Abstract
Drug users have very high rates of lifetime exposure to traumatic events, leading to significant psychiatric complications. In spite of the high rate of lifetime exposure, very little is known about the rate of ongoing re-exposure to new traumatic events in drug users. We investigated the rate of traumatic event re-exposure in male and female injecting drug users using syringe exchange services in Baltimore (N = 197). Participants were assessed monthly for traumatic event re-exposure for 16 months. Averaged over the entire follow-up period, 27% of participants were re-exposed to a traumatic event each month and 72% were re-exposed over the 16-month study period. Women were over twice as likely to report any traumatic event re-exposure as men (adjusted odds ratio [AOR] = 2.48; 95% CI = 1.54–3.99), with the specific events of life-threatening illness, death of a loved one, and injury or illness of a loved one being more common in women than men. Traumatic event re-exposure occurs far more often than previously reported, with women injecting drug users at the highest risk. Reassessment of traumatic events may help to identify people most in need and encourage entry into treatment.
Keywords: Traumatic event, Syringe exchange, Gender differences, Longitudinal
Introduction
Over 90% of drug users report having experienced at least one traumatic event in their lifetime, and often many more than one.1,2 Traumatic events cause considerable psychiatric distress and increase risk of subsequent psychiatric problems, including posttraumatic stress disorder3 (PTSD). Indeed, drug users have one of the highest rates of PTSD among any clinical population, with most prevalence estimates ranging over 25%.1,2 PTSD and other psychiatric disorders precipitated by traumatic events convey considerable disease burden to drug users, through the direct effects of psychiatric symptoms and the indirect effects of these symptoms on drug use and response to substance abuse treatment.4,5
In view of the high rates of lifetime traumatic event exposure in drug users, it is remarkable that so little is known about rates of trauma re-exposure in this high-risk population. The few studies using general community-based samples show a 3- to 5-year re-exposure rate of 20-40%, with no gender differences.6,7 The clinical relevance of these data is clear from studies that show that traumatic event re-exposure alone or followed by PTSD increases the risk of further psychiatric impairment, including both PTSD and drug use.6–8
There is good reason to believe that urban drug users experience a considerable amount of traumatic event re-exposure. Drug use, urban living, and low income are each associated with elevated risk of traumatic event exposure and re-exposure.9–12 In addition to these risk factors, past trauma exposure alone, which is present in nearly all drug users, further increases the risk for re-exposure.6,13,14 For example, a history of physical or sexual assault is associated with a 2- to 6-fold increase in risk for re-exposure to another violent event.15 That women are more likely to experience re-exposure to sexual and some other violent assaults than men7 suggests that within drug user populations they might be at higher risk for traumatic event re-exposure.
Nevertheless, only two studies have reported on traumatic event re-exposure rates in drug users. Dansky and colleagues16 provide data to show that 44% of a sample of 34 drug users in outpatient treatment had been re-exposed to a traumatic event over a 6-month follow-up. And more recently, Gil-Rivas et al.17 reported that in a larger sample of 322 drug users finishing residential treatment, 24% were re-exposed in the first 6 months of follow-up, and 29% reported re-exposure in the second 6 months. Both of these studies reported only on drug users in treatment, and few of the study participants used heroin or other injected drugs. Neither study reported rates by gender, leaving the question of gender differences unanswered. Thus, no data are currently available on traumatic event re-exposure in men and women injecting drug users out of treatment.
The present study is the first known prospective study to characterize the frequency and type of traumatic event re-exposure in urban male and female injecting drug users. A convenience sample of new registrants to a community syringe exchange program who were not currently in treatment was recruited and assessed for traumatic event re-exposure each month for 16 months. The purpose of this longitudinal study was to describe the monthly incidence of traumatic event re-exposure, to identify specific high-rate events, and to examine gender differences in re-exposure.
Methods
Participants
Participants were drawn from new registrants of the Baltimore Needle Exchange Program (BNEP), which operates from a recreational vehicle that visits several sites within Baltimore City to provide sterile injection materials, education about infectious disease risk, and referral to substance abuse treatment and other services. BNEP staff referred new registrants to a research van parked next to the BNEP to participate in a study evaluating strategies for increasing substance abuse treatment enrollment. The methodology has been fully described elsewhere.18 Assessments relevant to the present study were added approximately 1 year following the start of the parent study (April 2004); registrants were recruited until March 2007. During this time period, 277 registrants signed informed consent. Participants (n = 80) were excluded from the present study primarily if they either failed to complete the intake battery or had an acute psychiatric or medical problem that required emergent treatment (e.g., intent to harm self or others), leaving 197 study participants. Participants excluded from the present study, but included in the parent study, reported more heroin use at baseline; no other drug use or demographic characteristics differentiated excluded and included participants.18 The study was conducted in accordance with Declaration of Helsinki ethical guidelines and with Western Institutional Review Board review and approval.
