Abstract
While the incidence of toddlers’ diabetes is soaring, their mainstay insulins were withdrawn, namely the weak 10% or 20% insulin mixtures (WIM), which were injected only once or twice daily. Consequently, toddlers are coerced to use an insulin pump, multi-dose insulin regime (MuDIR), mix or dilute insulins. This paper highlights the difficulties and proposes a simple solution. While an insulin pump is the best available option, it is not readily available for everyone. Mixing insulins is not sufficiently precise in small doses. Although diluting insulin would allow precise dosing and reduce the dose variability secondary to dribbling after injections, it, like insulin mixing, deprives children from using the pen and related child-friendly accessories. In MuDIR, we inject 4-5 small doses of insulin instead of 1-2 daily larger doses of WIM. Thus, on using a half unit (½unit) insulin pen, a dose of 0.5, 1, 1.5 and 2 units are adjusted in steps of 100%, 50%, 33% or 25%; unlike the advisable 5%-20%. This does not easily match the tiny erratic meals of grazing toddlers. Maternal anxiety peaks on watching yo-yoing glycemia. Carers have to accept either persistently high sugar or wild fluctuation. The risks of such poor glycemic pattern are increasingly recognized. Using insulin U20 in a ½unit disposable pen allows deci-unit dosing, with 5%-20% dose-tuning, greater accuracy on delivering small doses and reduction of dose variability from dribbling. Deci-unit dosing may help avoid wide glycemic swings and provide the affordable alternative to insulin pumps for toddlers. Deci-unit pen materializes the Human Rights of Children, a safer and effective treatment.
Keywords: Child; Toddler; Diabetes; Insulin pen; Insulin mixture; Insulin dribbling; Deci-unit dosing; Deci-unit pen, Insulin U20; Glycemic control
TO THE EDITOR
Over the past few decades, standardization of insulin preparations to 100 unit/mL (U100) significantly reduced dosing errors. Insulin U20 was withdrawn with little resistance from pediatric diabetologists[1,2]. Recently, as the incidence of diabetes is soaring worldwide, especially in toddlers, and we became more aware of its complications, toddler-friendly insulin mixtures were discontinued[3,4]. The vulnerable youngsters are left fighting the merciless diabetes with inappropriate [mixing insulins, multiple dose insulin regimes (MuDIR)], cumbersome (diluting insulins) or unaffordable (insulin pump) therapeutic alternatives.
Toddler-friendly insulins were 10% or 20% rapid-intermediate weak insulin mixtures (WIM) that were injected once or twice daily. Doses were adjusted in coarse (15%-20%) or fine (5%-10%) tuning, for steady control. Withdrawal of WIM forced the use of insulin pumps, free insulin mixing or MuDIR.
Free insulin mixing is not a popular option anymore. Recently, diluting U100 insulin to U10 has been successfully studied[5]. This should prove to be a major boon to young diabetic patients and their families[6]. However, mixing or dilution necessitates the use of insulin syringes. The more accurate modern insulin delivery devices, pens, Microfine®, PenMate® and Autocover®, have redefined parents expectations[4]. Now, mixing is rarely acceptable since it is not as accurate or reliable as pens[7]. Mixing and diluting insulin share the inconvenience of carrying the unsightly syringes and needles around, especially on holidays. The highly technical insulin pump is not widely available, particularly in developing countries or at the outset, as it demands complex multidisciplinary care and resources, which are scarce.
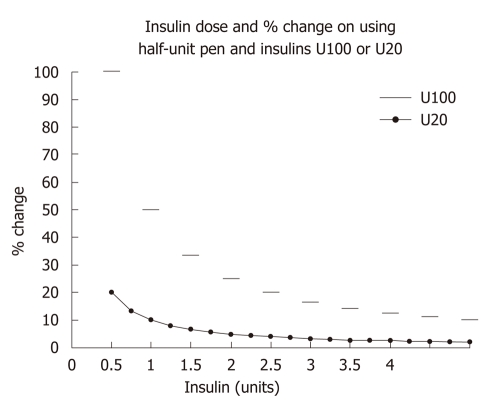
Using multiple 5-20 μL insulin doses is inaccurate[8]. As pens deliver insulin in half unit (½unit) steps, dose tuning becomes impractical (Figure 1), let alone dribbling of the concentrated insulin, U100. For instance, if a dose of ½unit proves insufficient, the next dose is one unit, a 100% increment. One wonders: (1) Would an adult diabetologist advise fine tuning a dose from 5 units to 10 units in one step? (2) Why should a mother accept dose adjusting from ½unit to 1 unit? Or stay at ½unit to avoid “hypos”?
Figure 1.
Percent changes in dosing on using ½unit pen with U100 and U20 insulins. (−−) Abrupt ½unit dosing (U100 current practice): Dose “jumping” is the only way for doses < 3 U. Dose coarse-tuning is available if doses > 3 U, fine-tuning in doses 5 U; (-•-) Smooth deci-unit dosing (U20 proposed alternative).
