Abstract
Aims
To evaluate the effectiveness of management of diabetic foot problems (DFP) by the National University Hospital (NUH) Multidisciplinary Diabetic Foot Team combined with a clinical pathway in terms of average length of stay (ALOS), readmission rates, hospitalisation cost per patient, major reamputation rate, and complication rate.
Methods
939 patients admitted to the Department of Orthopaedic Surgery, NUH, for DFP from 2002 (before team formation) to 2007 (after team formation). It consisted of six cohorts of patients – 61 for 2002, 70 for 2003, 148 for 2004, 180 for 2005, 262 for 2006, and 218 for 2007. All patients were managed by the NUH Multidisciplinary Diabetic Foot Team combined with a clinical pathway. Statistical analyses were carried out for five parameters (ALOS, hospitalisation cost per patient, major amputation rate, readmission rate, and complication rate).
Results
From 2002 to 2007, the ALOS was significantly reduced from 20.36 days to 12.20 days (p=0.0005). Major amputation rate was significantly reduced from 31.15 to 11.01% (p<0.0005). There was also a significant reduction in complication rate from 19.67 to 7.34% (p=0.005). There were reductions in the hospitalisation cost per patient and readmission rate after formation of the multidisciplinary team but they were not statistically significant.
Conclusion
Our evaluation showed that a multidisciplinary team approach combined with the implementation of a clinical pathway in NUH was effective in reducing the ALOS, major amputation rate, and complication rate of DFP.
Keywords: clinical pathways, diabetic foot, length of stay, infection, amputation
The prevalence of diabetes in Singapore was 8.2% in 2004 with the incidence of diabetic foot problems (DFP) in diabetic patients as high as 16.7 and 28.7% in the fifth and sixth decades of life, respectively (1). In Singapore, 700 lower extremity amputations (LEA) were performed annually due to diabetes-related complications (2). The major amputation rate among patients with DFP in the Department of Orthopaedic Surgery, National University Hospital (NUH) was 27.2% between 2005 and 2006 (3). Approximately 15% of diabetic patients develop a foot ulcer during their lifetime and 20% of these ulcers result in LEA (4). As diabetic patients have many comorbidities and complications, multidisciplinary team approaches have been adopted in various countries to manage diabetic foot problems (5–11).
The multidisciplinary diabetic foot team typically comprises an orthopaedic surgeon, a vascular surgeon, infectious diseases specialist, endocrinologist, podiatrist, nurse, case manager, and medical social worker. Other members may include pharmacists for easy access to diabetic medications and dieticians for educating diabetic patients on appropriate diets (10, 12). Certain multidisciplinary teams have included shoemakers and orthotists to make special shoes and orthoses for diabetic patients to prevent foot ulcers and injuries (7, 8, 13, 14).
In May 2003, the NUH Multidisciplinary Team for Diabetic Foot Problems was formed to reduce the major amputation rate, hospitalisation cost, average length of stay (ALOS), readmission rate, and complication rate. This study evaluated the effectiveness of the NUH multidisciplinary team in improving the management of DFP.
National University Hospital (NUH) multidisciplinary team and clinical pathway
Multidisciplinary team
The diabetic foot team is led by an orthopaedic surgeon and members of the team include an endocrinologist; an infectious disease specialist; a vascular surgeon; podiatrists; nurses specialised in wound care, foot care, and foot screening; and a case manager.
Clinical pathway
The diabetic foot team implemented a clinical pathway for patients with DFP. The clinical pathway consists of two parts: Part I – DFP not requiring below knee amputation (BKA) or above knee amputation (AKA), and Part II – DFP requiring BKA or AKA.
On admission, patients with DFP were classified by doctors according to King's College Classification. Patients diagnosed with Stages 3–5 (ulcer, cellulitis, and necrosis, respectively) of the classification system were placed on Part I of the clinical pathway while those diagnosed with Stage 6 (major amputation) were placed on Part II of the clinical pathway.