Assessments
Baseline Demographics and Drug Use
Demographic information was collected on all participants, including sex, age, race/ethnicity, education level, monthly income, employment status, and HIV status. All participants also completed the Addiction Severity Index19 (ASI) at baseline, a semistructured interview that provided data for the present study on number of days of heroin and cocaine use in the past month.
Posttraumatic Stress Disorder Symptoms
The Modified PTSD Symptom Scale—Revised (MPSS-R)20 was administered in an interview format at intake. The MPSS-R assesses both frequency (range: 0–3) and intensity (range: 0–4) of the 17 PTSD symptoms. A symptom was considered positive if both intensity and frequency were rated at 1 or higher, and participants were considered positive for PTSD when their positive symptom counts met DSM-IV criteria B–D.21
Traumatic Event Exposure
The Traumatic Life Events Questionnaire22 (TLEQ) was administered in an interview format both at intake and at the monthly follow-up interviews for 16 months. The well-validated TLEQ is considered the “gold standard” of traumatic event assessments,23,24 and appears preferable to other measures of traumatic events in drug user populations.1 It contains a comprehensive list of 22 behaviorally descriptive potential traumatic events (and a 23rd category of “other events” with examples) to assess the DSM-IV criterion A(1) for PTSD.21 The following question for adult physical assault is an example of the type of questions on the assessment: “Have you been robbed or been present during a robbery where the robber(s) used or displayed a weapon?” Once an event is endorsed, participants are asked how often the event happened to them and if they had experienced “intense fear, helplessness, or horror” to assess for DSM-IV criterion A(2) for PTSD (reaction to the event); all events reported here met this criterion. In the present study, if an event was endorsed but the answer on A(2) was unclear or missing, the traumatic event was coded as absent; this occurred for only seven events.
Interviewers were instructed to write down any information offered by the participant in response to the “other” question. All “other events” were reviewed for possible recoding. An event was recorded to “no event” if it did not meet the traumatic event (A1) criterion (e.g., “breakup with girlfriend”), and was recorded to another event category if it was more appropriate (e.g., “saw a girl on her bicycle hit by a truck,” recoded to motor vehicle accident). Of 104 “other events,” eight were recorded to “no event,” 24 were recorded to another traumatic event category, and 72 events remained in the “other event” category. The most common “other event” was seeing a dead or severely injured person.
For monthly follow-up administration, the TLEQ was modified slightly to limit reports to only those traumatic events experienced in the past month by prefacing each question with the phrase “In the past month….” Combat and events that occurred in childhood only (i.e., child physical assault, witness family violence, child sexual assault, young adult sexual assault) were removed from the follow-up interviews. As with the lifetime administration, any unclear or missing response to the A(2) criterion question was assumed to be negative; this occurred for 20 events. Of the 80 “other events” reported in monthly follow-ups, 25 were recorded to “no event,” 25 were recorded to another traumatic event category, and 30 remained “other events.” The most commonly endorsed “other events” at follow-up were seeing a dead or severely injured person and a physical assault by a family member.
To simplify presentation of the results, a few similar types of traumatic events were collapsed in the results for both lifetime and monthly interviews. Motor vehicle accidents and other accidents were grouped together as “accident.” Robbery with a weapon and adult physical assault without a weapon were categorized as “adult physical assault.” All sexual assaults before age 13 (including assaults by a peer or by someone at least 5 years older) were grouped into “childhood sexual assault.” Stalking and unwanted sexual attention (other than sexual assault) were categorized as “other threats.” Finally, “other events” included all responses that did not fit into other categories, as well as the specific TLEQ questions about miscarriage and abortion. The remaining categories reported here are responses to single items.
Procedure
Staff formally trained in the delivery of semistructured interviews25 administered the demographics form, ASI, MPSS-R and TLEQ at the beginning of the study. Following completion of the baseline assessment phase, participants were randomly assigned to one of three study conditions evaluating strategies for enhancing motivation to enroll in substance abuse treatment.18 Over the course of the study, participants were scheduled to attend monthly follow-up visits to complete the TLEQ and other parent study assessments, whether or not they had entered treatment.
