardiomyopathy) | Beta-blockers reduce mortality similarly in HF of ischemic or nonischemic etiology |
Notes:
Without contraindications;
Abbreviations: ACEI, angiotensin-converting enzyme inhibitor; ACS, acute coronary syndrome; HF, heart failure; LV, left ventricular; NYHA, New York Heart Association; MI, myocardial infarction; NSTEMI, non-ST elevation myocardial infarction.
The proportions of patients who received a beta-blocker during hospitalization for acute myocardial infarction was 35% in Lebanon, compared with higher proportions for the large, international GRACE registry (78%)49 or the Gulf-RACE registry of Middle-Eastern countries (60% for Gulf-RACE registry [2007], and 75% for the later Gulf RACE-2 registry [2008–2009]).50–53 Within the first Gulf-RACE population, men were more likely than women to receive a beta-blocker at presentation (63% versus 56%, P = 0.006).50 The proportions receiving a beta-blocker at discharge were 77% for the Gulf-RACE registry54 and 80% for Gulf RACE-2.51 Much of the controversy surrounding the use of beta-blockers has centered on their effects on glucose metabolism, with fear of exacerbation of dysglycemia, and the current evidence base suggests that this therapy should be avoided in patients with the metabolic syndrome.4 Meta-analyses have identified a significantly reduced risk of developing diabetes during treatment with an angiotensin-converting enzyme inhibitor versus placebo, while a slightly higher incidence of diabetes was observed with a beta-blocker relative to placebo.55 However, it should be noted, that beta-blockers are equally effective in improving clinical outcomes in hypertensive diabetic or nondiabetic patients.56
A perception of greater effects on clinical outcomes of other cardiovascular therapies, relative to beta-blockers, has been based on the results of further meta-analysis and two outcomes trials (the Losartan Intervention For Endpoint Reduction study and the Anglo-Scandinavian Cardiac Outcomes Trial).57–59 These differences in efficacy may be accounted for by the considerable heterogeneity of trial designs (meta-analyses) or by differences in achieved blood pressure (outcomes trials). Other trials do not reveal a difference in efficacy between beta-blockers and other therapies, and an exhaustive meta-analysis involving 464,000 patients enrolled in 147 randomized trials demonstrated no difference in the risk of coronary heart disease events in patients randomized to beta-blockers or to other therapies.60 Age also did not influence the patient outcome of beta-blocker therapy.52 There is no compelling evidence to suggest that beta-blockers are inferior to other therapies in terms of their potential for cardiovascular protection.
Concerns relating to adverse events with beta-blockers may also have been overstated. Briefing patients on the likelihood of sexual dysfunction increased the rate of reporting of this side effect, irrespective of its actual association with beta-blockade.61 The use of cardioselective beta-blockers may limit the potential for side effects, such as fatigue or sexual dysfunction.
Conclusion
The prevalence of coronary heart disease is high in countries in Africa and the Middle East. A high prevalence of cardiovascular risk factors implies a continuing burden of cardiovascular morbidity and mortality. Improving the lifestyles of patients in the region will be crucial for improving long-term outcomes, although cultural and other barriers will need to be overcome. Appropriate prescribing for the management of cardiovascular risk factors and established cardiovascular disease holds the key to improving outcomes in the short term. While more data on the appropriate use of all cardiovascular therapies in the Middle East would be welcome, data from Gulf-RACE in particular suggest that beta-blocker therapy may be underused in some countries, relative to western populations, despite the proven benefits of this therapy in a broad range of patient subgroups.
Footnotes
Disclosure
This publication is based on presentations and discussion at a meeting funded by Merck Serono. Dr Mike Gwilt (also funded by Merck Serono) assisted the authors in the preparation of the manuscript. WA has received honoraria from AstraZeneca, Sanofi, and Merck Sharpe and Dohme, and has acted as a consultant to AstraZeneca and Pfizer. GM has served as consultant or received speaker fees from Merck Serono, Novartis, Bayer, Servier, Menarini, Recordati, Takeda, Daiichi-Sankyo, and Boehringer Ingelheim. MI has provided additional consultancy services to Merck Serono. MAT, MIK, MSA, and RC declare no additional duality of interest.