On the day of admission, a detailed medical history including duration of diabetes, presence of comorbidities, and complications of diabetes was taken. A thorough clinical examination of the patient and the foot including assessment for neuropathy, vasculopathy, and immunopathy was performed by the orthopaedic surgeon. Baseline investigations were performed including full blood count; erythrocyte sedimentation rate; C-reactive protein, urea, and electrolytes; HbA1c; capillary blood glucose; blood culture; and wound culture. The patient was then referred to the podiatrist and other members of the team. Before discharge, nurses educated the patients and their family members on foot care and diabetes care.
The clinical pathway ensured that patients would be seen by all members of the diabetic foot team during hospitalisation and be treated in an efficient multidisciplinary setting. A weekly team ward round is carried out to ensure the patients have optimal glycaemic control, appropriate antibiotic coverage, follow-up on any surgical intervention performed, podiatric care, education on diabetes, foot care and footwear, and an appropriate discharge plan.
Materials and methods
To evaluate the effectiveness of the diabetic foot team approach, six cohorts of patients admitted for DFP to the Department of Orthopaedic Surgery at NUH were studied. They were classified under a diagnosis-related group (DRG) 520: diabetic foot and included yearly cohorts from 2002 (before team formation), 2003 (year of team formation) to 2007 (after team formation). A total of 939 patients were studied: 61 for 2002, 70 for 2003, 148 for 2004, 180 for 2005, 262 for 2006, and 218 for 2007.
All patients diagnosed with DFP at NUH were placed onto the clinical pathway and included in the study. Informed consent was obtained for each participant. Ethical approval was also obtained from the NUH Ethical Board. The ALOS, hospitalisation cost, major amputation rate, readmission rate, and complication rate for 2004, 2005, 2006, and 2007 were compared with those of 2002 (before team formation).
To calculate the hospitalisation cost only direct and tangible costs were taken into account. The bills took into account all charges for treatment including doctors’ professional fees.
The major amputation rate for each year was calculated by taking the proportion of study subjects each year that was placed onto Part II of the clinical pathway – DFP requiring BKA or AKA.
The readmission rate was based on the number of patients readmitted into the hospital within 15 days of the previous discharge date. The complications encountered in our cohort included urinary tract infections, pneumonia, wound infection, and septicaemia.
Statistical analysis
The one-way ANOVA was used to compare the ALOS and mean hospitalisation cost from 2002 to 2007, while the chi-square test was used to compare the amputation rate, readmission rate, and complication rate. Multiple comparisons with Bonferroni adjustment were utilised to compare year 2004 onwards with year 2002.
Results
The age of patients ranged from 21 to 91 years with a mean age being 60.0 years. The ratio of males to females was 1:1. From 2002 to 2007, there were 777 (82.7%) patients recruited into Part I of the clinical pathway and 162 (17.3%) patients recruited into Part II of the clinical pathway.
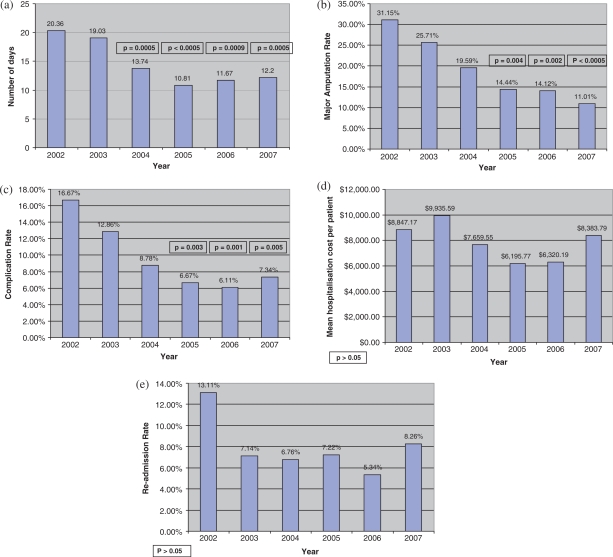
The ALOS in terms of days is 20.36, 19.03, 13.74, 10.81, 11.67, and 12.20 days in year 2002, 2003, 2004, 2005, 2006, and 2007, respectively (Fig. 1a). Multiple comparisons between 2002 (before team formation) and 2004, 2005, 2006, and 2007 show that the ALOS in year 2004, 2005, 2006, and 2007 was significantly lower than that in year 2002 (p=0.0005, p<0.0005, p=0.0009, and p=0.0005, respectively).