Statistical Analyses
Analyses were conducted using IBM SPSS Statistics 18.0 (SPSS Inc., Chicago, IL). Comparisons between subgroups were made using independent t-tests for continuous variables (with degree of freedom correction if indicated) and χ2 tests for categorical variables. Subgroups tested included intake only vs. follow-up attenders and men vs. women. Male and female participants were compared on the likelihood of traumatic event re-exposure (any event and individual events) using generalized estimating equations26 (GEE), specifying a binomial distribution for presence or absence of traumatic event in each of 16 months. Initial analyses were conducted without covariates. Due to baseline gender differences on age, and research demonstrating associations among age, race, and traumatic event exposure,27,28 subsequent analyses were adjusted for the time-invariant covariates age (years) and race (minority vs. white). We theorized that being in substance abuse treatment might reduce traumatic event re-exposure, so results were also adjusted for days in treatment each month (i.e., time-varying covariate). GEE results are presented with both unadjusted and adjusted odds ratios (OR and AOR) with 95% confidence intervals (CI).
Missing Data
To minimize missing data in this difficult-to-reach population, participants who missed one or more follow-up visits were asked retroactively about their experiences at the next attended visit. Of those completing the intake (N = 197), 162 (82%) attended at least one follow-up and 115 completed all follow-ups (71% of the follow-up sample). The median number of follow-ups attended in the follow-up sample (n = 162) was 16 while the average number of follow-ups attended was 13.22 (SEM = 0.40). The follow-up sample (n = 161; one was missing ASI data) reported more days of cocaine use at baseline than those not attending follow-up (n = 35; M [SEM] = 16.11 [0.92] vs. 11.63 [1.84]; t[194] = −2.08; p = 0.039). There were no significant differences in follow-up attendance with regard to other drug use or demographic characteristics. To rule out the possibility that any potential gender difference in re-exposure would be related to differential attendance to follow-ups, we compared the number of follow-ups for men and women within the follow-up sample. Using a simple t-test, it appears that women (n = 50) attended marginally more follow-ups than men ([n = 112]; 14.11 [0.57] vs. 12.80 [5.12]; t[123.65] = −1.74; p = 0.085). Because the distribution of this count variable is highly skewed, we then conducted a negative binomial regression. No relationship of gender on follow-up attendance was observed in this analysis (B [SE] = −0.10 [0.18]; 95% CI [−0.45 to −0.25]; p = 0.573).
Results
Sample Description
All participants were opioid dependent and none were in substance abuse treatment at intake. The intake sample was an average of 41 years old, had a greater proportion of men (72%), and most self-identified as Black (67% Black, 27% White, and 6% other [primarily multiracial]). Although 62% had at least a high school education, only 19% were employed and monthly income was low (median = $892). Participants had used heroin an average of 28 days and cocaine 15 days in the past month; approximately 8% were HIV + by self-report. Men were older than women (M [SEM] = 42.10 [0.73] vs. 39.21 [0.90]; t[129.54] = 2.488; p = 0.014), and more likely to be employed (23% vs. 9%; χ2(1) = 5.40; p = 0.02). No other significant gender differences on demographic variables were observed.
Lifetime History of Traumatic Events and Baseline PTSD
Over ninety percent of participants reported at least one qualifying lifetime traumatic event. Table 1 shows traumatic events reported by the sample, presented by gender. Exposure to violence was the norm, with three-quarters reporting a history of physical assault and nearly half of all participants reporting that they witnessed a physical assault. Men and women were equally likely to report these violent events. As expected, women were more likely than men to report sexual assault at any age, intimate partner violence, and threats including stalking and sexual harassment. Women were also more likely to report a history of life-threatening illness, illness or injury to a loved one, witnessing family violence, and “other” events.
Table 1.