References
- 1.World Health Organization. Data and statistics: mortality and health status. [Accessed January 12, 2012]. Available from: http://www.who.int/research/en/
- 2.Okrainec K, Banerjee DK, Eisenberg MJ. Coronary artery disease in the developing world. Am Heart J. 2004;148:7–15. doi: 10.1016/j.ahj.2003.11.027. [DOI] [PubMed] [Google Scholar]
- 3.The Task Force on Beta-Blockers of the European Society of Cardiology. Expert consensus document on b-adrenergic receptor blockers. Eur Heart J. 2004;25:1341–1362. doi: 10.1016/j.ehj.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 4.The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) 2007 Guidelines for the management of arterial hypertension. Eur Heart J. 2007;28:1462–1536. doi: 10.1093/eurheartj/ehm236. [DOI] [PubMed] [Google Scholar]
- 5.National Institute for Health and Clinical Excellence. NICE clinical guideline 127. Hypertension: clinical management of primary hypertension in adults. [Accessed January 12, 2012]. Available from: http://www.nice.org.uk/nicemedia/live/13561/56008/56008.pdf.
- 6.Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 7.Al Suwaidi J, Zubaid M, El-Menyar AA, et al. Prevalence and outcome of cigarette and waterpipe smoking among patients with acute coronary syndrome in six Middle-Eastern countries. Eur J Cardiovasc Prev Rehabil. 2011 Feb 25; doi: 10.1177/1741826710393992. [Epub ahead of print.] [DOI] [PubMed] [Google Scholar]
- 8.Guindon DE, Boisclair G World Health Organization Tobacco Free Initiative. Past, Current and Future Trends in Tobacco use. 2003. [Accessed January 12, 2012]. (HNP discussion paper series; economics of tobacco control paper 6). Available from: http://siteresources.worldbank.org/HEALTHNUTRITIONANDPOPULATION/Resources/281627-1095698140167/Guindon-PastCurrent-whole.pdf.
- 9.Ali WM, Zubaid M, Al-Motarreb A, et al. Association of khat chewing with increased risk of stroke and death in patients presenting with acute coronary syndrome. Mayo Clin Proc. 2010;85:974–980. doi: 10.4065/mcp.2010.0398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharraf YA, Bedir RA, Ibrahim MM. Prevalence and correlates of hypertensive complications in Egyptians. Med J Cairo Univ. 2003;71:747–753. [Google Scholar]
- 11.Ibrahim MM, Rizk H, Appel LJ, et al. Hypertension prevalence, awareness, treatment, and control in Egypt. Results from the Egyptian National Hypertension Project (NHP). NHP Investigative Team. Hypertension. 1995;26:886–890. doi: 10.1161/01.hyp.26.6.886. [DOI] [PubMed] [Google Scholar]
- 12.Ibrahim MM, Appel LJ, Rizk HH, et al. Cardiovascular risk factors in normotensive and hypertensive Egyptians. J Hypertens. 2001;19:1933–1940. doi: 10.1097/00004872-200111000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Abchee A, Puzantian H, Azar ST, et al. Predictors of coronary artery disease in the Lebanese population. Thromb Res. 2006;117:631–637. doi: 10.1016/j.thromres.2005.05.022. [DOI] [PubMed] [Google Scholar]
- 14.Sibai AM, Tohme RA, Saade GA for Lebanese Interventional Coronary Registry (LICOR) Working Group. Coronary angiography in Lebanon: use and overuse. Int J Cardiol. 2008;125:422–424. doi: 10.1016/j.ijcard.2007.01.051. [DOI] [PubMed] [Google Scholar]