Fig. 1.
(a) ALOS over period of study; (b) major amputation rate over period of study; (c) complication rate over period of study; (d) hospitalisation cost per patient over period of study; (e) re-admission rate over period of study.
The major amputation rate was 31.15, 25.71, 19.59, 14.44, 14.12, and 11.01% in year 2002, 2003, 2004, 2005, 2006, and 2007, respectively (Fig. 1b). Multiple comparisons between 2002 (before team formation) and 2004, 2005, 2006, and 2007 showed that the major amputation rate was significantly lower in year 2005, 2006, and 2007 compared with that in year 2002 (p=0.004, p=0.002, and p<0.0005, respectively).
The complication rate was 19.67, 12.86, 8.78, 6.67, 6.11, and 7.34% in year 2002, 2003, 2004, 2005, 2006, and 2007, respectively (Fig. 1c). Multiple comparisons between 2002 (before team formation) and 2004, 2005, 2006, and 2007 showed that the complication rate in year 2005, 2006, and 2007 was significantly lower than that in year 2002 (p=0.003, p=0.001, and p=0.005, respectively).
The mean hospitalisation cost per patient was SGD$8847.17, $9935.59, $7659.55, $6195.77, $6320.19, and $8383.79 in year 2002, 2003, 2004, 2005, 2006, and 2007, respectively (Fig. 1d). Multiple comparisons between 2002 (before team formation) and 2004, 2005, 2006, and 2007 were made. Compared with year 2002, the mean cost in the other years were not significantly different.
The readmission rate was 13.11, 7.14, 6.76, 7.22, 5.34, and 8.26% in year 2002, 2003, 2004, 2005, 2006, and 2007, respectively (Fig. 1e). Multiple comparisons between 2002 (before team formation) and 2004, 2005, 2006, and 2007 were made, however the difference was not significant (p=0.510).
Discussion
This study is a clinical evaluation of the value and effectiveness of a multidisciplinary, team-based approach along with a clinical pathway in managing DFP in the inpatient setting. Our analyses have shown a statistically significant decrease in the ALOS, major amputation rate, and complication rate.
Many teams have established a diabetic foot outpatient clinic to specialise in the treatment of DFP (5, 7–9, 13, 15), allowing continuity of care of the patients after discharge. A weekly diabetic foot clinic allocated solely for integrated management of DFP was created in NUH to further care for the diabetic patients with DFP and to follow-up on their progress, ensuring that their care is optimised even after discharge.
Sakka et al. included an antibiotic regime for treating diabetic foot infections (11). The first line of antibiotics was penicillin-based, the second line was used for patients allergic to penicillin, and the third regime was used for Methycillin Resistant Staphylococcus Aureus (MRSA) positive patients. The NUH protocol also included an antibiotic regime for diabetic foot infections. First-line antibiotics used were amoxicillin and clavulanic acid. The second-line antibiotic used for patients allergic to penicillin was vancomycin. Third-line antibiotics for MRSA and Pseudomonas infections were vancomycin and amikacin/ciprofloxacin, respectively.
Some teams conduct joint ward rounds for inpatient care of diabetic foot problems. Trautner et al. ruled that surgery can only be performed after indication rounds with diabetologists and surgeons (15). After surgery, problem rounds followed. Sakka et al. conducted weekly joint diabetes, vascular, and podiatry ward rounds (11). Such ward rounds allowed immediate discussions between various specialists to decide on the optimal mode of treatment. Similarly, the NUH team used the weekly combined ward rounds for endocrine control, implementing antibiotic regimens, and decision making for surgical intervention or podiatric treatment including footwear recommendations.