Lifetime traumatic event exposure of syringe exchange participants measured at intake, compared between genders
| Event | Men (n = 141)a % (n) | Women (n = 56) % (n) | pb |
|---|---|---|---|
| Natural disaster | 13 (18) | 13 (7) | 0.960 |
| Accident | 38 (53) | 48 (27) | 0.171 |
| Death of loved one | 53 (74) | 64 (36) | 0.132 |
| Illness/injury of loved one | 28 (40) | 45 (25) | 0.028 |
| Life-threatening illness | 20 (28) | 41 (23) | 0.002 |
| Combat | 4 (6) | 0 | 0.186 |
| Adult physical assault | 77 (108) | 71 (40) | 0.449 |
| Witness assault | 41 (58) | 46 (26) | 0.498 |
| Threatened with assault | 29 (41) | 32 (18) | 0.672 |
| Witness family violence | 38 (53) | 55 (31) | 0.023 |
| Child physical assault | 24 (34) | 32 (18) | 0.249 |
| Intimate partner violence | 9 (13) | 66 (37) | <0.001 |
| Child sexual assault | 9 (12) | 32 (18) | <0.001 |
| Young adult sexual assault | 4 (5) | 21 (12) | <0.001 |
| Adult sexual assault | 1 (2) | 25 (14) | <0.001 |
| Other threats | 7 (10) | 41 (23) | <0.001 |
| Other events | 40 (56) | 64 (36) | 0.002 |
| Any traumatic event | 92 (130) | 91 (51) | 0.778 |
aOne participant is missing data for “other events”
bAnalyses were conducted using χ2 or Fisher’s exact test (i.e., combat, any event)
Current PTSD was reported by 25% of the sample (n = 48; three participants were missing MPSS-R data). Women were much more likely to report current PTSD at baseline than men (43% vs. 17%; χ2(1) = 13.87; p < 0.001).
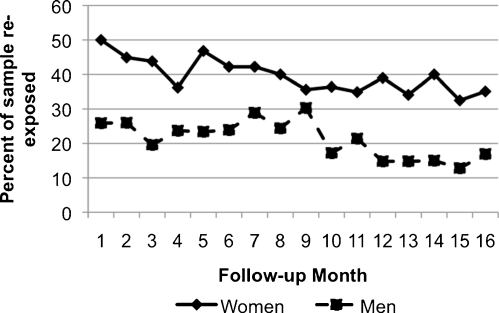
Monthly Re-exposure to Any Traumatic Event
When averaged over the entire follow-up period, 27% of participants were re-exposed to a traumatic event each month. Figure 1 presents the proportion of men and women attending each of the 16 monthly follow-ups who endorsed any traumatic event re-exposure in that month. Women were over twice as likely to be re-exposed as men (OR = 2.40 [1.52–3.79]). Adjusting for age, race, and days in treatment did not significantly alter the results (AOR = 2.46 [1.54–3.94]) and the covariates were nonsignificant (age: 1.01 [0.98–1.04]; race: 0.88 [0.51–1.49]; days in treatment: 1.00 [0.99–1.00]). Visual inspection of the results suggested that traumatic event re-exposure decreased over time in both genders, so the result was reanalyzed including time in the model. The effect of gender was essentially unchanged (AOR = 2.48 [1.54–3.99]) although the time covariate was significant, showing that each month decreased the likelihood of re-exposure by about 4% (OR = 0.96 ([0.94–0.98]). All subsequent analyses included time as a covariate. At the 6-month follow-up, 60% of the sample had reported at least one traumatic event re-exposure, including 78% of women and 52% of men. By 16 months, the overall cumulative exposure rate had increased to 72%; 86% of women and 66% of men had at least one trauma re-exposure.
FIGURE 1.
Gender differences in traumatic event re-exposure.