- 15.Sibai AM, Tohme RA, Saade GA, et al. The appropriateness of use of coronary angiography in Lebanon: implications for health policy. Health Policy Plan. 2008;23:210–217. doi: 10.1093/heapol/czn005. [DOI] [PubMed] [Google Scholar]
- 16.Dakik HA, Abdallah M, Karrowni W, et al. International variations in the ischemic burden post-acute myocardial infarction: prognostic implications. J Nucl Cardiol. 2009;16:251–254. doi: 10.1007/s12350-008-9023-3. [DOI] [PubMed] [Google Scholar]
- 17.Al-Nozha MM, Abdullah M, Arafah MR, et al. Hypertension in Saudi Arabia. Saudi Med J. 2007;28:77–84. [PubMed] [Google Scholar]
- 18.Al-Nozha MM, Al-Maatouq MA, Al-Mazrou YY, et al. Diabetes mellitus in Saudi Arabia. Saudi Med J. 2004;25:1603–1610. [PubMed] [Google Scholar]
- 19.Al-Nozha MM, Arafah MR, Al-Mazrou YY, et al. Coronary artery disease in Saudi Arabia. Saudi Med J. 2004;25:1165–1171. [PubMed] [Google Scholar]
- 20.Newson-Smith MS. Importing health conditions of expatriate workers into the United Arab Emirates. Asia Pac J Public Health. 2010;22:25S–30S. doi: 10.1177/1010539510373021. [DOI] [PubMed] [Google Scholar]
- 21.Awad HH, Zubaid M, Alsheikh-Ali AA, et al. Comparison of characteristics, management practices, and outcomes of patients between the Global Registry and the Gulf Registry of Acute Coronary Events. Am J Cardiol. 2011;108:1252–1258. doi: 10.1016/j.amjcard.2011.06.040. [DOI] [PubMed] [Google Scholar]
- 22.Al-Jarallah M, Al-Mallah MH, Zubaid M, et al. Trends in the use of evidence-based therapies early in the course of acute myocardial infarction and its influence on short term patient outcomes. Open Cardiovasc Med J. 2011;5:171–178. doi: 10.2174/1874192401105010171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Steg PG, Goldberg RJ, Gore JM, et al. GRACE Investigators. Baseline characteristics, management practices, and in-hospital outcomes of patients hospitalized with acute coronary syndromes in the Global Registry of Acute Coronary Events (GRACE) Am J Cardiol. 2002;90:358–363. doi: 10.1016/s0002-9149(02)02489-x. [DOI] [PubMed] [Google Scholar]
- 24.Omran AR. The epidemiological transition: a theory of the epidemiology of population change. Millbank Mem Fund Q. 1971;75:509–538. [PubMed] [Google Scholar]
- 25.Ghannem H. The challenge of preventing cardiovascular disease in Tunisia. Prev Chronic Dis. 2006;3:A13. [PMC free article] [PubMed] [Google Scholar]
- 26.Ben Romdhane H, Haouala H, Belhani A, et al. Epidemiological transition and health impact of cardiovascular disease in Tunisia. Tunis Med. 2005;83(Suppl 5):1–7. [PubMed] [Google Scholar]
- 27.National Institute for Statistics. [Accessed September 8, 2011]. Available from: http://www.ins.nat.tn.
- 28.Ghannem H, Hadj Fredj A. Prevalence of cardiovascular risk factors in the urban population of Soussa in Tunisia. J Public Health Med. 1997;19:392–396. doi: 10.1093/oxfordjournals.pubmed.a024666. [DOI] [PubMed] [Google Scholar]
- 29.Tazi MA, Abir-Khalil S, Chaouki N, et al. Prevalence of the main cardiovascular risk factors in Morocco: results of a National Survey, 2000. J Hypertens. 2003;21:897–903. doi: 10.1097/00004872-200305000-00013. [DOI] [PubMed] [Google Scholar]
- 30.TAHINA Project website. [Accessed January 12, 2012]. Available from: http://www.ins.nat.tn.