Patient education in foot care and diabetes control have also been emphasised in various team approaches (5, 7, 8, 10, 13). In particular, Park and Ahn (10) provided individualised teaching whereby a patient has a session with an endocrinologist, nurse, dietician, pharmacist, and a social worker. In our institute, the team round was the starting point for nurses and podiatrists to provide all patients with individualised education sessions on diabetes care and foot care and education on footwear.
Several studies have found that multidisciplinary management decreases the average length of stay in hospitals (5, 12, 16). Anichini et al. reported a progressive reduction in ALOS for diabetic foot lesions from 19.5 days in 1999 to 5.5 days in 2003 (5). Our study mirrors their findings, showing a significant reduction in ALOS from 20.4 days in 2002 to 12.2 days in 2007.
Rubin et al. with a multidisciplinary team showed a fall in hospitalisation cost by USD$47 per diabetic patient per month (16). On the other hand, Scanlon et al. found no significant difference in total costs between diabetic patients who received team-based care and those who did not (17). In our study, though the hospitalisation cost for patients with DFP decreased in 2004–2007 as compared to that of 2002, the reduction was not statistically significant.
The incidence of amputations has fallen due to multidisciplinary team efforts (5, 6, 8, 13, 18). Driver et al. found that the incidence rate of LEA decreased from 9.9 per 1,000 diabetics to 1.8 over 5 years due to multidisciplinary care (13). Canavan et al. had similar results with the LEA rate decreasing from 564.3 per 100,000 diabetics to 176.0 over 5 years (6). With respect to major amputations, Krishnan et al. (2008) reported a significant 82% reduction in the major amputation incidence from 36.4 per 10,000 diabetics to 6.7 per 10,000 diabetics over an 11-year period (18). Canavan et al. found that the relative risk of a diabetic undergoing a major amputation to that of a non-diabetic person decreased from 35.5 times to 7.7 over 5 years (6). In our study, we also found a significant decrease in major amputation rate from 31 to 11% over 6 years.
There was no report in literature on the effect of a multidisciplinary team approach on the readmission rate and complication rate for patients with diabetic foot problems. In our study, the readmission rate decreased over a 6-year period but the change was not statistically significant. However, we found a significantly lower complication rate in 2005, 2006, and 2007 (after team formation) of about 6.1 to 7.3% as compared to 19.7% in 2002 (before team formation).
In our study, since both the team approach and clinical pathway have been used in an integrated manner, we are unable to evaluate how much each individual component contributed to the clinical outcome.
Conclusion
Our evaluation showed that a multidisciplinary team approach combined with the implementation of a clinical pathway in NUH was effective in reducing the ALOS, major amputation rate, and complication rate of DFP.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
References
- 1.Epidemiology and Disease Control Division. National Health Survey. Singapore: Ministry of Health; 2004. pp. 3–7. [Google Scholar]
- 2.Epidemiology and Disease Control Division. Annual Report. Singapore: Ministry of Health; 2001. p. 35. [Google Scholar]
- 3.Nather A, Chionh SB, Chan YH, Chew JLL, Lin CB, Neo S, et al. Epidemiology of diabetic foot problems and predictive factors for limb loss. J Diabetes Complications. 2008;22:77–82. doi: 10.1016/j.jdiacomp.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 4.Reiber GE. The epidemiology of diabetic foot problems. Diabet Med. 1996;13:S6–S11. [PubMed] [Google Scholar]