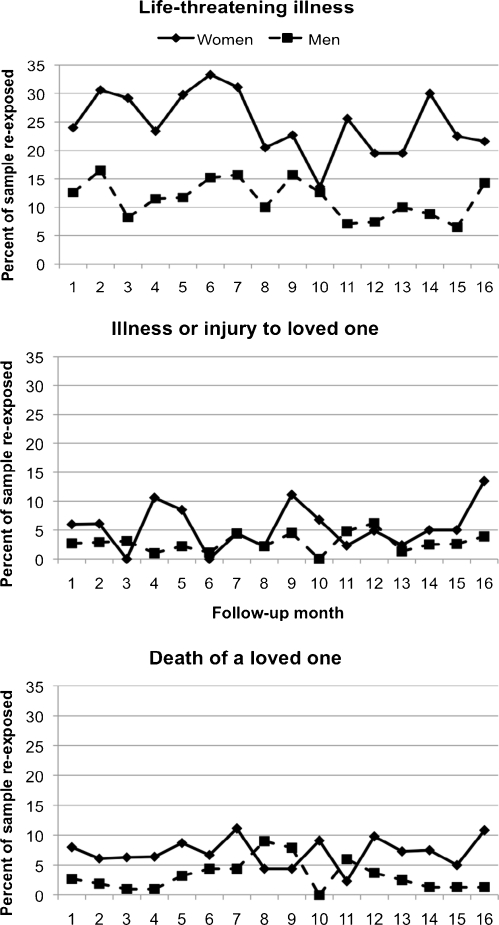
Individual Traumatic Event Re-exposure
To avoid inflating Type I error with multiple comparisons, men and women were compared on endorsement for individual events that occurred in at least 3% of the sample, averaged over the entire follow-up period. This criterion resulted in sample comparisons on rates of re-exposure to the following events: life-threatening illness, death of loved one, injury/illness of loved one, adult physical assault, and witnessing physical assault. Figure 2 presents the three most common events, all of which were more common in women than men. Life-threatening illness was over twice as likely in women than in men (OR = 2.64 [1.39–5.00]; AOR = 2.70 [1.39–5.24]), as was death of a loved one (OR = 2.26 [1.30–3.94]; AOR = 2.29 [1.30–4.01]) and illness/injury to a loved one (OR = 2.09 [1.08–4.03]; AOR = 2.38 [1.20–4.72]). No gender differences were found for likelihood of re-exposure to adult physical assault (OR = 0.75 [0.36–1.55]; AOR = 0.83 [0.41–1.71]) or witnessing physical assault (OR = 1.47 [0.76–2.82]; AOR = 1.34 [0.71–2.51]).
FIGURE 2.
Gender differences in re-exposure to specific traumatic events.
Discussion
High Rates of Traumatic Event Re-exposure
This first known prospective analysis of traumatic event re-exposure in injecting drug users found very high overall rates of re-exposure, with a substantially higher risk for women. One out of every four injecting drug users experienced a new traumatic event re-exposure each month. The present data is consistent with the two previous studies of other populations of drug users that observed a 24–44% re-exposure incidence within 6 months.16,17 Nevertheless, the 6- and 16-month cumulative re-exposure rates were much higher in the current study. That almost three-quarters of the syringe exchange sample were re-exposed to at least one traumatic event demonstrates that these rates cannot be attributed to the influence of a small high-risk group of individuals. The poverty-level income reported by drug users in this study, and living in a city with one of the highest violent crime rates in the country (i.e., Baltimore),29 likely contributed to their increased re-exposure risk. In fact, the high rates of lifetime exposure in this sample are similar to other studies of impoverished, urban community samples, supporting the validity of the present data.30
It should be noted that while traumatic re-exposure was reported across all of the 16 monthly assessments, overall rates of exposure decreased over time, with re-exposure risk dropping similarly for men and women by 6% and 10% per month, respectively. This finding may be due to selective study attrition: it is possible that those subjects who are engaged in violence dropped out of the study prematurely, thereby prospectively lowering rates of reported re-exposure in the remaining sample. An alternative speculation is that participation in a community syringe exchange program supports individuals making healthy behavior changes that lead to reduced exposure to dangerous situations over time, although treatment engagement itself did not appear to affect re-exposure rates.
Gender and Re-exposure to Violence and Other Traumatic Events
Overall, women injecting drug users were more than twice as likely to report traumatic event re-exposure as men, placing them at much higher risk of psychiatric sequelae, including PTSD.31 PTSD was more common in women at baseline, and given that both being female and having a prior episode of PTSD increases the risk of developing PTSD in response to a new traumatic event, higher rates of re-exposure for women are likely to translate to much greater risk of PTSD in women injecting drug users.6,9 Men and women were equally likely to report being physically assaulted or witnessing a physical assault, which translates to an exceptionally high rate of violence for women since community studies generally show that men are at considerably higher risk for violence than women.32 Male and female injecting drug users may place themselves at increased risk for traumatic events via criminal activity and exposure to dangerous people and situations;33,34 the higher rates of experiencing and witnessing physical assaults (compared to community samples) support this interpretation.