- 31.Albert MA. Heart failure in the urban African enclave of Soweto: a case study of contemporary epidemiological transition in the developing world. Circulation. 2008;118:2323–2325. doi: 10.1161/CIRCULATIONAHA.108.819821. [DOI] [PubMed] [Google Scholar]
- 32.Stewart S, Wilkinson D, Hansen C, et al. Predominance of heart failure in the Heart of Soweto Study cohort: emerging challenges for urban African communities. Circulation. 2008;118:2360–2367. doi: 10.1161/CIRCULATIONAHA.108.786244. [DOI] [PubMed] [Google Scholar]
- 33.Tibazarwa K, Ntyintyane L, Sliwa K, et al. A time bomb of cardiovascular risk factors in South Africa: results from the Heart of Soweto Study “Heart Awareness Days”. Int J Cardiol. 2009;132:233–239. doi: 10.1016/j.ijcard.2007.11.067. [DOI] [PubMed] [Google Scholar]
- 34.Kengne AP, Ntyintyane LM, Mayosi BM. A systematic overview of prospective cohort studies of cardiovascular disease in sub-Saharan Africa. Cardiovasc J Afr. 2011;22:1–10. doi: 10.5830/CVJA-2011-042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ntandou G, Delisle H, Agueh V, Fayomi B. Abdominal obesity explains the positive rural-urban gradient in the prevalence of the metabolic syndrome in Benin, West Africa. Nutr Res. 2009;29:180–189. doi: 10.1016/j.nutres.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 36.Salman Z, Kirk GD, Deboer MD. High rate of obesity-associated hypertension among primary schoolchildren in Sudan. Int J Hypertens. 2010;2011:629492. doi: 10.4061/2011/629492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fourth Joint Task Force of the European Society of Cardiology and other Societies on cardiovascular Disease Prevention in Clinical Practice. European guidelines on cardiovascular disease prevention in clinical practice: executive summary. Eur J Cardiovasc Prev Rehabil. 2007;14(Suppl 2):E1–E40. doi: 10.1097/01.hjr.0000277984.31558.c4. [DOI] [PubMed] [Google Scholar]
- 38.Al-Sarraj T, Saadi H, Volek JS, Fernandez ML. Metabolic syndrome prevalence, dietary intake, and cardiovascular risk profile among over-weight and obese adults 18–50 years old from the United Arab Emirates. Metab Syndr Relat Disord. 2010;8:39–46. doi: 10.1089/met.2009.0035. [DOI] [PubMed] [Google Scholar]
- 39.Al-Rethaiaa AS, Fahmy AE, Al-Shwaiyat NM. Obesity and eating habits among college students in Saudi Arabia: a cross sectional study. Nutr J. 2010;9:39. doi: 10.1186/1475-2891-9-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Galal OM. The nutrition transition in Egypt: obesity, undernutrition and the food consumption context. Public Health Nutr. 2002;5:141–148. doi: 10.1079/PHN2001286. [DOI] [PubMed] [Google Scholar]
- 41.Baron-Epel O, Haviv A, Garty N, Tamir D, Green MS. Who are the sedentary people in Israel? A public health indicator. Isr Med Assoc J. 2005;7:694–699. [PubMed] [Google Scholar]
- 42.Bryan SN, Tremblay MS, Pérez CE, Ardern CI, Katzmarzyk PT. Physical activity and ethnicity: evidence from the Canadian Community Health Survey. Can J Public Health. 2006;97:271–276. doi: 10.1007/BF03405602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Glans F, Eriksson KF, Segerström A, Thorsson O, Wollmer P, Groop L. Evaluation of the effects of exercise on insulin sensitivity in Arabian and Swedish women with type 2 diabetes. Diabetes Res Clin Pract. 2009;85:69–74. doi: 10.1016/j.diabres.2009.04.018. [DOI] [PubMed] [Google Scholar]
- 44.AlQuaiz AM, Tayel SA. Barriers to a healthy lifestyle among patients attending primary care clinics at a university hospital in Riyadh. Ann Saudi Med. 2009;29:30–35. doi: 10.4103/0256-4947.51818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sawaya JI, Jazra C, Farhat F, Alam S, Eid EV, Sabra R. In-hospital mortality after acute myocardial infarction in Lebanon: incidence, associations, and influence of newer treatment regimens. J Med Liban. 2000;48:63–69. French. [PubMed] [Google Scholar]