- 5.Anichini R, Zechinni F, Cerretini I, Meucci G, Fusilli D, Alviggi L, et al. Improvement of diabetic foot care after the implementation of the International Consensus on the Diabetic Foot (ICDF): results of a 5-year prospective study. Diabetes Res Clin Pract. 2007;75:153–8. doi: 10.1016/j.diabres.2006.05.014. [DOI] [PubMed] [Google Scholar]
- 6.Canavan RJ, Unwin NC, Kelly WF, Connolly VM. Diabetes- and nondiabetes-related lower extremity amputation incidence before and after the introduction of better organised diabetes foot care. Diabetes Care. 2008;31:459–63. doi: 10.2337/dc07-1159. [DOI] [PubMed] [Google Scholar]
- 7.Dargis V, Pantelejeva O, Jonushaite A, Vileikyte L, Boulton AJM. Benefits of multidisciplinary approach in the management of recurrent diabetic foot ulceration in Lithuania. Diabetes Care. 1999;22:1428–31. doi: 10.2337/diacare.22.9.1428. [DOI] [PubMed] [Google Scholar]
- 8.Edmonds ME, Blundell MP, Morris ME, Thomas EM, Cotton LT, Watkins PJ. Improved survival of the diabetic foot: the role of a specialised foot clinic. Q J Med. 1986;60:763–71. [PubMed] [Google Scholar]
- 9.Hedetoft C, Rasmussen A, Fabrin J, Kolendorf K. Four-fold increase in foot ulcers in type 2 diabetic subjects without an increase in major amputations by a multidisciplinary setting. Diabetes Res Clin Pract. 2008;83:353–7. doi: 10.1016/j.diabres.2008.11.025. [DOI] [PubMed] [Google Scholar]
- 10.Park JS, Ahn CW. Educational program for diabetic patients in Korea – multidisciplinary intensive management. Diabetes Res Clin Pract. 2007;77S:S194–8. doi: 10.1016/j.diabres.2007.01.056. [DOI] [PubMed] [Google Scholar]
- 11.Sakka KE, Fassiadis N, Gambhir RPS, Halawa M, Zayed H, Doxford M, et al. An integrated care pathway to save the critically ischaemic diabetic foot. Int J Clin Pract. 2006;60:667–9. doi: 10.1111/j.1368-5031.2006.00953.x. [DOI] [PubMed] [Google Scholar]
- 12.Leichter SB, August GL, Moore W. The business of hospital care of diabetic patients: 2. A new model for inpatient support services. Clinical Diabetes. 2003;21:136–9. [Google Scholar]
- 13.Driver VR, Madsen J., Goodman RA. Reducing amputation rates in patients with diabetes at a military medical centre. Diabetes Care. 2005;28:248–53. doi: 10.2337/diacare.28.2.248. [DOI] [PubMed] [Google Scholar]
- 14.Rose G, Duerkson F, Trepman E, Cheang M, Simonsen JN, Koulack J, et al. Multidisciplinary treatment of diabetic foot ulcers in Canadian aboriginal and non-aboriginal people. Foot Ankle Surg. 2008;14:74–81. doi: 10.1016/j.fas.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 15.Trautner C, Gatcke LM, Haastert B, Giani G, Mauckner P. Reduced incidence of lower-limb amputations in the diabetic population of a German city, 1990–2005. Diabetes Care. 2007;30:2633–7. doi: 10.2337/dc07-0876. [DOI] [PubMed] [Google Scholar]
- 16.Rubin RJ, Dietrich KA, Hawk AD. Clinical and economic impact of implementing a comprehensive diabetes management program in managed care. J Clin Endocrinol Metab. 1998;83:2635–42. doi: 10.1210/jcem.83.8.5075. [DOI] [PubMed] [Google Scholar]
- 17.Scanlon DP, Hollenbeak CS, Beich J, Dyer AM, Gabbay RA, Milstein A. Financial and clinical impact of team-based treatment for medicaid enrollees with diabetes in a federally qualified health center. Diabetes Care. 2008;31:2160–5. doi: 10.2337/dc08-0587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krishnan S, Fowler D, Nash F, Rayman G, Baker N. Reduction in diabetic amputations over 11 years in a defined U.K. population. Diabetes Care. 2008;31:99–101. doi: 10.2337/dc07-1178. [DOI] [PubMed] [Google Scholar]