Women were more likely than men to report experiencing a life-threatening illness during the course of the study. While injecting drug users as a population are more prone to serious illnesses than the general population,35 the reason for the gender finding is unclear. Women are generally more likely to seek medical care than men,36 which suggests that they may also be more attuned to their physical health and more likely to identify severe illness correctly. Women were also more likely to report re-exposure to death or illness of a loved one in the present study, a finding that diverges from community surveys showing that men are more at risk for these categories of trauma.9,11,32 Women drug users tend to maintain larger social networks than men over time,37 which may lead to women being more likely to learn of events happening to others in their network. Women were also more likely than men to report lifetime exposure to both of these traumatic events at baseline, suggesting that these gender differences may be lifelong.
Study Limitations
The importance of these results is moderated somewhat by imperfect generalizability to other drug user populations in other environments. While syringe exchange registrants often report higher drug use severity than other populations of drug users,38 they also demonstrate an interest in healthier behavior change (i.e., sterile injecting) despite continued drug use. The present sample was also recruited for a study of methods to increase treatment-seeking, so participants may have had more interest in treatment than other samples of out-of-treatment drug users. Finally, the majority of participants were impoverished and lived in Baltimore City, which has one of the highest rates of violent crime of all large metropolitan areas, likely increasing their risk of traumatic event re-exposure over injecting drug users with higher socioeconomic status or who live in less dangerous cities.
Implications of Traumatic Event Re-exposure
These results highlight the important and under-recognized problem of ongoing traumatic event re-exposure in drug users. Traumatic events, by their very nature, tax internal resources like coping skills as well as external resources, including money and social support.3 Drug users routinely experience deficits in these areas and so may be even more vulnerable to the impact of trauma than the general population. In addition, the well-known relationship between even a single traumatic event and the development of PTSD or other psychiatric problems39 is strengthened following multiple occurrences of trauma, particularly physical assaults.8,40 For drug users who are not in treatment, the occurrence of new traumatic events is likely to destabilize progress toward healthy behavior change by intensifying psychiatric and drug use severity,8,17,41 which, in turn, increases risk of further traumatic event exposure. Future studies should assess the mental health outcomes related to these very high re-exposure rates, with particular attention to the greater risk for women injecting drug users. Reassessment of new traumatic events on an ongoing basis may help identify those drug users most in need of treatment and thereby improve their prognosis.
Acknowledgements
This research was supported by NIH-NIDA grants K23DA015739 (Peirce) and R01DA012347 (Kidorf).
References
- 1.Peirce JM, Burke CK, Stoller KB, Neufeld KJ, Brooner RK. Assessing traumatic event exposure: comparing the Traumatic Life Events Questionnaire to the Structured Clinical Interview for DSM-IV. Psychol Assess. 2009;21(2):210–8. doi: 10.1037/a0015578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reynolds M, Mezey G, Chapman M, Wheeler M, Drummond C, Baldacchino A. Co-morbid post-traumatic stress disorder in a substance misusing clinical population. Drug Alcohol Depend. 2005;77(3):251–8. doi: 10.1016/j.drugalcdep.2004.08.017. [DOI] [PubMed] [Google Scholar]
- 3.Hobfoll SE, Johnson RJ, Ennis N, Jackson AP. Resource loss, resource gain, and emotional outcomes among inner city women. J Pers Soc Psychol. 2003;84(3):632–43. doi: 10.1037/0022-3514.84.3.632. [DOI] [PubMed] [Google Scholar]