- 46.The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008. Eur Heart J. 2008;29:2388–2442. doi: 10.1093/eurheartj/ehn309. [DOI] [PubMed] [Google Scholar]
- 47.Mendis S, Abegunde D, Yusuf S, et al. WHO study on prevention of recurrences of myocardial infarction and stroke (WHO-PREMISE) [Accessed January 12, 2012];Bulletin of the World Health Organization. 2005 83:820–828. Available from: http://www.who.int/bulletin/volumes/83/11/820.pdf. [PMC free article] [PubMed] [Google Scholar]
- 48.Alsheikh-Ali AA, Al-Mahmeed W, Porath A, et al. Prevalence and treatment of cardiovascular risk factors in outpatients with atherothrombosis in the Middle East. Heart Asia. 2011:77e81. doi: 10.1136/ha.2010.003145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Abdallah MH, Arnaout S, Karrowni W, Dakik HA. The management of acute myocardial infarction in developing countries. Int J Cardiol. 2006;111:189–194. doi: 10.1016/j.ijcard.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 50.Zubaid M, Rashed WA, Al-Khaja N, et al. Clinical presentation and outcomes of acute coronary syndromes in the gulf registry of acute coronary events (Gulf RACE) Saudi Med J. 2008;29:251–255. [PubMed] [Google Scholar]
- 51.El-Menyar A, Zubaid M, Rashed W, et al. Comparison of men and women with acute coronary syndrome in six Middle Eastern countries. Am J Cardiol. 2009;104:1018–1022. doi: 10.1016/j.amjcard.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 52.Alhabib KF, Hersi A, Alsheikh-Ali AA, et al. Prevalence, predictors, and outcomes of conservative medical management in non-ST-segment elevation acute coronary syndromes in Gulf RACE-2. Angiology. 2011 May 11; doi: 10.1177/0003319711409200. [Epub ahead of print.] [DOI] [PubMed] [Google Scholar]
- 53.Alhabib K, Hersi A, Almahmeed W, et al. Baseline characteristics, management practices, and long-term outcomes of Middle Eastern patients in the Second Gulf Registry of Acute Coronary Events (Gulf RACE-2) Ann Saudi Med. 2012;32:9–18. doi: 10.5144/0256-4947.2012.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zubaid M, Rashed WA, Almahmeed W, et al. Management and outcomes of Middle Eastern patients admitted with acute coronary syndromes in the Gulf Registry of Acute Coronary Events (Gulf RACE) Acta Cardiol. 2009;64:439–446. doi: 10.2143/AC.64.4.2041607. [DOI] [PubMed] [Google Scholar]
- 55.Elliott WJ, Meyer PM. Incident diabetes in clinical trials of antihypertensive drugs: a network meta-analysis. Lancet. 2007;369:201–207. doi: 10.1016/S0140-6736(07)60108-1. [DOI] [PubMed] [Google Scholar]
- 56.Turnbull F, Neal B, Algert C, et al. Effects of different blood pressure-lowering regimens on major cardiovascular events in individuals with and without diabetes mellitus: results of prospectively designed overviews of randomized trials. Arch Intern Med. 2005;165:1410–1419. doi: 10.1001/archinte.165.12.1410. [DOI] [PubMed] [Google Scholar]
- 57.Khan N, McAlister FA. Re-examining the efficacy of beta-blockers for the treatment of hypertension: a meta-analysis. CMAJ. 2006;174:1737–1742. doi: 10.1503/cmaj.060110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dahlöf B, Devereux RB, Kjeldsen SE, et al. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359:995–1003. doi: 10.1016/S0140-6736(02)08089-3. [DOI] [PubMed] [Google Scholar]
- 59.Dahlöf B, Sever PS, Poulter NR, et al. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendoflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomized controlled trial. Lancet. 2005;366:895–906. doi: 10.1016/S0140-6736(05)67185-1. [DOI] [PubMed] [Google Scholar]
- 60.Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. doi: 10.1136/bmj.b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Silvestri A, Galetta P, Cerquetani E, et al. Report of erectile dysfunction after therapy with beta-blockers is related to patient knowledge of side effects and is reversed by placebo. Eur Heart J. 2003;24:1928–1932. doi: 10.1016/j.ehj.2003.08.016. [DOI] [PubMed] [Google Scholar]