We propose using deci-unit dosing, i.e., using U20 in ½unit disposable pens, which is compared with ½unit dosing in Figure 1. At low doses, 5 units or less, adjustment could be best achieved by the proposed “0.1 unit dose tuning” rather than by “0.5 unit dose jumping”. The latter force mothers to keep a smaller dose longer and blood sugar higher to avoid “hypos” until the child grows.
With ½unit dosing, only as doses creep up to 3 units does coarse tuning become feasible but fine tuning is unavailable until doses exceed 5 units. Frequently, parents and professionals have to choose between a high “yo-yoing” control and persistently high glycemia. Annersten et al[9] reported significant insulin dribbling from needles [on average 4.7 mg (approximately 0.5 units) in NovoPen3] after 7 s; therefore, they recommended needle holding in the skin for 10 s to minimize dose loss. This practice might add fuel to the fire in a discontent child. Is this avoidable?
We studied the ½unit pens, new HumaPen Luxura HD® (HPL) and NovoPen Junior® (NPJ), by counting the number of drops that get through the tip of 5 mm/31G Microfine needles on slow pressing of the push button in each of the doses 0.5, 1, 1.5, 2, 2.5, 3, 3.5, 4.0, 4.5, 5.0, 10.0 units. Three pens of each type were tested and the experiment for each dose was repeated 10 times so that the number of drops in each dose is averaged from data of 30 experiments for each pen. The HPL dribbled a mean of 0.24 (SD = 0.21) units/drop and the NPJ dribbled 0.33 (0.32) (unpublished data). After insulin injection, a drop or rarely two might dribble from the needle tip. Losing one drop is sizable and variable; it constituted 63%, 30%, 20%, 15%, 12% and 10% of the doses 0.5, 1, 1.5, 2, 2.5 and 3 units, respectively.
Certainly, this highly variable insulin loss with dribbling further complicates diabetes care. Logically, insulin dribbling from U20 insulin would be only one fifth of the standard U100, raising hopes of reducing the 10 s injection hold-in time in needle-phobes.
Assuming no WIM return, the proposed alternative would be rapid insulin of U20. Using U20 in ½unit pen ensures deci-unit dosing and fine tuning. To avoid dispensing errors, the deci-unit pen should be disposable and only prescribed on a named patient basis. Thus, toddlers would continue benefiting from the ever-improving quality convenient pens and their child-friendly accessories.
Surely, there exists a compassionate insulin manufacturer who would love to cater for diabetic youngsters, however small the market is. The disposable deci-unit pen will allow a wider range of safer dosing and deci-unit tuning that is expected to improve accuracy on delivering small insulin doses. It, like diluting insulin, may also reduce insulin loss from dribbling which might ease-up injections due to a shorter holding-in time, besides allowing the continuing use of pens, the affordable alternative to insulin pumps for poor and developing nations.
Footnotes
Peer reviewer: Dr. Joshua J Neumiller, Washington State University, PO Box 1495, Spokane, WA 99210-1495, United States
S- Editor Wu X L- Editor Roemmele A E- Editor Zheng XM
References
- 1.McKinlay I, Farquhar JW. Use of 100 units/ml insulin in treatment of diabetic children. Arch Dis Child. 1976;51:796–798. doi: 10.1136/adc.51.10.796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dorchy H, Ernould C, Loeb H. Standardization of insulin preparations and syringes. Arch Dis Child. 1977;52:336. doi: 10.1136/adc.52.4.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DIAMOND Project Group. Incidence and trends of childhood Type 1 diabetes worldwide 1990-1999. Diabet Med. 2006;23:857–866. doi: 10.1111/j.1464-5491.2006.01925.x. [DOI] [PubMed] [Google Scholar]
- 4.Lteif AN, Schwenk WF. Accuracy of pen injectors versus insulin syringes in children with type 1 diabetes. Diabetes Care. 1999;22:137–140. doi: 10.2337/diacare.22.1.137. [DOI] [PubMed] [Google Scholar]
- 5.Stickelmeyer MP, Graf CJ, Frank BH, Ballard RL, Storms SM. Stability of U-10 and U-50 dilutions of insulin lispro. Diabetes Technol Ther. 2000;2:61–66. doi: 10.1089/152091599316757. [DOI] [PubMed] [Google Scholar]
- 6.Rosenzweig JL. The use of diluted insulin. Diabetes Technol Ther. 2000;2:67–68. doi: 10.1089/152091599316766. [DOI] [PubMed] [Google Scholar]
- 7.Asakura T, Seino H, Nakano R, Muto T, Toraishi K, Sako Y, Kageyama M, Yohkoh N. A comparison of the handling and accuracy of syringe and vial versus prefilled insulin pen (FlexPen) Diabetes Technol Ther. 2009;11:657–661. doi: 10.1089/dia.2009.0006. [DOI] [PubMed] [Google Scholar]
- 8.Gnanalingham MG, Newland P, Smith CP. Accuracy and reproducibility of low dose insulin administration using pen-injectors and syringes. Arch Dis Child. 1998;79:59–62. doi: 10.1136/adc.79.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Annersten M, Frid A. Insulin pens dribble from the tip of the needle after injection. Pract Diab Int. 2000;17:109–111. [Google Scholar]