- 4.Hien DA, Nunes E, Levin FR, Fraser D. Posttraumatic stress disorder and short-term outcome in early methadone treatment. J Subst Abuse Treat. 2000;19(1):31–7. doi: 10.1016/S0740-5472(99)00088-4. [DOI] [PubMed] [Google Scholar]
- 5.Read JP, Brown PJ, Kahler CW. Substance use and posttraumatic stress disorders: symptom interplay and effects on outcome. Addict Behav. 2004;29(8):1665–72. doi: 10.1016/j.addbeh.2004.02.061. [DOI] [PubMed] [Google Scholar]
- 6.Breslau N, Peterson EL, Schultz LR. A second look at prior trauma and the posttraumatic stress disorder effects of subsequent trauma: a prospective epidemiological study. Arch Gen Psychiatry. 2008;65(4):431–7. doi: 10.1001/archpsyc.65.4.431. [DOI] [PubMed] [Google Scholar]
- 7.Stein MB, Höfler M, Perkonigg A, et al. Patterns of incidence and psychiatric risk factors for traumatic events. Int J Methods Psychiatr Res. 2002;11(4):143–53. doi: 10.1002/mpr.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hedtke KA, Ruggiero KJ, Fitzgerald MM, et al. A longitudinal investigation of interpersonal violence in relation to mental health and substance use. J Consult Clin Psychol. 2008;76(4):633–47. doi: 10.1037/0022-006X.76.4.633. [DOI] [PubMed] [Google Scholar]
- 9.Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998;55(7):626–32. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- 10.Breslau N, Lucia VC, Alvarado GF. Intelligence and other predisposing factors in exposure to trauma and posttraumatic stress disorder: a follow-up study at age 17 years. Arch Gen Psychiatry. 2006;63(11):1238–45. doi: 10.1001/archpsyc.63.11.1238. [DOI] [PubMed] [Google Scholar]
- 11.Breslau N, Wilcox HC, Storr CL, Lucia VC, Anthony JC. Trauma exposure and posttraumatic stress disorder: a study of youths in urban America. J Urban Health. 2004;81(4):530–44. doi: 10.1093/jurban/jth138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gillespie CF, Bradley B, Mercer K, et al. Trauma exposure and stress-related disorders in inner city primary care patients. Gen Hosp Psychiatry. 2009;31(6):505–14. doi: 10.1016/j.genhosppsych.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Breslau N, Davis GC, Andreski P. Risk factors for PTSD-related traumatic events: a prospective analysis. Am J Psychiatry. 1995;152(4):529–35. doi: 10.1176/ajp.152.4.529. [DOI] [PubMed] [Google Scholar]
- 14.Orcutt HK, Erickson DJ, Wolfe J. A prospective analysis of trauma exposure: the mediating role of PTSD symptomatology. J Trauma Stress. 2002;15(3):259–66. doi: 10.1023/A:1015215630493. [DOI] [PubMed] [Google Scholar]
- 15.Acierno R, Resnick H, Kilpatrick DG, Saunders B, Best CL. Risk factors for rape, physical assault, and posttraumatic stress disorder in women: examination of differential multivariate relationships. J Anxiety Disord. 1999;13(6):541–63. doi: 10.1016/S0887-6185(99)00030-4. [DOI] [PubMed] [Google Scholar]
- 16.Dansky BS, Brady KT, Saladin ME. Untreated symptoms of PTSD among cocaine-dependent individuals. Changes over time. J Subst Abuse Treat. 1998;15(6):499–504. doi: 10.1016/S0740-5472(97)00293-6. [DOI] [PubMed] [Google Scholar]
- 17.Gil-Rivas V, Prause J, Grella CE. Substance use after residential treatment among individuals with co-occurring disorders: the role of anxiety/depressive symptoms and trauma exposure. Psychol Addict Behav. 2009;23(2):303–14. doi: 10.1037/a0015355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kidorf M, King VL, Neufeld K, Peirce J, Kolodner K, Brooner RK. Improving substance abuse treatment enrollment in community syringe exchangers. Addiction. 2009;104(5):786–95. doi: 10.1111/j.1360-0443.2009.02560.x. [DOI] [PubMed] [Google Scholar]
- 19.McLellan T, Kushner H, Metzger D, et al. The fifth edition of the Addiction Severity Index. J Subst Abuse Treat. 1992;9(3):199–213. doi: 10.1016/0740-5472(92)90062-S. [DOI] [PubMed] [Google Scholar]
- 20.Falsetti SA, Resnick HS, Resick PA, Kilpatrick DG. The Modified PTSD Symptom Scale: a brief self-report measure of posttraumatic stress disorder. Behav Ther. 1993;16(3):161–2. [Google Scholar]
- 21.Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994: 427–428.
- 22.Kubany ES, Haynes SN, Leisen MB, et al. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: the Traumatic Life Events Questionnaire. Psychol Assess. 2000;12(2):210–24. doi: 10.1037/1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- 23.Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. 2004;11(4):330–41. doi: 10.1177/1073191104269954. [DOI] [PubMed] [Google Scholar]
- 24.Weathers FW, Keane TM. The Criterion A problem revisited: controversies and challenges in defining and measuring psychological trauma. J Trauma Stress. 2007;20(2):107–21. doi: 10.1002/jts.20210. [DOI] [PubMed] [Google Scholar]
- 25.Brooner RK, King VL, Kidorf M, Schmidt CW, Jr, Bigelow GE. Psychiatric and substance use comorbidity among treatment-seeking opioid abusers. Arch Gen Psychiatry. 1997;54(1):71–80. doi: 10.1001/archpsyc.1997.01830130077015. [DOI] [PubMed] [Google Scholar]
- 26.Zeger SL, Liang KY, Albert PS. Models for longitudinal data: a generalized estimating equation approach. Biometrics. 1988;44(4):1049–60. doi: 10.2307/2531734. [DOI] [PubMed] [Google Scholar]
- 27.Breslau N. The epidemiology of trauma, PTSD, and other posttrauma disorders. Trauma Violence Abuse. 2009;10(3):198–210. doi: 10.1177/1524838009334448. [DOI] [PubMed] [Google Scholar]
- 28.Roberts AL, Gilman SE, Breslau J, Breslau N, Koenen KC. Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychol Med. 2011;41(1):71–83. doi: 10.1017/S0033291710000401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.U.S. Department of Justice – Federal Bureau of Investigation. Table 6. Crime in the United States by Metropolitan Statistical Area. Crime in the United States, 2008. 2009. Available at: http://www.fbi.gov/ucr/cius2008/data/table_06.html. Accessed on: April 23, 2010.
- 30.Alim TN, Graves E, Mellman TA, et al. Trauma exposure, posttraumatic stress disorder and depression in an African-American primary care population. J Natl Med Assoc. 2006;98(10):1630–6. [PMC free article] [PubMed] [Google Scholar]
- 31.Kidorf M, Disney ER, King VL, Neufeld K, Beilenson PL, Brooner RK. Prevalence of psychiatric and substance use disorders in opioid abusers in a community syringe exchange program. Drug Alcohol Depend. 2004;74(2):115–22. doi: 10.1016/j.drugalcdep.2003.11.014. [DOI] [PubMed] [Google Scholar]
- 32.Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: a quantitative review of 25 years of research. Psychol Bull. 2006;132(6):959–92. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- 33.Darke S, Torok M, Kaye S, Ross J, McKetin R. Comparative rates of violent crime among regular methamphetamine and opioid users: offending and victimization. Addiction. 2010;105(5):916–9. doi: 10.1111/j.1360-0443.2009.02872.x. [DOI] [PubMed] [Google Scholar]
- 34.Chilcoat HD, Breslau N. Investigations of causal pathways between PTSD and drug use disorders. Addict Behav. 1998;23(6):827–40. doi: 10.1016/S0306-4603(98)00069-0. [DOI] [PubMed] [Google Scholar]
- 35.Cherubin CE, Sapira JD. The medical complications of drug addiction and the medical assessment of the intravenous drug user: 25 years later. Ann Intern Med. 1993;119(10):1017–28. doi: 10.7326/0003-4819-119-10-199311150-00009. [DOI] [PubMed] [Google Scholar]
- 36.Verbrugge LM. The twain meet: empirical explanations of sex differences in health and mortality. J Health Soc Behav. 1989;30(3):282–304. doi: 10.2307/2136961. [DOI] [PubMed] [Google Scholar]
- 37.Timko C, Finney JW, Moos RH. The 8-year course of alcohol abuse: gender differences in social context and coping. Alcohol Clin Exp Res. 2005;29(4):612–21. doi: 10.1097/01.ALC.0000158832.07705.22. [DOI] [PubMed] [Google Scholar]
- 38.Neufeld K, King V, Peirce J, Kolodner K, Brooner R, Kidorf M. A comparison of 1-year substance abuse treatment outcomes in community syringe exchange participants versus other referrals. Drug Alcohol Depend. 2008;97(1–2):122–9. doi: 10.1016/j.drugalcdep.2008.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McFarlane AC. Posttraumatic stress disorder: a model of the longitudinal course and the role of risk factors. J Clin Psychiatry. 2000;61(S5):15–20. [PubMed] [Google Scholar]
- 40.Breslau N, Anthony JC. Gender differences in the sensitivity to posttraumatic stress disorder: an epidemiological study of urban young adults. J Abnorm Psychol. 2007;116(3):607–11. doi: 10.1037/0021-843X.116.3.607. [DOI] [PubMed] [Google Scholar]
- 41.Krause ED, Kaltman S, Goodman LA, Dutton MA. Avoidant coping and PTSD symptoms related to domestic violence exposure: a longitudinal study. J Trauma Stress. 2008;21(1):83–90. doi: 10.1002/jts.20288. [DOI] [PubMed] [Google Scholar]